Overview
In the article titled “7 Key ADA Blood Glucose Guidelines for Effective Diabetes Management,” the central question revolves around the essential guidelines for managing blood glucose levels in those living with diabetes. It’s important to recognize that navigating diabetes can be challenging, and understanding these guidelines is crucial for effective management. The American Diabetes Association (ADA) emphasizes the significance of regular blood glucose monitoring, which includes both pre-meal and post-meal testing. Many patients find that this practice not only helps in tracking their condition but also fosters a sense of control over their health.
Moreover, the article highlights the importance of personalized care plans and lifestyle modifications. These tailored approaches can enhance overall health outcomes, offering support for individuals on their journey toward effective diabetes management. By focusing on what works best for each person, we can create a nurturing environment that promotes well-being and encourages positive changes. Remember, you are not alone in this journey; there are resources and communities ready to support you every step of the way.
Introduction
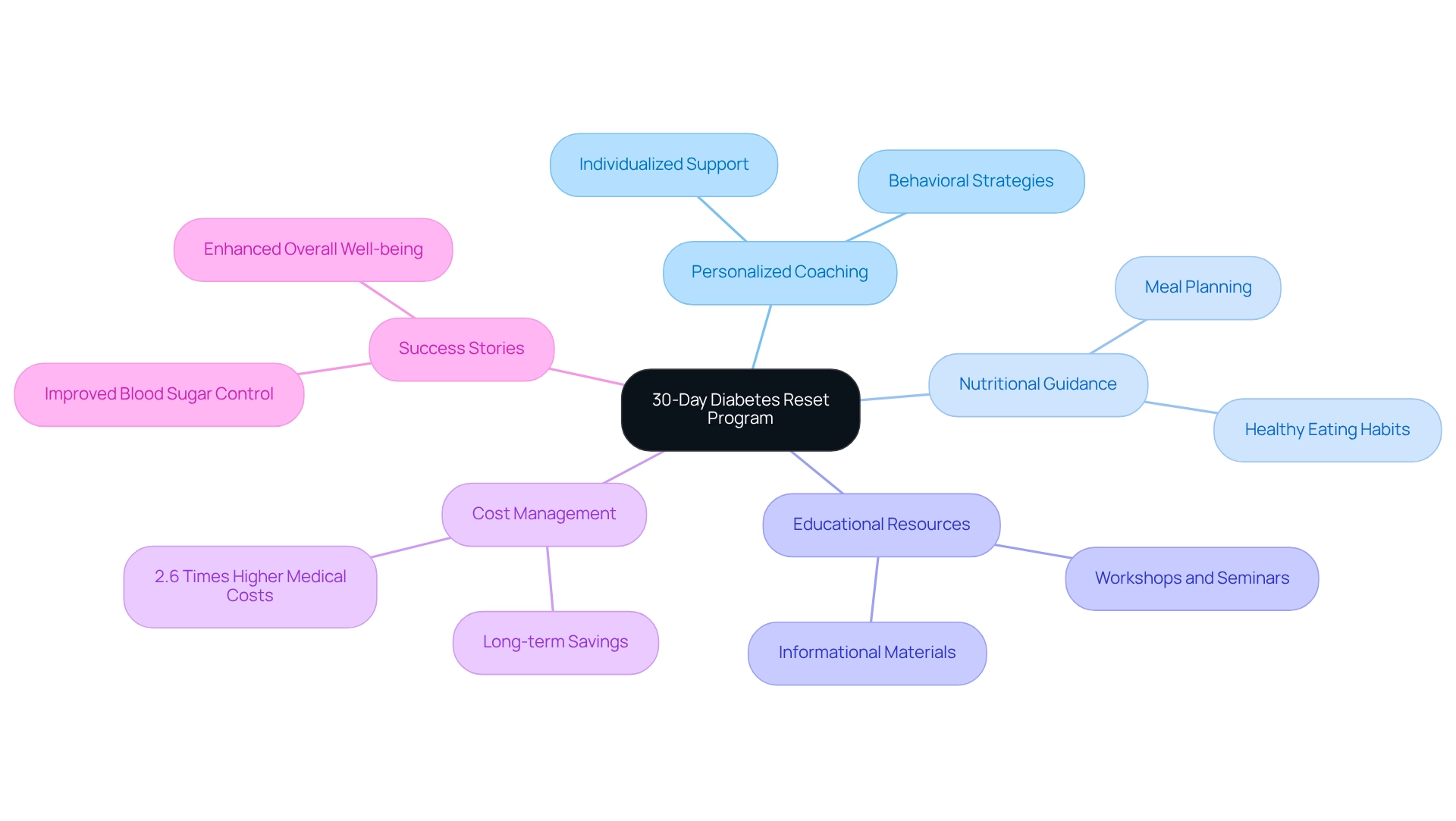
In the face of an escalating diabetes epidemic, effective management strategies have never been more crucial. It’s important to recognize that many individuals are struggling with the challenges of diabetes, and the Integrative Wellness Center’s 30-Day Diabetes Reset Program stands out as a beacon of hope. This program offers a comprehensive approach that empowers individuals to take charge of their health. By combining personalized coaching, nutritional guidance, and valuable educational resources, it not only addresses the symptoms of diabetes but also tackles its underlying causes.
As healthcare costs continue to rise, the need for sustainable solutions is paramount. Many patients find that success stories from participants who have experienced transformative changes serve as a powerful reminder of what is possible. This program exemplifies the growing recognition of personalized care in achieving lasting health improvements.
This article delves into the multifaceted strategies for managing diabetes, highlighting the importance of education, lifestyle modifications, and tailored care plans. Together, these elements pave the way for a healthier future, encouraging readers to reflect on their own journeys and consider the support available through the 30-Day Diabetes Reset Program.
Integrative Wellness Center: 30-Day Diabetes Reset Program for Effective Management
The 30-Day Diabetes Reset Program at the Integrative Wellness Center offers a compassionate approach to help patients manage their condition effectively. This program combines personalized coaching, nutritional guidance, and a wealth of educational resources, equipping participants with essential tools for sustainable health improvements. It’s important to recognize that by emphasizing lifestyle changes, individuals can gain a deeper understanding of their condition and implement strategies that foster long-term wellness.
Many patients find that managing diabetes can lead to overwhelming medical expenditures—statistics show they incur costs that are 2.6 times higher than those without the condition. This highlights the critical need for effective management. The 30-Day Diabetes Reset Program addresses this need by focusing on the underlying causes rather than merely managing symptoms, ultimately helping to reduce these costs through improved health outcomes. Access to better diabetes care is essential to limit complications associated with the disease, and this program exemplifies that commitment.
Success stories from participants truly illustrate the transformative impact of the program. Many report not only better blood sugar control but also enhanced overall well-being, thanks to the actionable insights and practical tools provided throughout the program. As Dr. Jason Shumard states, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being.” This personalized approach to diabetes management reflects a growing recognition of the importance of individualized care in achieving lasting health outcomes. It’s this nurturing philosophy that positions the Integrative Wellness Center as a leader in functional medicine for reversing type 2 diabetes and hypothyroidism.
