Overview
Managing diabetes can be a challenging journey, and understanding your blood sugar levels is crucial. The Glucose Management Indicator (GMI) offers a compassionate approach by estimating average blood sugar levels through continuous glucose monitoring (CGM) data. This method provides immediate insights into glucose trends, surpassing traditional HbA1c tests.
It’s important to recognize that GMI has practical applications in diabetes management. By highlighting individual glucose patterns, it empowers you to make informed decisions about your health. Many patients find that this personalized approach not only enhances their understanding but also supports their overall well-being.
However, there is still a need for further research to enhance GMI’s accuracy and reliability. This ongoing work is essential in providing you with the best tools for personalized diabetes care. Together, we can navigate this path toward healthier living and improved management of your condition.
Introduction
In the journey of managing diabetes, it’s essential to recognize the challenges that come with understanding glucose metrics. Many patients find that grasping these nuances can significantly impact their health outcomes. The Glucose Management Indicator (GMI) stands out as a transformative tool, offering a timely glimpse into average blood glucose levels based on continuous glucose monitoring (CGM) data. Unlike traditional measures like hemoglobin A1c (HbA1c), GMI provides insights that reflect recent glucose trends. This allows for more immediate adjustments in treatment strategies, which can be incredibly reassuring for those navigating their diabetes.
As healthcare evolves, it’s becoming increasingly clear how GMI, when paired with lifestyle modifications and personalized care, can empower individuals to take charge of their health. This holistic approach not only enhances diabetes management but also fosters a sense of control and well-being. It’s important to recognize that every small step taken toward understanding and managing diabetes is a step toward a healthier future.
Define the Glucose Management Indicator (GMI)
The Diabetes GMI serves as a vital tool for estimating average blood sugar levels over time, drawing from continuous sugar monitoring (CGM) data. It provides an estimate of the hemoglobin A1c (HbA1c) level, a standard measure for assessing long-term sugar regulation for those facing blood sugar challenges. By transforming CGM average sugar readings into an estimated HbA1c percentage, GMI reflects sugar levels over the previous 14 days. This metric, known as diabetes gmi, is particularly beneficial for diabetes management, as it offers a more immediate insight into sugar trends compared to traditional HbA1c tests, which reflect averages over two to three months.
It’s important to recognize that incorporating holistic lifestyle strategies can significantly enhance the effectiveness of diabetes gmi in managing type 2 diabetes. For example, a balanced diet rich in local produce, such as avocados and berries, can support better glucose control. Many patients find that regular physical activity, made enjoyable by the scenic parks and trails in San Marcos, not only improves insulin sensitivity but also complements the insights gained from GMI readings. Additionally, engaging with community wellness programs can provide essential support and resources tailored to individual needs, empowering patients to make informed health decisions.
Recent studies highlight the need for larger, multi-national research to better understand GMI’s clinical implications, particularly concerning HbA1c levels. A study conducted at the University of Washington Diabetes Care Center analyzed data from 641 individuals, revealing significant discrepancies between GMI and actual A1c levels; only 11% of participants had less than a 0.1 percentage point difference between their GMI and A1c. Factors such as the type of blood sugar condition and kidney function influenced these discrepancies. Such findings emphasize the importance of diabetes GMI in delivering timely insights for individuals managing their condition, ultimately enabling them to make informed health choices. Additionally, studies indicate that people of color have slightly higher average A1C levels than white individuals, underscoring the relevance of diabetes GMI in diverse populations. For personalized guidance and support tailored to your unique needs, consider reaching out to Dr. Jason Shumard in San Marcos, CA. He is dedicated to helping you navigate your diabetes management journey with compassion and expertise.
