Introduction
The management of diabetes has become a pressing concern for millions, with the prevalence of the condition rising steadily across various demographics. As patients navigate the complexities of diabetes care, understanding the spectrum of available medications—both oral and injectable—plays a crucial role in effective treatment.
This article delves into the diverse classes of A1C-lowering medications, their mechanisms of action, potential side effects, and the essential lifestyle modifications that can enhance overall health outcomes. Furthermore, it highlights the vital role of healthcare providers in supporting patients through personalized care and education.
With advancements in medication and a growing emphasis on holistic health strategies, patients are better equipped to manage their condition and improve their quality of life.
Overview of Diabetes Medications: Oral and Injectable Options
Diabetes treatments, such as a1c medication, are primarily divided into two categories: oral and injectable options. Oral treatments, including a1c medication such as Metformin, Sulfonylureas, and DPP-4 inhibitors, serve various functions essential for effective management of blood sugar levels.
- Metformin enhances insulin sensitivity.
- Sulfonylureas stimulate insulin release from the pancreas.
- DPP-4 inhibitors work to delay carbohydrate absorption, thereby aiding in glycemic control.
In contrast, injectable treatments, which may include a1c medication such as GLP-1 receptor agonists and insulin therapies, are necessary for individuals with more advanced conditions or those who do not achieve adequate control with oral medications alone. Understanding these distinctions is crucial for patients to effectively navigate their treatment options, including a1c medication. Additionally, addressing the anxiety that accompanies the worry surrounding potential complications of this condition is vital.
Emphasizing a holistic approach, we begin by re-evaluating the origin of your condition, allowing us to address health at the root level through integrative methodologies. With approximately 97.6 million adults in the U.S. living with prediabetes, the need for clear understanding and early intervention strategies is paramount. This is particularly evident among older adults, where 27.2 million individuals aged 65 years or older are affected.
According to a report, the high prevalence of prediabetes underscores the importance of preventive measures and early intervention strategies. Furthermore, crude prevalence statistics reveal significant disparities, with:
- American Indian or Alaska Native adults at 16.0%
- Black non-Hispanic adults at 12.5%
- Hispanic adults at 10.3%
The public’s attitudes remain largely unchanged, with six in ten adults believing that Medicare should cover the cost of GLP-1 drugs for weight loss when prescribed for individuals who are overweight.
By thoroughly grasping these treatment categories and adopting a holistic routine, patients can participate in informed conversations with their healthcare providers, ensuring a customized approach to their condition.
Key Classes of A1C Medications and Their Mechanisms
In managing Type 2 conditions, understanding the main categories of A1C medication is crucial, but it’s also vital to embrace a comprehensive approach that tackles the underlying causes of the illness and reduces the worry that frequently comes with concerns about possible complications. The major classes of A1C medication utilized in diabetes management include:
-
Biguanides (e.g., Metformin): This class primarily reduces hepatic glucose production while enhancing insulin sensitivity in peripheral tissues.
Notably, studies indicate that Metformin can lead to significant A1C reductions in individuals who have not previously received treatment, with average decreases modeled at approximately 1.5% after 26 weeks of treatment.
-
DPP-4 Inhibitors (e.g., Sitagliptin): These agents increase levels of incretin hormones, facilitating lower blood glucose levels by stimulating insulin secretion and inhibiting glucagon release post-meal.
Recent findings suggest that DPP-4 inhibitors are effective A1C medication, making them a popular choice for many patients.
-
SGLT2 Inhibitors (e.g., Canagliflozin): By preventing glucose reabsorption in the kidneys, SGLT2 inhibitors promote increased glucose excretion through urine, thus contributing to lower blood sugar levels.
This mechanism not only aids in glycemic control but also offers cardiovascular benefits, as highlighted in current research.
-
GLP-1 Receptor Agonists (e.g., Liraglutide): Similar to DPP-4 inhibitors, these agents mimic incretin hormones, stimulating insulin release in response to meals and slowing gastric emptying.
