Overview
This article shines a light on the American Diabetes Association (ADA) guidelines for diagnosing diabetes, recognizing the emotional and physical challenges faced by many. It’s important to understand that accurate testing methods and personalized management strategies can make a significant difference in one’s journey toward better health.
The article details the diagnostic criteria, such as the A1C test and fasting plasma glucose levels, emphasizing how these tests are vital in understanding individual health needs. Many patients find that tailored care plans, along with education, are essential to improving their health outcomes.
Ultimately, the goal is to foster a supportive environment where individuals feel empowered to take charge of their health. By embracing these guidelines, you can embark on a path that not only addresses your diabetes but also nurtures your overall well-being.
Introduction
In a world where diabetes affects so many lives, it’s crucial to understand its various classifications and effective management strategies. This chronic metabolic disorder, marked by elevated blood glucose levels, touches millions globally. Each type—Type 1, Type 2, and gestational diabetes—presents its own unique challenges, and many patients find themselves navigating a complex landscape.
It’s important to recognize that tailored management approaches can make a significant difference. Recent research emphasizes the vital role of lifestyle changes, early detection, and multidisciplinary care in improving health outcomes. By exploring the diagnostic criteria set forth by the American Diabetes Association, healthcare providers can empower patients to take control of their health.
Together, we can navigate the complexities of diabetes with confidence and compassion.
Define Diabetes: Classifications and Terminology
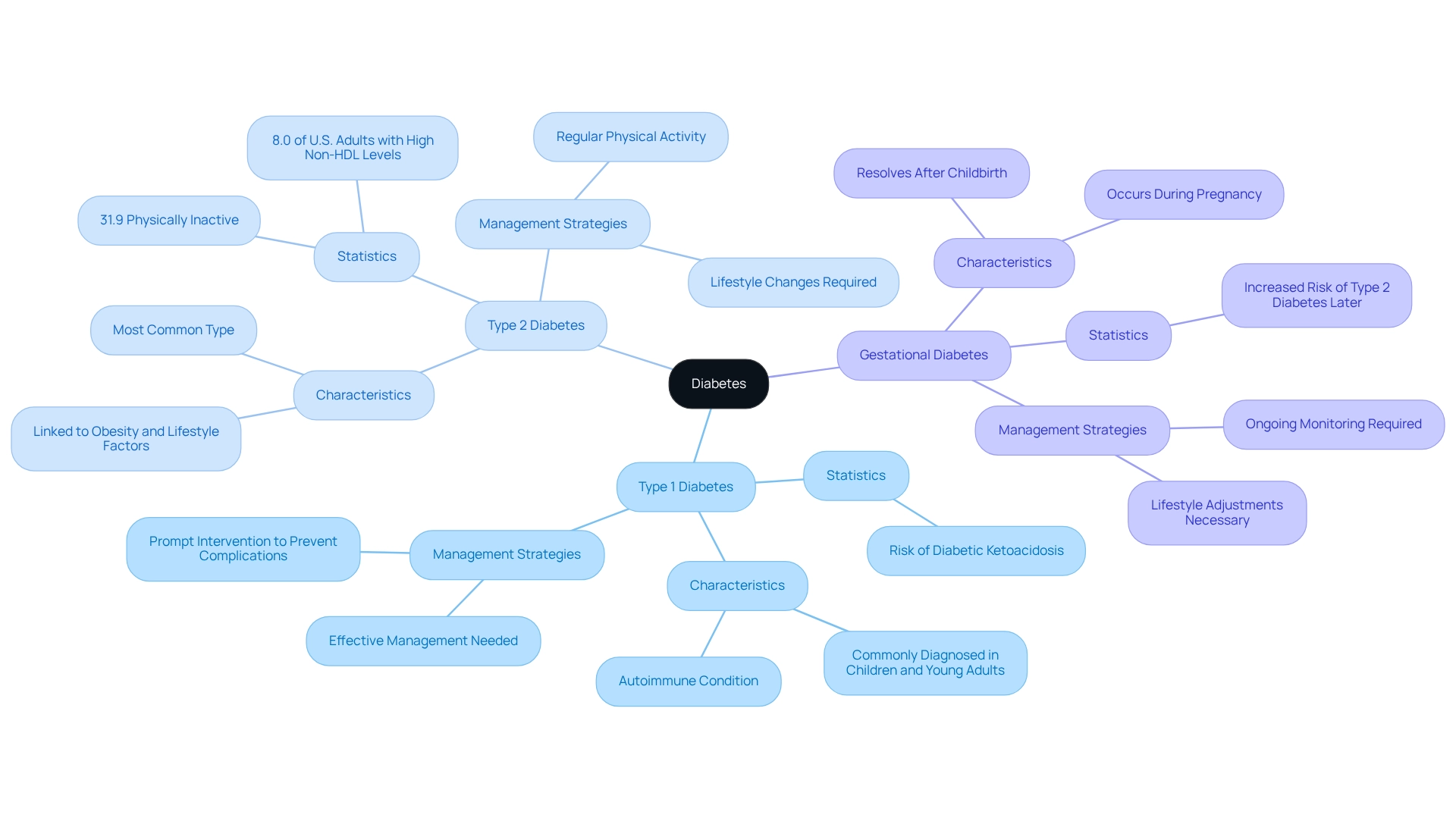
Diabetes is a long-term metabolic condition that can be challenging, marked by increased blood glucose levels due to issues in insulin secretion, insulin action, or both. Understanding the different types of diabetes can help us navigate this journey together.
