Overview
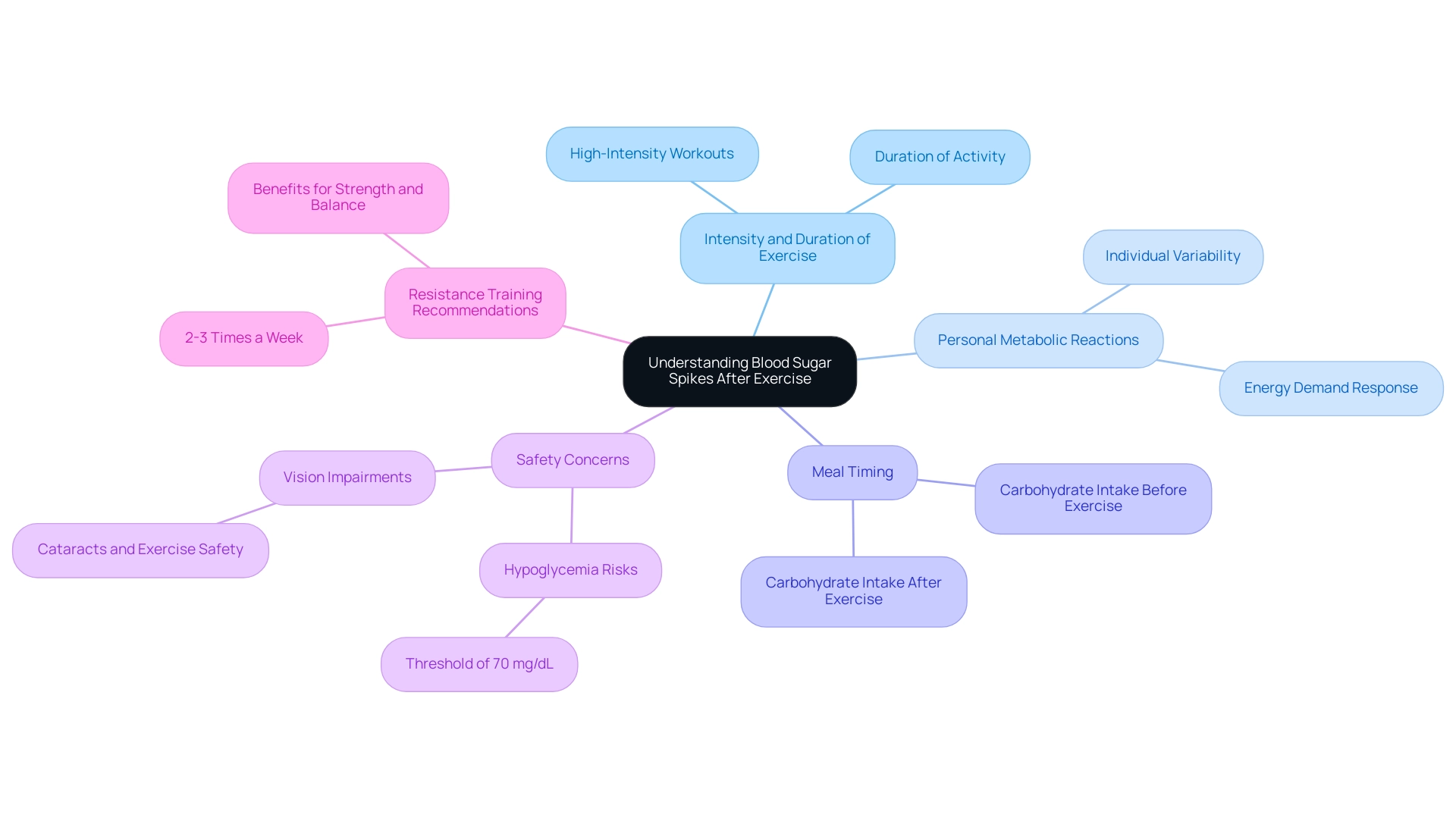
Blood sugar levels can rise after exercise due to various factors, including the intensity of the workout, individual metabolic responses, and nutritional timing. The article explains that high-intensity activities can stimulate glucose production and release hormones that elevate blood sugar, while inadequate meal planning can exacerbate these fluctuations, emphasizing the importance of tailored exercise and dietary strategies for effective diabetes management.