This dual action is particularly effective at controlling postprandial blood sugar levels.
-
Insulin: For individuals experiencing more severe insulin resistance or deficiency, insulin therapy is critical.
It plays a vital role in regulating blood sugar levels by facilitating glucose uptake into cells.
-
Meglitinides: These drugs stimulate insulin secretion by binding to a different site on the SUR1 receptor in beta cells, leading to effects similar to sulfonylureas but with a rapid onset and short duration, making them suitable for controlling postprandial glucose levels effectively.
-
Bromocriptine-QR: It is important to note that Bromocriptine-QR is contraindicated in individuals at high risk for hypotension and those with severe psychotic disorders, and it should not be used with strong CYP3A4 inhibitors.
While A1C medication is essential in controlling blood sugar levels, a holistic approach that highlights lifestyle adjustments—such as dietary changes, consistent exercise, and stress reduction methods—can further empower patients.
Understanding the mechanisms of these drugs, their role in a comprehensive diabetes management plan, and the potential dangers of traditional treatments is crucial for achieving optimal health outcomes.
Potential Side Effects of A1C Medications
A1C lowering treatments, such as A1C medication, play a crucial role in managing blood glucose levels; however, they are not without side effects. Among the most common are gastrointestinal disturbances, notably with Metformin, which can lead to symptoms such as nausea and diarrhea. Statistics reveal that gastrointestinal issues with Metformin affect a significant portion of users, often necessitating adjustments in dosage or medication type.
In fact, gastrointestinal issues can contribute to emergency situations, as evidenced by the 202,000 emergency department visits in 2020 for hypoglycemia, underscoring the seriousness of improper insulin dosage.
- Dipeptidyl peptidase-4 (DPP-4) inhibitors have been reported to cause joint pain and, in rare instances, pancreatitis.
- Sodium-glucose cotransporter-2 (SGLT2) inhibitors may result in urinary tract infections or dehydration, while glucagon-like peptide-1 (GLP-1) receptor agonists can cause nausea and an increased heart rate.
- A notable case study on Sotagliflozin demonstrated significant A1C reductions and weight loss, showcasing its effectiveness as an A1C medication even in individuals with reduced renal function.
Although insulin therapy is essential for many individuals, improper dosage can lead to hypoglycemia, a serious concern that emphasizes the importance of careful management. The American Diabetes Association (ADA) recommends that patients should actively communicate any side effects to their healthcare providers to facilitate necessary adjustments in their treatment plans. According to the ADA, new types of treatments are recommended as first-line options for adults with type 2 conditions who also have issues such as atherosclerotic cardiovascular disease, heart failure, or kidney disease.
This cooperative method is crucial to enhance control of blood sugar levels while reducing negative effects.
