Overview
The article titled “Caring Implementation of the DKA Protocol: A Step-by-Step Guide for Healthcare Providers” offers a nurturing framework for healthcare professionals to manage diabetic ketoacidosis (DKA) effectively.
It’s important to recognize that managing DKA can be overwhelming for both patients and providers. This guide emphasizes the significance of an interprofessional team approach, patient education, and personalized care strategies. By focusing on these elements, we can improve outcomes and ensure that every patient feels supported.
Many patients find that understanding their condition is crucial to their recovery. This article provides detailed protocols for diagnosis, treatment, and preventive measures, all aimed at enhancing patient safety and health management.
Through compassionate care and collaboration, healthcare providers can make a meaningful difference in the lives of those affected by DKA. Let’s work together to create a supportive environment that fosters healing and well-being.
Introduction
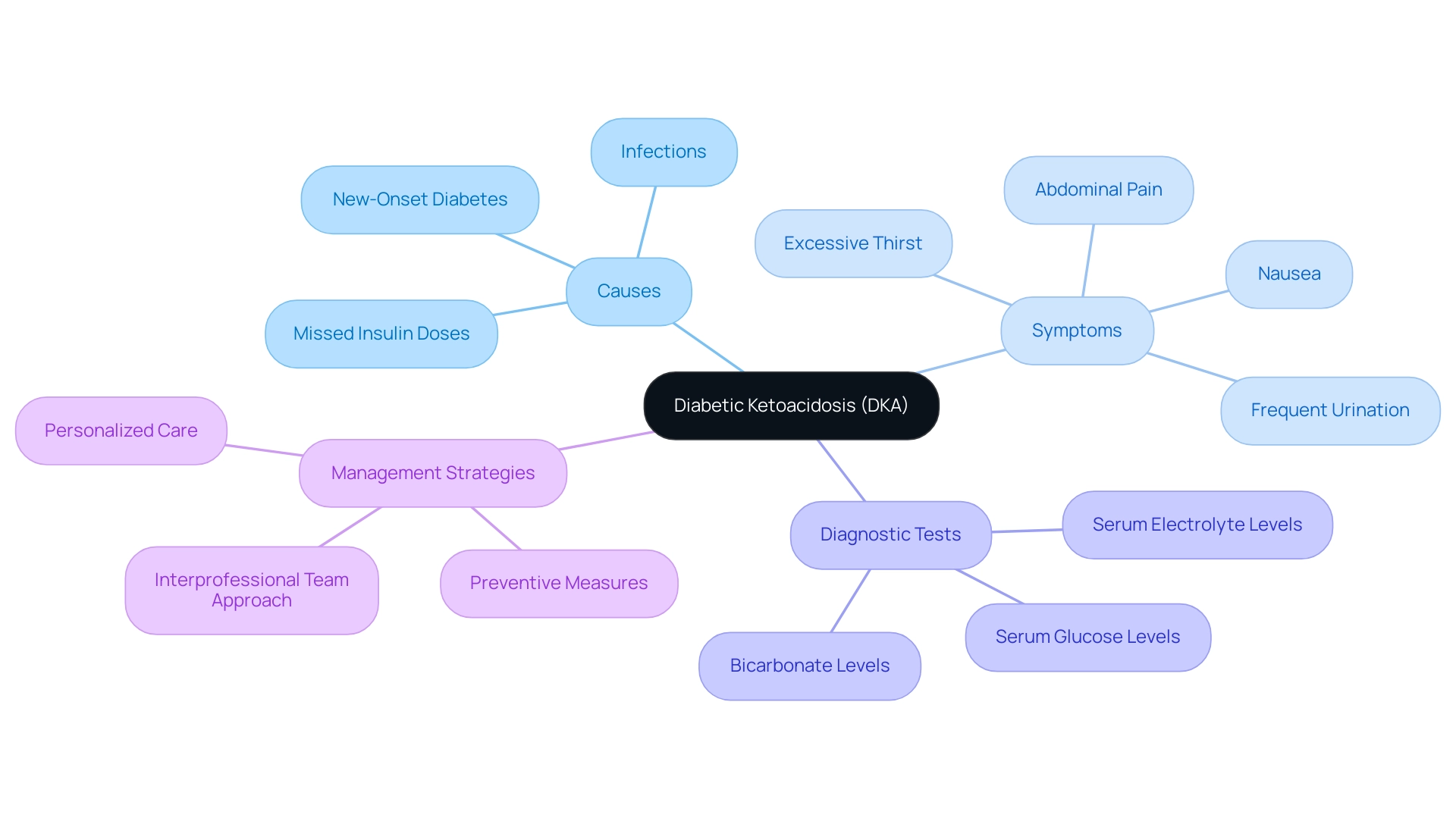
In the realm of diabetes management, Diabetic Ketoacidosis (DKA) presents a significant challenge, one that requires urgent attention from both healthcare providers and patients. It’s important to recognize that DKA is characterized by a dangerous triad of uncontrolled hyperglycemia, metabolic acidosis, and elevated ketone levels. This condition can escalate rapidly, often triggered by factors such as infections or missed insulin doses. Many patients find that understanding the causes, symptoms, and effective management protocols of DKA is crucial, especially as its prevalence continues to rise.