Introduction
Navigating the complexities of blood sugar management during and after exercise is particularly crucial for individuals living with type 2 diabetes. While physical activity is a cornerstone of effective diabetes management, it can also lead to unexpected spikes in blood glucose levels.
Understanding the interplay between exercise intensity, nutritional strategies, and individual physiological responses is essential for optimizing health outcomes. From the hormonal responses triggered by high-intensity workouts to the critical timing of meals, a comprehensive approach to managing blood sugar can empower individuals to take control of their diabetes.
This article delves into the multifaceted relationship between exercise and blood sugar levels, providing insights and practical strategies to help those affected make informed decisions for their health.
Understanding Blood Sugar Spikes After Exercise
Individuals managing type 2 diabetes face a significant challenge because after exercise blood sugar goes up. Although physical activity is widely acknowledged for its role in improving glucose regulation, various factors can result in a situation where after exercise blood sugar goes up. The intensity and duration of the activity are primary considerations; for instance, after exercise blood sugar goes up, as high-intensity workouts may provoke a more pronounced glucose response due to the body’s increased demand for energy.
Moreover, personal metabolic reactions can differ significantly, which may explain why after exercise blood sugar goes up, individuals can experience varying outcomes in glucose levels. The timing of meals relative to exercise is crucial, as inadequate carbohydrate intake before or after physical activity can contribute to fluctuations in glucose levels, particularly since after exercise blood sugar goes up. It is crucial for individuals to recognize that if glucose levels fall to 70 mg/dL (3.9 mmol/L) or below, they should cease exercising to avoid hypoglycemia.
Research indicates that understanding these elements is essential for diabetes management, particularly because after exercise blood sugar goes up. Individuals can make informed decisions regarding their fitness routines, ensuring they optimize their health while minimizing the risk of adverse effects, particularly because after exercise blood sugar goes up. Participating in resistance training 2-3 times a week on nonconsecutive days can enhance strength, balance, and daily living activities, which is advantageous for overall health and glycemic control.
As mentioned by O. Peter Adams from the Faculty of Medical Sciences, HIE is unlikely to cause hypoglycemia during and right after physical activity, particularly because after exercise blood sugar goes up, emphasizing the significance of customized activity strategies in managing blood sugar levels. Furthermore, it’s essential for individuals with diabetes to consider safety concerns, such as the effect of cataracts on their capability to engage in physical activity, as diminished vision may require avoiding specific tasks.
Physiological Mechanisms Behind Elevated Blood Sugar Levels
During physical activity, the body responds to increasing demands by releasing hormones, particularly adrenaline and cortisol. These hormones play a crucial role in stimulating glucose production in the liver and facilitating the release of stored glucose into the bloodstream. This physiological reaction can lead to increased glucose levels, particularly because after exercise blood sugar goes up, especially during high-intensity exercise.
Studies show that the kind of physical activity undertaken greatly affects these sugar level variations. For instance, anaerobic activities, such as weight lifting and sprinting, are more likely to cause a spike in blood glucose levels, indicating that after exercise blood sugar goes up compared to moderate aerobic activities like walking or cycling. It’s crucial to acknowledge that individuals with type 2 conditions may also encounter psychological obstacles to physical activity, as the strong link between complications and depression can reduce the drive to participate in movement.
Addressing the anxiety that accompanies the concern surrounding potential complications of this condition is crucial, as it can empower patients to take control of their health. Comprehending these physiological processes is essential for individuals controlling type 2 conditions, as it enables them to foresee and efficiently regulate their blood sugar levels, particularly because after exercise blood sugar goes up, concerning their physical activity routines. As mentioned by Dr. Salwa J. Zahalka, MD, ‘These findings highlight the intricacy of the pathophysiology involved in physical activity and the influence that metabolic disorders have on these processes.’