Lifestyle Considerations When Taking A1C Medications
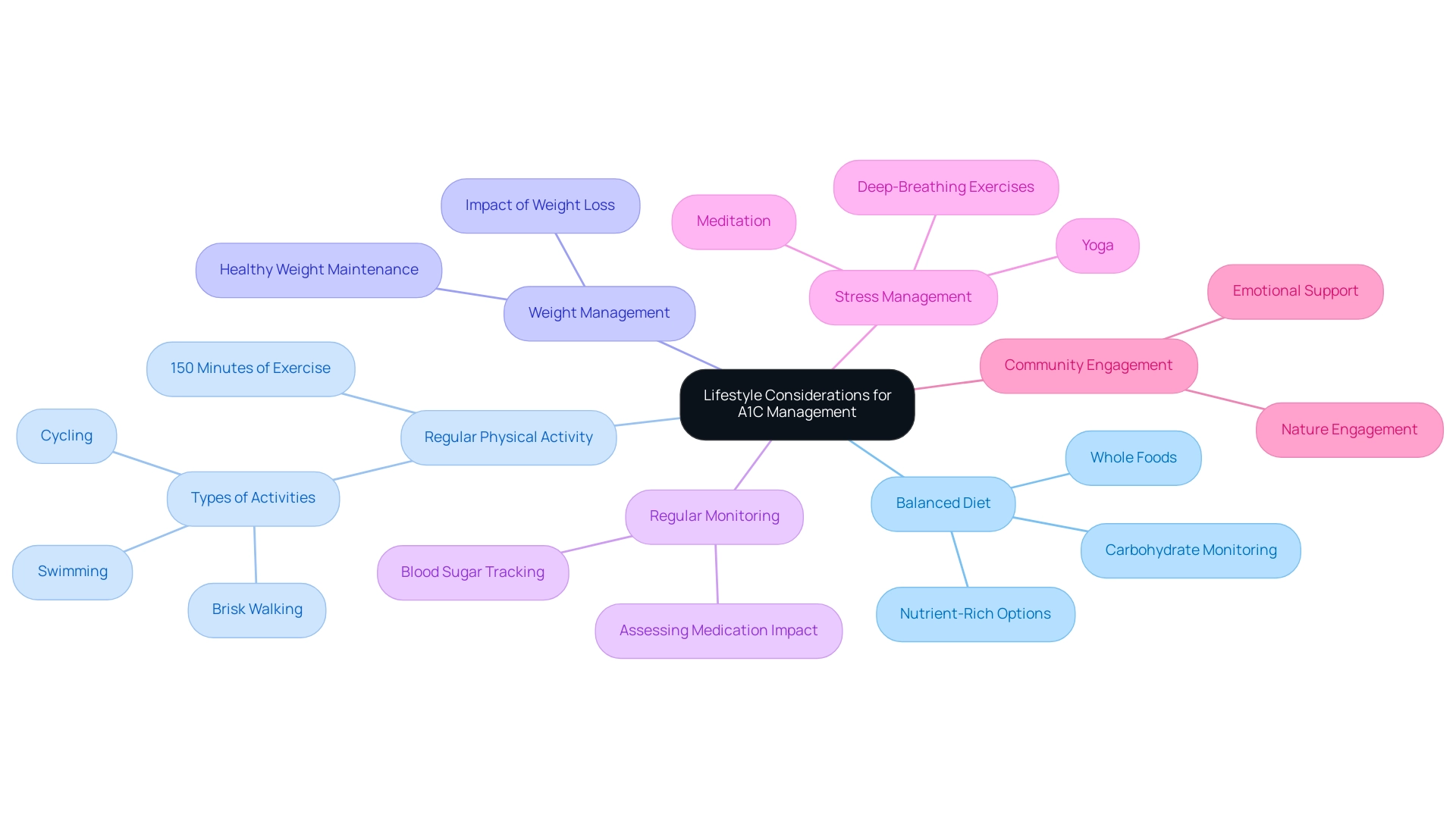
When managing Type 2, it is crucial to combine A1C medication with specific lifestyle changes that can significantly improve overall health outcomes. These lifestyle modifications include:
-
Balanced Diet: Prioritize whole foods rich in nutrients, such as a variety of vegetables, whole grains, lean proteins, and healthy fats.
Emphasizing whole grain options is vital for blood sugar control and sustained energy. Careful monitoring of carbohydrate intake is essential to prevent spikes in blood sugar levels, adversely affecting A1C readings.
-
Regular Physical Activity: Engaging in at least 150 minutes of moderate exercise per week, such as brisk walking, swimming, or cycling, enhances insulin sensitivity and aids in weight management. This level of activity is recommended to support overall metabolic health.
-
Weight Management: Maintaining a healthy weight is essential for improved blood sugar regulation and can significantly reduce the risk of complications linked to this condition. Weight loss, even in small amounts, has been shown to positively impact glucose levels.
-
Regular Monitoring: Consistent tracking of blood sugar levels allows individuals to assess how their medications and lifestyle choices influence their health. This self-monitoring is a crucial aspect of efficient blood sugar control.
