Overview
The ADA criteria for prediabetes include specific thresholds for fasting plasma glucose, oral glucose tolerance tests, and HbA1c levels, which help identify individuals at risk for developing type 2 diabetes. The article emphasizes the importance of these criteria in facilitating early detection and management, as well as the need for holistic lifestyle changes to prevent progression to type 2 diabetes and reduce associated healthcare costs.
Introduction
The escalating prevalence of prediabetes presents a significant public health challenge, with nearly 88 million adults in the United States currently affected. Defined by specific thresholds in blood glucose and HbA1c levels, prediabetes serves as a crucial warning sign for individuals at risk of developing type 2 diabetes.
The American Diabetes Association (ADA) has established clear diagnostic criteria to facilitate early detection and intervention, emphasizing the importance of lifestyle modifications in reversing this condition. As the economic burden of diabetes continues to rise, understanding the implications of prediabetes and implementing effective management strategies is essential.
This article delves into the ADA’s guidelines, the critical role of lifestyle changes, and the pressing need for proactive screening to combat the progression from prediabetes to type 2 diabetes.
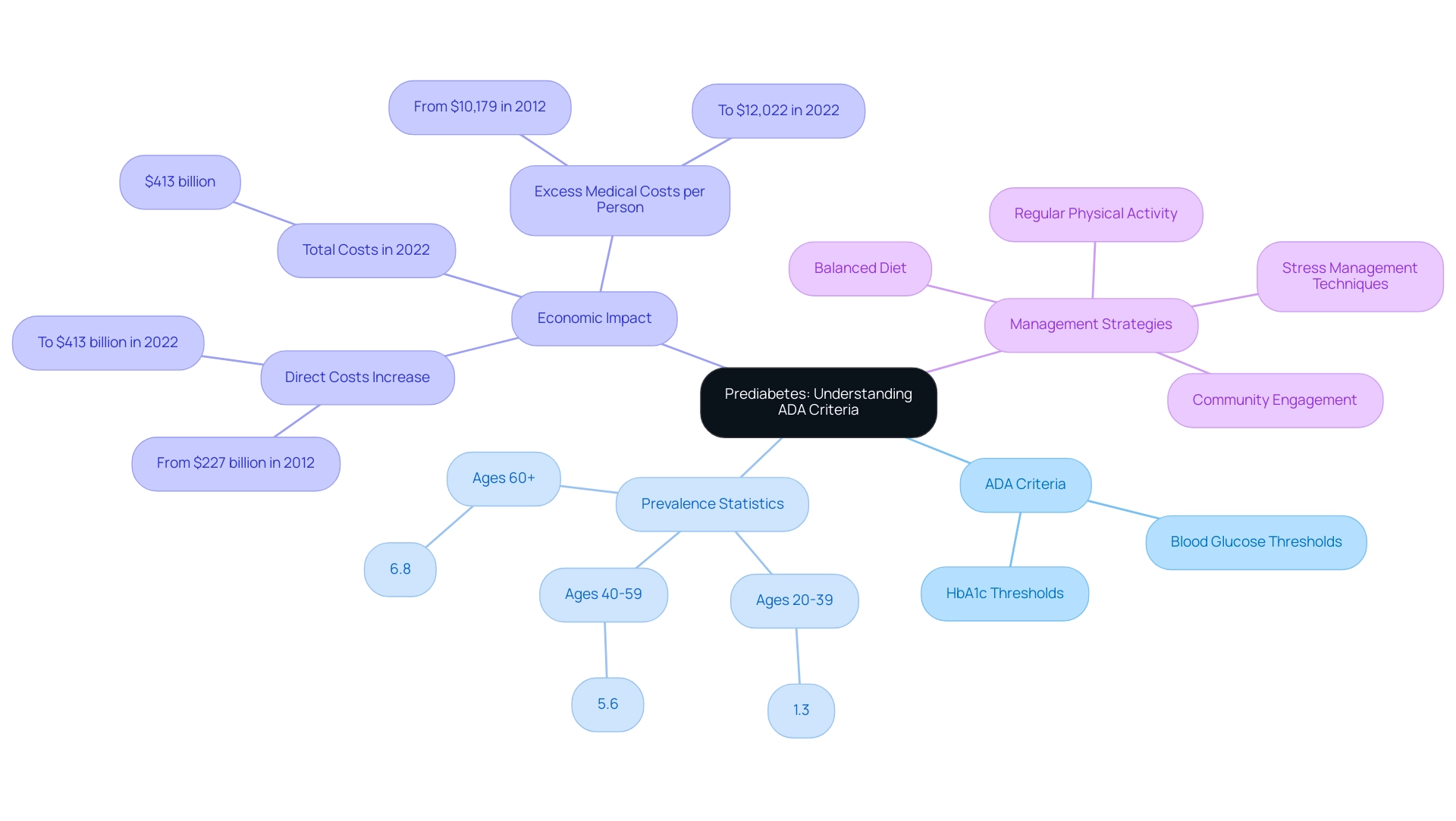
Defining Prediabetes: Understanding the ADA Criteria
Prediabetes is a serious health issue characterized by increased blood glucose levels that do not meet the ADA criteria for prediabetes. The American Diabetes Association (ADA) outlines the ADA criteria for prediabetes, defining elevated blood sugar levels based on specific thresholds for blood glucose and HbA1c, which serve as a crucial indicator that a person is at increased risk for developing type 2 sugar intolerance. Recent statistics reveal that the prevalence of undiagnosed diabetes has escalated, particularly among older adults, with rates increasing from:
- 1.3% in adults ages 20–39
- 5.6% for ages 40–59
- 6.8% for age 60 and older
According to the National Center for Health Statistics, this emphasizes the urgency of addressing elevated blood sugar levels through effective lifestyle changes and holistic approaches that empower patients. In 2024, current estimates indicate that nearly 88 million adults in the United States are living with prediabetes, which underscores the importance of understanding the ADA criteria for prediabetes for timely intervention. The economic consequences are significant; the total direct and indirect expenses related to diagnosed conditions reached an estimated $413 billion in 2022, with direct costs rising from $227 billion in 2012.
This reflects a growing burden on healthcare systems and emphasizes the need for enhanced management and prevention efforts for this condition. Early intervention strategies, such as embracing nature, nutrition, and community support, can significantly mitigate this risk. The identification of prediabetes according to the ADA criteria for prediabetes is not just a diagnostic tool but also a prompt for improved management and preventive initiatives, ultimately striving to lessen the shift to type 2 and enhance overall outcomes.
Specifically, adopting four essential strategies—such as:
- A balanced diet rich in whole foods
- Regular physical activity
- Stress management techniques
- Community engagement
can enhance health outcomes. Additionally, from 2012 to 2022, excess medical costs per person related to this condition increased from $10,179 to $12,022, further illustrating the financial burden of this ailment.
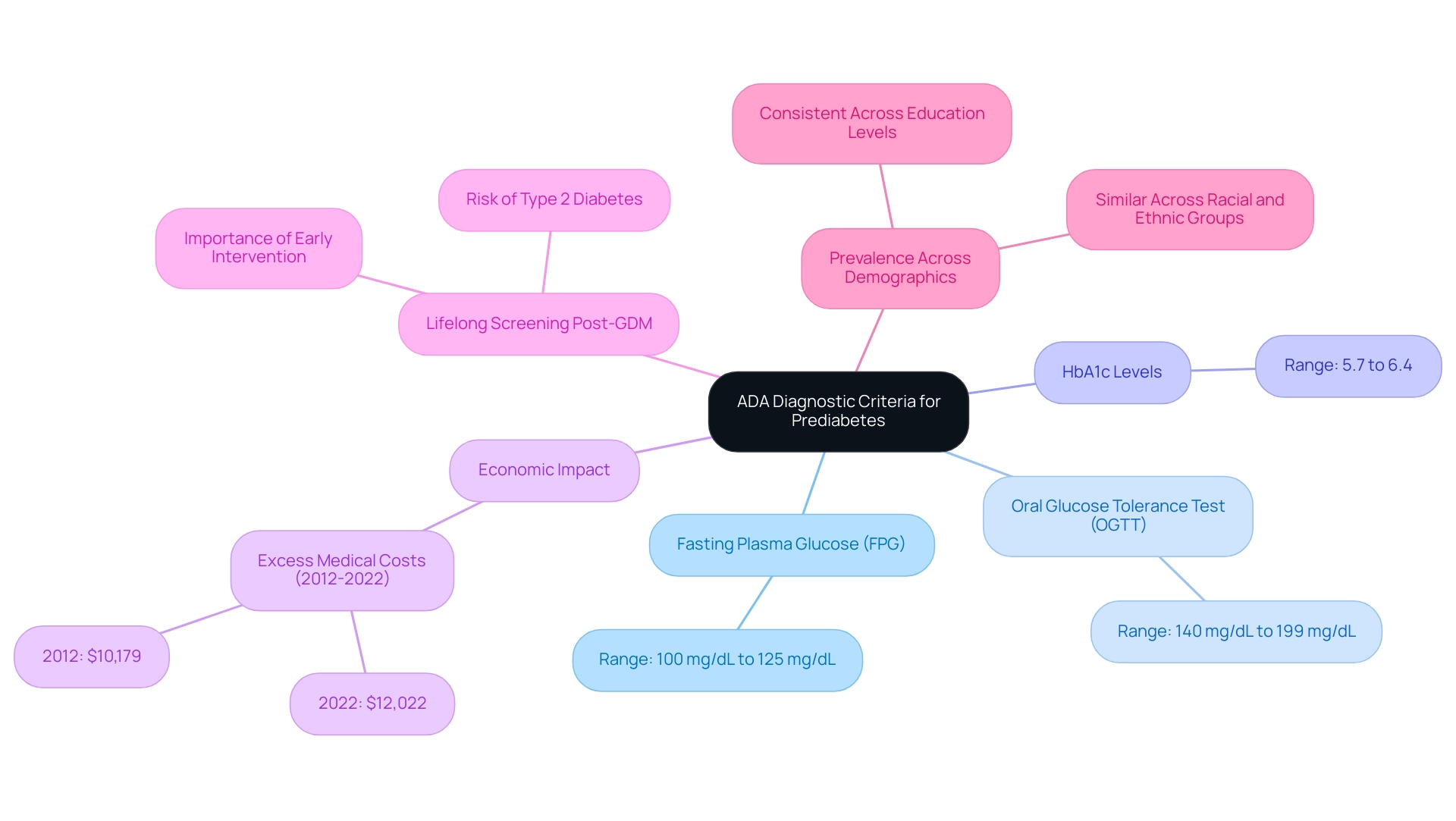
ADA Diagnostic Criteria for Prediabetes: Key Measurements and Thresholds