American Diabetes Association: Key Blood Glucose Monitoring Guidelines
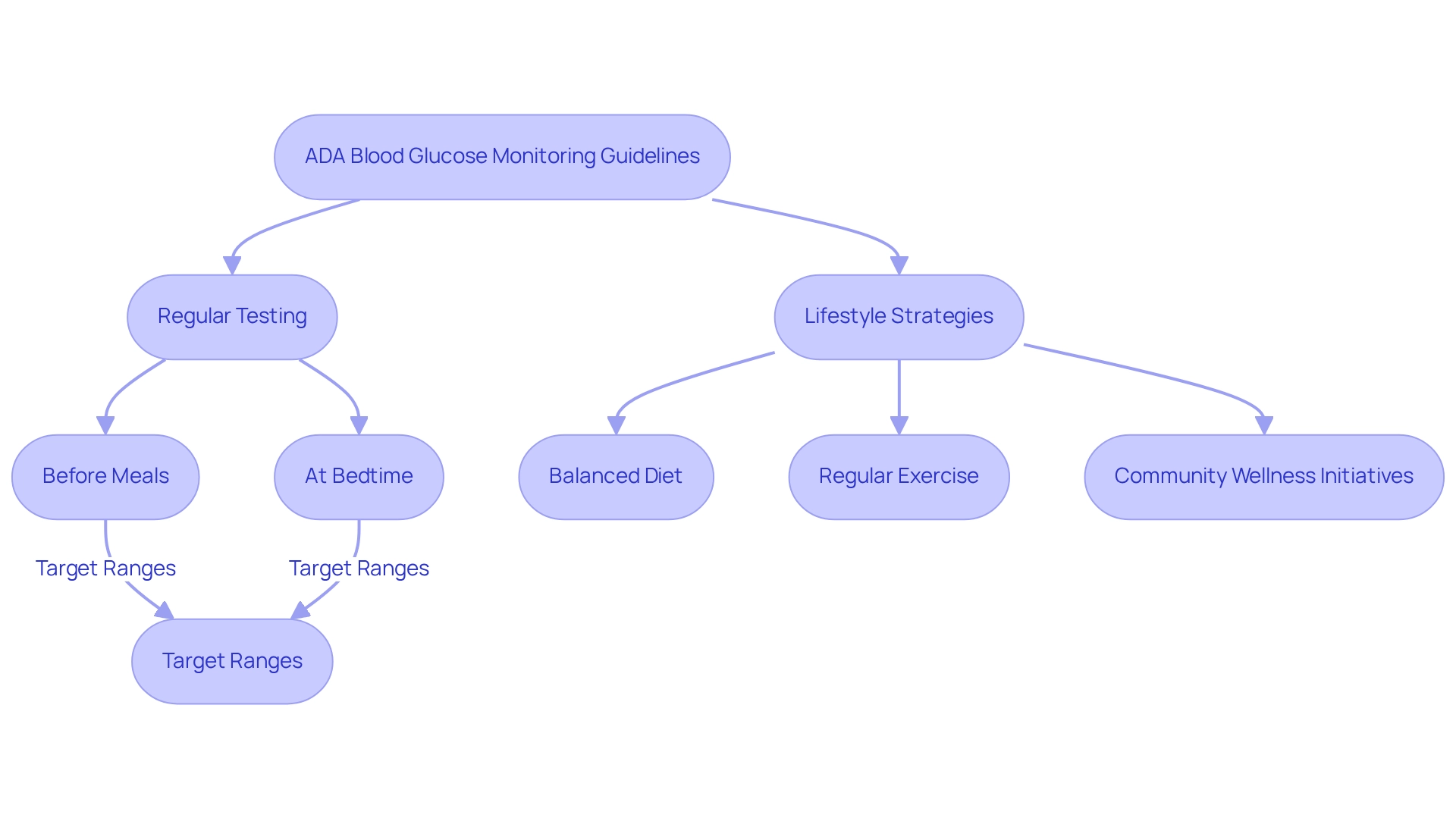
The American Diabetes Association (ADA) provides essential ADA blood glucose guidelines for glucose monitoring, emphasizing the importance of regular testing to achieve and maintain optimal sugar levels. It’s crucial to test before meals and at bedtime, with specific target ranges set for fasting and postprandial glucose levels. By adhering to these guidelines, individuals can make informed decisions about their diet and medication, which can greatly enhance health outcomes.
It’s important to recognize that incorporating holistic lifestyle strategies, such as those available in San Marcos, CA, can further improve the effectiveness of these monitoring practices. Adopting a balanced diet rich in local produce like avocados and berries, engaging in regular outdoor exercise, and participating in community wellness initiatives can all contribute to better sugar regulation. For example, the vibrant farmers’ markets in the area offer access to fresh, nutritious foods that support a diabetes-friendly diet, while the scenic parks and trails provide perfect settings for physical activity.
Many patients find that effective blood glucose monitoring is vital, as it plays a key role in managing their condition. The National Diabetes Statistics Report reveals a troubling increase in type 2 diabetes diagnoses, including 5,293 new cases among children and adolescents aged 10 to 19 years. This trend underscores the urgent need for proactive monitoring and management strategies, reinforcing the importance of the ADA blood glucose guidelines as an invaluable resource for individuals.
Experts in diabetes emphasize the significance of the ADA blood glucose guidelines. Regular glucose monitoring not only aids in immediate health management but also fosters long-term well-being. Monera Abdulkareem Alayuni, an MBBS, asserts, “Regular blood glucose testing is essential for effective management of the condition, as it enables individuals to comprehend their situation more clearly and make necessary adjustments to their treatment plans.” The ADA blood glucose guidelines for 2025 promote personalized monitoring strategies that take individual lifestyle factors into account, ensuring that everyone can effectively manage their condition.
Real-world examples show the success of these monitoring practices. Case studies reveal that individuals who consistently follow ADA guidelines report improved glycemic control and a stronger sense of empowerment in managing their condition. Furthermore, current research on self-monitoring glucose (SMBG) practices indicates that understanding the barriers and facilitators of sharing SMBG results can enhance management strategies. The study titled “Future Research Directions in SMBG Practices” highlights the need for further exploration of these factors, which could lead to more effective sharing practices and better patient outcomes.
In summary, the ADA blood glucose guidelines serve as a vital resource for individuals with diabetes, providing a framework for effective management. By combining these guidelines with comprehensive lifestyle modifications, such as those available in San Marcos, individuals can enhance their health management plan, leading to improved health outcomes and a better quality of life.
A1C Testing: Understanding Your Long-Term Blood Sugar Control
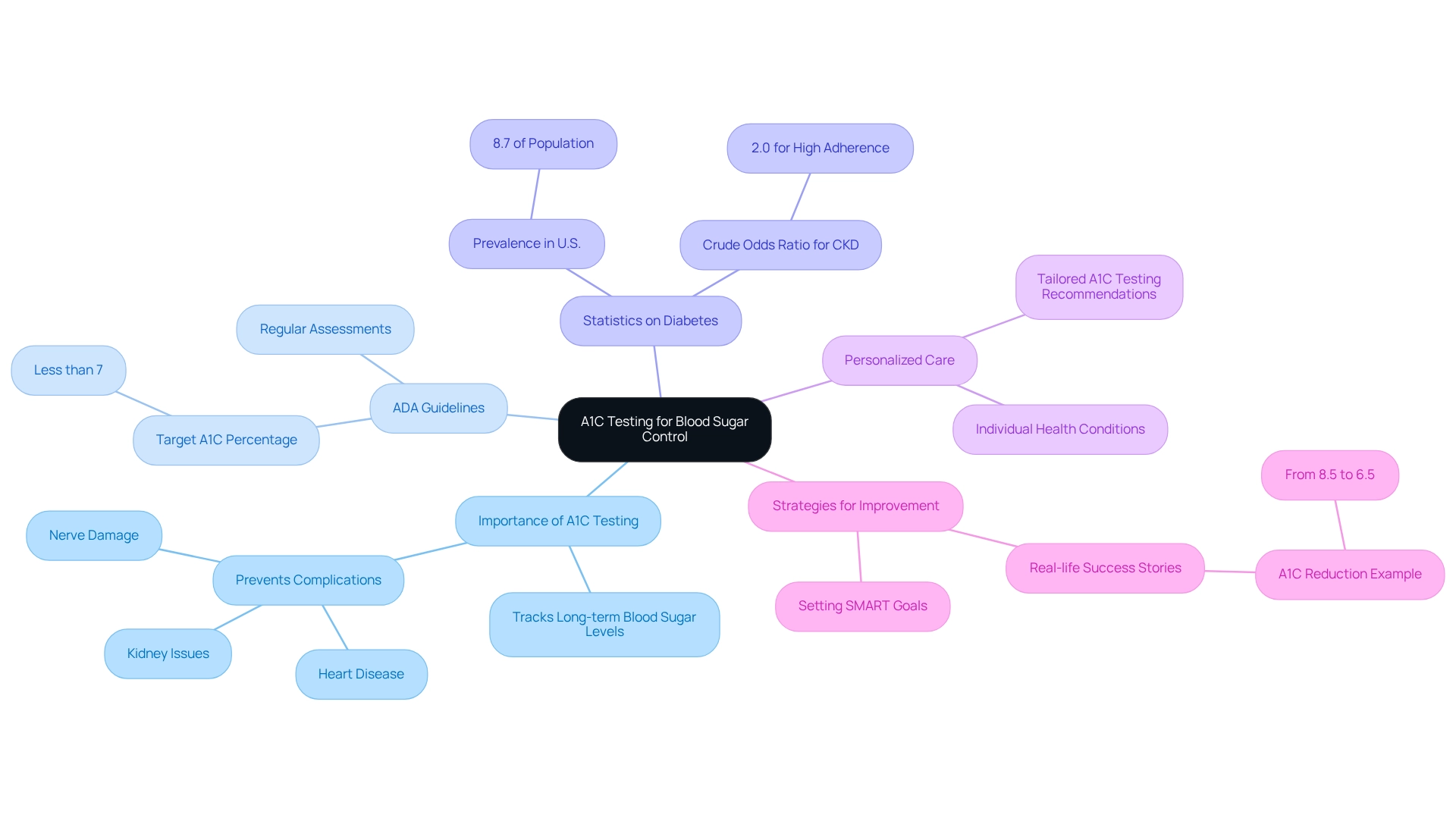
A1C testing serves as a vital tool for tracking long-term blood sugar management, helping you understand your average glucose levels over the past two to three months. The ADA blood glucose guidelines recommend that most adults with diabetes aim for an A1C target of less than 7%. This goal is crucial because maintaining A1C values within this range can significantly lower the risk of complications, such as heart disease, nerve damage, and kidney issues.
