Overview
Managing type 2 diabetes can be challenging, but effective insulin treatment and lifestyle modifications can make a significant difference. It’s important to recognize that proper insulin administration, combined with education and support, plays a crucial role in controlling blood sugar levels. This not only helps to prevent serious health complications but also empowers individuals to take charge of their health journey. Statistics show the benefits of hormone therapy and the positive impact of patient adherence to management strategies. By focusing on these aspects, we can encourage a healthier lifestyle together.
Introduction
Type 2 diabetes is a growing global concern that affects millions of people, often leading to serious health complications such as cardiovascular disease and kidney damage. It’s important to recognize that understanding the role of insulin in managing this condition is crucial. Effective hormone therapy can significantly improve blood sugar control and overall health outcomes. However, many individuals find themselves facing challenges in administering insulin properly and navigating their treatment plans.
How can patients empower themselves with knowledge and resources to master their diabetes management effectively?
Many patients feel overwhelmed by the complexities of their condition, but it’s essential to remember that you are not alone in this journey. With the right support and information, you can take charge of your health. By exploring effective strategies and resources, you can make informed decisions that lead to better management of your diabetes. This journey towards mastering your diabetes management starts with understanding and compassion.
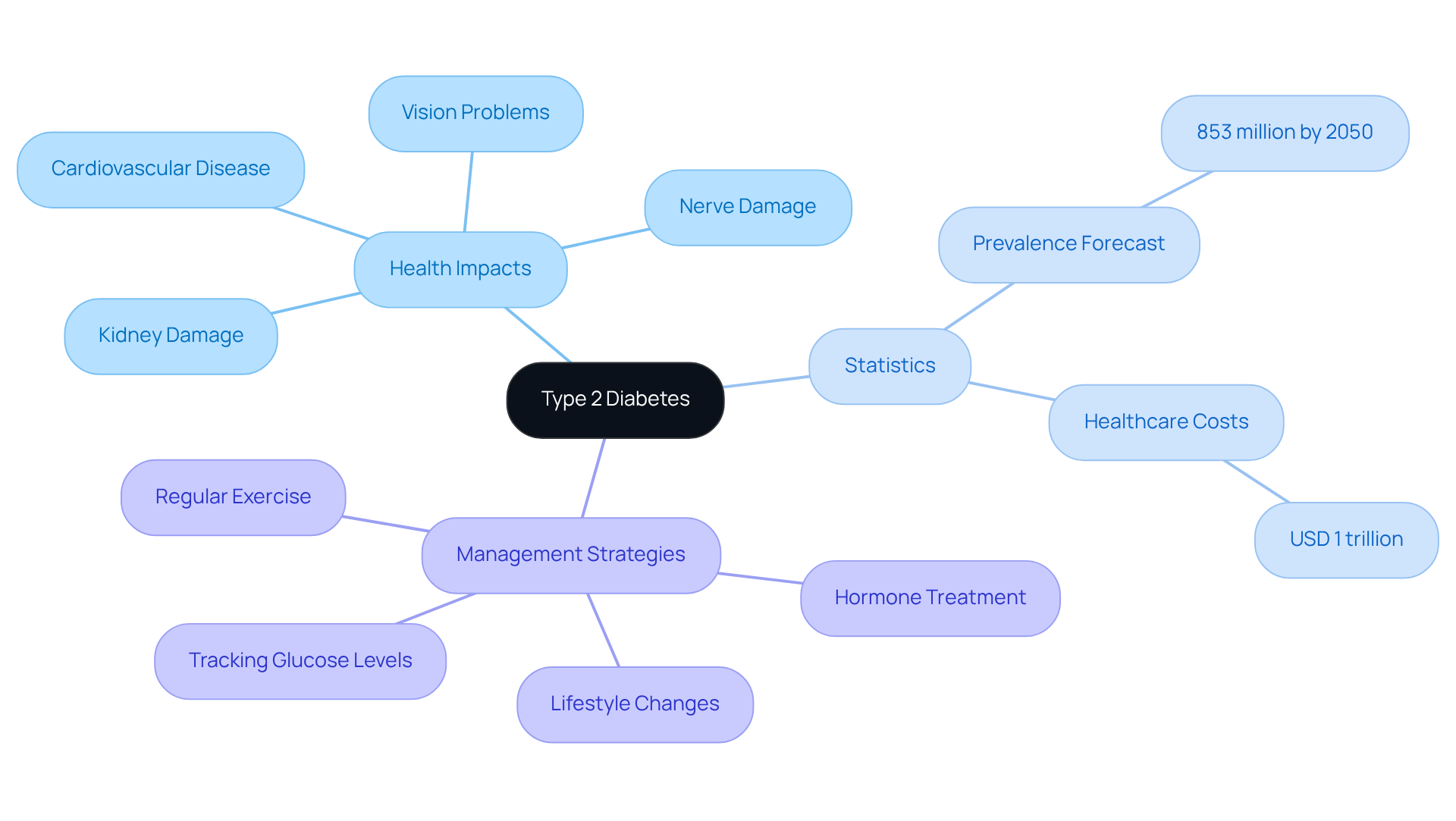
Define Type 2 Diabetes and Its Impact on Health
Type 2 diabetes: insulin resistance is a chronic condition that many individuals face. This means that in type 2 diabetes: insulin, the body’s cells may not respond as they should, which leads to elevated blood sugar levels. It’s important to recognize that this condition can lead to severe health complications, such as:
- Cardiovascular disease
- Kidney damage
- Nerve damage
- Vision problems