The American Diabetes Association (ADA) has established ADA criteria for prediabetes, which are essential for diagnosing elevated blood sugar levels and facilitating early detection and management to prevent complications such as gestational diabetes. The ADA criteria for prediabetes include:
- Fasting Plasma Glucose (FPG) levels ranging from 100 mg/dL to 125 mg/dL
- Oral Glucose Tolerance Test (OGTT) results indicating blood sugar levels between 140 mg/dL and 199 mg/dL two hours post glucose intake
- HbA1c levels falling within the 5.7% to 6.4% range
These measurements are crucial for healthcare providers, as they not only aid in diagnosing at-risk individuals but also serve as a foundation for developing targeted management plans.
The prevalence of prediabetes is consistent across various racial and ethnic groups and education levels, underscoring the widespread impact of this condition. Furthermore, from 2012 to 2022, excess medical costs per person related to the condition rose significantly from $10,179 to $12,022, highlighting the economic burden and the importance of early diagnosis. Recent findings highlight the significance of monitoring FPG levels, as the cumulative points score for categorization can range from 0 to 17, indicating varying degrees of vulnerability among individuals.
A case study titled ‘Lifelong Screening for Diabetes Post-GDM’ illustrates the practical application of these diagnostic criteria; it shows that individuals diagnosed with gestational diabetes mellitus (GDM) should undergo lifelong screening for prediabetes and type 2 disorders, facilitating early intervention and treatment. This structured approach, which aligns with an integrative method to managing the condition, is supported by experts who advocate for adherence to the ADA criteria for prediabetes, thereby reinforcing the necessity of early intervention and continuous management to mitigate the risk of progression to type 2. Additionally, it is crucial to recognize the dangers associated with traditional treatments for insulin resistance, which can lead to severe outcomes.