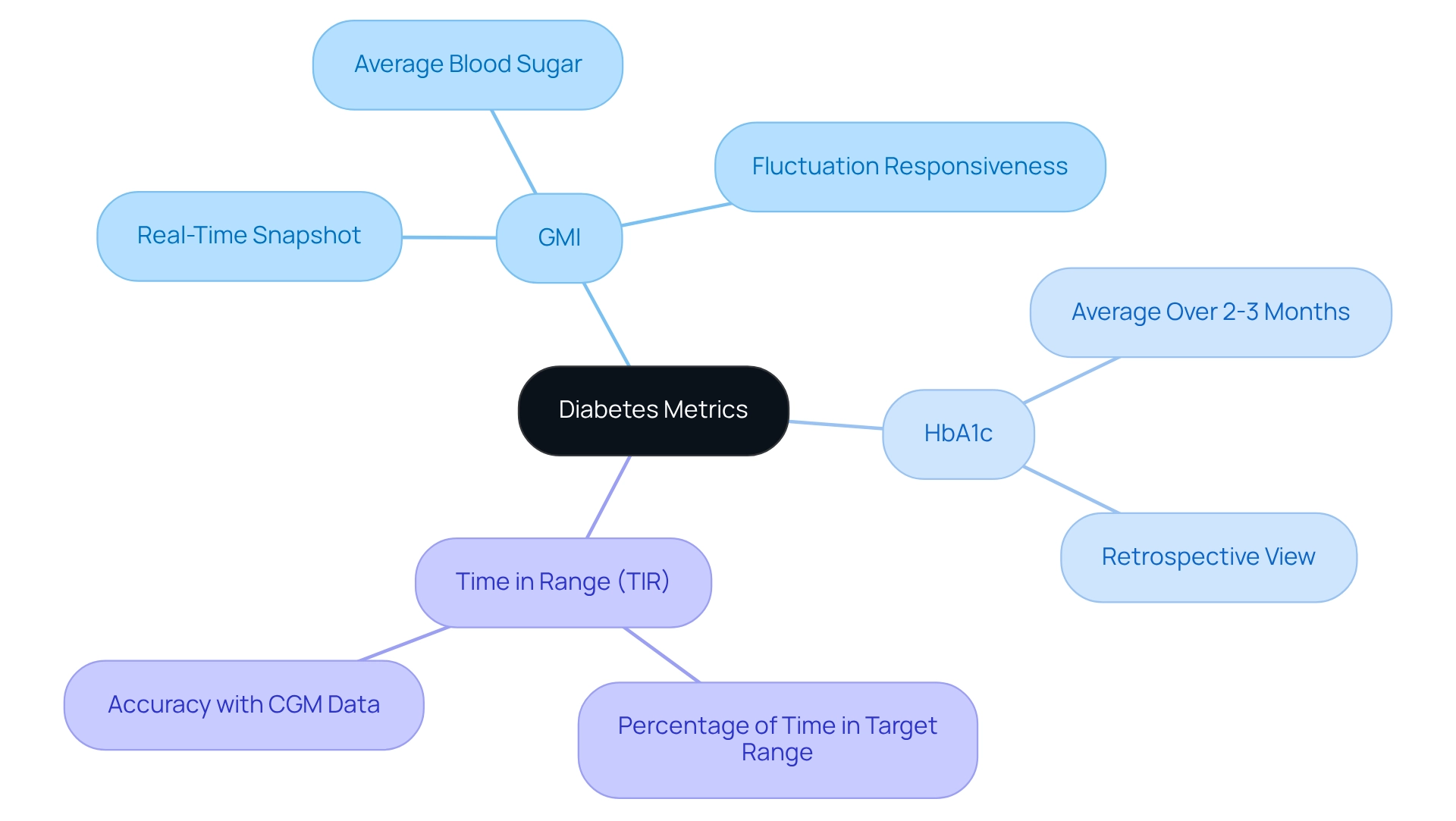
Differentiate GMI from HbA1c and Other Metrics
It’s important to recognize that diabetes gmi and HbA1c differ significantly in their approach to measuring sugar levels. While HbA1c reflects an average of blood sugar levels over two to three months, providing a retrospective view, it may not capture recent fluctuations. In contrast, diabetes gmi, which is derived from continuous monitoring of blood sugar data, offers a real-time snapshot of sugar levels. This responsiveness is vital, as it enables individuals to respond quickly to fluctuations in their blood sugar levels, and many patients find that diabetes GMI is derived from average blood sugar levels, revealing variations that HbA1c might overlook.
Additional metrics, such as time in range (TIR), enhance these measurements by showing the percentage of time an individual’s blood sugar levels stay within a target range. This broader view on sugar control is essential for both patients and healthcare providers. For instance, studies indicate that 14 days or more of CGM data can yield a more accurate estimate of time spent in hypoglycemia and glucose variability. Furthermore, for a cohort of 528 individuals, the absolute value of the difference between the diabetes gmi and laboratory A1C was ≥1.0% for 2–4% of values, highlighting the significance of employing multiple metrics for effective management of the condition.
Jason Shumard emphasizes health education by providing resources, including his comprehensive guide on reversing diabetes, available for free at events. This approach not only educates individuals about their conditions but also enables them to take control of their health. As highlighted in transformative experiences, individuals have expressed gratitude for the knowledge gained. One individual remarked, ‘Comprehending these metrics is essential for individuals to manage their treatment choices efficiently.’ By grasping the nuances between diabetes gmi, HbA1c, and TIR, patients can better navigate their treatment options and enhance their overall health outcomes. This aligns with the broader trend towards personalized health management, where understanding individual metrics plays a crucial role in tailoring effective care.