It’s important to recognize that regular A1C testing is essential for identifying trends in blood sugar levels. This enables timely adjustments to treatment plans and lifestyle choices. Statistics reveal that individuals who consistently adhere to A1C testing have a crude odds ratio of 2.0 for chronic kidney disease compared to those with lower adherence. This underscores the importance of regular monitoring, as it can help prevent serious complications related to diabetes.
In 2024, the National Diabetes Statistics Report highlighted that approximately 8.7% of the U.S. population is diagnosed with diabetes, with significant disparities evident across various demographics such as race, education, and income. Many patients find that tailored A1C testing recommendations and frequency can vary based on individual health conditions and treatment responses, which is why personalized care is so important.
Expert insights reinforce the significance of A1C testing in managing blood sugar effectively, as outlined in the ADA blood glucose guidelines. Endocrinologists advocate for regular assessments, emphasizing that achieving and maintaining target A1C levels according to the ADA blood glucose guidelines can lead to improved health outcomes and a better quality of life. Elizabeth Selvin, a professor in the Bloomberg School’s Department of Epidemiology, notes that “Trends in Diabetes Treatment and Control in United States Adults—1999-2018” illustrates the critical role of A1C monitoring in effective diabetes management.
Incorporating effective strategies for tracking progress can significantly enhance your engagement. For example, setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can foster accountability and motivation. Have you considered aiming to reduce your A1C by a certain percentage within a set timeframe? Real-life instances show the success of individuals who have effectively controlled their A1C measurements. One patient, after committing to regular A1C testing and making lifestyle changes, successfully reduced their A1C from 8.5% to 6.5%. This transformation highlights the positive impact of proactive health management. By prioritizing A1C testing and structured goal-setting, you can take meaningful steps toward better health and lessen your reliance on conventional medical interventions.
Fasting Blood Glucose Levels: What You Need to Know
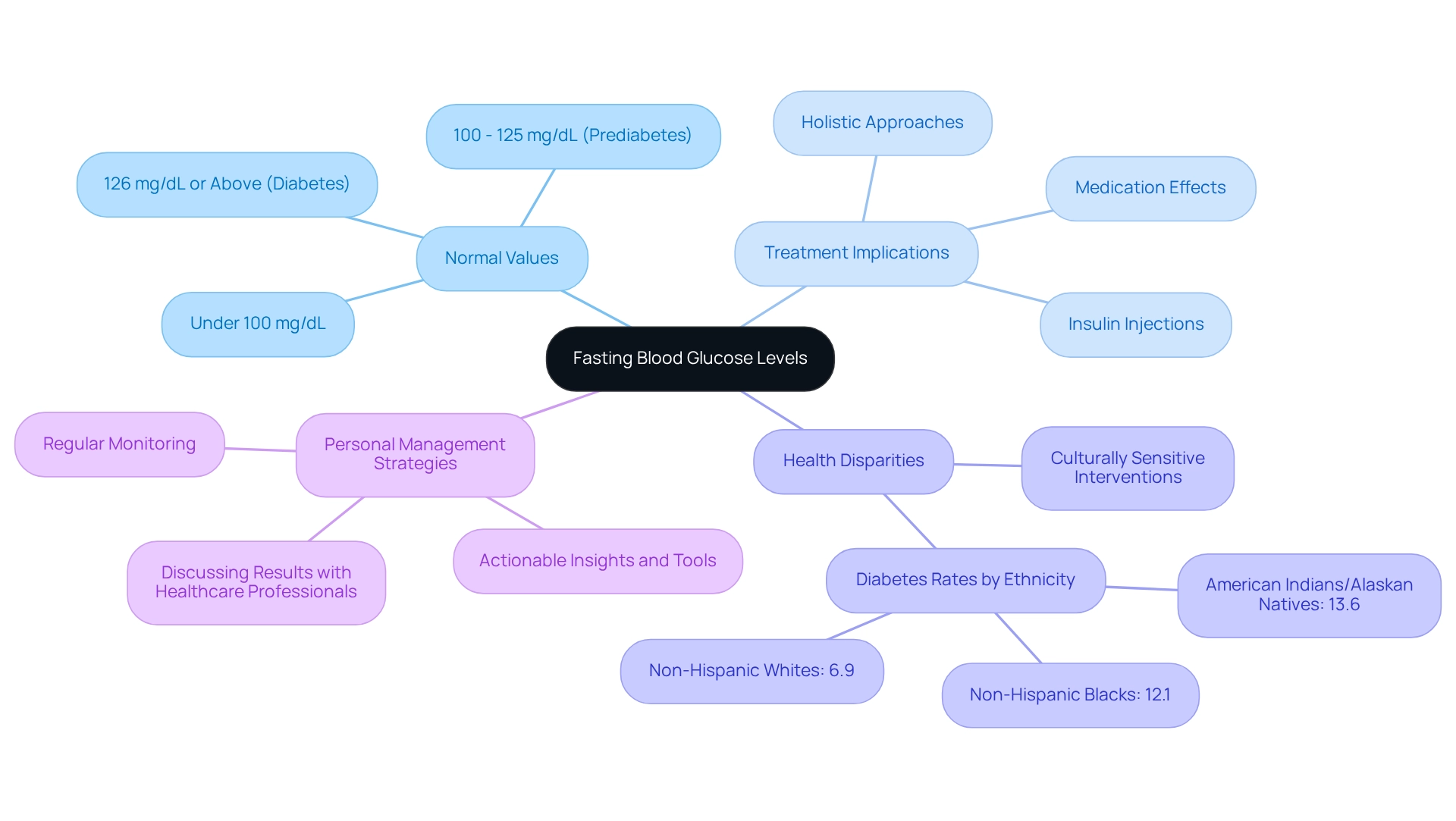
Fasting blood glucose readings play a vital role in identifying and managing blood sugar conditions, particularly after an overnight fast. According to the ADA blood glucose guidelines, normal fasting glucose values are defined as under 100 mg/dL. Values between 100 and 125 mg/dL may indicate prediabetes, while readings of 126 mg/dL or above confirm the condition. Regular monitoring of these levels is essential, as it provides valuable insights into how your body responds to food and medication. This knowledge empowers you to make informed dietary and lifestyle choices.