For instance, type 2 diabetes is the primary reason for new instances of blindness among individuals aged 18-64, with 10.1% of adults reporting significant vision challenges or blindness. Furthermore, many patients find that roughly 39.2% of adults with diagnosed blood sugar issues also experience chronic kidney disease, highlighting the serious risks linked to this condition.
The impact of type 2 diabetes extends beyond personal health, contributing significantly to worldwide health costs, which have reached at least USD 1 trillion—a staggering 338% increase over the past 17 years. Cardiovascular well-being is especially affected, as individuals with elevated glucose levels face a greater risk of heart disease. Research shows that high blood pressure is common in 80.6% of those with elevated glucose levels. This can feel overwhelming, but understanding these connections is the first step toward taking control.
Given the rising prevalence of type 2 diabetes: insulin, projected to affect 853 million adults by 2050, it is crucial for individuals to grasp the importance of effective management strategies. These encompass:
- Hormone treatment
- Lifestyle changes like maintaining a healthy weight
- Participating in regular exercise
- Consistently tracking glucose levels
By adopting these strategies, patients can significantly reduce the risk of complications and improve their overall health outcomes. Remember, small changes can lead to significant improvements in your health and well-being. Let’s embark on this journey together, focusing on what you can do today for a healthier tomorrow.
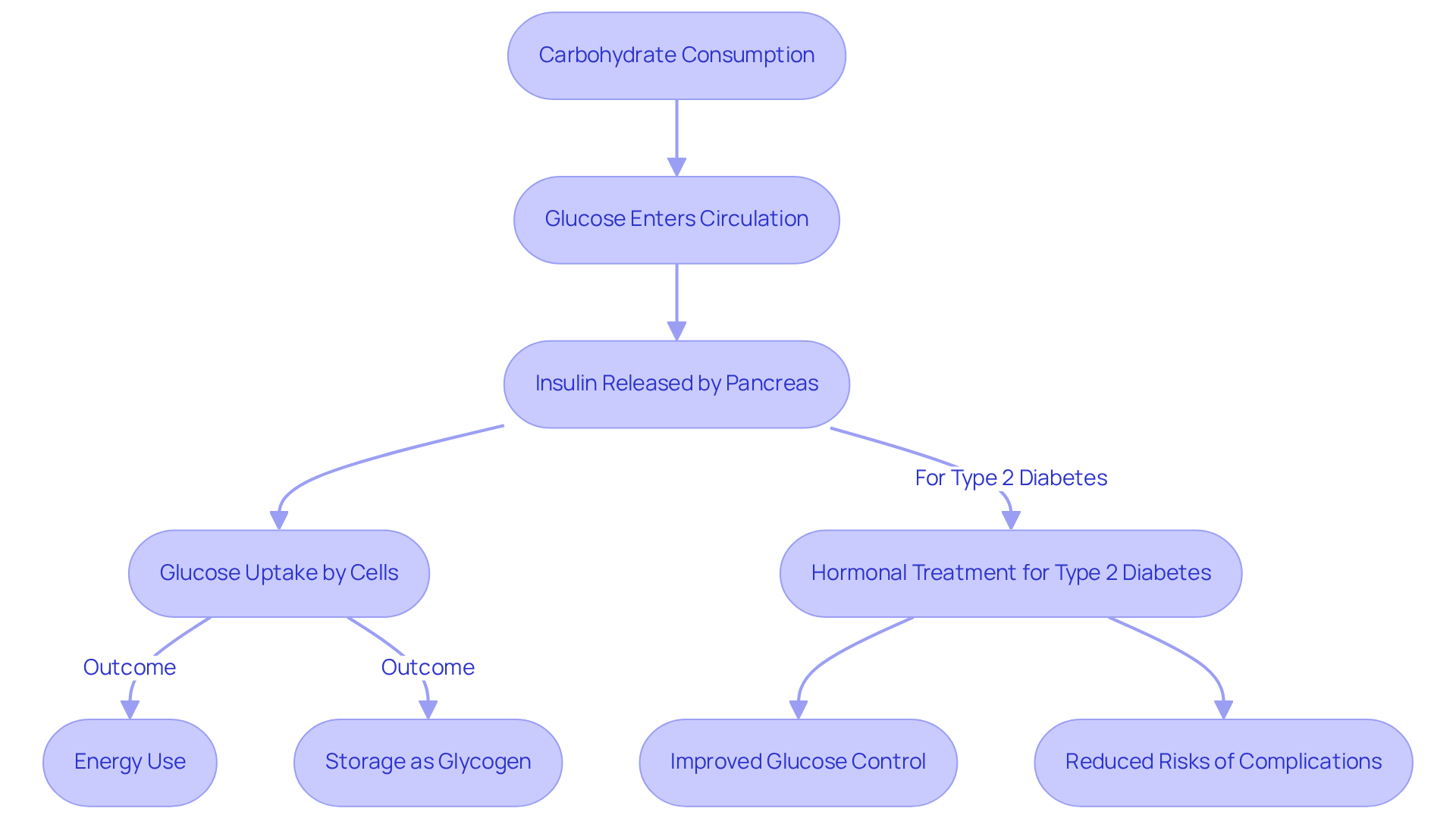
Explain Insulin’s Function in Blood Sugar Regulation
Insulin, a vital hormone produced by the pancreas, plays a crucial role in regulating sugar levels in our bloodstream. When we consume carbohydrates, they transform into glucose, which then enters our circulation. Insulin helps usher this glucose into our cells, where it can be used for energy or stored for later. However, for individuals facing type 2 diabetes, the body often struggles to respond effectively to this hormone, resulting in elevated blood sugar levels. This challenge underscores the importance of hormonal treatment, especially for type 2 diabetes, in managing blood sugar levels with care and effectiveness.
