Introduction
Understanding the complex relationship between alcohol consumption and blood sugar levels is essential for individuals managing diabetes. Alcohol can have unpredictable effects on glucose levels, leading to both hypoglycemia and hyperglycemia, depending on various factors such as:
- The type of alcohol
- The quantity consumed
- Whether food is ingested alongside
This article delves into the nuances of how alcohol interacts with blood sugar management, providing:
- Evidence-based strategies for safe consumption
- Insights on reading alcohol labels
- The importance of communication with healthcare providers
By recognizing the signs of blood sugar fluctuations and developing a personalized action plan, individuals can make informed choices that support their health and well-being while navigating social situations involving alcohol.
The Interplay Between Alcohol and Blood Sugar Levels
Beverage consumption can significantly influence blood sugar levels, leading to both increases and decreases based on several factors, including the quantity and type of beverage consumed, as well as whether it is ingested with food. When alcohol and blood sugar are present, the liver prioritizes the metabolism of ethanol over glucose production, which impairs glucose availability in the bloodstream. This shift often results in hypoglycemia, particularly when beverages containing alcohol and blood sugar are consumed on an empty stomach.
A systematic review highlighted a notable finding: growth hormone secretion was significantly diminished between midnight and 4:00 a.m., indicating potential disruptions in metabolic processes during this period. Conversely, the relationship between alcohol and blood sugar can lead to increases in blood sugar levels when consuming alcoholic drinks high in sugar. Individuals managing type 2 conditions must exercise caution, as these fluctuations can complicate their situation and elevate the risk of severe hypoglycemic episodes.
A randomized parallel study conducted by Zheng in 2012 illustrated the effects of ethanol on insulin sensitivity, showcasing how variations in consumption contribute to differing insulin and glucose levels among participants. Furthermore, the ‘sick-quitter effect’ observed by Dolly O Baliunas highlights the dangers linked to avoiding beverages for health reasons, potentially raising the risk of developing blood sugar issues. This highlights the importance of careful reflection on beverage intake in blood sugar management.
Consistent observation of glucose levels prior to and following consumption is recommended to enhance understanding of personal reactions, thereby facilitating more efficient management of the condition. Furthermore, tackling the underlying factors of the illness can assist in reducing the stress that frequently comes with concerns about possible complications. By adopting a comprehensive regimen that includes understanding the effects of alcohol and blood sugar on glucose levels, patients can empower themselves to manage their health more effectively.
Strategies for Managing Blood Sugar While Drinking Alcohol