Explore Practical Applications of GMI in Diabetes Management
The practical applications of the diabetes GMI in diabetes management are extensive and impactful. It’s important to recognize that diabetes GMI enables individuals and healthcare professionals to identify patterns in blood sugar levels. This capability enables prompt actions that can help avert complications. By consistently monitoring diabetes GMI, individuals can make informed adjustments to their dietary choices, physical activity, and medication dosages to achieve optimal blood sugar control.
Many patients find that diabetes GMI serves as a motivational resource, inspiring them to embrace healthier habits by providing timely feedback on their blood sugar management efforts. This real-time information empowers individuals to take charge of their health, fostering a proactive approach to diabetes GMI management.
In educational settings, diabetes GMI serves as a valuable tool for teaching individuals about the effects of lifestyle choices on their glucose levels. For instance, starting a structured walking program can significantly enhance overall wellness and vitality. Individuals are encouraged to evaluate their current fitness levels and set realistic goals, such as committing to a daily walk of 10-15 minutes. Tracking progress through journals or apps can help maintain motivation and celebrate achievements along the way. As noted in the user manual, organized strolling initiatives have a success rate of 89.5%, highlighting the effectiveness of a structured approach.
A case study from Dr. Shumard’s center demonstrates how individuals have effectively utilized diabetes GMI to modify their lifestyle choices, resulting in substantial enhancements in their health outcomes. One individual, diagnosed with a blood sugar condition at a young age, has not only managed her situation effectively but has also completed over 78 marathons. This showcases the potential of diabetes GMI in inspiring lifestyle changes. This success story aligns with the innovative methodologies employed at Dr. Shumard’s center, which focus on personalized care and education.
Statistics indicate that advanced models, including machine learning and linear regression, have decreased HbA1c estimation errors by as much as 26% compared to conventional GMI formulas. This highlights the significance of precise glucose monitoring in care. As Jennifer Larson aptly states, “This is important because the more you can keep your blood sugar levels in that range, the less likely you are to develop complications.” As we progress through 2025, the incorporation of diabetes GMI into blood sugar management continues to advance, offering individuals the resources they need to regain their health and improve their quality of life. Additionally, tools like Bezzy can be accessed via web or mobile app for community support, further aiding patients in their diabetes management journey.
Evaluate the Accuracy and Reliability of GMI
The accuracy and reliability of diabetes GMI have been the focus of extensive research, showcasing its importance in estimating HbA1c levels. However, it’s important to recognize that GMI does not always correlate perfectly with laboratory measurements. Individual differences in hemoglobin glycation rates and the duration of continuous glucose monitoring (CGM) usage can significantly influence diabetes GMI readings. For instance, a study titled “Individualizing Diabetes Treatment Based on GMI and HbA1c” found that participants with HbA1c values nearing 9% were up to 24% more likely to have GMI estimates within 0.5 percentage points of their actual HbA1c levels. This underscores the variability in accuracy across different populations.
Many patients find that GMI may sometimes overestimate or underestimate HbA1c levels, particularly in those with specific health conditions, such as anemia or certain hemoglobinopathies. This variability necessitates a cautious interpretation of diabetes GMI results, emphasizing the need for clinicians to consider diabetes GMI alongside other clinical data and patient-specific factors. As Elizabeth Selvin from the Johns Hopkins Bloomberg School of Public Health states, “We recommend that clinicians rely on mean glucose directly from CGM, not GMI, an estimated HbA1c value.” By combining GMI with thorough individual evaluations, healthcare providers can enhance management strategies tailored to specific needs.
Incorporating personalized functional medicine strategies, such as those offered by Dr. Jason Shumard at the Integrative Wellness Center, can further improve the management of blood sugar conditions. By focusing on tailored nutrition and state-of-the-art testing, patients can receive individualized treatment plans that address their unique health profiles. Furthermore, adopting lifestyle changes like a balanced diet, regular exercise, and effective stress management is essential for managing Type 2 diabetes effectively.
Current studies, supported by multiple research grants and organizations, continue to enhance our understanding of the diagnostic abilities of diabetes GMI, emphasizing its significance in personalized care for metabolic disorders. As the field evolves, it is crucial for practitioners to stay informed about the latest findings regarding the accuracy and reliability of diabetes GMI, ensuring that patients receive the most effective and individualized treatment possible. For personalized guidance and support tailored to your unique needs, consider reaching out to Dr. Shumard. Schedule Now.