Recent studies, including the Apple Heart and Movement Study in collaboration with the Apple Women’s Health Study, further illuminate the relationship between physical activity, activity intensity, and hormonal responses. This understanding enables patients to enhance their physical activity for improved glucose management, in accordance with a comprehensive strategy that tackles the underlying factors of the condition. A holistic regimen that focuses on lifestyle changes, including diet and stress management, can significantly improve overall health outcomes.
Furthermore, if hypoglycemia impacts physical activity routines, individuals should seek guidance from their healthcare provider for a customized treatment plan to ensure safe and effective management of their condition during physical engagement.
The Role of Nutrition and Timing of Meals
Nutrition is a vital element in regulating glucose levels, particularly in relation to physical activity for those with type 2 diabetes. Consuming carbohydrates prior to a workout is important for providing energy; however, if not paired with adequate protein and healthy fats, it can lead to elevated post-exercise glucose levels. Research indicates a noteworthy likelihood ratio chi square for blood glucose response at 31.47, with a p-value of less than 0.01, underscoring the importance of nutritional strategies in blood glucose management.
Furthermore, for individuals with type 1 diabetes, balancing insulin doses with food intake and activity is crucial, providing a broader perspective on diabetes management. The timing of meals also plays a crucial role; eating too close to workout time may exacerbate glucose levels during and contribute to the phenomenon where after exercise blood sugar goes up. To enhance glucose regulation, individuals should strive to eat a well-balanced meal a few hours prior to exercising.
Tracking glucose levels before, during, and after physical activity is essential, especially since after exercise blood sugar goes up, allowing for the modification of nutritional intake to create an effective routine. A relevant case study titled “Measurements and Outcomes” demonstrates this by monitoring capillary glucose levels at various intervals after carbohydrate consumption to assess the primary outcome of postprandial glucose response. Recent findings suggest that increasing protein intake post-exercise can further mitigate the risk of hypoglycemia and enhance recovery, aligning with established sports nutrition guidelines.