It’s important to recognize that traditional treatments for blood sugar management, like insulin injections and medications, can sometimes worsen insulin resistance in certain patients. Many individuals have shared their experiences, noting that the very treatments intended to help can inadvertently complicate their condition. This highlights the need for a more holistic approach to managing blood sugar levels. Such an approach should not only focus on regulating blood sugar but also on understanding the underlying factors contributing to insulin resistance. For those with type 2 metabolic disorder, the challenge often lies in the body’s struggle to effectively utilize the insulin it produces, rather than a mere lack of insulin.
The significance of fasting glucose measurements is underscored by concerning statistics showing that non-Hispanic Black children experience the highest rates of type 2 diabetes. This reality emphasizes the urgent need for culturally sensitive health interventions. Additionally, disparities in diabetes prevalence among different racial and ethnic groups—13.6% among American Indians/Alaskan Natives, 12.1% among non-Hispanic Blacks, and 6.9% among non-Hispanic Whites—further highlight the importance of targeted education and resources to address these disparities effectively.
Experts stress the necessity of tracking fasting glucose readings as outlined in the ADA blood glucose guidelines. Educators in this field assert that understanding the ADA blood glucose guidelines is crucial for effective management and prevention strategies. As Dr. Jason Shumard wisely states, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being.” As we approach the ADA blood glucose guidelines for 2025, it will be essential for both patients and healthcare providers to consistently monitor fasting glucose levels in the ongoing effort to combat this condition.
To take charge of your health, make it a habit to regularly check your fasting glucose readings and discuss your results with your healthcare professional. This proactive approach can significantly enhance your diabetes management, leading you toward a healthier future.
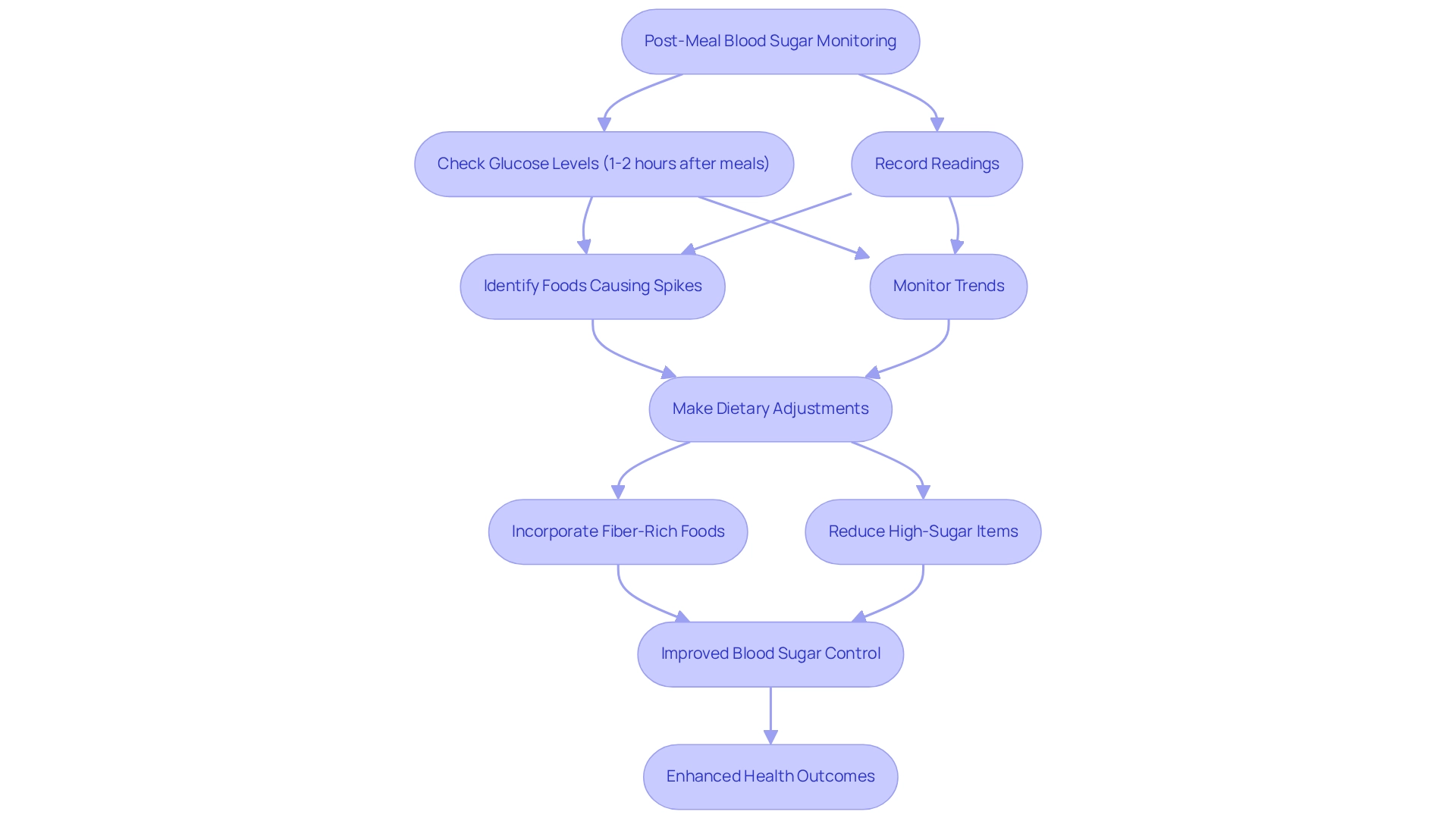
Post-Meal Blood Sugar Monitoring: Guidelines and Best Practices
Post-meal glucose monitoring is essential for understanding how various foods affect sugar levels. According to the ADA blood glucose guidelines, it is recommended to check glucose levels 1-2 hours after meals, aiming for a target of less than 180 mg/dL for most adults. This practice not only helps identify specific foods that may cause spikes in blood sugar but also empowers individuals to make informed dietary choices. By maintaining a thorough record of post-meal readings, you can uncover trends that lead to better blood sugar management.
It’s important to recognize that the statistics are concerning: in 2017-2018, 5,293 children and adolescents were diagnosed with type 2 diabetes. This underscores the urgency of implementing effective monitoring strategies. Many patients find that their dietary choices significantly influence their post-meal glucose levels. For instance, incorporating fiber-rich foods can help mitigate spikes, while high-sugar items may lead to elevated readings.
Real-life examples illustrate the positive impact of dietary adjustments based on post-meal glucose readings. Patients who have modified their meals to include more whole grains and vegetables often report improved blood sugar control. Dr. Jason Shumard emphasizes, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being.” This holistic approach aligns with the ADA blood glucose guidelines, which advocate for regular monitoring and suggest that individuals aim for post-meal glucose levels that support their overall health goals.
By adopting these best practices for post-meal blood sugar monitoring, you can take proactive steps toward managing your diabetes, leading to enhanced health outcomes and a better quality of life. Dr. Shumard’s Integrative Wellness Center aligns with these recommendations, offering innovative methodologies and tailored care to assist individuals in making informed dietary choices, particularly through his transformative 30-Day Diabetes Reset program. Call 858-564-7081 to discover how Dr. Shumard can help you restore your health! Additionally, hear from our patients: “I lost 55 lbs and my A1C improved from 9.1 to 5.7 after joining the program!