Therefore, adopting crucial approaches for managing blood sugar levels during pregnancy is essential to prevent gestational complications and ensure the well-being of both the mother and child.
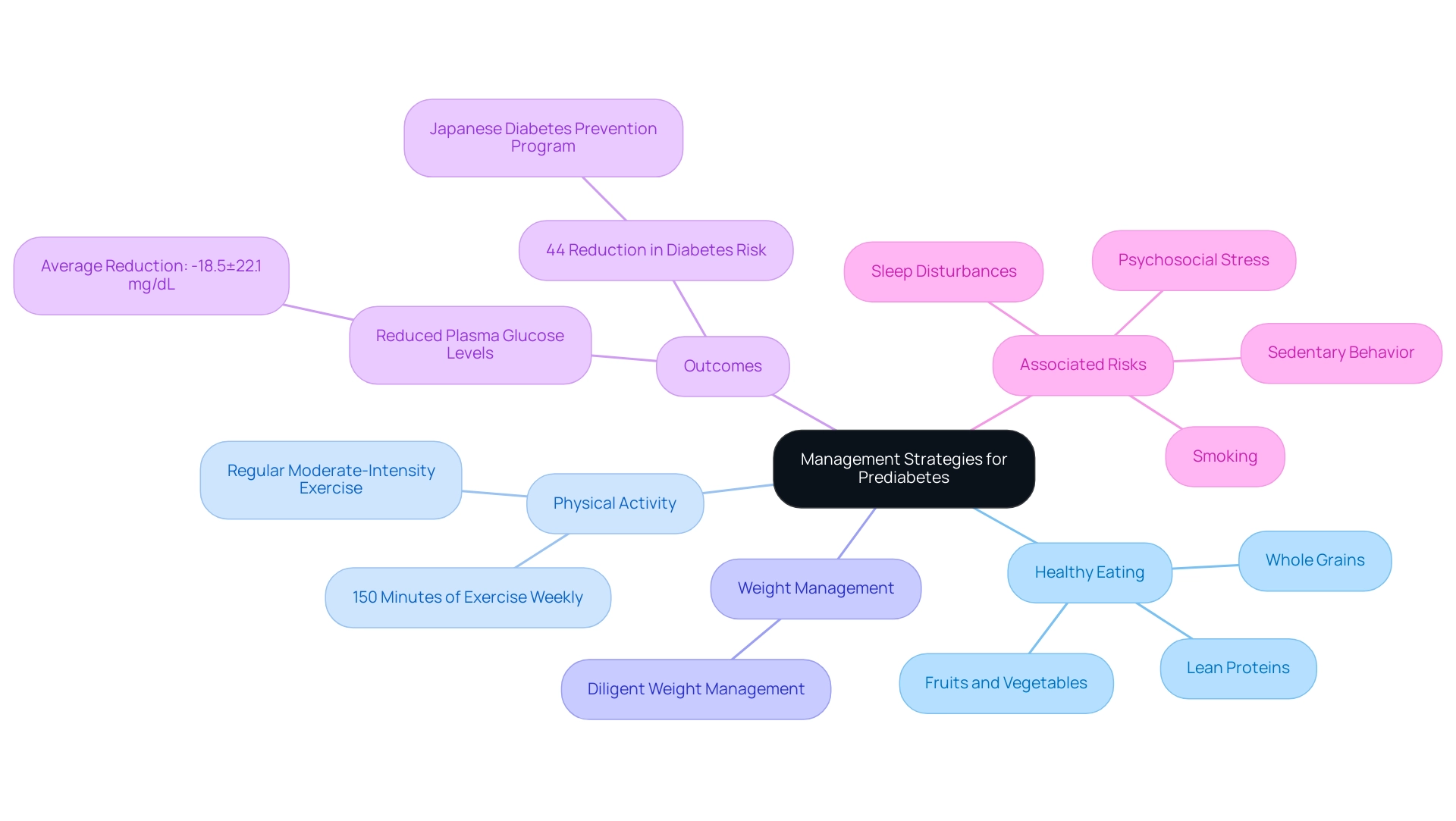
Lifestyle Modifications and Management Strategies for Prediabetes
Lifestyle modifications are essential in effectively managing prediabetes, as outlined in the ADA criteria for prediabetes by the American Diabetes Association. Their guidelines recommend a comprehensive approach that aligns with the ADA criteria for prediabetes, including:
- Healthy eating
- Regular physical activity
- Diligent weight management
Specifically, individuals are encouraged to engage in at least 150 minutes of moderate-intensity exercise each week.
