Overview
Type 2 diabetes can feel overwhelming, as it is a long-lasting metabolic condition marked by insulin resistance and relative insulin deficiency. This often leads to elevated blood glucose levels and a range of health complications. It’s important to recognize that managing this condition effectively is crucial. Many patients find that implementing lifestyle changes—such as improved nutrition and regular exercise—can significantly enhance insulin sensitivity and overall health outcomes.
Have you ever felt frustrated by the daily challenges of managing your diabetes? You’re not alone. Many individuals share similar experiences, and it’s completely understandable to seek support. By focusing on small, achievable changes, you can take meaningful steps toward a healthier lifestyle.
Consider joining the 30-Day Diabetes Reset program, where you can find guidance tailored to your needs. Remember, every step you take is a step toward better health. Together, we can navigate this journey with compassion and care.
Introduction
In the face of a global diabetes epidemic, understanding the intricacies of type 2 diabetes is more crucial than ever. This chronic metabolic disorder, marked by insulin resistance and relative insulin deficiency, affects millions and presents significant health challenges. As the prevalence of this condition continues to rise, it’s important to recognize its mechanisms, progression, and effective management strategies.
Many individuals living with type 2 diabetes experience daily struggles that can feel overwhelming. From the differences between type 1 and type 2 diabetes to the vital role of lifestyle changes, it’s essential to approach this journey with compassion and understanding. A comprehensive strategy that integrates nutrition, exercise, and education can empower you to take charge of your health.
By delving into these key concepts, this article aims to illuminate the path toward better management and improved quality of life for those affected by type 2 diabetes. Together, we can explore effective ways to navigate this condition, fostering hope and resilience along the way.
Define Type 2 Diabetes: Key Concepts and Mechanisms
Diabetes type 2 explained reveals that it is a long-lasting metabolic condition that many individuals struggle with, characterized by resistance to insulin and a relative deficiency of this crucial hormone. Under this condition, the body’s cells show reduced responsiveness to insulin, which is vital for glucose uptake, leading to increased blood glucose levels. It’s important to recognize that the key mechanisms involved include:
- Insulin Resistance: This occurs when the body’s cells become less responsive to insulin, impairing their ability to absorb glucose effectively.
- Beta Cell Dysfunction: Over time, the pancreas may struggle to produce adequate amounts of insulin needed to counteract the effects of resistance, leading to further complications.
- Increased Glucose Production: The liver may produce excess glucose, exacerbating hyperglycemia and complicating management efforts.
Many patients find that recent research emphasizes the commonality of glucose resistance among those with type 2 diabetes, impacting a significant segment of the population. The metabolic consequences of this condition can feel overwhelming, including hyperglycemia, hypertension, dyslipidemia, and elevated inflammatory markers, all of which contribute to the overall health burden.
Understanding the significance of addressing insulin resistance is essential in the context of diabetes type 2 explained as a fundamental aspect of managing the condition. Effective interventions often focus on lifestyle changes, such as dietary adjustments and increased physical activity, which can enhance glucose sensitivity and support beta cell function. However, many conventional therapies, including medications and hormone treatments, tend to alleviate symptoms rather than address the underlying causes of the illness. These traditional methods can sometimes lead to side effects that jeopardize long-term well-being.
While continuous glucose monitoring (CGM) shows promise in managing insulin resistance, it’s crucial to remember that lifestyle changes remain the cornerstone of effective diabetes management. Comprehending these mechanisms is vital for creating focused management strategies that empower individuals to take charge of their health, as diabetes type 2 explained can significantly improve their quality of life. As Dr. Shumard states, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being.
