Introduction
The A1C test serves as a critical barometer for individuals managing diabetes, providing insight into average blood sugar levels over a span of two to three months. Its significance extends beyond mere diagnosis; it is an essential tool for ongoing management and risk assessment of diabetes-related complications.
With the increasing prevalence of diabetes, particularly among specific demographics, understanding A1C results and their implications has never been more vital.
This article delves into the functionality of the A1C test, the interpretation of its results, effective management strategies, and common misconceptions that can hinder patient care. By equipping readers with comprehensive knowledge about the A1C test, the aim is to empower individuals to take control of their health, make informed decisions, and ultimately improve their quality of life.
Understanding the A1C Test: Importance and Functionality
The A1C test, also referred to as the glycated hemoglobin test, is a vital tool for monitoring A1C for diabetics, as it measures the average blood sugar levels over the past two to three months. It plays an essential part not only in diagnosing type 2 blood sugar issues but also in the continuous oversight of the condition. This test evaluates the percentage of hemoglobin molecules in the blood that are bound to glucose; a higher A1C for diabetics signifies poorer blood sugar control and correlates with an increased risk of diabetes-related complications.
According to a statistic from recent years, the awareness of prediabetes among Hispanic adults rose to 20.9%, underscoring the importance of monitoring A1C levels within this demographic. Care plans for older individuals with blood sugar issues and additional health conditions should include agents that lower cardiorenal risk, regardless of glycemia, to improve overall strategies. Comprehending the implications of this test enables individuals to gauge their long-term glucose levels effectively, guiding necessary lifestyle adjustments and medication management.
As emphasized in the International Expert Committee report on the role of the A1C assay in diagnosing the condition, monitoring A1C for diabetics is crucial for enhancing outcomes and customizing treatment approaches. Additionally, a recent case study evaluated the feasibility of measuring HbA1c from dried blood spots collected on filter paper compared to venous blood samples, showing high correlation with routine measurements and favorability among participants for its convenience. A transformative success tale from the Integrative Wellness Center demonstrates the power of a holistic approach: an individual who had battled with blood sugar issues for ten years lost 55 pounds and significantly improved their A1C for diabetics from 9.1 to 5.7 through personalized care and attention.
This underscores the potential of addressing root causes and enabling individuals to take charge of their health, which can also assist in reducing the anxiety that frequently accompanies managing this condition. Lastly, it’s important to note that Emily Eyth and Roopa Naik declared no relevant financial relationships with ineligible companies, ensuring transparency in the discussion of the A1C test.
Interpreting A1C Results: What Do the Numbers Mean?
The A1C for diabetics results are expressed as a percentage, serving as an important indicator of blood sugar control over the previous three months. The subsequent ranges classify individuals according to their blood sugar levels:
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher
For adults identified with this condition, the American Diabetes Association advises keeping an A1C level below 7%. This target is crucial, as higher percentages may necessitate modifications in diet, exercise, or medication regimens. Grasping the implications of these A1C figures is crucial for individuals, as it enables them to make informed choices concerning their treatment approaches and assists in reducing the risk of possible complications, ultimately alleviating concerns about developing severe and debilitating health issues.
At the Integrative Wellness Center, we emphasize a holistic strategy for reversing the condition by tackling root causes and offering thorough insights into care. Our treatment options consist of personalized nutrition plans, exercise regimens, and stress reduction techniques. Transformative patient success stories have shown that effective A1C for diabetics oversight can lead to better health results and lessen anxiety regarding complications related to blood sugar issues.
Recent statistics indicate that poorly managed A1C levels can have significant financial implications, with excess medical costs related to the condition increasing from $10,179 in 2012 to $12,022 in 2022. Moreover, Qiuping Gu from the National Center for Health Statistics emphasizes the ongoing prevalence of diagnosed and undiagnosed conditions among adults, underscoring the importance of proactive management. A case study titled ‘Hemoglobin A1c and Permissive Hyperglycemia in ICU Patients’ further highlights the critical role of managing A1C levels, particularly the A1C for diabetics, in intensive care settings, demonstrating its profound impact on patient outcomes.