This article delves into the intricacies of DKA—from its diagnostic criteria and laboratory findings to step-by-step management and preventive measures. Our goal is to equip you with essential knowledge to combat this serious condition and empower you to take control of your health. Remember, you are not alone in this journey; together, we can navigate the complexities of diabetes management.
Understanding Diabetic Ketoacidosis: An Overview
Diabetic Ketoacidosis (DKA) is a serious and potentially life-threatening complication of diabetes. It is characterized by uncontrolled hyperglycemia, metabolic acidosis, and elevated ketone levels. This condition often arises when the body lacks sufficient insulin, leading to the breakdown of fat for energy and an increase in ketone production. In 2025, the prevalence of DKA continues to be a significant concern, with recent studies showing an increase in hospital admissions related to DKA, highlighting the urgent need for effective treatment methods.
It’s important to recognize that the onset of DKA can be triggered by various factors, such as:
- Infections
- Missed insulin doses
- The emergence of new-onset diabetes
Understanding these underlying causes is essential for healthcare providers to implement timely interventions. Many patients find that being aware of the early signs of DKA—such as excessive thirst, frequent urination, nausea, and abdominal pain—can make a significant difference in their health outcomes.
Initial laboratory studies for DKA usually include:
- Serum glucose levels
- Serum electrolyte levels
- Bicarbonate levels
These tests are critical for understanding the diagnosis and treatment of this condition. A recent analysis of diabetes incidence across U.S. counties revealed stark variations, with rates of diagnosed diabetes ranging from 2.2 to 53.5 per 1,000 people in 2020. This variability underscores the necessity for targeted public health initiatives to address diabetes and its complications, especially in areas with high incidence rates.
Effective management of DKA requires an interprofessional team approach. Involving a diverse group of healthcare professionals ensures comprehensive care. This collaborative strategy not only improves outcomes for individuals but also promotes a deeper understanding of DKA among providers. Dr. Jason Shumard emphasizes, “By offering individuals actionable insights and practical resources, the center creates a setting where people can regain their wellness and well-being.”
This philosophy is central to the approach at Integrative Wellness Center, where personalized functional medicine strategies, including tailored nutrition plans and regular testing, empower individuals to manage their diabetes effectively.
Real-world examples illustrate the complications that can arise from DKA, such as prolonged hospital stays and increased healthcare costs. These outcomes further emphasize the importance of preventive measures and education. Dr. Shumard’s dedication to comprehensive wellness solutions and customized nutrition plays a vital role in assisting individuals in reducing these risks and managing their well-being.
In summary, a thorough understanding of the DKA protocol, including its causes and management, is crucial for healthcare providers. By prioritizing personalized care and education, as demonstrated by Dr. Jason Shumard’s holistic approach, healthcare professionals can enable individuals to take control of their health and reduce the risks associated with this serious condition.
Recognizing the Signs and Symptoms of DKA