-
Type 1 Diabetes: This is an autoimmune condition where the pancreas produces little to no insulin, often diagnosed in children and young adults. Recent research emphasizes the critical need for effective management strategies. If left untreated, complications can arise, including a serious condition known as diabetic ketoacidosis, which can lead to sudden death. It’s essential to seek prompt intervention to prevent such outcomes.
-
Type 2 Diabetes: This is the most common type, frequently linked to obesity and lifestyle factors. In this case, the body either becomes resistant to insulin or fails to produce enough. Current statistics reveal that about 8.0% of U.S. adults with diagnosed conditions have a non-HDL cholesterol level of 190 mg/dL or higher. This highlights the importance of thorough oversight, including lifestyle changes like maintaining a healthy weight and engaging in regular physical activity. In San Marcos, CA, individuals can embrace outdoor activities like hiking and walking, which not only enhance physical fitness but also improve insulin sensitivity and blood sugar control.
-
Gestational Diabetes: This form occurs during pregnancy and typically resolves after childbirth. However, it significantly increases the risk of developing type 2 diabetes later in life, necessitating ongoing monitoring and lifestyle adjustments according to the ADA guidelines diagnosis of diabetes. Comprehending these classifications is vital for healthcare providers, as it enables them to tailor their diagnostic and treatment strategies to the specific type of illness an individual faces. For instance, a recent case study revealed that 31.9% of adults with high blood sugar levels were physically inactive, defined as engaging in less than 10 minutes of moderate or vigorous activity weekly. This inactivity can lead to poor health outcomes, underscoring the need for increased physical activity initiatives among this population. By addressing these factors, healthcare providers can better support patients in managing their conditions effectively. This aligns with the holistic approach emphasized by Dr. Shumard’s center, which focuses on nutrition, community support, and stress control to empower meaningful lifestyle changes. Remember, you are not alone in this journey, and together we can find a path toward better health.
Explore Diagnostic Criteria: ADA Guidelines for Testing
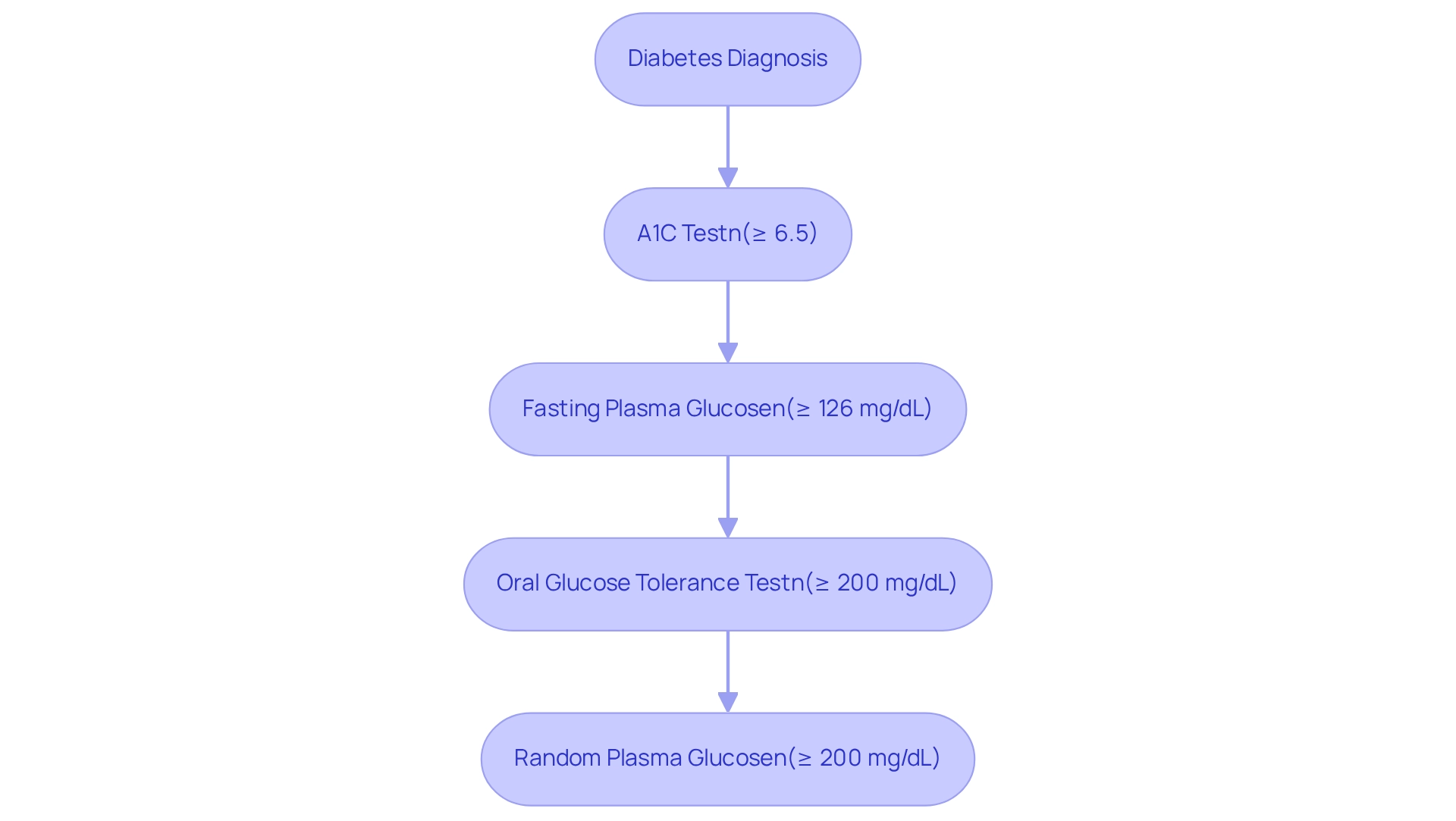
The American Diabetes Association (ADA) establishes ADA guidelines for the diagnosis of diabetes, which are essential for healthcare providers to ensure accurate identification and effective management. These criteria include:
- A1C Test: An A1C measurement of 6.5% or above indicates a high blood sugar condition, reflecting average blood glucose readings over the previous 2-3 months. It’s concerning that a significant percentage of U.S. adults with diabetes have non-HDL readings exceeding 190 mg/dL, suggesting an increased cardiovascular risk linked to the condition.
