Overview
Managing type 2 diabetes can feel overwhelming, but there is hope. This article focuses on nine medications that effectively lower A1C levels, helping you regain control of your health. Among these, metformin, GLP-1 receptor agonists, and SGLT2 inhibitors stand out, each working through unique mechanisms to improve blood sugar control. It’s important to recognize that these medications often work best alongside personalized treatment plans that consider your individual needs and lifestyle factors.
Many patients find that understanding how these medications function can empower them in their journey. By addressing the challenges you face, we can explore how these options might fit into your life. Remember, you are not alone in this; countless individuals share similar experiences and concerns.
As you consider these medications, think about how they might support your journey toward healthier living. With the right approach, you can take meaningful steps toward managing your diabetes effectively. Embracing this journey not only involves medication but also a commitment to a holistic treatment plan that nurtures your well-being.
Let’s take this journey together, exploring the possibilities that lie ahead. You deserve support and understanding as you navigate this path.
Introduction
In the battle against diabetes, innovative treatment strategies have emerged, offering hope and empowerment to those affected by this chronic condition. It’s important to recognize that living with diabetes can be challenging, and the Integrative Wellness Center’s 30-Day Diabetes Reset Program stands at the forefront, combining dietary education, physical activity, and behavioral coaching to help participants take charge of their health.
Many patients find that from the widely prescribed metformin to advanced therapies like GLP-1 receptor agonists and SGLT2 inhibitors, a variety of medications are available, each designed to lower A1C levels and enhance overall well-being.
This article explores the multifaceted landscape of diabetes management, highlighting personalized approaches that integrate functional medicine, lifestyle modifications, and cutting-edge treatments. By understanding these options, individuals can navigate their diabetes journey with confidence and clarity, paving the way for a healthier future.
Integrative Wellness Center: 30-Day Diabetes Reset Program
Are you feeling overwhelmed by managing your diabetes? The 30-Day Diabetes Reset Program at the Integrative Wellness Center is here to support you on your journey. This transformative initiative equips you with the tools and knowledge needed to manage your condition effectively. Through a clinically validated approach, this program combines:
- Dietary education
- Physical activity
- Behavioral coaching
These elements foster sustainable lifestyle changes that can truly make a difference.
Imagine learning to recognize and remove foods that raise your blood sugar while engaging in consistent exercise. You’ll even create a customized action plan that encourages long-term well-being. Many patients find that envisioning a life where they maintain their glucose balance without relying on insulin and medication is not just a dream, but a reachable goal.
It’s about feeling revitalized and reducing the worry associated with potential complications related to blood sugar issues, and this program is designed not only to incorporate a1c lowering medications but also to empower you to take charge of your health journey.