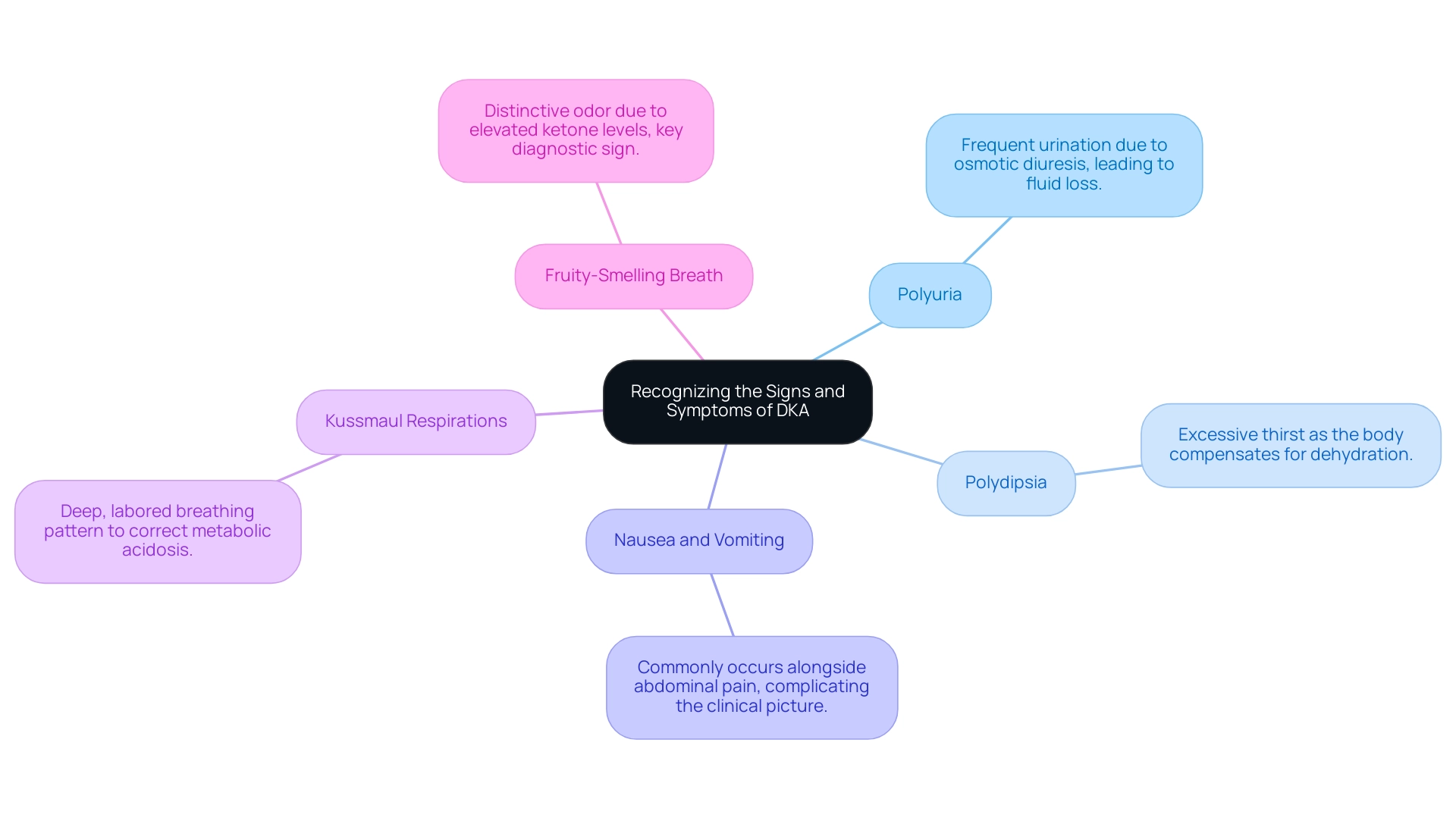
Healthcare providers must maintain a high level of vigilance for the classic signs and symptoms of diabetic ketoacidosis (DKA protocol), as early recognition is crucial for effective intervention. It’s important to recognize that the primary indicators include:
- Polyuria: Patients often experience frequent urination due to osmotic diuresis, which can lead to significant fluid loss.
- Polydipsia: Excessive thirst is a common response as the body attempts to compensate for dehydration resulting from fluid loss.
- Nausea and Vomiting: These symptoms frequently occur alongside abdominal pain, which can complicate the clinical picture.
- Kussmaul Respirations: This deep, labored breathing pattern is the body’s effort to correct metabolic acidosis, which is addressed in the DKA protocol.
- Fruity-Smelling Breath: The presence of elevated ketone levels often results in a distinctive fruity odor, serving as a key diagnostic sign.
Many patients find that understanding these symptoms can empower them in their health journey. Statistics indicate that in 2025, a significant percentage of individuals with type 2 diabetes present with these classic symptoms, emphasizing the need for healthcare providers to be adept at recognizing the DKA protocol. Reports indicate that nearly 30% of individuals admitted for diabetes-related complications exhibit these signs, which underscores the urgency of prompt diagnosis and treatment according to the DKA protocol.
Patients should be treated according to the DKA protocol with insulin until resolution, defined as blood glucose less than 200 mg/dl and two of the following: serum bicarbonate level greater than or equal to 15 mEq/l, venous pH greater than 7.3, or calculated anion gap less than or equal to 12 mEq/l.
Recent studies emphasize the importance of an interprofessional team approach in effectively managing the DKA protocol. This collaborative strategy not only enhances outcomes for individuals but also reinforces the necessity of education and self-management support to prevent complications like ketoacidosis. Real-life examples from case studies illustrate how timely recognition of DKA symptoms has led to improved experiences and outcomes, with many individuals expressing gratitude for the proactive care they received.
For example, one individual shared, “Thanks to the Integrative Wellness Center’s approach, I was able to comprehend my condition better and manage my well-being more effectively.”
Dr. Jason Shumard’s Functional Medicine Approach emphasizes the effectiveness of a holistic strategy in managing such conditions, enabling individuals to take charge of their well-being through personalized nutrition and lifestyle changes. Monitoring progress through techniques like fitness applications and journals, as well as establishing SMART objectives, can greatly improve individual involvement and responsibility in their wellness journey.
Healthcare professionals are encouraged to stay informed about the latest expert opinions and articles on the DKA protocol for symptom recognition, as this knowledge is vital for delivering high-quality care. As Dr. Shumard states, “By providing individuals with actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being, ultimately leading to improved quality of life and reduced reliance on conventional medical interventions.” By promoting a culture of awareness and education, providers can greatly influence the handling of diabetic ketoacidosis through the DKA protocol and enhance the overall quality of life for those they serve.