At the Integrative Wellness Center, Dr. Jason Shumard champions a holistic approach to diabetes management through functional medicine. This method not only prioritizes hormone therapy but also embraces lifestyle changes and dietary guidance, empowering patients on their health journeys. Have you considered how small changes in your daily routine can make a significant impact?
Statistics show that hormone treatment can significantly improve glucose control for patients with type 2 diabetes. Research reveals that patients adhering to their medication regimens often achieve target blood glucose levels, thereby reducing the risk of complications such as cardiovascular disease and kidney failure. Many patients report feeling more energized and experiencing an overall improvement in their well-being after beginning hormone treatment, which highlights its transformative potential in managing type 2 diabetes.
Moreover, insulin’s role extends beyond simply regulating glucose. It assists in energy storage by converting excess glucose into glycogen, which our bodies can utilize during fasting or times of increased energy demand. This dual function is essential for maintaining metabolic balance, especially for those with type 2 diabetes. By restoring normal sugar levels, hormone treatment not only mitigates immediate health risks but also plays a vital role in preventing long-term complications associated with type 2 diabetes.
The Integrative Wellness Center also emphasizes community support, offering resources and assistance to help patients manage their blood sugar effectively. By creating a nurturing environment, patients can share their experiences and strategies, enriching their overall wellness journey. However, it’s important to recognize the challenges that can accompany hormone therapy, such as the frequency of injections and the necessity for blood sugar monitoring, to provide a balanced view of its role in controlling blood sugar.
As you navigate your health journey, remember that every step counts. Together, we can work towards achieving your health goals with compassion and understanding.