Strategies for Managing A1C Levels: Lifestyle and Medication
To effectively manage A1C for diabetics, several strategies should be prioritized:
-
Dietary Modifications: A balanced diet is crucial. Emphasize whole grains, lean proteins, fruits, and vegetables while minimizing sugar and refined carbohydrates.
According to recent findings, making these dietary changes can significantly influence A1C levels, as indicated by a change in the healthy food score among men (β = 0.10, P = 0.03). Notably, a study by Knowler et al. (2002) found that lifestyle intervention or metformin can reduce the incidence of type 2 conditions, underscoring the importance of dietary adjustments.
Nutritionist Madelyn Wheeler notes that dietary adjustments are fundamental to improving A1C for diabetics and overall health.
-
Regular Physical Activity: Engaging in a minimum of 150 minutes of moderate-intensity aerobic exercise weekly, complemented by strength training at least twice a week, has shown to lower A1C levels effectively.
Recent studies affirm that consistent exercise contributes positively to glycemic control, which was also highlighted at the American Diabetes Association 82nd Scientific Sessions on June 5, 2022.
-
Medication Adherence: It is vital to adhere to prescribed medication regimens.
Regular consultations with healthcare providers can ensure that any necessary adjustments to medications are made in a timely manner for optimal control of A1C for diabetics.
-
Monitoring Blood Sugar Levels: Regularly checking blood glucose levels aids in identifying patterns that can inform dietary and activity adjustments.
The analysis of data collected at baseline, 3 months, and 6 months, including demographic information and health measurements, has highlighted the importance of continuous monitoring in achieving better A1C for diabetics outcomes. Additionally, we start by re-examining the source of your diabetes. From there, we can address health at the root level using a holistic regimen, which may include dietary changes, stress reduction techniques, and lifestyle adjustments that collectively help alleviate anxiety about potential complications.
This case study context illustrates the impact of dietary interventions on A1C levels. By implementing these strategies, individuals can take significant steps toward effective A1C for diabetics management and improved overall health.
How Often Should You Test Your A1C? Guidelines and Recommendations
According to the American Diabetes Association, individuals diagnosed with diabetes should undergo A1C testing at least twice annually to maintain their A1C for diabetics when their blood glucose levels remain stable and within the target range. For individuals experiencing changes in therapy or those who are not achieving their glucose targets, it is recommended that testing occurs quarterly. This consistent monitoring is essential, as it enables timely interventions and adjustments to plans, thereby promoting optimal health outcomes.
Significantly, a study by Balintescu A. emphasizes that ‘Hemoglobin A1c and permissive hyperglycemia in individuals in the intensive care unit with metabolic disorders’ can greatly influence outcomes for individuals. Furthermore, while A1C is not recommended for screening CFRD, it is widely used in practice. Given the rising prevalence of complications related to diabetes—estimated to increase by 10% per decade—regular A1C for diabetics testing is essential for effective management of the condition.
By re-evaluating the origin of your condition and embracing a comprehensive strategy that tackles underlying issues, individuals can empower themselves through knowledge and reduce anxiety related to possible complications. The revised tables (9.3 and 9.4) show adjustments in cost for several agents, which is important for patients to consider when managing their condition.