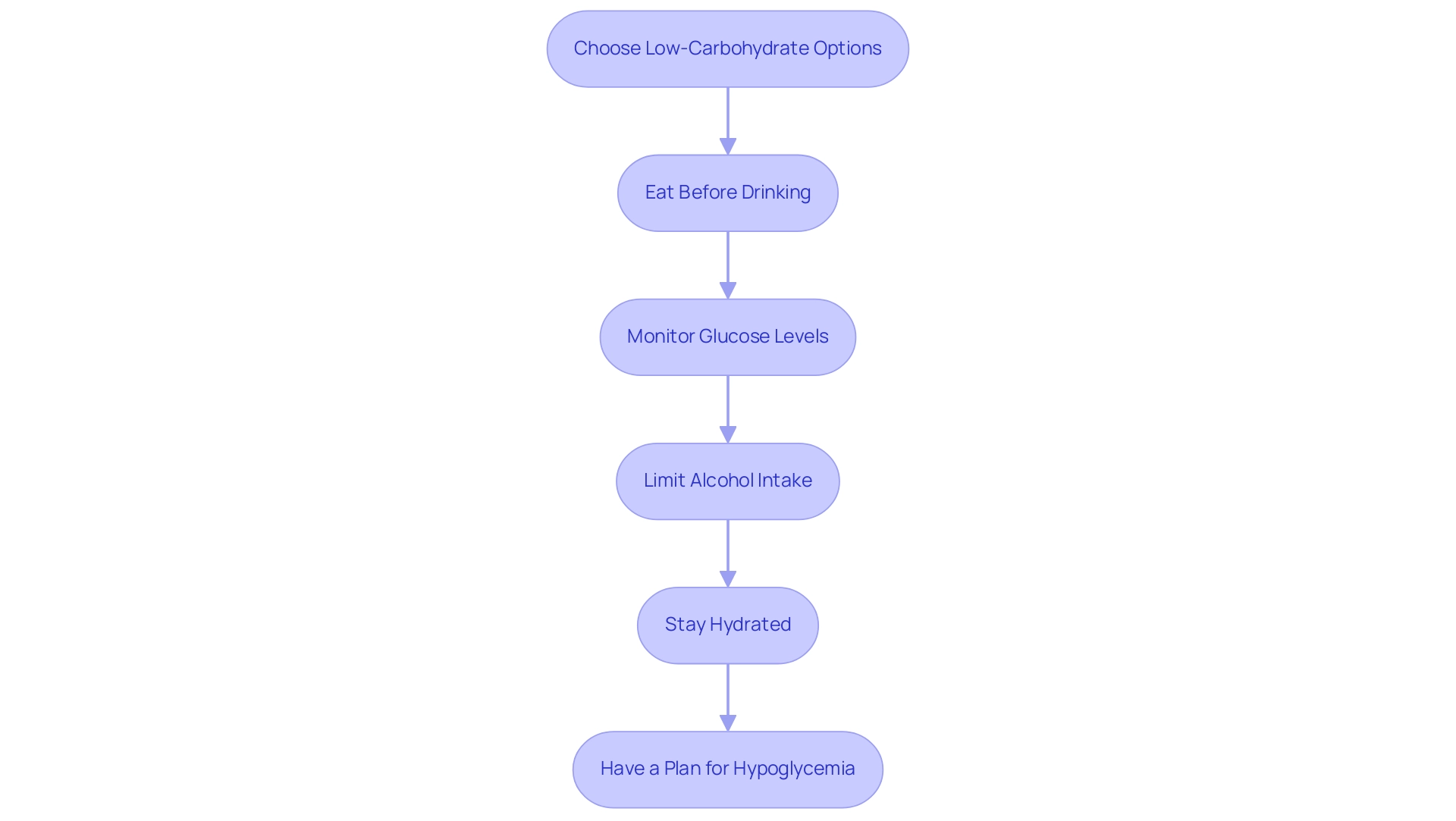
Effectively controlling alcohol and blood sugar levels is essential for individuals with diabetes when consuming alcoholic drinks. Here are several evidence-based strategies:
- Choose Low-Carbohydrate Options: Select beverages with lower carbohydrate content, such as dry wines or spirits mixed with soda water, while avoiding sweet cocktails and dessert wines.
- Eat Before Drinking: It is beneficial to consume a balanced meal or snack prior to drinking. This practice can help stabilize glucose levels and significantly lower the risk of hypoglycemia.
- Monitor Glucose Levels: Regularly checking glucose before and after consuming various types of beverages provides insight into how different kinds of drinks affect your body.
- Limit Alcohol Intake: Moderation is essential; limiting consumption to one drink for women and two for men is recommended to minimize potential health risks. Additionally, negative interactions between alcohol and blood sugar medications have been documented, increasing the risk of hypoglycemia and other complications.
- Stay Hydrated: Consuming water between alcoholic drinks can assist in preserving hydration and support consistent glucose levels.
- Have a Plan for Hypoglycemia: Always keep a source of fast-acting carbohydrates, such as glucose tablets or juice, readily available in case of unexpected drops in glucose levels.
These strategies are backed by insights from nutritionists, who highlight the significance of responsible drinking and informed choices to manage sugar levels effectively while enjoying social occasions. Moreover, a case study titled ‘Effect of Evening Beverage Consumption on Next-Morning Glucose Control in Type 1 Diabetes’ found that moderate evening beverage intake, which can affect alcohol and blood sugar levels, led to significantly lower fasting and postprandial glucose levels the next morning, with five subjects experiencing hypoglycemia, indicating a risk for those consuming beverages. This corresponds with the findings of Vonghia et al., who noted that acute alcohol intoxication can acutely influence alcohol and blood sugar levels.
Understanding Alcohol Labels and Ingredients
When selecting alcoholic drinks, a thorough review of labels is essential for effectively regulating alcohol and blood sugar levels. It is important to identify the total carbohydrates and sweeteners listed, as these components have a direct impact on glucose levels. For instance, after deducting half of the sweetener substance, a product may count as 20 grams of carbohydrate, considerably influencing glucose levels.
Components like malted barley or additional sweeteners can further boost carbohydrate levels, making it crucial to remain cautious. Comprehending the beverage by volume (ABV) is similarly crucial, as the relationship between alcohol and blood sugar can be affected differently by more potent drinks than those with lower ABV. Furthermore, one must take into account the mixers used in cocktails, which often include concealed sweeteners that can increase carbohydrate intake.