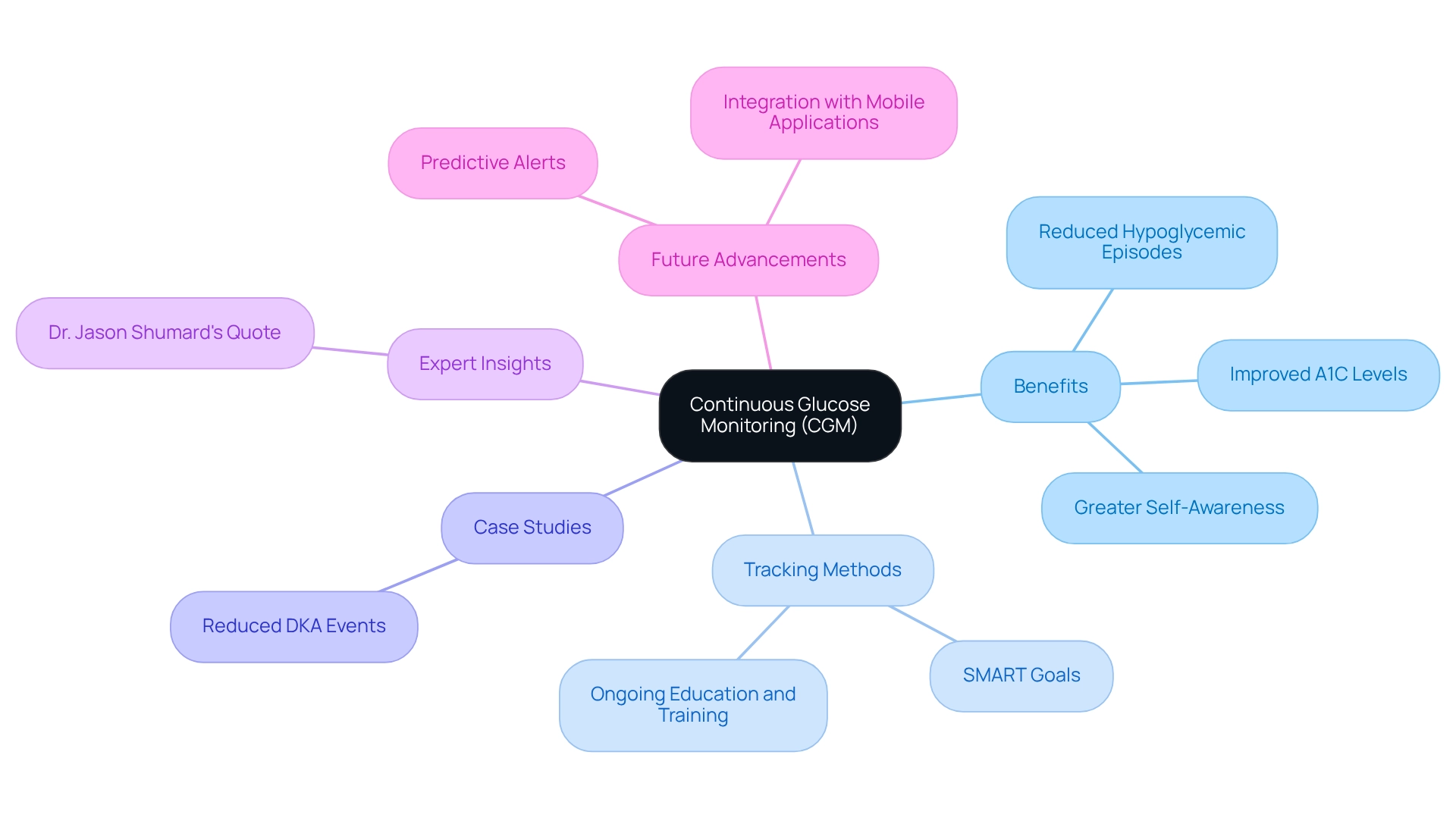
Continuous Glucose Monitoring: Enhancing Diabetes Management
Continuous glucose monitoring (CGM) systems offer a transformative approach to diabetes management, providing real-time insights into blood glucose levels. This innovative technology empowers you to track your glucose fluctuations throughout the day, enabling informed choices about your diet, exercise, and medication. Research shows that using CGM is linked to significant improvements in A1C levels, with studies revealing reductions of up to 0.5% to 1% among users. Additionally, CGM has been associated with fewer hypoglycemic episodes, enhancing overall safety and quality of life.
To truly harness the benefits of CGM, consider implementing effective tracking methods and setting SMART goals—specific, measurable, attainable, relevant, and time-bound. For example, you might aim to keep your blood glucose levels within a target range for a month or reduce your A1C by a certain percentage over a specific timeframe. Many patients find that structured goal-setting boosts motivation and accountability, leading to improved health outcomes.
A compelling case study illustrates the effectiveness of CGM in reducing the occurrence of diabetic ketoacidosis (DKA) among younger adults. The study found that individuals under 26 who used CGM technology experienced a lower rate of DKA events, highlighting CGM’s critical role in preventing serious diabetes-related complications. This connection underscores how CGM not only supports daily management but also serves as a vital tool in preventing severe health crises.
Expert insights further emphasize the benefits of CGM, particularly its capacity to promote greater self-awareness and self-management. As Dr. Jason Shumard wisely noted, “The results of this evaluation should not be used to make any medical decisions and should be considered in conjunction with professional medical advice.” This statement reinforces the importance of integrating CGM data with professional guidance to achieve optimal health outcomes.
Moreover, ongoing education and training are essential for maximizing CGM use. Continuous learning enables you to fully leverage the advantages of CGM technology, empowering you on your health journey. By regularly assessing your progress and adjusting your goals, you can cultivate a sense of accomplishment and maintain your engagement in health management.
Looking ahead, the advancements in CGM technology in 2025 promise to enhance its effectiveness, featuring predictive alerts and integration with mobile applications. These innovations make it easier for you to manage your condition proactively. Real-world examples abound, showcasing how individuals have successfully utilized CGM to improve their management of diabetes, leading to better health outcomes and a more empowered approach to living with this condition.
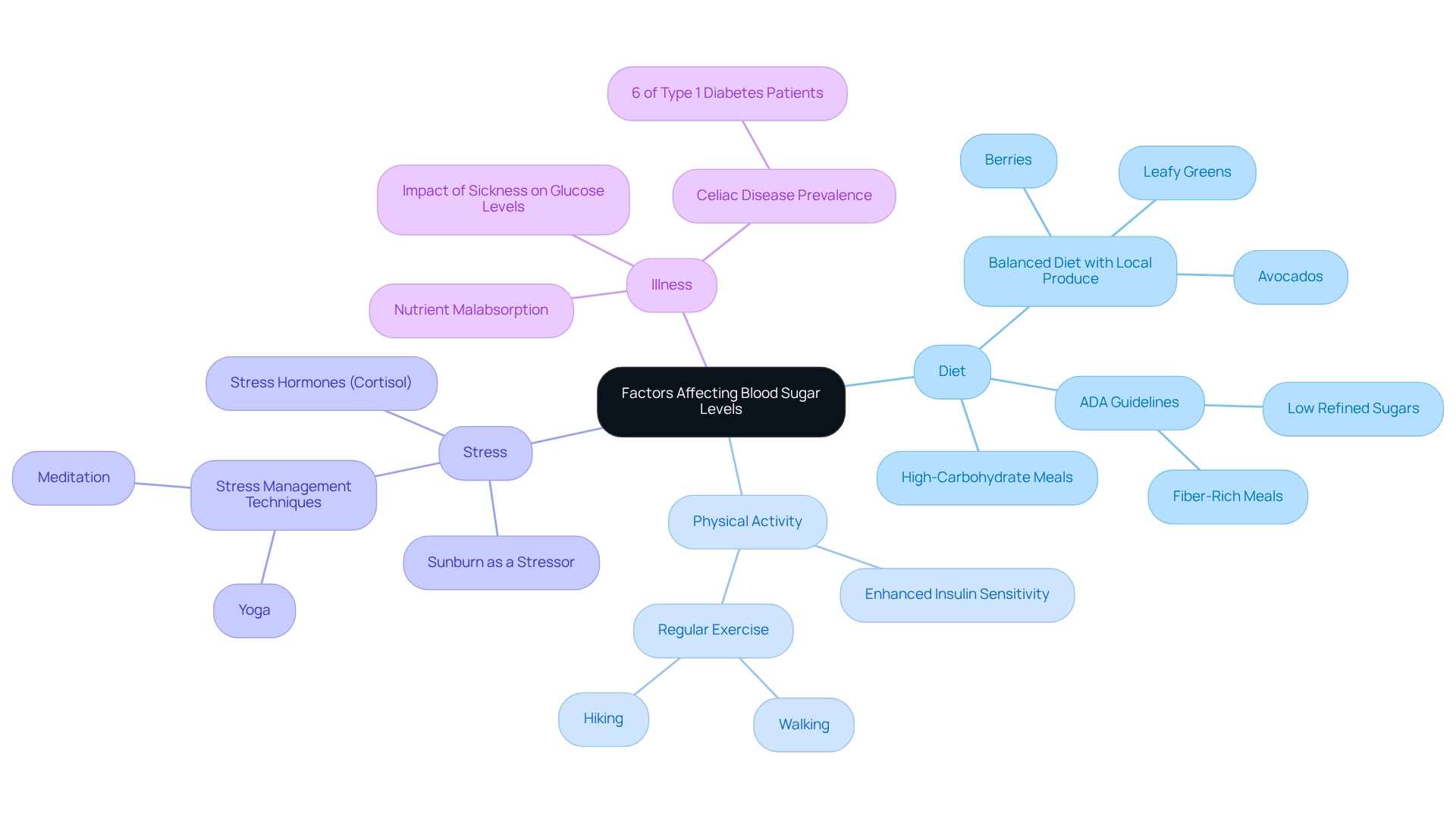
Factors Affecting Blood Sugar Levels: Key Considerations for Diabetics
Blood sugar concentrations in people with diabetes can be influenced by various factors, including diet, physical activity, stress, and illness. Have you ever noticed how high-carbohydrate meals can lead to significant increases in glucose? On the other hand, regular physical activity is known to effectively reduce these levels. Engaging in consistent physical activities, such as walking or hiking in the beautiful parks and trails of San Marcos, not only supports weight control but also enhances insulin sensitivity, which is crucial for glucose regulation. The area’s lovely weather and outdoor lifestyle make it easier to integrate physical activity into daily life.