-
Stress Management: Incorporating stress-reducing practices, such as yoga, meditation, or deep-breathing exercises, is crucial since stress can negatively impact blood sugar levels.
-
Embracing Nature and Community Support: Engaging with nature and community can provide emotional support and promote a positive lifestyle shift.
Significantly, a recent study suggested that the percentage of reported lifestyle modifications among individuals with blood sugar issues was lower than results from comparable studies in the Netherlands and the USA, emphasizing the necessity for enhanced lifestyle oversight strategies. Additionally, consider lesser-known strategies such as mindfulness practices or specific herbal supplements that may improve your plan. Addressing emotional aspects, including anxiety surrounding complications related to blood sugar issues, is essential for holistic care.
By incorporating these lifestyle factors with A1C medication, individuals can establish a more effective plan for controlling their condition and enhance their quality of life. The most recent comprehension of cardiovascular illness treatment in individuals with Type 2 conditions highlights the significance of these lifestyle modifications, as they can result in considerable enhancements in health outcomes. For more personalized strategies and support, click to register.
The Role of Healthcare Providers in Diabetes Management
Healthcare providers are essential to efficient management of the condition, offering customized knowledge and assistance to address individual needs. At Dr. Jason Shumard’s Integrative Wellness Center, the emphasis is on empowering individuals to remove anxiety regarding possible diabetes-related issues through holistic care and education. Regular consultations with a primary care physician or endocrinologist are essential for monitoring progress, adjusting treatments, and addressing specific concerns.
Dietitians at the center contribute by creating personalized nutrition plans, while educators play a key role in assisting patients in understanding their a1c medication and implementing self-management techniques. Additionally, mental health professionals are essential in managing the psychological aspects associated with living with this condition. A significant case study, titled ‘ABCs of Diabetes Control,’ reveals that only 11.1% of adults achieved all criteria for A1C, blood pressure, cholesterol, and smoking cessation, indicating substantial challenges in optimal health oversight.
This underscores the necessity of a cohesive healthcare team. Dr. Shumard emphasizes that his mission is to educate individuals on the benefits of a healthy lifestyle and to address the root causes of their conditions, thus fostering a transformative approach to health. Building a robust connection with the healthcare team improves patient-provider communication, guarantees that individuals obtain the highest quality of care, and cultivates a supportive atmosphere for effective health oversight.
Furthermore, the use of P-CGM devices, which can be owned or leased by healthcare providers, plays a crucial role in monitoring glucose levels, with varying costs depending on the manufacturer and specific CPT codes used for billing procedures. Recent statistics indicate a decrease in HbA1c among African American individuals from 30% to 18%, demonstrating the effectiveness of a1c medication in focused management strategies for the condition. Keeping abreast of current trends in care team approaches is essential for healthcare providers to adapt and optimize their strategies for improved patient outcomes.