However, alongside careful beverage choices, staying hydrated with local drinks in San Marcos—such as infused water, herbal teas, or natural, no-sugar-added options—can support overall health and blood sugar regulation. By acquiring awareness of these elements, individuals overseeing type 2 health conditions can make informed choices regarding beverage intake and hydration approaches. Furthermore, the TTB Procedure 2020-1 outlines methods for testing nutrient content in alcoholic beverages, ensuring that the claims made on labels are reliable.
As Andrew Jones from the University of Liverpool notes, the effectiveness of energy labeling in alcoholic drinks is a significant consideration in obesity policy, underscoring the importance of understanding what is consumed. Future studies should also concentrate on the unforeseen effects of energy labeling and its possible contribution to tackling obesity, highlighting the importance of comprehending beverage labels and hydration for managing both alcohol and blood sugar levels. This knowledge empowers individuals to navigate their choices more effectively and maintain better control over their blood sugar levels.
Communicating with Healthcare Providers
Open dialogue regarding alcohol and blood sugar intake is essential for patients managing Type 2 blood sugar issues. At the Integrative Wellness Center, our holistic approach empowers individuals by encouraging discussions with healthcare providers that align with their unique health needs. These discussions are crucial for:
- Evaluating risks linked to beverage consumption, especially concerning alcohol and blood sugar
- Recommending safe drinking thresholds
- Making required modifications to health management plans
By addressing the root causes of anxiety, our providers help patients feel more secure in their health journey. For instance, studies show that:
- The median number of participants involved in research related to substance use was 790
- The mean number of participants was 1,667
This highlights the significant population affected by these issues. Routine assessments are crucial for swiftly responding to any variations in beverage intake, particularly regarding alcohol and blood sugar, thus promoting a more comprehensive approach to health management.
As one patient noted, ‘When they say, ‘If you drink more than 20 units a week,’ you don’t care … It doesn’t make a ha’p’orth [half-pennyworth] of difference to an alcoholic, or an alcoholic-dependent person, or an addictive personality. It doesn’t.’ This perspective underscores the challenges faced by individuals with issues related to alcohol and blood sugar dependency.
Furthermore, a study by Vadlamudi et al. in 2008, which involved 181 graduate nursing students in the USA, demonstrated that educational interventions significantly improved confidence and attitudes towards alcohol-related practices. This demonstrates the broader effect of effective patient-provider communication in managing health.
Such proactive engagement at the Integrative Wellness Center can enhance overall management of the condition and support healthier lifestyle choices, ultimately helping patients eliminate anxiety over potential complications.
Recognizing Signs of Blood Sugar Fluctuations
People handling diabetes must stay alert in identifying the indicators of glucose variations, especially following the intake of alcohol and blood sugar. Hypoglycemia can manifest as symptoms such as:
- Sweating
- Shaking
- Confusion
- Dizziness
Conversely, hyperglycemia may present with:
- Increased thirst
- Frequent urination
- Fatigue
Research indicates that hypoglycemia occurs more frequently when beverages are ingested in combination with glucose, with studies showing that hypoglycemia occurred more frequently following simultaneous ingestion of drinks plus glucose than following glucose alone. This finding underscores the importance of monitoring one’s body for symptoms following drinking episodes, particularly those related to alcohol and blood sugar.
Prompt action is essential—consuming fast-acting carbohydrates can effectively counter low glucose levels, while adjusting insulin doses may be necessary for elevated glucose concentrations.
Ongoing observation and awareness of one’s own physiological reactions can significantly enhance safety when consuming beverages. For instance, the statistic ΔTG at 180′ during OGATT was measured at 4.9 ± 11.9 mg/dL, indicating notable changes in glucose metabolism. Furthermore, we express our gratitude to Mark Cleasby, PhD, from Edanz Group for reviewing a draft of this manuscript, emphasizing the necessity for individuals with health concerns to understand how alcohol and blood sugar can affect their glucose management.
Developing a Personal Action Plan
To effectively develop a personal action plan for managing beverage consumption and its impact on alcohol and blood sugar levels, individuals must begin by thoroughly assessing their current drinking habits in relation to their diabetes management objectives. Key considerations include:
- The frequency of beverage intake
- The types of drinks consumed
- The typical food choices made during drinking occasions
Understanding insulin resistance is crucial, as traditional treatments may carry significant risks, including severe health outcomes that could even lead to death.