Nutrition plays a vital role in managing glucose concentrations. A balanced diet rich in local produce, like avocados, berries, and leafy greens, can help regulate sugar levels and promote overall well-being. Have you considered shopping at local farmers’ markets? Not only do they provide access to fresh, nutritious options, but they also foster community connections that can enhance motivation and support. Additionally, think about participating in community wellness programs available in San Marcos, offering resources and support tailored to diabetes management.
It’s important to recognize that stress is another significant factor; it can elevate sugar concentrations due to the release of stress hormones like cortisol. This hormonal response can lead to persistent hyperglycemia, making it essential for individuals to develop stress management techniques. Many patients find that practices such as yoga and meditation, offered by nearby studios, can help alleviate stress and improve mental wellness, thereby promoting better sugar regulation.
Sickness can also affect glucose levels, as the body’s response to infection or injury often results in elevated sugar levels. Did you know that around 6% of individuals with type 1 diabetes also have celiac disease? This condition can complicate glucose management and is significantly more prevalent than in the general population. It highlights the importance of thorough health evaluations for individuals with this condition. Celiac disease can lead to nutrient malabsorption, further complicating diabetes management, making it crucial for patients to be aware of their dietary restrictions.
Expert opinions emphasize the importance of diet and exercise in managing blood sugar as outlined in the ADA blood glucose guidelines. Health professionals recommend adhering to the ADA blood glucose guidelines by consuming balanced meals rich in fiber and low in refined sugars, along with regular physical activity, to maintain stable glucose levels. Stacy M. Loneman, R.N., CDCES, advises, “If you experience ongoing hyperglycemia, discuss with your team about modifying your treatment plan.” Real-life examples show how lifestyle changes, like adopting a Mediterranean diet or incorporating daily walks, have led to better blood sugar management for many patients.
Furthermore, case studies have shown that common stressors, such as sunburn, can unintentionally impact glucose levels. It’s essential for individuals to recognize both clear and subtle influences on their health. By understanding these factors, including the risk of foot issues due to nerve damage and poor blood circulation, individuals with high blood sugar can take proactive steps to manage their condition more effectively. To enhance your health management journey, explore local resources and community programs that can provide support and guidance tailored to your needs.
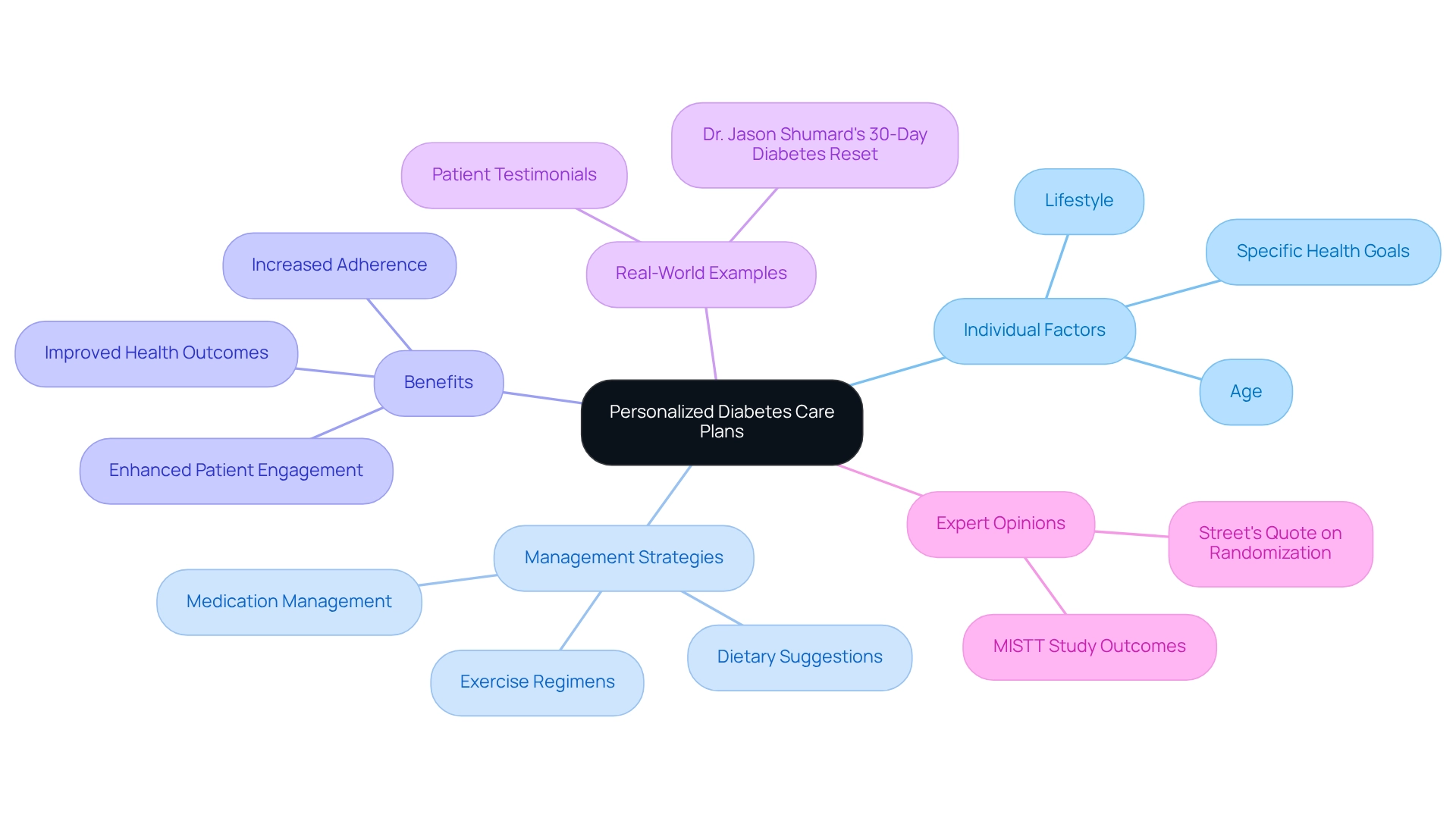
Personalized Diabetes Care Plans: Tailoring Management to Your Needs
Creating personalized diabetes care plans is crucial for effective management of type 2 diabetes. It’s important to recognize that these plans must consider individual factors such as age, lifestyle, and specific health goals. Working with healthcare professionals enables individuals to develop thorough plans that include dietary suggestions, exercise regimens, and medication management tailored to their unique requirements. This personalized approach not only enhances adherence to treatment but also significantly improves overall health outcomes.