Diagnostic Criteria and Laboratory Findings for DKA
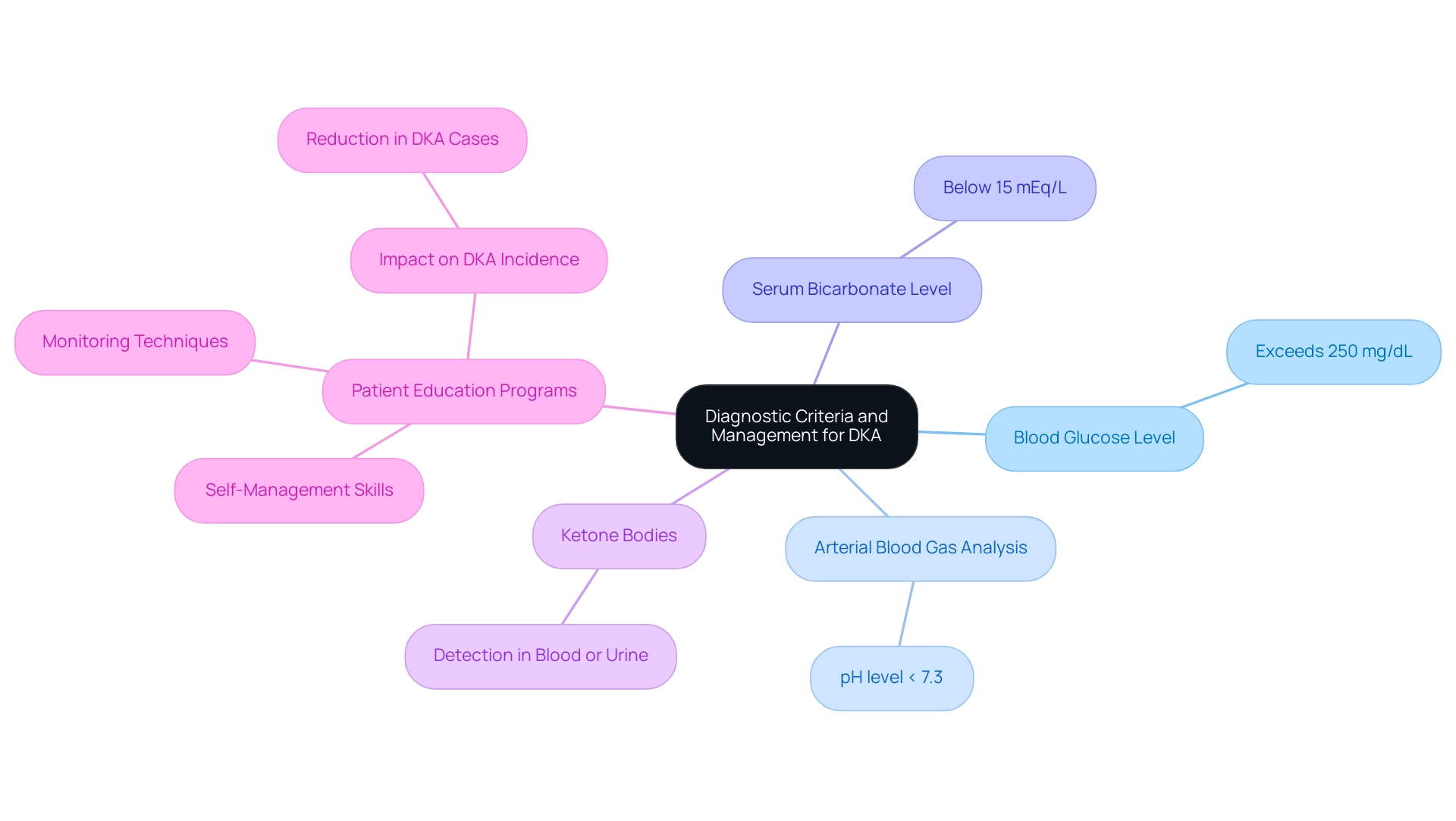
To accurately diagnose Diabetic Ketoacidosis (DKA), healthcare providers must assess several critical criteria:
- Blood Glucose Level: A hallmark of DKA is a blood glucose level typically exceeding 250 mg/dL, indicating significant hyperglycemia.
- Arterial Blood Gas Analysis: A pH level of less than 7.3 signifies acidosis, a key indicator of DKA.
- Serum Bicarbonate Level: Levels falling below 15 mEq/L further confirm the presence of metabolic acidosis associated with DKA.
- Ketone Bodies: The detection of ketone bodies in either blood or urine is essential for establishing the diagnosis.
These laboratory findings are not only pivotal for confirming DKA but also for distinguishing it from other hyperglycemic emergencies, such as Hyperglycemic Hyperosmolar State (HHS). It’s important to recognize that the precise interpretation of these results is vital for starting the appropriate DKA protocol, as it can significantly influence outcomes.
Many patients find that understanding the severity of their condition is crucial. Recent statistics indicate that typical free water loss in DKA can reach approximately 6 liters, or nearly 100 mL/kg of body weight. Furthermore, educational programs focused on diabetes management, such as those provided at Dr. Jason Shumard’s Integrative Wellness Center, have shown effectiveness in lowering the incidence of DKA by empowering individuals with self-management skills. These programs instruct individuals on how to track blood glucose levels and modify insulin during times of illness or stress, promoting a sense of control over their well-being.
As Dr. Jason Shumard states, “By providing individuals with actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being, ultimately leading to improved quality of life and reduced reliance on conventional medical interventions.” This proactive approach not only enhances safety but also aligns with the holistic philosophy of care emphasized at Dr. Shumard’s center. It reinforces the importance of personalized care and education in managing the DKA protocol effectively.