Dietary adjustments should focus on whole grains, fruits, vegetables, and lean proteins to enhance general well-being and decrease the likelihood of developing diabetes. At the Integrative Wellness Center, we promote a comprehensive method to reversing the condition that addresses root causes and empowers patient well-being. This approach not only aims to enhance physical well-being but also seeks to alleviate the anxiety that accompanies the concern surrounding potential complications of this condition.
As Murray Heimberg, MD, PhD, stated, ‘Implementing structured lifestyle changes is essential in the battle against elevated blood sugar levels and its advancement to type 2 conditions.’ Evidence shows that participants who reversed to normal glucose regulation (NGR) experienced a notable decrease in two-hour plasma glucose levels, averaging a reduction of −18.5±22.1 mg/dL, compared to only −1.29±19.0 mg/dL among those with persistent prediabetes. Additionally, smoking, inactivity, sleep issues, and psychological stress are associated with heightened susceptibility to health problems, emphasizing the significance of tackling these elements in lifestyle modifications.
The Japanese Diabetes Prevention Program exemplifies the success of such holistic interventions, where participants received consistent individual instructions and lifestyle support over three years, achieving a remarkable 44% reduction in risk for the condition. These statistics highlight the significant effect that targeted lifestyle changes can have in preventing the progression to type 2, as also shown in the study by Kosaka et al., which stressed the effectiveness of lifestyle intervention in preventing type 2 in Japan. By re-evaluating the origin of your condition, we can tackle well-being at the root level using a comprehensive approach.
Understanding the Risks: Progression from Prediabetes to Type 2 Diabetes
Individuals identified with prediabetes according to the ADA criteria for prediabetes face an increased risk of advancing to type 2, with research showing that without adequate intervention, 15% to 30% of these individuals will progress to the condition within five years. This progression can lead to serious health complications, including:
- Cardiovascular diseases
- Nerve damage
- Kidney dysfunction
As Wagenknecht LE notes, ‘Data are model-adjusted incidence estimates,’ emphasizing the significance of these statistics.
In Utah, the condition is projected to affect 10.2% of the population by 2030, while states like Alabama, Florida, and Mississippi may exceed 18%. According to recent research, intensive lifestyle changes provided at the Integrative Wellness Center can lower the likelihood of developing type 2 conditions by an impressive 58% among overweight or obese adults with elevated blood sugar. For instance, one patient, after engaging in a tailored nutrition and exercise program, successfully reversed their prediabetes status, showcasing the transformative impact of our approach.
Furthermore, gestational diabetes often serves as an indicator of underlying β-cell dysfunction, elevating the likelihood of later diabetes in mothers and highlighting the necessity for lifelong screening. Comprehending insulin resistance is essential, as conventional therapies can occasionally worsen the condition, resulting in serious complications. These findings emphasize the critical significance of early detection and proactive lifestyle changes in line with the ADA criteria for prediabetes, enabling patients to take control of their well-being.
Supervising and tackling these challenges not only helps in averting blood sugar issues but also reduces the likelihood of related health complications, thus highlighting the importance of continuous awareness and management of prediabetes through a comprehensive approach.