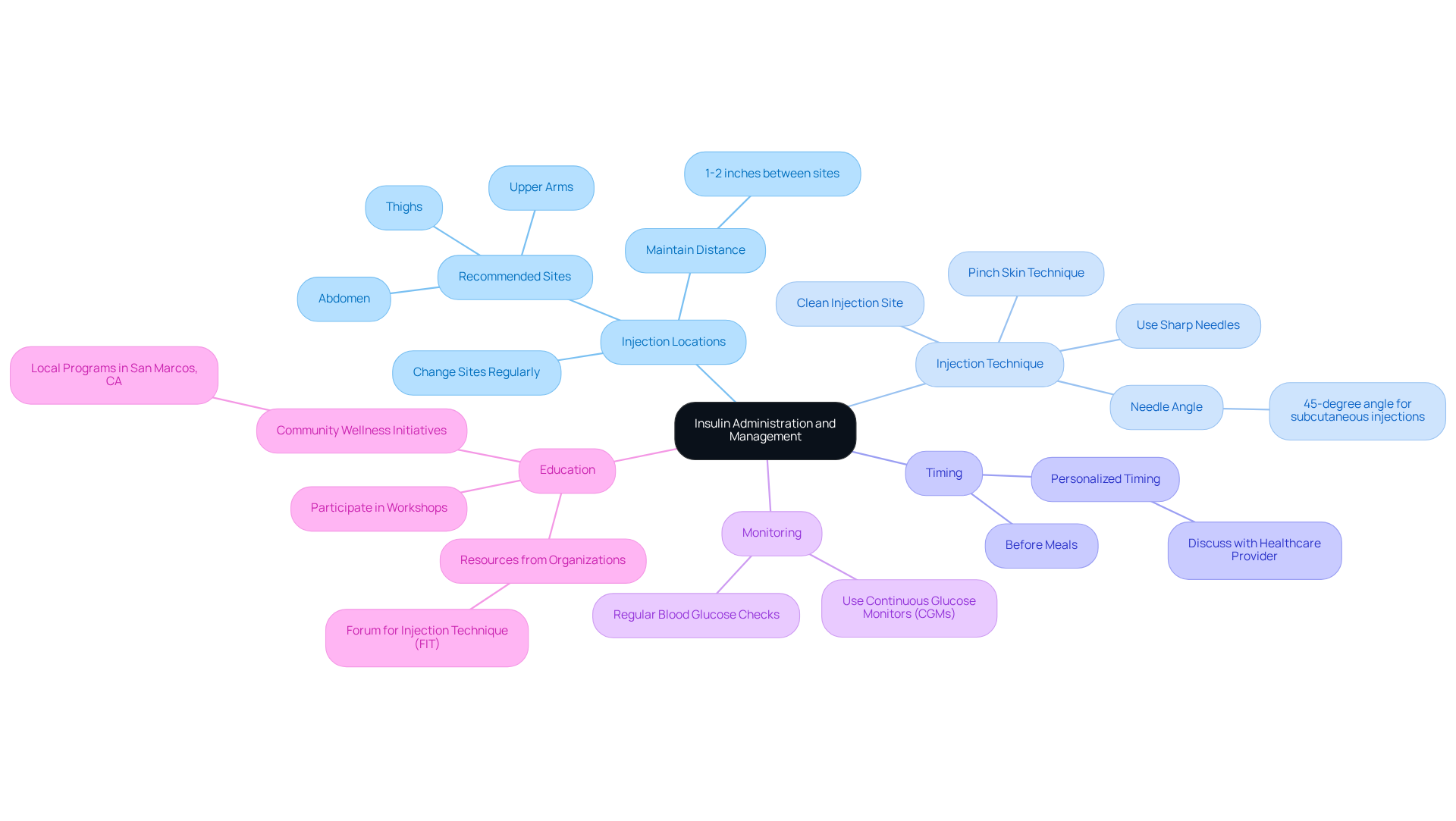
Outline Techniques for Insulin Administration and Management
Administering the hormone correctly is essential for effective diabetes management. It’s important to recognize that many individuals face challenges in this area. Here are some key techniques to enhance your insulin administration:
-
Injection Locations: Frequently changing injection locations is crucial to avoid lipodystrophy, which can lead to fat accumulation and irregular absorption of the hormone. Recommended sites include the abdomen, thighs, and upper arms. Maintaining a distance of at least 1-2 inches between injection sites is vital for optimal results.
-
Injection Technique: Many patients find that for subcutaneous injections, pinching the skin and inserting the needle at a 45-degree angle can make a significant difference. Using sharp needles and ensuring the injection site is clean can greatly improve comfort and effectiveness. Studies indicate that proper injection techniques can enhance long-term glycemic control.
-
Timing: Administering the hormone at suitable intervals, usually before meals, is key to effectively managing postprandial glucose spikes. Personalized timing should be discussed with your healthcare provider to align with your individual needs.
-
Monitoring: Regularly checking blood glucose levels helps you understand how the hormone affects your body and allows for necessary dosage adjustments. Continuous glucose monitors (CGMs) provide real-time data, assisting in refining strategies for hormone regulation.