Step-by-Step Management of DKA: Protocol Implementation
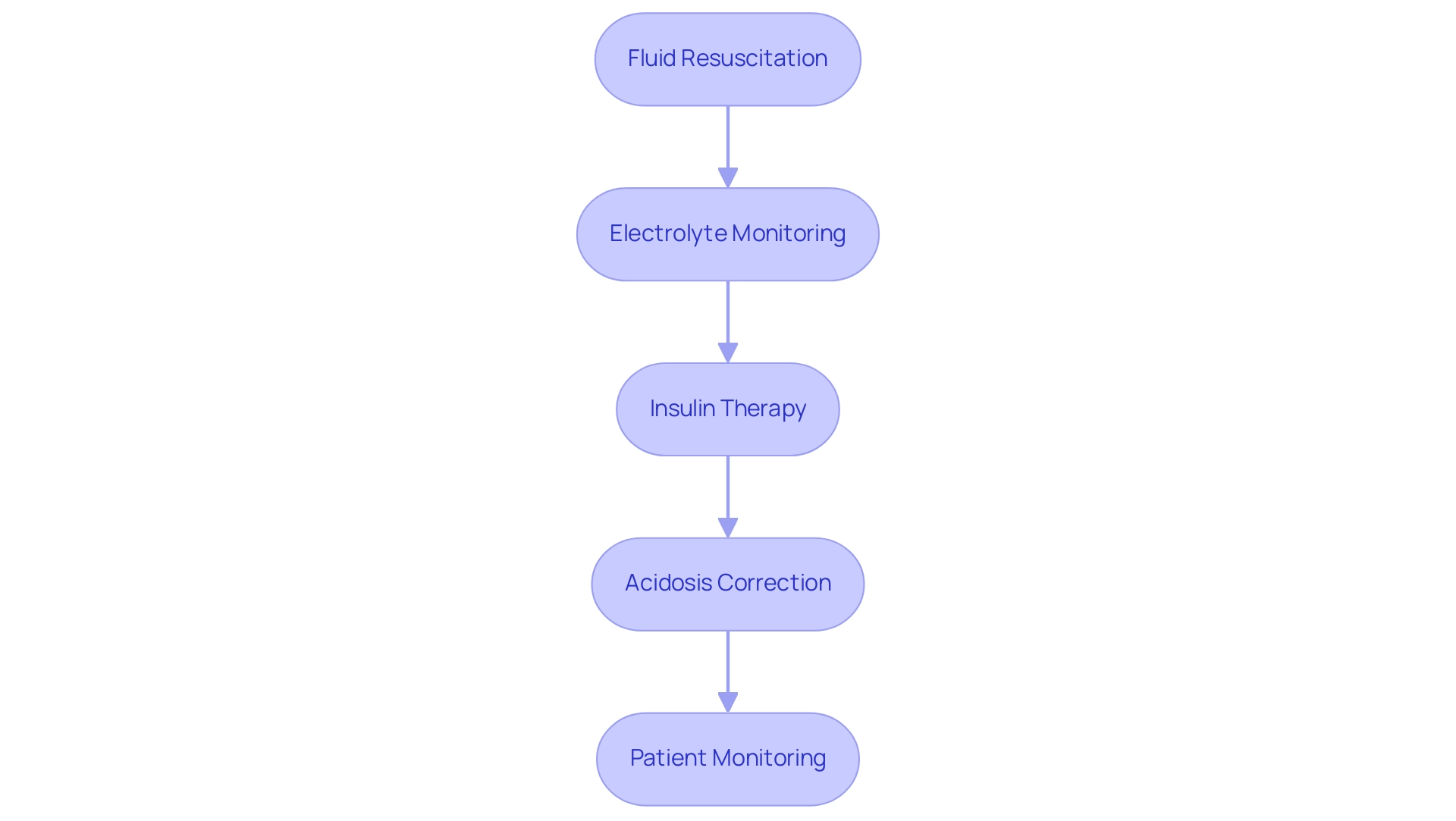
Effective management of the DKA protocol is crucial for stabilizing individuals and preventing complications. Let’s explore a step-by-step protocol that outlines the essential components of DKA treatment:
-
Fluid Resuscitation: It’s important to initiate treatment with isotonic saline (0.9% NaCl) at a rate of 15-20 mL/kg/h to address dehydration. This step is vital, as adequate fluid replacement can significantly enhance outcomes for individuals. Recent studies indicate that timely fluid resuscitation is particularly effective in improving outcomes for those with DKA, reinforcing the need for adherence to the DKA protocol.
-
Electrolyte Monitoring: Close monitoring of potassium levels is essential, as hypokalemia may develop due to insulin therapy. Regular assessments help in timely interventions to prevent cardiac complications. Many patients find that understanding these changes can alleviate some of their concerns.
-
Insulin Therapy: Starting a continuous intravenous insulin infusion is key to effectively lowering blood glucose levels and suppressing ketone production. This approach is supported by recent guidelines emphasizing the importance of insulin in DKA management. Notably, phosphate therapy did not change the duration of DKA or insulin dosage required in a study involving 44 individuals, highlighting the need for careful consideration of treatment options.
-
Acidosis Correction: Regularly monitoring arterial blood gases and bicarbonate levels is crucial in evaluating the resolution of acidosis. This assessment is critical in determining the effectiveness of the DKA protocol for treatment.
-
Patient Monitoring: Continuous monitoring of vital signs, blood glucose, and electrolytes is necessary to adjust treatment as needed. This vigilant approach helps in identifying any potential complications early, providing peace of mind.
Incorporating these steps systematically not only stabilizes the individual but also enhances the likelihood of a successful recovery. Additionally, integrating effective strategies for progress tracking and goal setting can empower individuals in managing their diabetes. Utilizing methods such as SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost focus and motivation in their wellness management journey.