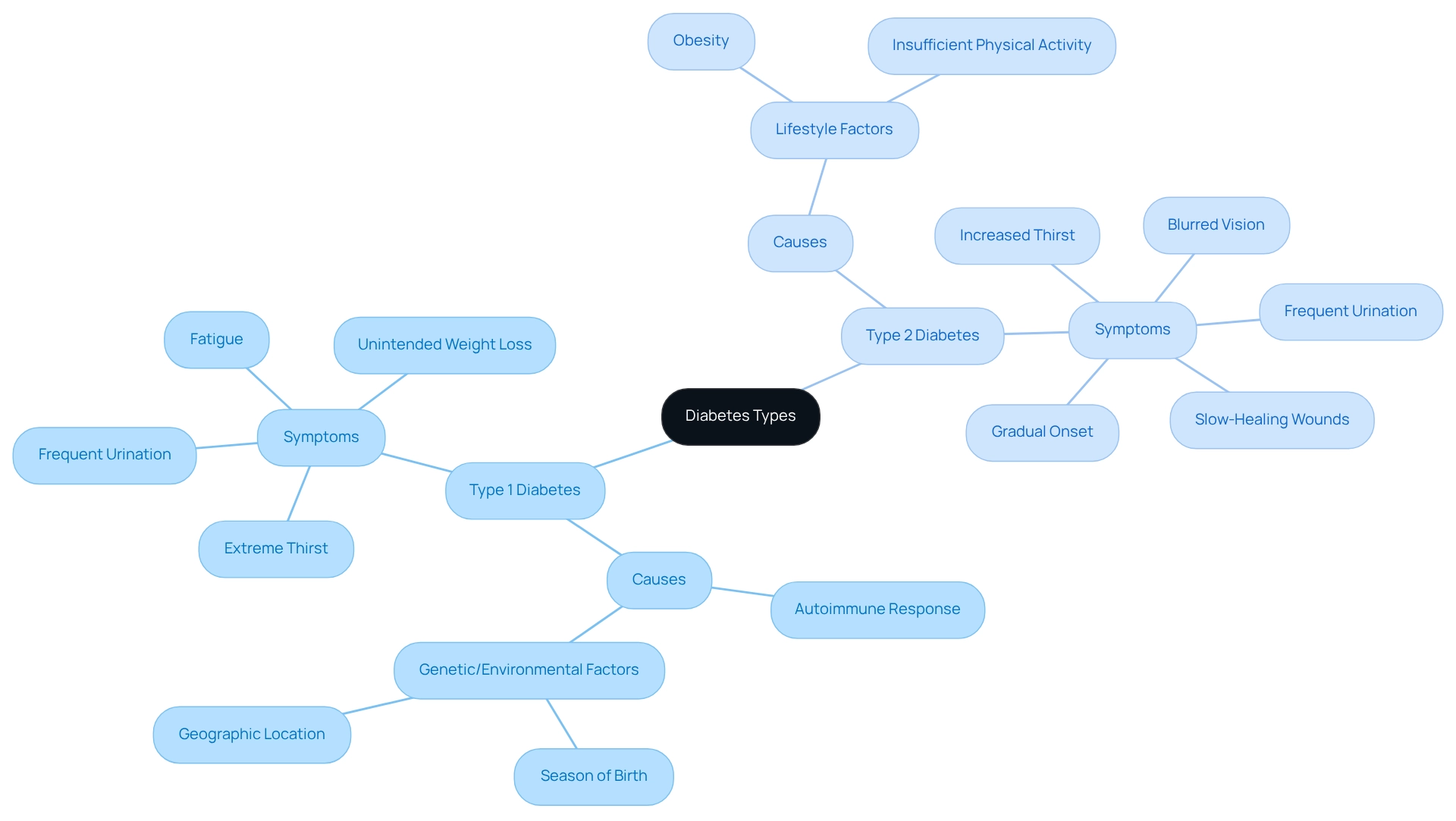
Differentiate Between Type 1 and Type 2 Diabetes: Causes and Symptoms
Class 1 and class 2 conditions reveal distinct origins and signs that are essential to understand.
Class 1 Condition: This autoimmune disorder occurs when the immune system mistakenly targets and destroys the insulin-producing beta cells in the pancreas. Symptoms often appear suddenly, manifesting as extreme thirst, frequent urination, fatigue, and unintended weight loss. It’s important to recognize that recent findings indicate genetic and environmental factors, such as the season of birth and geographic location, may influence how this condition progresses.
On the other hand, diabetes type 2 explained is mainly linked to lifestyle factors, such as obesity and insufficient physical activity. It tends to develop gradually, often without noticeable symptoms in the early stages. Many patients find that the common symptoms of diabetes type 2 explained include increased thirst, frequent urination, slow-healing wounds, and blurred vision. Alarmingly, the prevalence of conditions related to diabetes type 2 explained has been increasing significantly, with a reported annual rise of 4.8% from 2002 to 2012. This trend underscores the urgent need for lifestyle interventions.
Understanding these differences is crucial for effective management and treatment strategies. By recognizing the unique challenges each type of condition presents, healthcare professionals can tailor interventions to better meet the specific needs of individuals. Together, we can navigate these journeys toward healthier living.
Explore the Progression of Type 2 Diabetes: Understanding Changes Over Time
Diabetes type 2 explained illustrates that it is a progressive condition that unfolds through distinct stages, each carrying significant implications for management and health outcomes. It’s important to recognize that understanding these stages can empower you in your journey toward better health. The key stages include:
- Insulin Resistance: Initially, the body compensates for this resistance by producing more of the hormone. This phase often goes unnoticed, yet it lays the groundwork for future challenges. Have you ever felt like your body is working harder than it should?
- Prediabetes: At this stage, blood sugar levels are elevated but not high enough to be classified as a health condition. Recognizing prediabetes is crucial, as it serves as a warning sign and a chance for intervention. Current data shows that a significant portion of the population is affected by prediabetes, with many advancing to type 2 if lifestyle changes are not made. This is a call to action for many of us.
- Type 2 Condition: As the situation progresses, the pancreas may struggle to produce enough insulin, leading to higher blood sugar levels. This phase often brings various wellness challenges, including an increased risk of depression. In fact, individuals with high blood sugar are twice as likely to encounter this condition compared to those who are not affected.