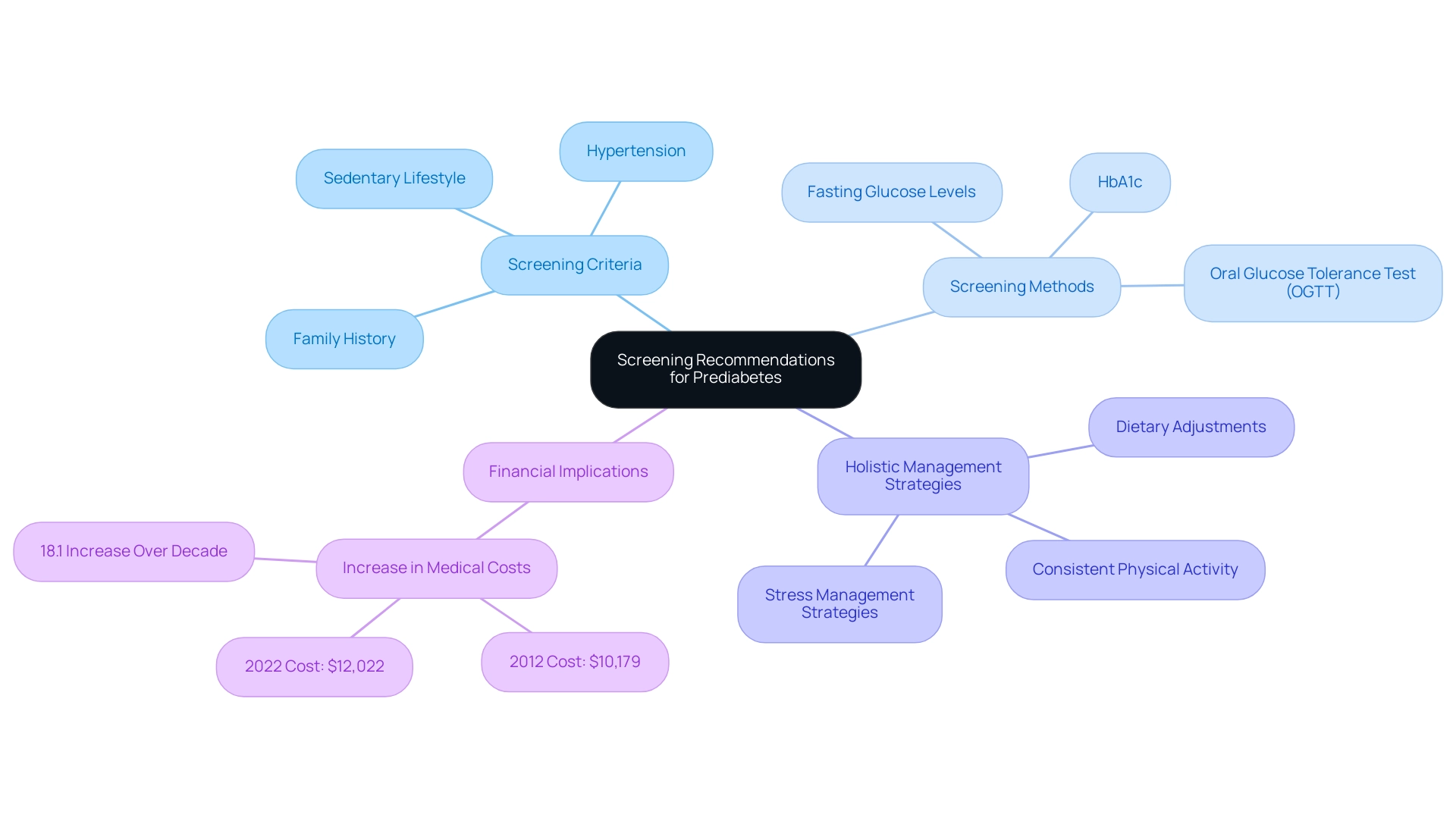
Screening Recommendations: How the ADA Identifies Prediabetes
The American Diabetes Association (ADA) emphasizes the importance of regular screening for adults aged 45 and older, particularly for those who are overweight or meet the ADA criteria for prediabetes, including factors such as:
- A family history of this condition
- Hypertension
- A sedentary lifestyle
However, addressing this condition requires more than just screening; it calls for a holistic approach that tackles the root causes of the disease. This method not only aims to manage blood sugar levels effectively but also seeks to alleviate the anxiety that often accompanies concerns about potential complications.