- Fasting Plasma Glucose (FPG): A fasting plasma glucose level of 126 mg/dL (7.0 mmol/L) or higher points to the presence of diabetes.
- Oral Glucose Tolerance Test (OGTT): A 2-hour plasma glucose measurement of 200 mg/dL (11.1 mmol/L) or greater during a 75g OGTT indicates a diabetic condition.
- Random Plasma Glucose: A random plasma glucose level of 200 mg/dL (11.1 mmol/L) or higher in a patient showing classic symptoms of hyperglycemia or hyperglycemic crisis confirms the diagnosis.
These criteria are essential for accurate diagnosis and are in accordance with the ADA guidelines for the diagnosis of diabetes for 2025, which emphasize the importance of early detection and intervention. Many patients find that screening for undiagnosed prediabetes or elevated blood sugar levels, especially those planning pregnancy or with risk factors, can significantly improve management outcomes for both mother and child. Dr. Jason Shumard highlights, “If you had gestational issues, you should be tested for blood sugar conditions no later than 12 weeks after your baby is born,” underscoring the critical nature of timely screening.
It’s important to recognize that understanding the risks associated with traditional treatments for diabetes is vital. Insulin resistance can sometimes worsen with the insulin injections and medications often prescribed. This emphasizes the need for a comprehensive approach to blood sugar control, particularly for individuals with type 2 diabetes, where the body may struggle to use the insulin it produces effectively. Expert opinions from diabetes associations reinforce the importance of A1C testing as a reliable diagnostic tool, with the latest recommendations advocating for its use in routine screenings. By following these guidelines, healthcare providers can implement suitable strategies, ultimately leading to improved health outcomes for individuals.
In this journey, remember that you are not alone. Seeking support and understanding can make a significant difference in managing diabetes effectively.
Implement Management Strategies: Applying ADA Guidelines in Patient Care
Implementing the ADA guidelines diagnosis of diabetes in healthcare requires a multifaceted strategy that emphasizes personalized care and education.
-
Personalized Care Plans: It’s vital to customize strategies for each individual’s unique lifestyle, preferences, and health conditions. Personalization is essential, as studies show that tailored care plans greatly enhance outcomes. For instance, there’s been a notable rise in adherence to treatment protocols. However, it’s concerning that the proportion of individuals with type 2 diabetes reaching their blood pressure goals has dropped by 3.6 percentage points, underscoring the need for effective control strategies.