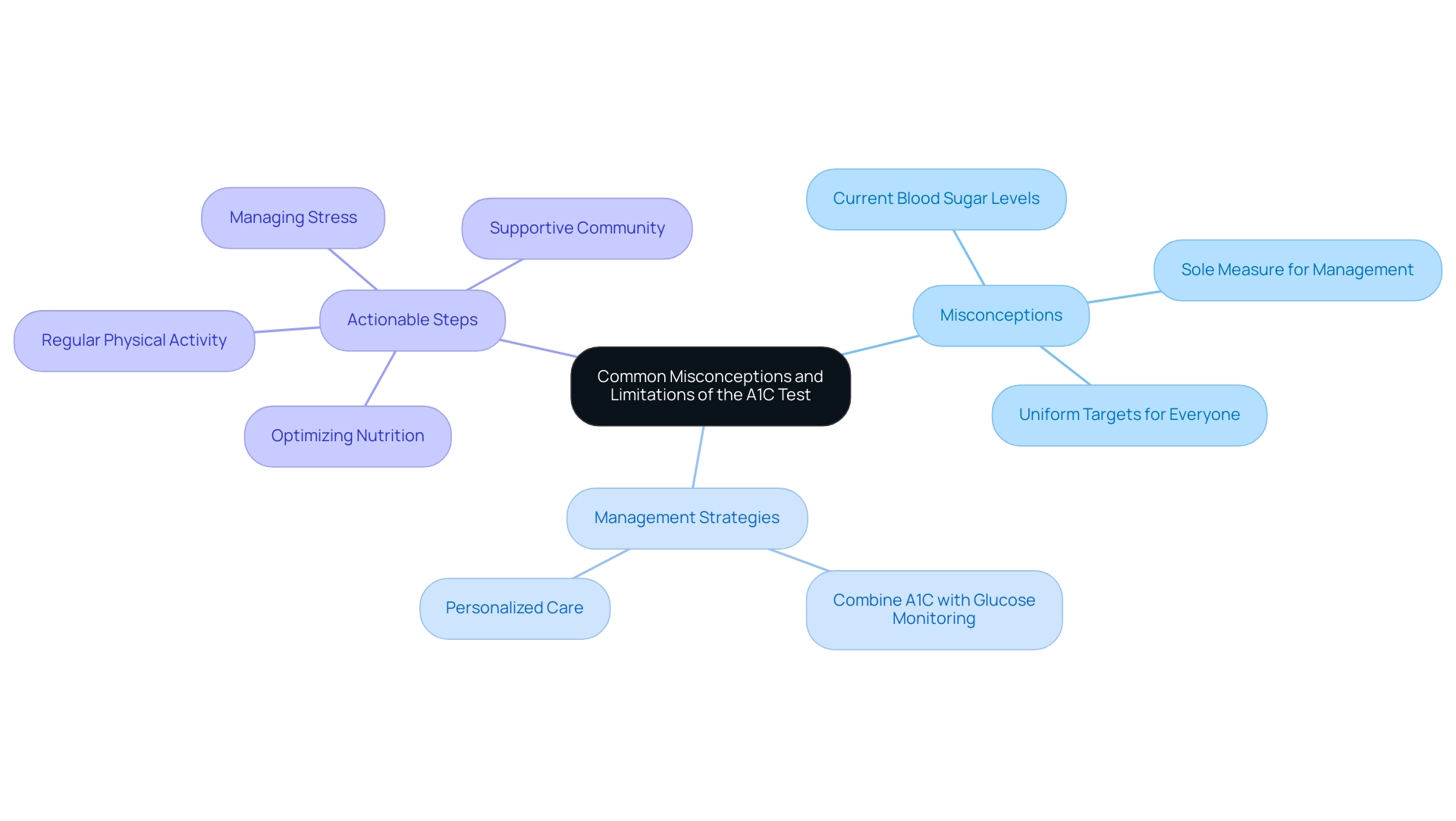
Common Misconceptions and Limitations of the A1C Test
Misunderstandings related to the A1C for diabetics test can significantly affect blood sugar control. One prevalent misconception is that the A1C test measures current blood sugar levels. In reality, this test reflects an average A1C for diabetics over the past two to three months, thus not capturing daily fluctuations.
Another common belief is that the A1C test is the sole measure necessary for managing blood sugar; however, for effective management, it is vital for diabetics to combine A1C results with regular glucose monitoring to obtain a comprehensive view of one’s condition control. Additionally, many individuals assume that uniform A1C targets apply to everyone. In reality, A1C for diabetics should be customized to each individual’s distinctive health situation, emphasizing the significance of personalized care and education in diabetes treatment.