For instance, an individual might set a goal to reduce their blood glucose levels by a certain percentage within a specified timeframe, fostering accountability and engagement in their treatment plan. To further enhance progress tracking, individuals can utilize various methods such as fitness apps, journals, and pedometers to monitor their daily activities and health metrics.
Case studies highlight that addressing precipitating factors, such as infections, is crucial in managing DKA effectively. Infections are common triggers for DKA in both new-onset and established diabetes individuals, and prompt identification and treatment of these underlying infections can lead to better outcomes and prevention of recurrence.
As Charles “Chuck” Henderson, the ADA’s chief executive officer, stated, “Improving the lives of people affected by diabetes is a key part of the ADA’s mission.” By adhering to these best practices and integrating structured goal-setting, healthcare providers can ensure a higher quality of care for individuals experiencing the DKA protocol, ultimately contributing to the broader objective of enhancing diabetes care.
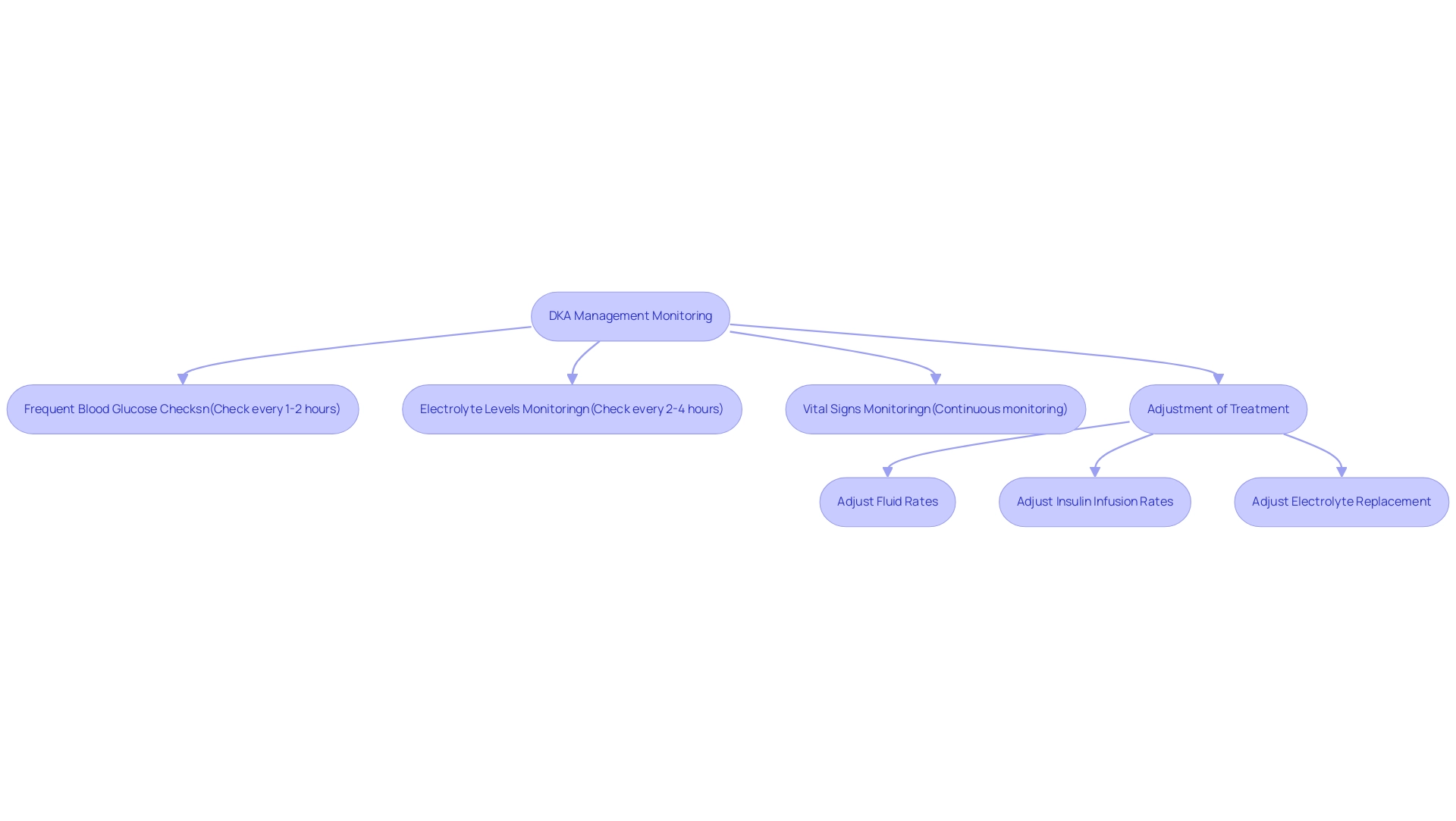
Monitoring and Adjusting Treatment in DKA Management
Monitoring during the management of diabetic ketoacidosis (DKA) is crucial for ensuring safety and optimizing treatment outcomes according to the DKA protocol. It’s important to recognize that effective monitoring can make a significant difference in the lives of those affected. Key components of this vital process include:
-
Frequent Blood Glucose Checks: Blood glucose levels should be monitored every 1-2 hours to inform insulin dosing accurately. This frequent assessment is vital, as individuals with DKA face a 1.55 times greater risk of stroke compared to those without the condition, underscoring the need for vigilant monitoring.