Research shows that personalized care plans lead to improved engagement and satisfaction for individuals. Many patients find that following tailored management strategies can make a real difference. For instance, a study utilizing Wilcoxon signed rank tests demonstrated that individuals who adhered to these strategies showed a marked improvement in their blood sugar levels over a six-month period, with adherence rates increasing by over 30%. Moreover, healthcare providers stress that tailoring management strategies cultivates a sense of ownership among individuals, empowering them to take charge of their health.
Real-world examples illustrate the effectiveness of personalized care. One notable case involved an individual who, through Dr. Jason Shumard’s 30-Day Diabetes Reset program, shared, “I was on 2 different meds that weren’t working and was told that I needed insulin. After joining the program, I lost 55 lbs and reduced my A1C from 9.1 to 5.7 within eight months.” Another patient, who had been on various treatments for blood sugar regulation and other health issues, expressed, “I feel so much better… I don’t need my meds anymore!!!” Such outcomes highlight the significance of personalized strategies in managing blood sugar levels.
As we approach 2025, the focus on customized care plans for managing blood sugar conditions continues to expand, with experts supporting their incorporation into standard practice. By prioritizing customized approaches, healthcare providers can significantly boost adherence and enhance health results, ultimately leading to an improved quality of life for individuals managing their condition. As noted by Street, the randomization of primary care clinics to different arms in studies underscores the importance of tailored approaches in clinical settings. Moreover, the main results of MISTT, which encompass individual-centered quality of life and individual engagement in managing healthcare, further emphasize the importance of personalized care plans.
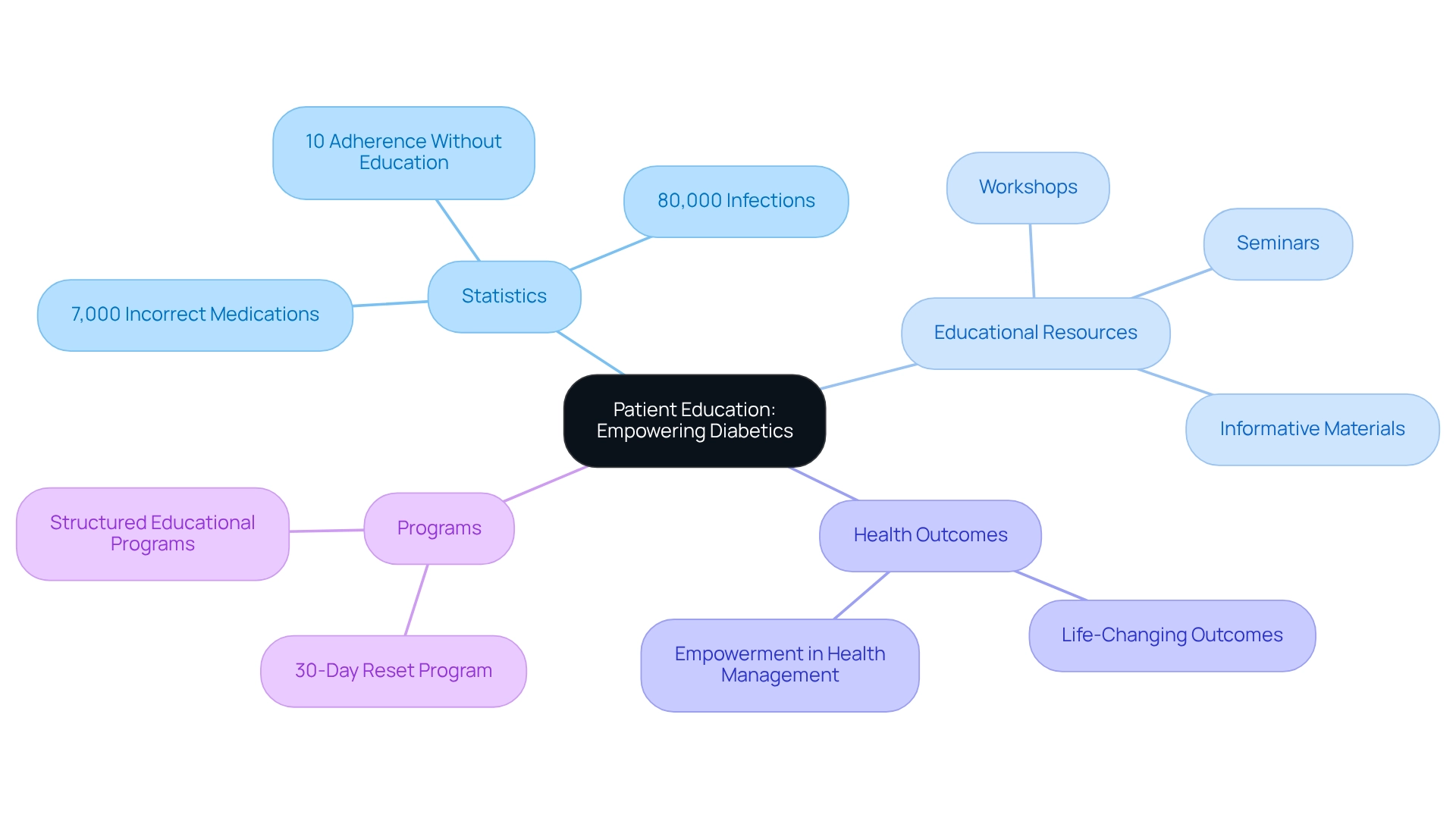
Patient Education: Empowering Diabetics with Knowledge
Educating individuals is a fundamental pillar in effectively managing health conditions. It’s crucial to recognize the alarming statistics:
- 7,000 incorrect medications are administered in hospitals
- 80,000 infections are acquired in these settings
By gaining a comprehensive understanding of their condition, treatment options, and self-care strategies, individuals can take control of their health. Educational resources, such as workshops, seminars, and informative materials, play a vital role in equipping individuals with knowledge about the ADA blood glucose guidelines, blood sugar monitoring, dietary choices, and the necessity of regular check-ups. This proactive approach nurtures confidence and motivates individuals to engage in effective self-care habits.
Statistics reveal that only 10% of individuals who have not received education on managing blood sugar adhere to at least 9 out of 10 suggested self-care and clinical practices. This underscores the significance of educational initiatives. At Dr. Jason Shumard’s center, individuals have reported life-changing outcomes through structured educational programs that align with ADA blood glucose guidelines, demonstrating the transformative effect of knowledge on blood sugar management. Many patients find that effective self-care strategies are essential for handling their condition.
As one health expert noted, some individuals may undervalue the importance of education, believing they already possess adequate knowledge. This highlights the need for ongoing education and support, particularly through workshops and seminars related to blood sugar management that follow the ADA blood glucose guidelines, including the comprehensive 30-Day Reset program offered by Dr. Shumard, which allows patients to access the latest resources and insights. Such opportunities ultimately lead to improved health outcomes and a decreased reliance on traditional medical interventions. It’s important to recognize that taking these steps can be a game changer for many. By investing in education and self-care, individuals can truly transform their health journey.