According to the GRADE guidelines published in the Journal of Clinical Epidemiology, it is essential to set realistic goals for managing alcohol and blood sugar consumption, as these guidelines provide a structured approach to evaluating health interventions. Incorporating specific strategies discussed in this tutorial is crucial, such as:
- Seeking professional guidance on safe drinking limits
- Exploring alternatives to traditional treatments
Maintaining a detailed log that tracks drinking patterns alongside the corresponding effects of alcohol and blood sugar responses is essential for recognizing trends and facilitating informed adjustments to their plan.
As noted by the GP, it is vital to use this assessment not as an intervention but to rule out any serious underlying conditions that could elevate GGT levels. This personal action plan should be revisited regularly, particularly following any changes in health status, to ensure it continues to align with overall health management goals. By embracing an integrative approach, as exemplified in a case study on a telephone-based stepped care intervention for alcohol-related disorders, individuals with Type 2 diabetes can implement effective management strategies that not only optimize their health outcomes but also address broader health concerns, such as hypothyroidism, through functional medicine.
Conclusion
Understanding the intricate relationship between alcohol and blood sugar levels is critical for individuals managing diabetes. The evidence presented highlights how various factors, such as the type of alcohol consumed and whether it is ingested with food, can lead to significant fluctuations in glucose levels. Caution is paramount, as both hypoglycemia and hyperglycemia present risks that can complicate diabetes management. By implementing evidence-based strategies, such as:
- Choosing low-sugar options
- Monitoring blood sugar levels
- Communicating openly with healthcare providers
individuals can navigate these challenges more effectively.
Furthermore, being informed about alcohol labels and ingredients empowers individuals to make healthier choices, thereby minimizing the impact on their blood sugar levels. Recognizing the signs of blood sugar fluctuations is equally important, as quick and appropriate responses can prevent serious health complications. Developing a personal action plan tailored to one’s unique circumstances allows for proactive management of alcohol consumption alongside diabetes care.
In conclusion, by understanding the interplay between alcohol and blood sugar, individuals can take informed steps that support their health and well-being. Prioritizing education, monitoring, and communication with healthcare professionals is essential for effective diabetes management and can lead to a more balanced approach to social situations involving alcohol.
Frequently Asked Questions
How does beverage consumption affect blood sugar levels?
Beverage consumption can significantly influence blood sugar levels, leading to increases or decreases based on factors such as the type and quantity of beverage consumed and whether it is ingested with food.
What happens to glucose production when alcohol is consumed?
When alcohol is present, the liver prioritizes the metabolism of ethanol over glucose production, which can impair glucose availability in the bloodstream, often resulting in hypoglycemia, especially if consumed on an empty stomach.
What is the significance of growth hormone secretion in relation to blood sugar?
A systematic review found that growth hormone secretion is significantly diminished between midnight and 4:00 a.m., indicating potential disruptions in metabolic processes during this time, which could affect blood sugar regulation.
How can alcoholic drinks affect blood sugar levels differently?
Alcoholic drinks high in sugar can lead to increases in blood sugar levels, while those with lower carbohydrate content may have a lesser effect. This variability is crucial for individuals managing type 2 diabetes.
What is the ‘sick-quitter effect’?
The ‘sick-quitter effect’ refers to the dangers associated with avoiding beverages for health reasons, as it may raise the risk of developing blood sugar issues.
What practices are recommended for managing blood sugar levels when consuming alcohol?
Recommended practices include choosing low-carbohydrate options, eating before drinking, monitoring glucose levels, limiting alcohol intake, staying hydrated, and having a plan for hypoglycemia.
Why is it important to eat before drinking alcohol?
Eating a balanced meal or snack before drinking can help stabilize glucose levels and significantly lower the risk of hypoglycemia.
How can individuals monitor their glucose levels effectively?
Regularly checking glucose levels before and after consuming various beverages provides insights into how different drinks affect the body.
What are the recommended limits for alcohol consumption?
It is recommended to limit alcohol intake to one drink for women and two for men to minimize potential health risks.
What should individuals do in case of hypoglycemia?
It’s important to keep a source of fast-acting carbohydrates, such as glucose tablets or juice, readily available in case of unexpected drops in glucose levels.
What does research indicate about evening beverage consumption and glucose control?
A case study found that moderate evening beverage intake can lead to significantly lower fasting and postprandial glucose levels the next morning, indicating a risk for hypoglycemia in those consuming beverages.