Sheila Williams, an Associate Professor, stresses the significance of these strategies, stating, “The combination of nutrition and physical activity is essential for effective glucose management,” which supports the statistical analysis highlighted in this discussion.
Individual Variability in Blood Sugar Responses
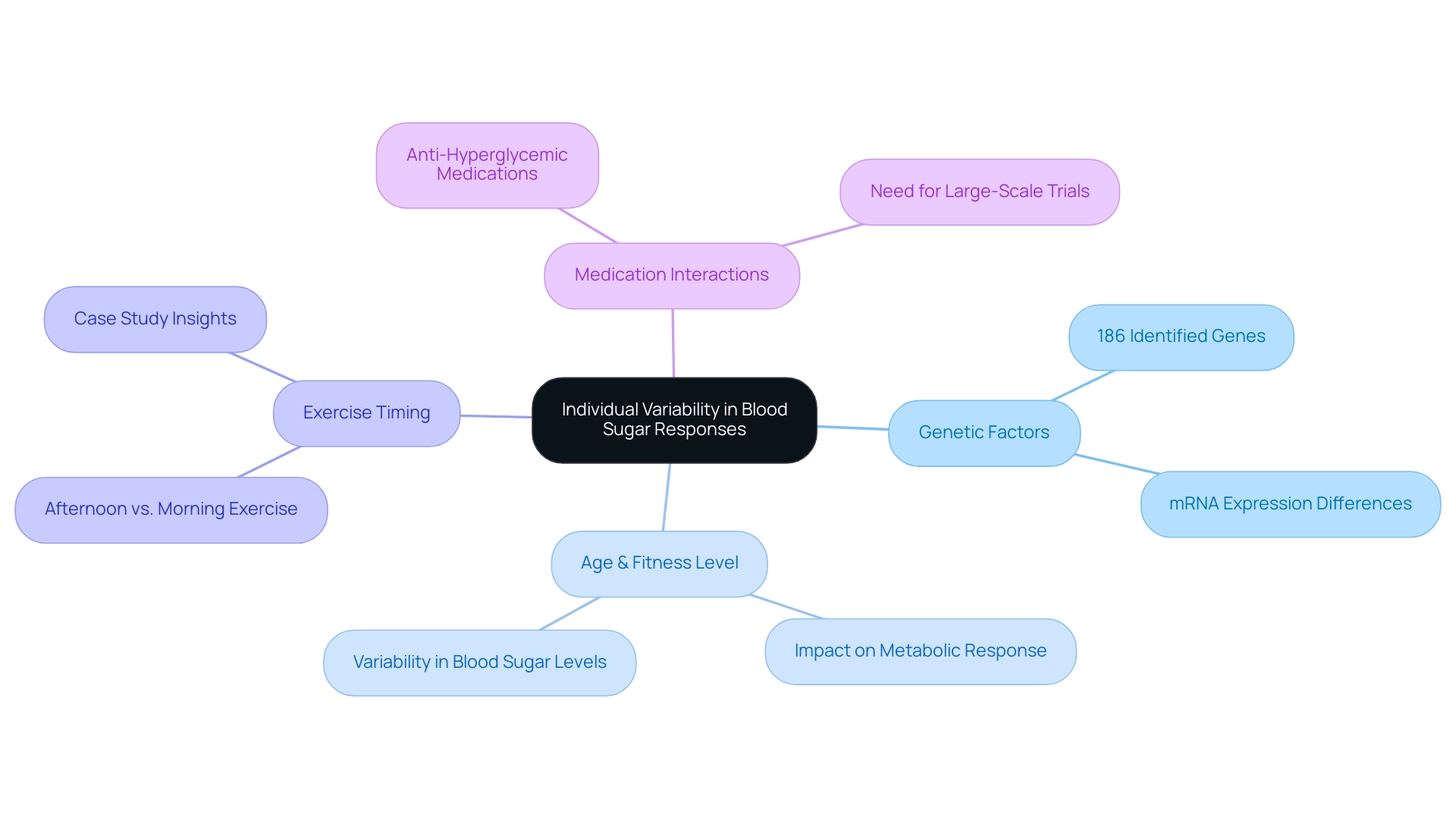
Individual variability is a fundamental factor influencing blood sugar responses to exercise, particularly in individuals managing Type 2 Diabetes Mellitus (T2DM). A holistic approach, addressing the root causes of the illness and re-examining these sources, empowers patients to take charge of their health while potentially reducing anxiety surrounding the complications of their condition. Research has identified 186 genes with differential mRNA expressions between ‘responders’ and ‘non-responders’, suggesting a genetic basis for these variations.
Factors such as age, fitness level, and the use of diabetes medications can significantly impact the metabolic response to physical activity. For instance, while some individuals may experience a significant spike in sugar levels after exercise (blood sugar goes up following high-intensity workouts), others might see a decrease in glucose levels under similar conditions. Praet SF notes,
Time spent hyperglycemic was significantly lower during the subsequent 24 h following physical activity,
indicating the potential benefits of physical activity on glucose management post-activity.
A case study, Impact of Exercise Timing on Glucose Levels in T2DM Patients, further illustrates this; it demonstrated that participants who engaged in afternoon aerobic sessions exhibited notable improvements in their mean glucose levels compared to those who exercised in the morning. This emphasizes the significance of customizing fitness strategies to personal physiological reactions, ultimately enabling individuals to control their condition effectively. Furthermore, comprehending the public health consequences of this condition in the 21st century, as mentioned in a Lancet article, highlights the essential requirement for efficient blood sugar management techniques through physical activity.
Moreover, acknowledging the existing evidence gaps concerning the interactions between anti-hyperglycemic medications and physical activity emphasizes the need for large-scale prospective trials to guide clinical guidelines. By considering these factors, including the reduction of anxiety related to complications of blood sugar issues, individuals can better navigate their physical activity routines and optimize their health management within a holistic framework.