-
Education: Participating in workshops or seminars can keep you updated on best practices for insulin control. Resources from organizations focused on managing blood sugar levels, such as the Forum for Injection Technique (FIT), offer valuable insights and training on effective injection techniques and site rotation strategies. Consistent education is vital, as many patients report inadequate training on proper injection methods, which can lead to complications. Furthermore, consider engaging with local community wellness initiatives in San Marcos, CA, which can provide customized assistance and resources for managing health effectively, promoting a sense of responsibility and motivation in your wellness journey.
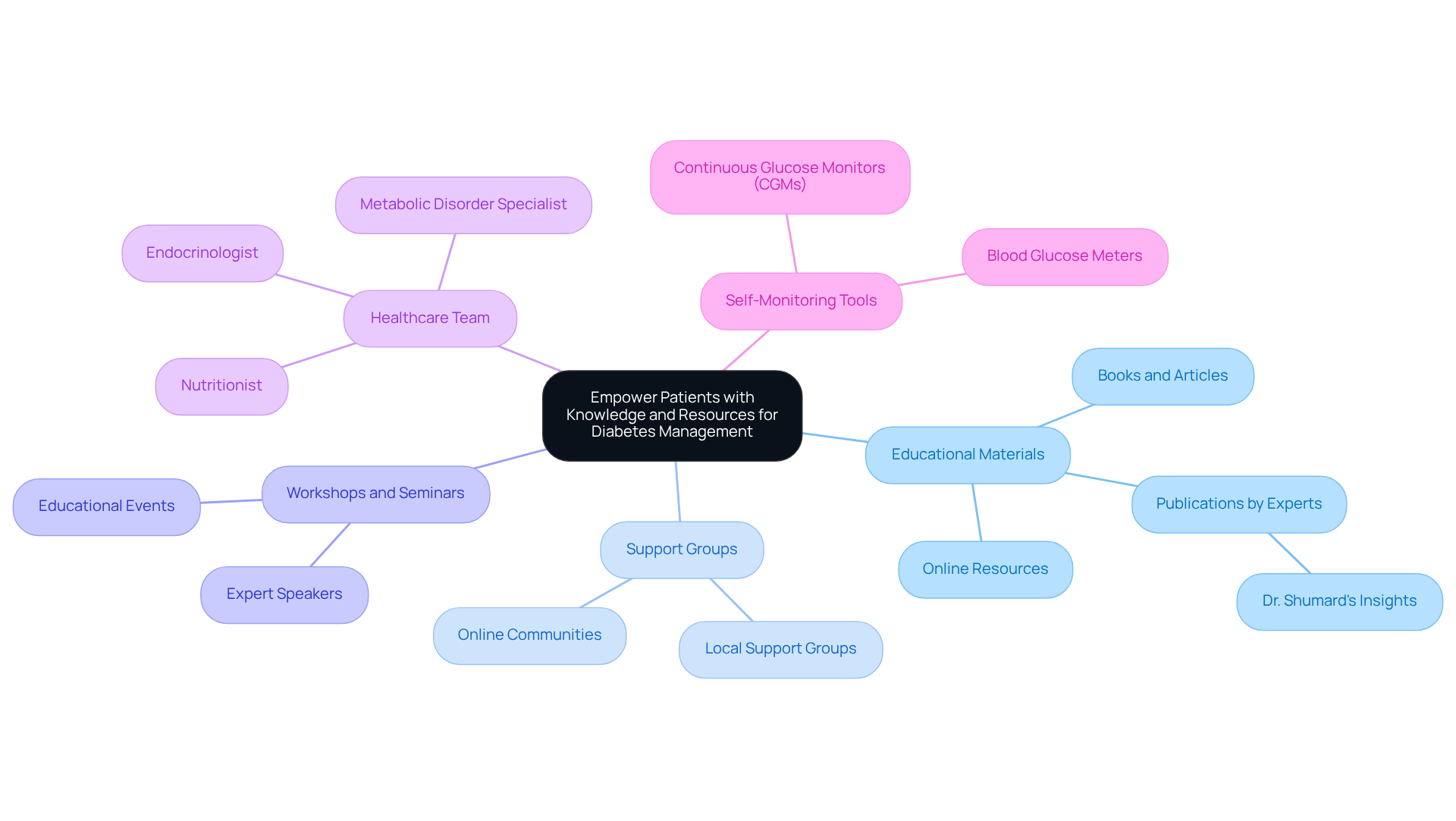
Empower Patients with Knowledge and Resources for Diabetes Management
Empowerment through education is a fundamental aspect of effective health control, especially for those navigating the challenges of diabetes. It’s important to recognize that having the right resources can make a significant difference in your journey. Here are some essential strategies to consider:
-
Educational Materials: Consider utilizing books, articles, and online resources focused on managing diabetes-related issues. Insightful publications by Dr. Shumard, for instance, offer valuable knowledge on reversing the condition and achieving optimal health.