- Issues: Over time, unmanaged high blood sugar can lead to serious complications such as cardiovascular disease, neuropathy, and kidney damage. The financial and wellness challenges associated with the condition are substantial, with medical expenses rising considerably.
Acknowledging these phases is crucial for you, as it highlights the importance of early intervention and proactive lifestyle changes. Participating in regular physical activity is especially important; research indicates that 31.9% of adults with diagnosed conditions are not active. This underscores the need for programs that promote improved well-being among this group. By understanding what diabetes type 2 explained entails, you can take informed steps toward managing your health effectively. Remember, you are not alone on this journey, and every small change can lead to significant improvements.
Implement Holistic Management Strategies: Nutrition, Exercise, and Education
Managing diabetes type 2 explained can feel overwhelming, but a holistic approach can truly make a difference in your journey. Let’s explore some key components that can help you take control of your health.
- Nutrition: It’s essential to focus on a balanced diet filled with whole foods. Think of incorporating more fruits, vegetables, lean proteins, and whole grains into your meals. Limiting processed foods and added sugars is crucial, as these can lead to spikes in blood sugar levels. Many people have found that making these dietary changes leads to significant improvements in their blood glucose control and overall well-being.
- Exercise: Aim for at least 150 minutes of moderate aerobic activity each week, along with strength training exercises at least twice a week. Regular physical activity not only boosts insulin sensitivity but also helps manage blood pressure and cholesterol levels. Engaging in both aerobic and resistance training can enhance your quality of life and lower the risk of cardiovascular complications, as diabetes type 2 explained emphasizes the importance of physical activity and self-management education. This knowledge allows you to make informed choices about your health, leading to better diabetes management.
By implementing these strategies, you can experience improved blood sugar regulation, enhanced mental well-being, and a better quality of life. Remember, a holistic approach that combines nutrition, exercise, and education is vital for achieving lasting health benefits and reducing reliance on medications. It’s important to recognize that you’re not alone in this journey—many have walked this path and found success. Take the first step today toward a healthier, more fulfilling life.
Conclusion
Managing type 2 diabetes can feel overwhelming, but understanding its complexities is the first step toward empowerment. Recognizing key mechanisms like insulin resistance and beta cell dysfunction is crucial, as is distinguishing between type 1 and type 2 diabetes. This distinction highlights the importance of addressing lifestyle factors that significantly influence the onset and progression of type 2 diabetes.
It’s important to recognize that this journey involves multiple stages, from insulin resistance to potential complications. Early intervention is vital. Many patients find that engaging in proactive lifestyle changes, such as maintaining a balanced diet and incorporating regular physical activity, can dramatically alter their health outcomes. The evidence supporting these strategies reinforces the idea that individuals with type 2 diabetes have the power to reclaim their health through informed choices.
Ultimately, a holistic management strategy that integrates nutrition, exercise, and education is essential for those living with type 2 diabetes. By fostering a supportive environment and promoting self-management education, individuals can enhance their quality of life and reduce the risk of complications. Embracing this journey with compassion and determination not only paves the way for greater resilience but also fosters hope for a brighter future in the face of diabetes.
Frequently Asked Questions
What is diabetes type 2?
Diabetes type 2 is a long-lasting metabolic condition characterized by insulin resistance and a relative deficiency of insulin, leading to increased blood glucose levels.
What are the key mechanisms involved in diabetes type 2?
The key mechanisms include insulin resistance, beta cell dysfunction, and increased glucose production by the liver.
What is insulin resistance?
Insulin resistance occurs when the body’s cells become less responsive to insulin, impairing their ability to absorb glucose effectively.
How does beta cell dysfunction affect diabetes type 2?
Over time, the pancreas may struggle to produce enough insulin to counteract insulin resistance, leading to further complications in managing blood glucose levels.
What role does the liver play in diabetes type 2?
The liver may produce excess glucose, which exacerbates hyperglycemia and complicates management efforts.
What are the metabolic consequences of diabetes type 2?
The metabolic consequences include hyperglycemia, hypertension, dyslipidemia, and elevated inflammatory markers, all contributing to the overall health burden.
How can insulin resistance be managed in diabetes type 2?
Effective management often focuses on lifestyle changes, such as dietary adjustments and increased physical activity, which can enhance glucose sensitivity and support beta cell function.
What are the limitations of conventional therapies for diabetes type 2?
Many conventional therapies, including medications and hormone treatments, tend to alleviate symptoms rather than address the underlying causes, and they can sometimes lead to side effects that jeopardize long-term well-being.
How does continuous glucose monitoring (CGM) help in managing diabetes type 2?
Continuous glucose monitoring (CGM) shows promise in managing insulin resistance, but lifestyle changes remain the cornerstone of effective diabetes management.
Why is understanding the mechanisms of diabetes type 2 important?
Understanding these mechanisms is vital for creating focused management strategies that empower individuals to take charge of their health and significantly improve their quality of life.