-
Electrolyte Levels: Potassium levels must be checked every 2-4 hours, particularly during the initial treatment phase. Many patients find that electrolyte imbalances are common in DKA, making timely adjustments essential to prevent complications.
-
Vital Signs: Continuous monitoring of heart rate, blood pressure, and respiratory rate is necessary to detect any signs of deterioration. This proactive approach enables healthcare providers to respond swiftly to any changes in the individual’s condition, ensuring they feel supported throughout their care journey.
-
Adjustment of Treatment: It is imperative to be prepared to adjust fluid rates, insulin infusion rates, and electrolyte replacement based on the individual’s response. This dynamic approach is essential for effective management within the DKA protocol. Case studies illustrate that meticulous discharge planning and education greatly decrease recurrences of DKA. Dr. Jason Shumard highlights, “By offering individuals with actionable insights and practical tools, the center cultivates a setting where people can regain their wellness and well-being.”
In 2025, current recommendations emphasize the importance of an interprofessional team in managing DKA, including triage nurses, intensivists, endocrinologists, and social workers. This collaborative effort is particularly advantageous for individuals encountering socioeconomic challenges, ensuring comprehensive care that addresses both medical and social needs.
To further enable individuals in their health oversight, incorporating effective strategies for progress tracking and goal setting is essential. Utilizing methods such as SMART goals—specific, measurable, attainable, relevant, and time-bound—can enhance engagement and motivation. For example, individuals may establish a goal to track their blood glucose levels regularly or to reach a particular objective in their dietary control.
By prioritizing structured goal-setting and consistent progress tracking, individuals can cultivate a sense of achievement and maintain engagement in their health management journey. The case study titled ‘Enhancing Healthcare Team Outcomes for DKA Protocol’ illustrates how coordinated care under the DKA protocol can lead to improved results for individuals, reinforcing the center’s commitment to personalized care and education. By implementing these monitoring protocols and adjustments, healthcare providers can enhance health outcomes and foster a supportive environment for recovery.
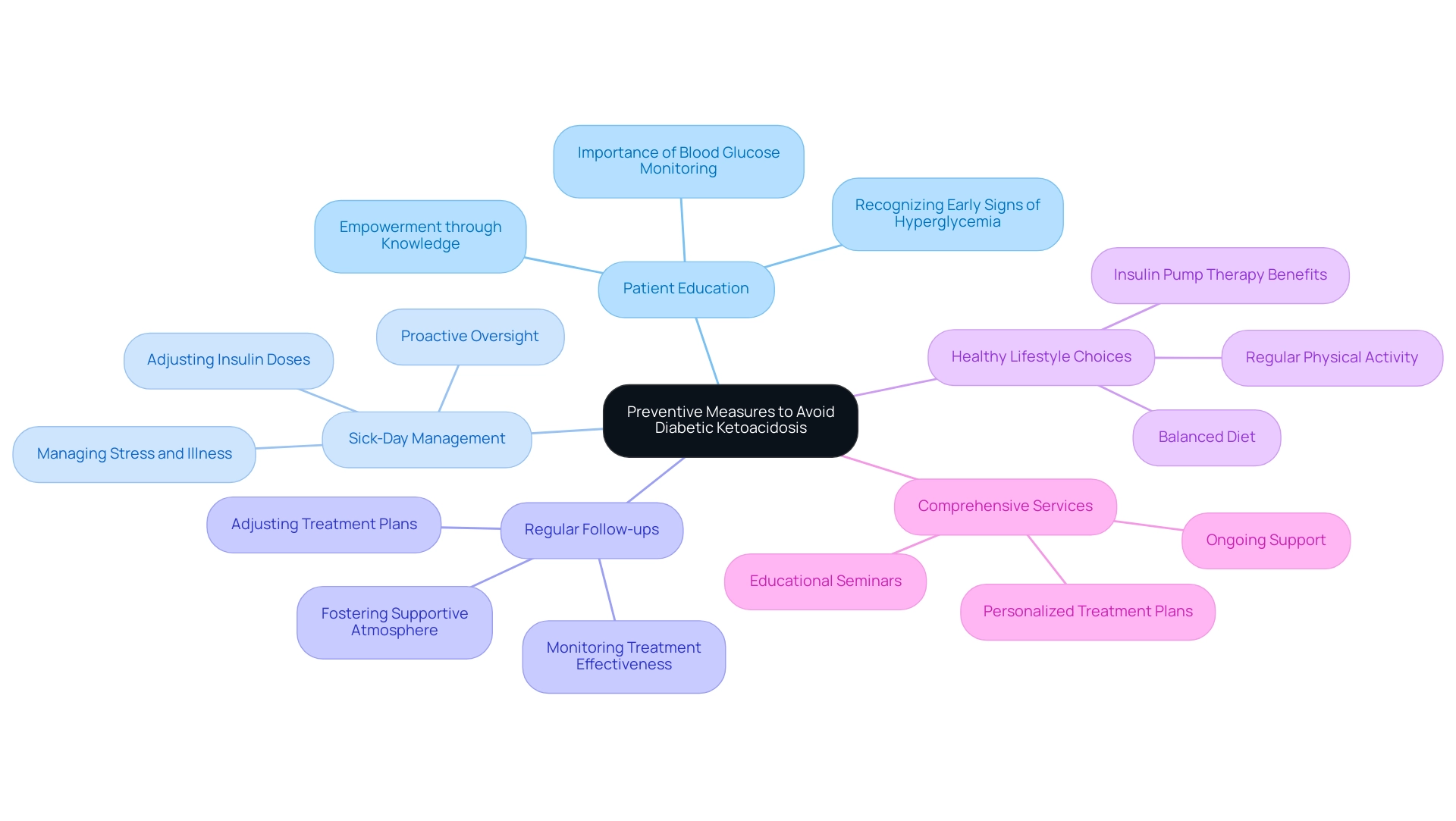
Preventive Measures to Avoid Diabetic Ketoacidosis
Preventive measures for Diabetic Ketoacidosis (DKA) are essential in managing diabetes effectively and minimizing the risks associated with this serious condition. It’s important to recognize that implementing key strategies can make a significant difference in your health journey.