Future Directions in Diabetes Medications
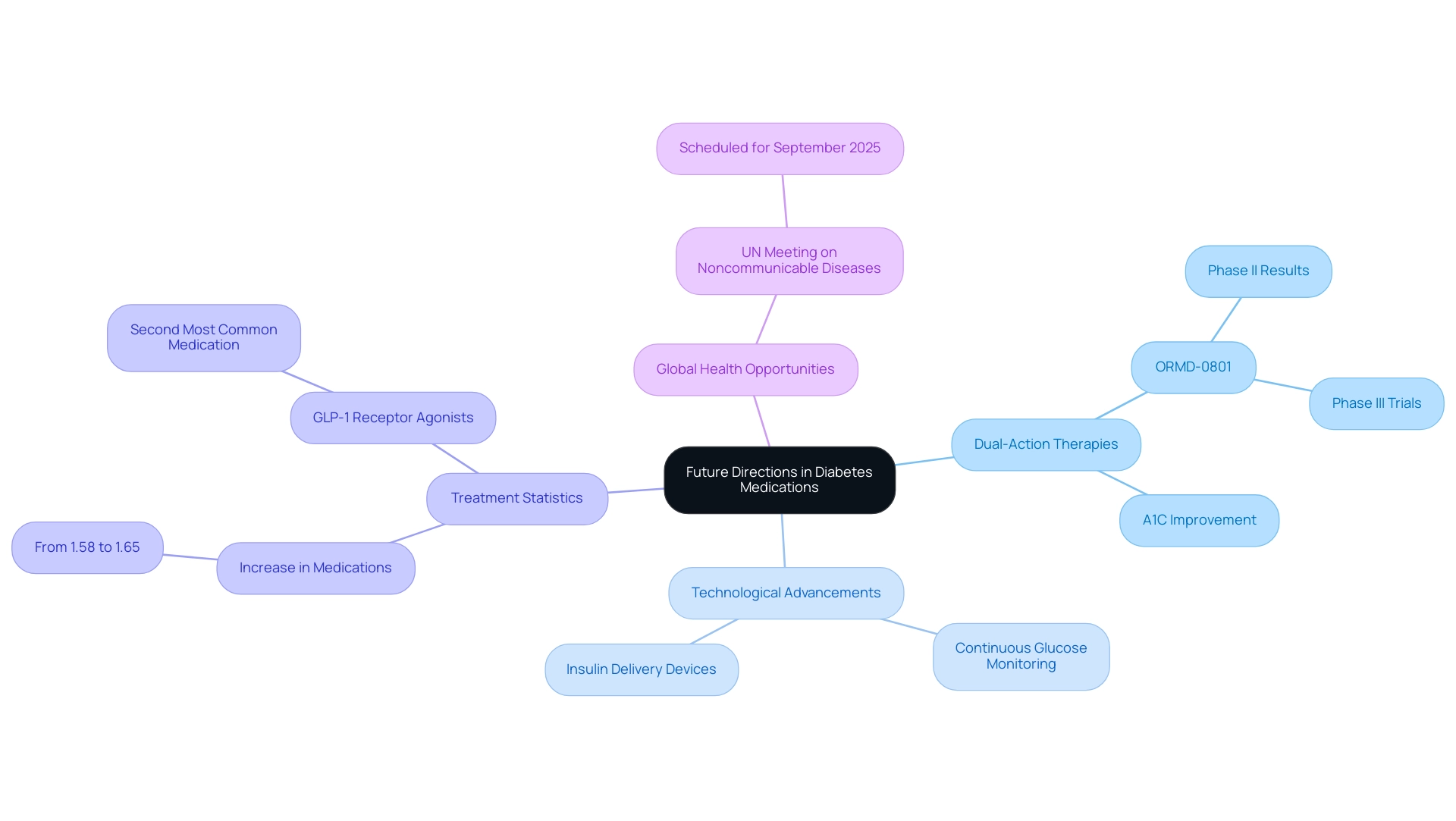
The landscape of diabetes therapies is continuously evolving, driven by ongoing research focused on developing more effective treatments. Notably, the emergence of dual-action therapies, which integrate the mechanisms of existing medications, is showing promise in enhancing A1C levels, particularly when combined with a1c medication to reduce side effects. For instance, ORMD-0801, an oral insulin capsule by Oramed, is currently undergoing Phase III trials after demonstrating positive results in Phase II.
As noted by Eldor et al.,
The oral insulin capsule ORMD-0801 showed promising results in Phase II trials, and individuals with T2DM are currently being enrolled for Phase III to further evaluate the drug’s future potential.
Moreover, advancements in technology, such as continuous glucose monitoring systems and innovative insulin delivery devices, are significantly improving personalized care for individuals with blood sugar issues. Research into genetic factors influencing treatment for this condition is also paving the way for more tailored therapeutic approaches.