-
Support Groups: Many patients find that engaging with local or online support groups can be incredibly beneficial. Sharing experiences with others facing similar challenges nurtures a sense of belonging and provides emotional support, which is essential for effectively managing your condition.
-
Workshops and Seminars: Participating in educational events can help you stay updated on the latest advancements in glucose care and treatment techniques. These gatherings often feature knowledgeable speakers who provide useful advice for everyday management.
-
Healthcare Team: Collaborating with a healthcare team that includes a metabolic disorder specialist, nutritionist, and endocrinologist can lead to a customized management plan. This multidisciplinary approach ensures that all aspects of your health are addressed, ultimately leading to better outcomes.
-
Self-Monitoring Tools: Investing in tools like blood glucose meters and continuous glucose monitors (CGMs) can empower you to track your progress. Regularly reviewing your data with your healthcare provider can help optimize your treatment plan, allowing for timely adjustments based on your individual needs.
By utilizing these resources and strategies, you can take proactive steps in managing your diabetes. Remember, each small action can lead to improved health outcomes and a better quality of life. You are not alone on this journey; support is available, and together we can work towards a healthier future.
Conclusion
Mastering type 2 diabetes management is crucial for improving health outcomes and minimizing complications associated with this chronic condition. It’s important to recognize that understanding the role of insulin and the significance of effective administration techniques empowers individuals to take control of their health. By embracing a holistic approach that combines hormone treatment, lifestyle changes, and community support, patients can significantly enhance their quality of life and reduce the risks linked to type 2 diabetes.
Many patients find that key strategies for managing type 2 diabetes include:
- Recognizing the importance of insulin in blood sugar regulation
- Adopting effective administration techniques
- Valuing education and resources
The insights shared illustrate that successful management is not solely about medication; it also involves adopting healthy habits, staying informed, and engaging with supportive communities. This multifaceted approach can lead to substantial improvements in overall well-being.
Ultimately, the journey to mastering type 2 diabetes requires commitment and proactive measures. By utilizing available resources, participating in educational opportunities, and seeking support from healthcare professionals and peer groups, individuals can navigate their health challenges more effectively. Empowerment through knowledge and community engagement is crucial for transforming the management of type 2 diabetes into a more manageable and less daunting experience. Together, these steps pave the way for a healthier future, where individuals can thrive despite the challenges of diabetes.
Frequently Asked Questions
What is Type 2 diabetes?
Type 2 diabetes is a chronic condition characterized by insulin resistance, where the body’s cells do not respond effectively to insulin, leading to elevated blood sugar levels.
What are the health complications associated with Type 2 diabetes?
Type 2 diabetes can lead to severe health complications, including cardiovascular disease, kidney damage, nerve damage, and vision problems.
How does Type 2 diabetes affect vision?
Type 2 diabetes is a leading cause of blindness among individuals aged 18-64, with 10.1% of adults experiencing significant vision challenges or blindness.
What is the connection between Type 2 diabetes and kidney disease?
Approximately 39.2% of adults with diagnosed blood sugar issues also experience chronic kidney disease, highlighting the serious risks associated with Type 2 diabetes.
What is the economic impact of Type 2 diabetes?
The worldwide health costs associated with Type 2 diabetes have reached at least USD 1 trillion, marking a 338% increase over the past 17 years.
How does Type 2 diabetes affect cardiovascular health?
Individuals with elevated glucose levels are at a greater risk of heart disease, with high blood pressure being common in 80.6% of those with elevated glucose levels.
What is the projected prevalence of Type 2 diabetes by 2050?
Type 2 diabetes is projected to affect 853 million adults worldwide by 2050.
What are some effective management strategies for Type 2 diabetes?
Effective management strategies include hormone treatment, lifestyle changes like maintaining a healthy weight, participating in regular exercise, and consistently tracking glucose levels.
How can small changes impact health outcomes for those with Type 2 diabetes?
Adopting small changes in lifestyle and health management can significantly reduce the risk of complications and improve overall health outcomes for individuals with Type 2 diabetes.