-
Patient Education: Empowering patients through education is vital. Teaching the significance of regular blood glucose monitoring and recognizing early signs of hyperglycemia can lead to timely interventions, significantly reducing the risk of DKA. Many individuals find that being knowledgeable helps them feel more in control of their health, leading to enhanced wellness results. Dr. Jason Shumard highlights, “By offering individuals actionable insights and practical tools, the center cultivates a setting where people can regain their wellness and well-being.” This approach resonates in testimonials from those who have transformed their health journeys, underscoring the importance of understanding their condition and taking proactive steps.
-
Sick-Day Management: Many patients find that knowing how to adjust their insulin doses during periods of illness or stress is crucial. This proactive approach is essential in preventing the DKA protocol, as stress and illness can lead to fluctuations in blood glucose levels. Effective sick-day oversight can be a game-changer in preserving stability during difficult times, as observed by individuals who have successfully navigated these situations with support from Dr. Shumard’s team.
-
Regular Follow-ups: Routine check-ups are critical for monitoring diabetes management. These follow-ups allow healthcare providers to evaluate treatment effectiveness and make necessary adjustments, ensuring that individuals stay aligned with their wellness objectives. Consistent interaction with healthcare professionals fosters a supportive atmosphere for patients, as demonstrated by success stories where ongoing assistance has led to considerable wellness improvements.
-
Healthy Lifestyle Choices: Encouraging a balanced diet and regular physical activity is fundamental in maintaining stable blood glucose levels. Lifestyle modifications not only contribute to overall health but also play a significant role in the DKA protocol for prevention. Patients who adopt healthier habits often experience better control over their diabetes. Notably, insulin pump therapy has been associated with lower risks of severe DKA and hypoglycemia, highlighting the importance of effective management strategies. Numerous individuals have shared transformative outcomes after embracing these holistic methods, reinforcing the center’s commitment to individualized care.
-
Comprehensive Services: The Integrative Wellness Center offers a variety of services tailored to meet the distinct needs of individuals with type 2 diabetes. These encompass personalized treatment plans, educational seminars, and ongoing support, empowering individuals to take charge of their health. By incorporating these services into their care, individuals can better manage their diabetes and reduce the risk of complications like those outlined in the DKA protocol.
By embracing these strategies, healthcare providers can significantly reduce the risk of the DKA protocol among those they care for. The incorporation of individual education, proactive oversight during illness, consistent follow-ups, and encouragement of healthy lifestyle choices establishes a comprehensive strategy for diabetes care. This holistic methodology aligns with the innovative practices championed by Dr. Jason Shumard, who emphasizes the importance of empowering individuals with knowledge and tools for effective health management.
A case study titled “Dr. Jason Shumard’s Functional Medicine Approach” illustrates how patient education and empowerment lead to life-changing outcomes, reinforcing the importance of the discussed preventive measures.
Conclusion
Understanding and managing Diabetic Ketoacidosis (DKA) is essential for both healthcare providers and patients navigating the complexities of diabetes. It’s important to recognize that DKA can be overwhelming, but with the right knowledge and support, individuals can effectively manage their health. This article highlights the critical components of DKA, including its causes, symptoms, diagnostic criteria, and step-by-step management protocols. Recognizing early signs such as excessive thirst, frequent urination, and fruity-smelling breath can lead to timely interventions, ultimately improving patient outcomes.
Many patients find that effective management requires a collaborative approach involving an interprofessional team to ensure comprehensive care. Fluid resuscitation, insulin therapy, and vigilant monitoring of blood glucose and electrolytes are integral to stabilizing patients. Moreover, patient education and proactive strategies, such as sick-day management and regular follow-ups, empower individuals to take control of their health, reducing the risk of DKA.
In conclusion, a thorough understanding of DKA, coupled with personalized care and ongoing education, can significantly mitigate its risks. By fostering an environment of awareness and support, healthcare providers can inspire patients to reclaim their health and enhance their quality of life. The commitment to innovative, holistic approaches in diabetes management serves as a beacon of hope for those affected by this serious condition, reinforcing the importance of collaboration, education, and proactive health management. Together, we can navigate this journey toward better health, ensuring that no one has to face it alone.