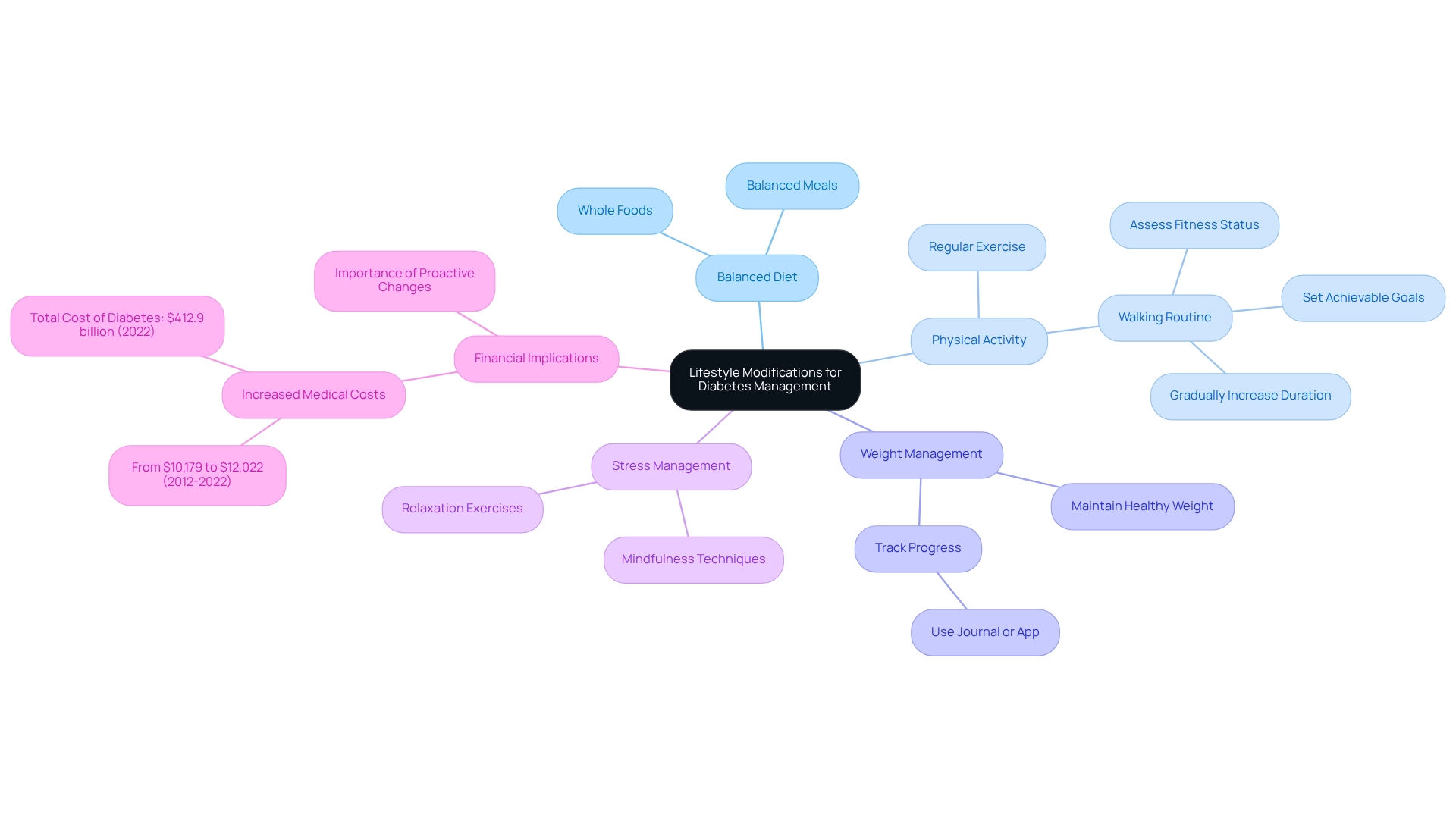
Lifestyle Modifications: Essential Strategies for Diabetes Management
Lifestyle changes are vital for effective diabetes management, significantly impacting sugar control and overall health. It’s important to recognize that adopting a balanced diet rich in whole foods can improve glycemic control and reduce reliance on medications. Many patients find that consistent physical activity, like walking, holds equal significance; research shows that those who engage in regular exercise can lower their blood sugar and enhance insulin sensitivity. To successfully embark on a walking routine, individuals should first assess their current fitness status and set achievable goals, such as committing to a daily walk of 10-15 minutes. Selecting an appropriate environment for walking, whether indoors or outdoors, is crucial for safety and comfort. Developing a consistent schedule and gradually increasing both the duration and frequency of walks can significantly enhance overall wellness and vitality.
Maintaining a healthy weight further contributes to improved health outcomes, as excess weight is a major risk factor for complications. Tracking progress through a journal or an app can help maintain motivation and allow individuals to celebrate their achievements along the way. Incorporating stress management techniques, such as mindfulness and relaxation exercises, can also lead to improved blood sugar levels. It’s essential to understand that stress can negatively influence glycemic control, making it vital for those with the condition to discover effective coping strategies. These techniques fit into a comprehensive lifestyle modification strategy that aligns with Dr. Shumard’s holistic approach to health.
Statistics show the significant effect of lifestyle modifications:
- The additional medical expenses linked to this condition increased from $10,179 to $12,022 per individual between 2012 and 2022.
- This increase highlights the financial burden of unmanaged health issues and underscores how proactive lifestyle changes can help reduce these costs.
- Furthermore, the total cost of diagnosed diabetes in the U.S. reached $412.9 billion in 2022, with a significant portion attributed to direct medical expenses.
These figures emphasize the importance of adopting healthier habits to prevent complications and reduce healthcare costs.
Real-world examples illustrate the success of these strategies. Many patients, like those in Dr. Shumard’s 30-Day Diabetes Reset program, have reported life-changing outcomes after implementing dietary changes and increasing their physical activity levels, leading to improved quality of life and better health management. Expert advice consistently supports these approaches, with nutritionists advocating for dietary strategies that prioritize whole foods and balanced meals in line with ADA blood glucose guidelines to help control blood sugar effectively. As Benjamin Franklin wisely stated, “The best doctor gives the least medicine.” By embracing these lifestyle modifications, individuals with diabetes can take significant steps toward reclaiming their health and enhancing their well-being.
Conclusion
The journey towards effective diabetes management can feel overwhelming, but it’s important to recognize that you are not alone. A comprehensive approach that includes personalized care, education, and lifestyle changes is essential. The Integrative Wellness Center’s 30-Day Diabetes Reset Program exemplifies this holistic strategy, empowering you with the tools necessary for sustainable health improvements. By addressing the underlying causes of diabetes rather than merely managing symptoms, you can achieve better health outcomes and reclaim your well-being.
Education is a key component of this journey. With the right resources and support, you can gain a deeper understanding of your condition and make informed decisions. The American Diabetes Association’s guidelines for blood glucose monitoring, A1C testing, and dietary adjustments highlight the importance of proactive management. Many patients find that personalized care plans and lifestyle modifications lead to transformative results, significantly improving blood sugar control and enhancing overall quality of life.
As we face an escalating diabetes epidemic, the importance of adopting effective management strategies cannot be overstated. By embracing a holistic approach that prioritizes individualized care, continuous education, and lifestyle changes, you can take charge of your health and navigate your diabetes journey with confidence. The 30-Day Diabetes Reset Program serves as a beacon of hope, demonstrating that with the right support and resources, lasting health improvements are within reach. You deserve to feel empowered and supported on this path to better health.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at the Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a compassionate approach designed to help patients manage their diabetes effectively. It combines personalized coaching, nutritional guidance, and educational resources to equip participants with the tools necessary for sustainable health improvements.
How does the program help reduce diabetes-related costs?
The program addresses the underlying causes of diabetes rather than just managing symptoms, which can lead to improved health outcomes and ultimately reduce the overwhelming medical expenditures that patients typically incur.
What are some reported benefits from participants of the program?
Participants have reported better blood sugar control and enhanced overall well-being, thanks to the actionable insights and practical tools provided throughout the program.
What role do the ADA blood glucose guidelines play in diabetes management?
The ADA blood glucose guidelines emphasize the importance of regular testing for glucose monitoring, helping individuals achieve and maintain optimal sugar levels, which is crucial for effective diabetes management.
Why is regular blood glucose monitoring important?
Regular blood glucose monitoring is vital as it aids in immediate health management and fosters long-term well-being, allowing individuals to make informed decisions about their diet and medication.
How can lifestyle strategies enhance diabetes management?
Incorporating holistic lifestyle strategies, such as a balanced diet rich in local produce and regular outdoor exercise, can further improve the effectiveness of blood glucose monitoring and overall health management.
What is the significance of A1C testing in diabetes management?
A1C testing is essential for tracking long-term blood sugar management, helping individuals understand their average glucose levels over the past two to three months, and is recommended to be kept below 7% to lower the risk of complications.
What are the benefits of personalized A1C testing recommendations?
Personalized A1C testing recommendations can vary based on individual health conditions and treatment responses, which is important for effective diabetes management and achieving better health outcomes.
Can you provide an example of success from A1C testing?
One patient successfully reduced their A1C from 8.5% to 6.5% after committing to regular A1C testing and making lifestyle changes, demonstrating the positive impact of proactive health management.