Patients are encouraged to discuss their specific A1C for diabetics targets with healthcare providers, as addressing these misconceptions is crucial for effective oversight. A recent evaluation by David B. Sacks observed that comprehending the factors affecting glucose and A1C for diabetics testing can enhance individual confidence in their care strategy. Moreover, a correlation statistic reveals that there is a significant negative association between total knowledge scores and age (r = -0.34, p < 0.001), suggesting that younger individuals tend to possess better understanding related to health care.
This highlights the importance of customized education programs for individuals with blood sugar issues, as a related case study showed that individuals frequently face challenges in grasping management due to deep-seated misconceptions. By creating well-structured educational programs, healthcare providers can tackle these knowledge gaps, enabling individuals with Type 2 to adopt a proactive stance towards their health and lessen anxiety about possible complications. To further assist individuals, it is essential to incorporate actionable strategies, such as the four lesser-known power-plays for enhancing health and reversing the condition, which include:
- Optimizing nutrition
- Engaging in regular physical activity
- Managing stress effectively
- Fostering a supportive community
Recognizing the emotional aspects of diabetes management, such as anxiety and frustration, can also empower patients to navigate their journey with greater confidence and resilience.
Conclusion
Understanding the A1C test is fundamental for effectively managing diabetes and mitigating the risks associated with the condition. This test not only aids in diagnosing diabetes but also plays a crucial role in ongoing management by providing a clear picture of average blood sugar levels over the past few months. By interpreting A1C results accurately, individuals can make informed decisions about their health, tailoring lifestyle changes and medication adherence to meet their specific needs.
Implementing strategies such as:
- Dietary modifications
- Regular physical activity
- Consistent monitoring of blood sugar levels
can significantly impact A1C management. These approaches empower individuals to take control of their diabetes, leading to improved health outcomes and reduced anxiety regarding potential complications. Moreover, addressing common misconceptions about the A1C test and its role in diabetes management is essential for fostering a comprehensive understanding of personal health.
In conclusion, prioritizing A1C testing and management is vital in the broader context of diabetes care. By equipping patients with knowledge and effective strategies, healthcare providers can help them navigate their health journeys with confidence. Ultimately, proactive management of A1C levels not only enhances individual well-being but also contributes to a healthier community overall.
Frequently Asked Questions
What is the A1C test and why is it important for diabetics?
The A1C test, also known as the glycated hemoglobin test, measures the average blood sugar levels over the past two to three months. It is crucial for diagnosing type 2 diabetes and for ongoing monitoring of the condition, as higher A1C levels indicate poorer blood sugar control and an increased risk of diabetes-related complications.
How does the A1C test help in managing diabetes?
The A1C test helps individuals understand their long-term glucose levels, guiding necessary lifestyle adjustments and medication management. It is essential for customizing treatment approaches and enhancing health outcomes for diabetics.
What are the A1C percentage ranges for blood sugar levels?
The A1C results are classified as follows: Normal: Below 5.7%, Prediabetes: 5.7% to 6.4%, Diabetes: 6.5% or higher.
What is the recommended A1C target for adults with diabetes?
The American Diabetes Association recommends that adults with diabetes maintain an A1C level below 7% to reduce the risk of complications.
What are some treatment strategies for managing A1C levels?
Effective management of A1C levels includes personalized nutrition plans, exercise regimens, and stress reduction techniques. A holistic approach that addresses root causes can lead to better health outcomes.
Are there any recent statistics regarding the financial implications of poorly managed A1C levels?
Yes, recent statistics show that excess medical costs related to diabetes increased from $10,179 in 2012 to $12,022 in 2022, highlighting the financial burden of poorly managed A1C levels.
What was a notable case study related to the A1C test?
A case study demonstrated the feasibility of measuring HbA1c from dried blood spots, showing high correlation with routine measurements and convenience for participants. Additionally, a success story from the Integrative Wellness Center illustrated how personalized care led to significant weight loss and improved A1C levels.
What is the significance of awareness of prediabetes among specific demographics?
Awareness of prediabetes among Hispanic adults has risen to 20.9%, emphasizing the importance of monitoring A1C levels in this demographic to prevent diabetes and its complications.