-
Education and Support: Providing individuals with crucial information about managing their condition is key. This includes emphasizing nutrition, physical activity, and self-assessment of blood glucose values. Effective diabetes education, according to the ADA guidelines for the diagnosis of diabetes, has been shown to enhance individual engagement, leading to better health outcomes. As Tiffany Danczak wisely stated, “Don’t let yourself fall, you gotta pick yourself right up and strive to do better and be better!”
-
Regular Monitoring and Goal Setting: Establishing a routine for follow-ups to evaluate blood glucose measurements, A1C, and other health indicators is essential. Many patients find that incorporating SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost their focus and motivation. For example, individuals might set a goal to lower their A1C levels or gradually increase their physical activity. Utilizing tracking methods, such as fitness apps and journals, can enhance this process. Regularly reviewing progress fosters accountability and allows for adapting goals in response to changing health conditions. Research indicates that persistence in goal-setting can positively impact performance, demonstrating the effectiveness of structured goal-setting.
-
Multidisciplinary Approach: Encouraging teamwork among healthcare experts, including dietitians and educators, is crucial for delivering comprehensive care. This team-oriented strategy improves the support system available to patients, promoting a holistic approach to health oversight.
-
Behavioral Interventions: Implementing strategies that encourage behavior modification, such as regular exercise and balanced nutrition, is essential. These interventions foster healthy habits that aid in long-term success in controlling blood sugar.
The economic burden associated with diabetes in the U.S. highlights the financial strain many individuals experience, reinforcing the importance of effective strategies for managing this condition. By integrating these approaches, including structured goal-setting and consistent progress tracking, healthcare providers can significantly enhance patient engagement and improve diabetes management outcomes. Ultimately, this leads to a better quality of life for individuals living with diabetes.
Conclusion
Understanding diabetes and its classifications is essential for effective management and improved health outcomes. It’s important to recognize that diabetes comes in distinct forms—Type 1, Type 2, and gestational diabetes—each presenting unique challenges that require tailored approaches. Early detection and adherence to the American Diabetes Association’s diagnostic criteria are crucial, as timely intervention can significantly influence patient well-being.
Many patients find that implementing personalized management strategies empowers them. By focusing on individualized care plans, education, regular monitoring, and multidisciplinary collaboration, healthcare providers can enhance the effectiveness of diabetes management. Integrating lifestyle changes, such as increased physical activity and balanced nutrition, further supports patients in taking control of their health.
Ultimately, navigating the complexities of diabetes is a shared journey that calls for compassion, understanding, and a commitment to holistic care. By prioritizing tailored strategies and fostering patient engagement, we can achieve a positive impact on health outcomes, paving the way for a healthier future for those affected by this chronic condition. Remember, you are not alone on this journey; together, we can create a supportive environment that encourages healthy living.
Frequently Asked Questions
What is diabetes?
Diabetes is a long-term metabolic condition characterized by increased blood glucose levels due to problems with insulin secretion, insulin action, or both.
What are the main types of diabetes?
The main types of diabetes are Type 1 Diabetes, Type 2 Diabetes, and Gestational Diabetes.
What is Type 1 Diabetes?
Type 1 Diabetes is an autoimmune condition where the pancreas produces little to no insulin, often diagnosed in children and young adults. It requires effective management to prevent serious complications, such as diabetic ketoacidosis.
What is Type 2 Diabetes?
Type 2 Diabetes is the most common type, often associated with obesity and lifestyle factors. In this condition, the body either becomes resistant to insulin or does not produce enough insulin.
How prevalent is Type 2 Diabetes among U.S. adults?
Approximately 8.0% of U.S. adults with diagnosed conditions have a non-HDL cholesterol level of 190 mg/dL or higher, indicating the importance of monitoring and lifestyle changes.
What is Gestational Diabetes?
Gestational Diabetes occurs during pregnancy and usually resolves after childbirth, but it increases the risk of developing Type 2 Diabetes later in life, necessitating ongoing monitoring and lifestyle adjustments.
Why is it important for healthcare providers to understand the different types of diabetes?
Understanding the different types of diabetes allows healthcare providers to tailor their diagnostic and treatment strategies to the specific type of illness an individual faces.
What lifestyle changes can help manage Type 2 Diabetes?
Maintaining a healthy weight and engaging in regular physical activity, such as hiking and walking, can improve insulin sensitivity and blood sugar control.
What is the significance of physical activity for those with high blood sugar levels?
A case study indicated that 31.9% of adults with high blood sugar levels were physically inactive, which can lead to poor health outcomes. Increasing physical activity is crucial for better management of diabetes.
How does Dr. Shumard’s center approach diabetes management?
Dr. Shumard’s center emphasizes a holistic approach that includes nutrition, community support, and stress control to empower patients to make meaningful lifestyle changes.