The financial implications of this condition are significant, with excess medical costs per person rising from $10,179 in 2012 to $12,022 in 2022, representing an 18.1% increase over the decade, highlighting the urgent need for proactive management. Screening methods include blood tests that evaluate:
- Fasting glucose levels
- HbA1c
- Outcomes from an Oral Glucose Tolerance Test (OGTT)
As Dr. Jill Jin mentions in the JAMA Patient Page, ‘early identification of prediabetes, according to the ADA criteria for prediabetes, is crucial for effective management and can significantly halt the progression to type 2 conditions.’
Moreover, empowering patients through functional medicine can lead to better management strategies for Type 2 conditions, hypothyroidism, and cognitive decline. For example, a comprehensive routine may involve:
- Dietary adjustments
- Consistent physical activity
- Stress management strategies
All of which can aid in decreasing anxiety and enhancing overall well-being. Recent trends indicate a concerning rise in the incidence of this condition among U.S. children and adolescents, especially among non-Hispanic Black youth, further underscoring the need for robust screening programs.
Thus, timely screening, combined with a holistic approach, not only aids in individual health management but also contributes to broader public health strategies aimed at mitigating the burden of diabetes in the population.
Conclusion
The alarming rise in prediabetes prevalence highlights an urgent public health issue that demands immediate attention. With nearly 88 million American adults currently affected, understanding the American Diabetes Association’s diagnostic criteria is essential for early detection and intervention. Recognizing the thresholds for:
- Fasting plasma glucose
- HbA1c levels
- Oral glucose tolerance tests
provides a framework for timely action that can significantly alter health trajectories.
Implementing lifestyle modifications remains the cornerstone of managing prediabetes. By embracing a balanced diet, engaging in regular physical activity, and addressing psychosocial stressors, individuals can effectively reduce their risk of progressing to type 2 diabetes. The evidence is clear: structured lifestyle changes not only lower blood glucose levels but also enhance overall well-being, as demonstrated by successful interventions across various programs.
Moreover, the necessity for proactive screening cannot be understated. Regular assessments for those at risk—especially adults over 45 or those with additional risk factors—are critical for identifying prediabetes early. This approach, coupled with a holistic view of health management, empowers individuals to take control of their health and mitigate the potential complications associated with diabetes.
In summary, the fight against prediabetes is a collective responsibility that requires both individual commitment and systemic support. By prioritizing early detection, lifestyle interventions, and comprehensive screening practices, it is possible to reverse the trend of rising diabetes rates and foster a healthier future for all.
Frequently Asked Questions
What is prediabetes and why is it a serious health issue?
Prediabetes is a serious health issue characterized by increased blood glucose levels that do not meet the criteria for diabetes. It indicates a higher risk for developing type 2 diabetes and requires timely intervention.
What are the ADA criteria for diagnosing prediabetes?
The ADA criteria for prediabetes include: 1. Fasting Plasma Glucose (FPG) levels ranging from 100 mg/dL to 125 mg/dL. 2. Oral Glucose Tolerance Test (OGTT) results indicating blood sugar levels between 140 mg/dL and 199 mg/dL two hours after glucose intake. 3. HbA1c levels falling within the 5.7% to 6.4% range.
What are the prevalence rates of prediabetes among different age groups?
The prevalence of undiagnosed diabetes has increased among older adults: 1. 1.3% in adults ages 20–39. 2. 5.6% for ages 40–59. 3. 6.8% for age 60 and older.
How many adults in the United States are estimated to be living with prediabetes?
In 2024, it is estimated that nearly 88 million adults in the United States are living with prediabetes.
What are the economic implications of prediabetes?
The economic consequences of prediabetes are significant, with total direct and indirect expenses related to diagnosed conditions reaching an estimated $413 billion in 2022, and excess medical costs per person increasing from $10,179 in 2012 to $12,022 in 2022.
What strategies can help manage and prevent prediabetes?
Essential strategies for managing and preventing prediabetes include: – A balanced diet rich in whole foods. – Regular physical activity. – Stress management techniques. – Community engagement.
Why is early intervention important for individuals diagnosed with gestational diabetes?
Early intervention is crucial for individuals diagnosed with gestational diabetes mellitus (GDM) to undergo lifelong screening for prediabetes and type 2 disorders, facilitating timely treatment and reducing the risk of complications.