Strategies for Managing Blood Sugar Levels During and After Exercise
Maintaining glucose levels effectively during and after exercise is essential for individuals with type 2 conditions, particularly because after exercise blood sugar goes up, which can lead to anxiety regarding possible complications of the illness. A holistic approach begins by re-examining the source of your diabetes, allowing for comprehensive health management at the root level. Ongoing glucose monitoring is among the most efficient techniques, offering real-time tracking of glucose level variations.
As mentioned by the Mayo Clinic Staff, ‘And it can help prevent glucose fluctuations that could be harmful.’ This technology provides valuable insights for prompt interventions, ensuring stable glucose levels. Additionally, adjusting carbohydrate intake before and after physical activity is significant; for instance, each glucose tablet contains 4 grams of carbohydrate, serving as a practical reference for managing these levels.
Incorporating a blend of aerobic and resistance training is essential, as resistance training of any intensity is recommended to improve strength, balance, and daily living activities. Furthermore, remaining sufficiently hydrated is essential, as dehydration can result in heightened glucose spikes, especially after exercise blood sugar goes up. By implementing these strategies within a holistic framework, such as setting specific goals for carbohydrate intake and exercise types, individuals can optimize their exercise routines and achieve better blood sugar management, especially since after exercise blood sugar goes up, empowering their health effectively.
Conclusion
Understanding and managing blood sugar levels during and after exercise is vital for individuals with type 2 diabetes. The interplay between exercise intensity, nutritional strategies, and individual physiological responses directly impacts blood glucose control. High-intensity workouts can lead to increased blood sugar spikes due to hormonal responses, while the timing and composition of meals play a critical role in stabilizing these levels.
Moreover, recognizing individual variability in metabolic responses highlights the importance of personalized exercise and nutrition plans. Factors such as genetics, age, and medication usage can significantly influence how one’s body reacts to physical activity. By leveraging continuous glucose monitoring and tailoring exercise routines to individual needs, individuals can better manage their diabetes and enhance their overall health.
In conclusion, adopting a comprehensive approach that integrates exercise, nutrition, and personal health factors is essential for effective diabetes management. With informed strategies and an understanding of their body’s responses, individuals can take proactive steps to optimize their health outcomes, ensuring that exercise becomes a beneficial component of their diabetes management plan.
Frequently Asked Questions
Why do individuals managing type 2 diabetes experience an increase in blood sugar after exercise?
After exercise, blood sugar levels can rise due to various factors, including the intensity and duration of the activity, which can provoke a pronounced glucose response as the body demands more energy.
What role do hormones play in blood sugar levels during physical activity?
During physical activity, hormones like adrenaline and cortisol are released, stimulating glucose production in the liver and the release of stored glucose into the bloodstream, which can lead to increased blood sugar levels.
How does the type of physical activity affect blood sugar levels?
The kind of physical activity significantly impacts blood sugar variations; anaerobic activities like weight lifting and sprinting are more likely to cause spikes in blood glucose compared to moderate aerobic activities like walking or cycling.
What should individuals with diabetes do if their glucose levels drop to 70 mg/dL (3.9 mmol/L) or below?
Individuals should cease exercising to avoid hypoglycemia if their glucose levels fall to 70 mg/dL (3.9 mmol/L) or below.
How can meal timing influence blood sugar levels in relation to exercise?
The timing of meals relative to exercise is crucial; inadequate carbohydrate intake before or after physical activity can contribute to fluctuations in glucose levels.
What are some recommended types of exercise for individuals with type 2 diabetes?
Engaging in resistance training 2-3 times a week on nonconsecutive days can enhance strength, balance, and daily living activities, which are beneficial for overall health and glycemic control.
What psychological factors might affect physical activity participation in individuals with type 2 diabetes?
Individuals may face psychological obstacles, such as anxiety and depression, which can reduce their motivation to engage in physical activity due to concerns about complications related to their condition.
What should individuals do if hypoglycemia impacts their physical activity routines?
Individuals should seek guidance from their healthcare provider for a customized treatment plan to ensure safe and effective management of their condition during physical engagement.