The Future of GMI in Diabetes Care
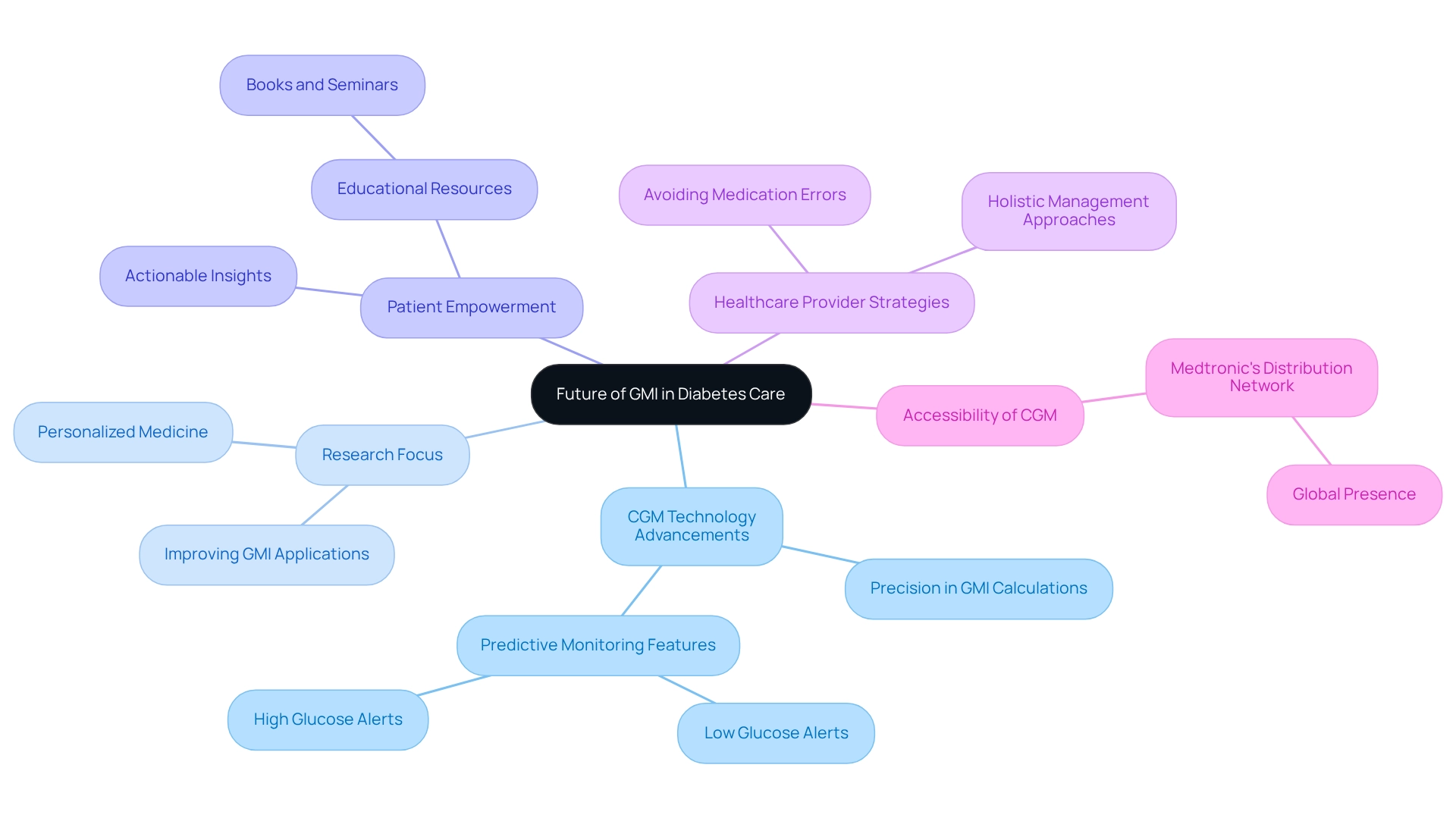
The future of the Glucose Management Indicator (GMI) in blood sugar care is indeed promising, particularly due to the remarkable progress in continuous glucose monitoring (CGM) technology. As CGM devices become integral to management plans, we can expect a rise in the use of diabetes GMI. It’s important to recognize that research will likely focus on improving the precision of GMI calculations, which could lead to more tailored applications for diverse populations.
Many patients find that understanding their glucose levels can be transformative. For instance, studies have shown that the mean CGM sugar level dropped from 8.3±2.5 mmol/l to 8.2±1.6 mmol/l after self-monitoring blood sugar (SMBG), and then significantly to 7.7±1.6 mmol/l at the end of the CGM period, underscoring the effectiveness of CGM technology in managing sugar levels (P<0.05). With healthcare providers increasingly prioritizing personalized medicine, GMI is poised to play a vital role in crafting management strategies that meet individual needs.