The typical quantity of treatments for blood sugar regulation per individual has increased from 1.58 in 2018 to 1.65 in 2023, indicating a change in care that highlights the necessity for effective strategies that balance clinical advantages and expenses without placing extra financial pressures on individuals. This trend raises concerns about ensuring that increased drug use leads to improved health outcomes. Additionally, with the Fourth High-level Meeting of the United Nations General Assembly on the prevention and control of noncommunicable diseases scheduled for September 2025, there is a timely opportunity to address these issues on a global scale.
Staying informed about these developments is crucial, as patients may soon gain access to novel treatment options, including the increasingly popular GLP-1 receptor agonists, which have become the second most common a1c medication, significantly improving their diabetes management.
Conclusion
The management of diabetes requires a multifaceted approach that encompasses both medication and lifestyle modifications. Understanding the various classes of A1C-lowering medications—ranging from oral options like Metformin and DPP-4 inhibitors to injectable therapies such as GLP-1 receptor agonists and insulin—is vital for effective treatment. Each category has unique mechanisms of action that contribute to glycemic control, and recognizing these differences allows patients to engage more meaningfully with their healthcare providers.
Moreover, the importance of addressing potential side effects cannot be overstated. While medications play a crucial role in managing blood glucose levels, their associated risks highlight the need for careful monitoring and open communication between patients and healthcare professionals. This collaborative approach is essential to tailor treatment plans that minimize adverse effects while maximizing health benefits.
In addition to pharmacological interventions, adopting healthy lifestyle practices—such as maintaining a balanced diet, engaging in regular physical activity, and managing stress—can significantly enhance diabetes management outcomes. These lifestyle changes, combined with medication, empower patients to take control of their health and improve their quality of life.
Healthcare providers are pivotal in this journey, offering expertise, support, and education to help patients navigate their treatment options effectively. As the landscape of diabetes medications continues to evolve, staying informed about new therapies and personalized treatment strategies will be crucial for achieving optimal health outcomes. By embracing a holistic approach that integrates medication, lifestyle changes, and healthcare support, patients can better manage their diabetes and work towards a healthier future.
Frequently Asked Questions
What are the main categories of diabetes treatments?
Diabetes treatments are primarily divided into two categories: oral and injectable options.
What are some examples of oral diabetes treatments?
Examples of oral diabetes treatments include Metformin, Sulfonylureas, and DPP-4 inhibitors.
How does Metformin work?
Metformin enhances insulin sensitivity and reduces hepatic glucose production.
What is the function of Sulfonylureas in diabetes management?
Sulfonylureas stimulate insulin release from the pancreas.
What role do DPP-4 inhibitors play in managing diabetes?
DPP-4 inhibitors work to delay carbohydrate absorption, aiding in glycemic control by increasing incretin hormone levels.
When are injectable treatments necessary for diabetes patients?
Injectable treatments, such as GLP-1 receptor agonists and insulin therapies, are necessary for individuals with more advanced conditions or those who do not achieve adequate control with oral medications alone.
What is the significance of understanding diabetes treatment options?
Understanding these distinctions is crucial for patients to effectively navigate their treatment options and engage in informed conversations with healthcare providers.
What is the prevalence of prediabetes in the U.S.?
Approximately 97.6 million adults in the U.S. live with prediabetes, with notable prevalence among older adults.
What demographic groups show significant disparities in prediabetes prevalence?
Prevalence disparities include American Indian or Alaska Native adults at 16.0%, Black non-Hispanic adults at 12.5%, and Hispanic adults at 10.3%.
What is the public opinion regarding Medicare coverage for GLP-1 drugs?
Six in ten adults believe that Medicare should cover the cost of GLP-1 drugs for weight loss when prescribed for individuals who are overweight.
What holistic approaches are suggested for diabetes management?
A holistic approach includes lifestyle adjustments such as dietary changes, consistent exercise, and stress reduction methods, alongside understanding the mechanisms of diabetes medications.