Moreover, the incorporation of predictive elements in CGM systems, such as notifications for low and high sugar levels, will enhance monitoring capabilities, enabling proactive management of diabetes GMI. Dr. Jason Shumard emphasizes, “By providing individuals with actionable insights and practical tools, the center fosters an environment where people can reclaim their health and well-being.” This comprehensive approach is especially crucial in hospital settings, where precise sugar management can help avoid medication errors and improve overall health outcomes.
Overall, the diabetes GMI is on track to become a fundamental component of blood sugar management, significantly enhancing our ability to monitor and control glucose levels effectively. Furthermore, Dr. Shumard’s educational materials empower individuals to understand diabetes GMI as well as CGM technology, aligning with the center’s holistic strategy for managing diabetes. The robust distribution network of companies like Medtronic, operating in over 150 countries, further enhances the accessibility of CGM technology, providing patients with valuable options for their diabetes GMI journey.
Conclusion
The Glucose Management Indicator (GMI) marks a significant step forward in diabetes management, offering a real-time perspective on blood glucose levels that traditional metrics like hemoglobin A1c (HbA1c) simply cannot provide. By utilizing continuous glucose monitoring (CGM) data, GMI empowers individuals to make timely adjustments to their treatment strategies, enhancing their ability to manage diabetes effectively. Moreover, integrating lifestyle modifications—such as improved diet and physical activity—can amplify the benefits of GMI, encouraging patients to take control of their health.
It’s important to recognize the differences between GMI, HbA1c, and other metrics, as understanding these distinctions is crucial for both patients and healthcare providers. Each metric provides unique insights into glucose control. When leveraged collectively, they can lead to more informed decisions in diabetes management. The practical applications of GMI extend beyond mere numbers; they serve as a motivational tool and an educational resource, fostering a proactive approach among patients.
Many patients find that while GMI presents a promising future, it’s essential to acknowledge the variability in its accuracy and reliability across different populations. Ongoing research will continue to refine GMI’s applications, ensuring it aligns with the evolving landscape of personalized diabetes care. As advancements in CGM technology continue to emerge, GMI is poised to play an integral role in shaping the future of diabetes management, ultimately leading to improved health outcomes for individuals navigating this chronic condition. Together, we can embrace these advancements and take meaningful steps toward better health.
Frequently Asked Questions
What is the Diabetes GMI and how is it used?
The Diabetes GMI (Glucose Management Indicator) is a tool that estimates average blood sugar levels over time using continuous glucose monitoring (CGM) data. It provides an estimate of the hemoglobin A1c (HbA1c) level, reflecting sugar levels over the previous 14 days, which aids in diabetes management by offering immediate insights into sugar trends.
How does Diabetes GMI differ from traditional HbA1c tests?
While HbA1c reflects average blood sugar levels over two to three months, providing a retrospective view, Diabetes GMI offers a real-time snapshot of sugar levels based on continuous monitoring. This allows individuals to respond quickly to fluctuations in their blood sugar levels.
What lifestyle strategies can enhance the effectiveness of Diabetes GMI?
Incorporating holistic lifestyle strategies, such as maintaining a balanced diet rich in local produce and engaging in regular physical activity, can significantly enhance the effectiveness of Diabetes GMI in managing type 2 diabetes.
What do recent studies say about the accuracy of Diabetes GMI compared to actual HbA1c levels?
Recent studies indicate that there can be significant discrepancies between GMI and actual HbA1c levels. For example, a study at the University of Washington found that only 11% of participants had less than a 0.1 percentage point difference between their GMI and HbA1c levels, with factors like blood sugar condition type and kidney function influencing these discrepancies.
Why is understanding Diabetes GMI important for diverse populations?
Studies suggest that people of color have slightly higher average A1C levels than white individuals, highlighting the relevance of Diabetes GMI in providing timely insights for effective diabetes management across diverse populations.
What additional metrics can be used alongside Diabetes GMI for better diabetes management?
Additional metrics, such as time in range (TIR), can enhance diabetes management by showing the percentage of time an individual’s blood sugar levels stay within a target range, providing a broader view of glucose control.
How can individuals learn more about managing their diabetes?
Individuals can gain insights and personalized guidance by reaching out to healthcare professionals, such as Dr. Jason Shumard, who offers resources and education on diabetes management, including a comprehensive guide on reversing diabetes available at events.