It becomes a fundamental aspect of our strategy for managing blood sugar, allowing you to feel more in control and confident in your choices. Remember, you are not alone in this journey, and together we can work towards a healthier future.
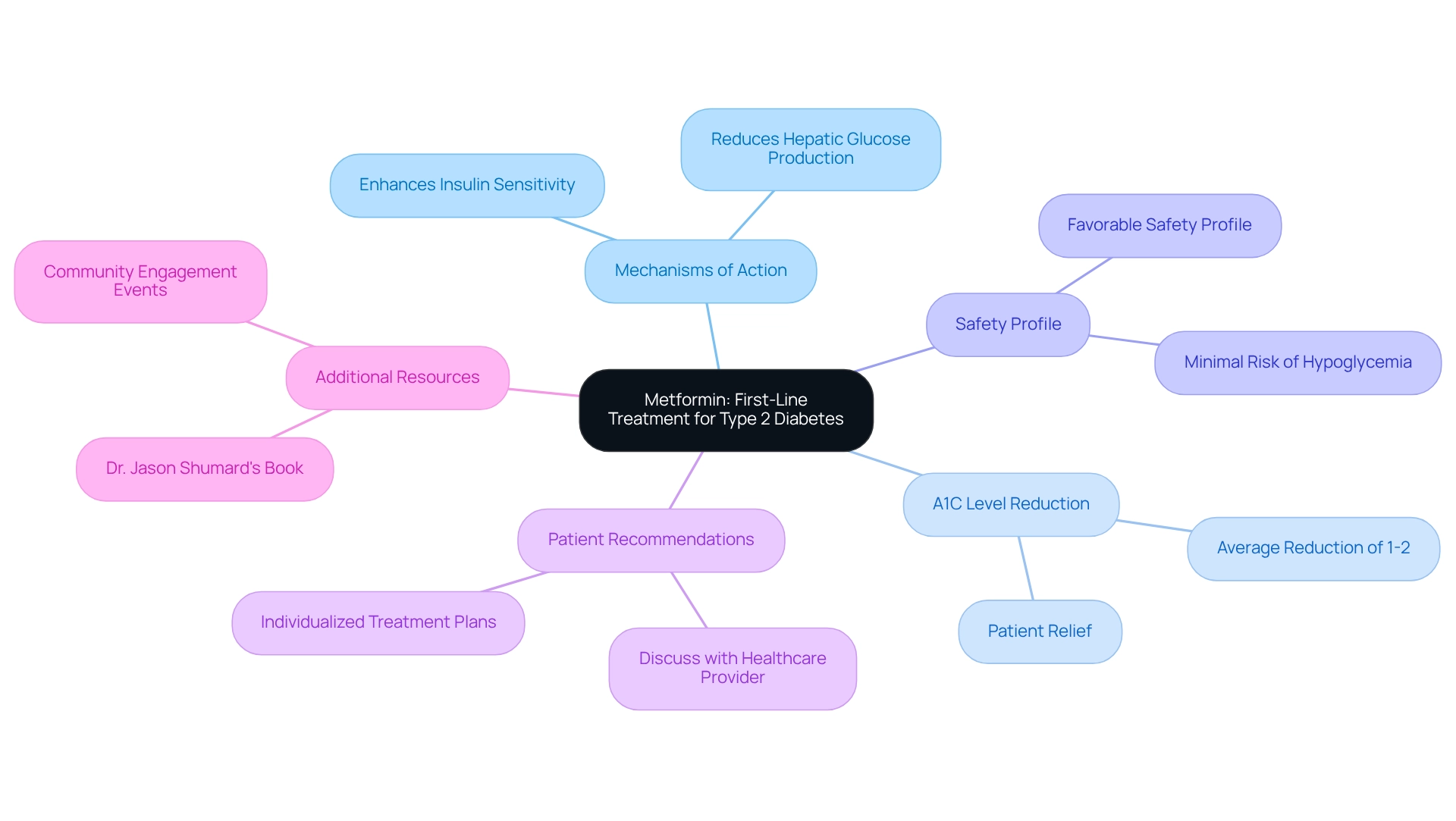
Metformin: First-Line Treatment for Type 2 Diabetes
Metformin is often the first choice for new patients managing type 2 diabetes, and it’s understandable why. This medication primarily works by reducing hepatic glucose production and enhancing insulin sensitivity, which can significantly help in lowering blood sugar levels. Many patients find that metformin, as one of the A1C lowering medications, can reduce A1C levels by approximately 1-2%, providing a sense of relief in their management journey. It’s important to recognize that metformin has a favorable safety profile, with minimal risk of hypoglycemia when used alone. However, every individual’s experience is unique. Patients are encouraged to discuss the potential benefits and side effects of metformin with their healthcare provider to determine if it aligns with their treatment plan.
To further enhance your management of blood sugar levels, consider exploring Dr. Jason Shumard’s comprehensive resources. His insightful book on functional medicine strategies for type 2 diabetes and thyroid dysfunction could be a valuable addition to your journey. Many patients have found real solutions within its pages.
We invite you to attend our next event, where you can gain valuable information and receive a free copy of this essential guide. This opportunity will help you unlock tailored solutions for your individual health needs. Register now to reserve your seat and take an active role in our community engagement efforts. Together, we can navigate this journey towards better health.
GLP-1 Receptor Agonists: Effective A1C Lowering Agents
Living with type 2 diabetes can be challenging, and it’s important to recognize the emotional and physical struggles that many face. GLP-1 receptor agonists, such as liraglutide and semaglutide, are A1C lowering medications that offer effective solutions for reducing A1C values in individuals like you. These medications work by mimicking the incretin hormone, which:
- Stimulates insulin secretion after meals
- Suppresses glucagon release
- Slows gastric emptying
Many patients find that A1C lowering medications can reduce A1C levels by 1-2% while also promoting weight loss, making them especially beneficial for those who are overweight. Moreover, these A1C lowering medications also reduce the risk of cardiovascular events, which adds to their appeal as a viable option for managing diabetes.
Incorporating GLP-1 receptor agonists into a personalized functional medicine approach can provide a comprehensive strategy that not only addresses the symptoms of diabetes but also considers your unique medical history, lifestyle choices, and genetic factors. Functional medicine practitioners often utilize assessments like metabolic panels and genetic testing to create tailored treatment plans.
This holistic perspective is designed to support sustainable diabetes management and highlights the long-term benefits of functional medicine for improving overall health. Remember, you are not alone in this journey, and there are compassionate options available to help you thrive.
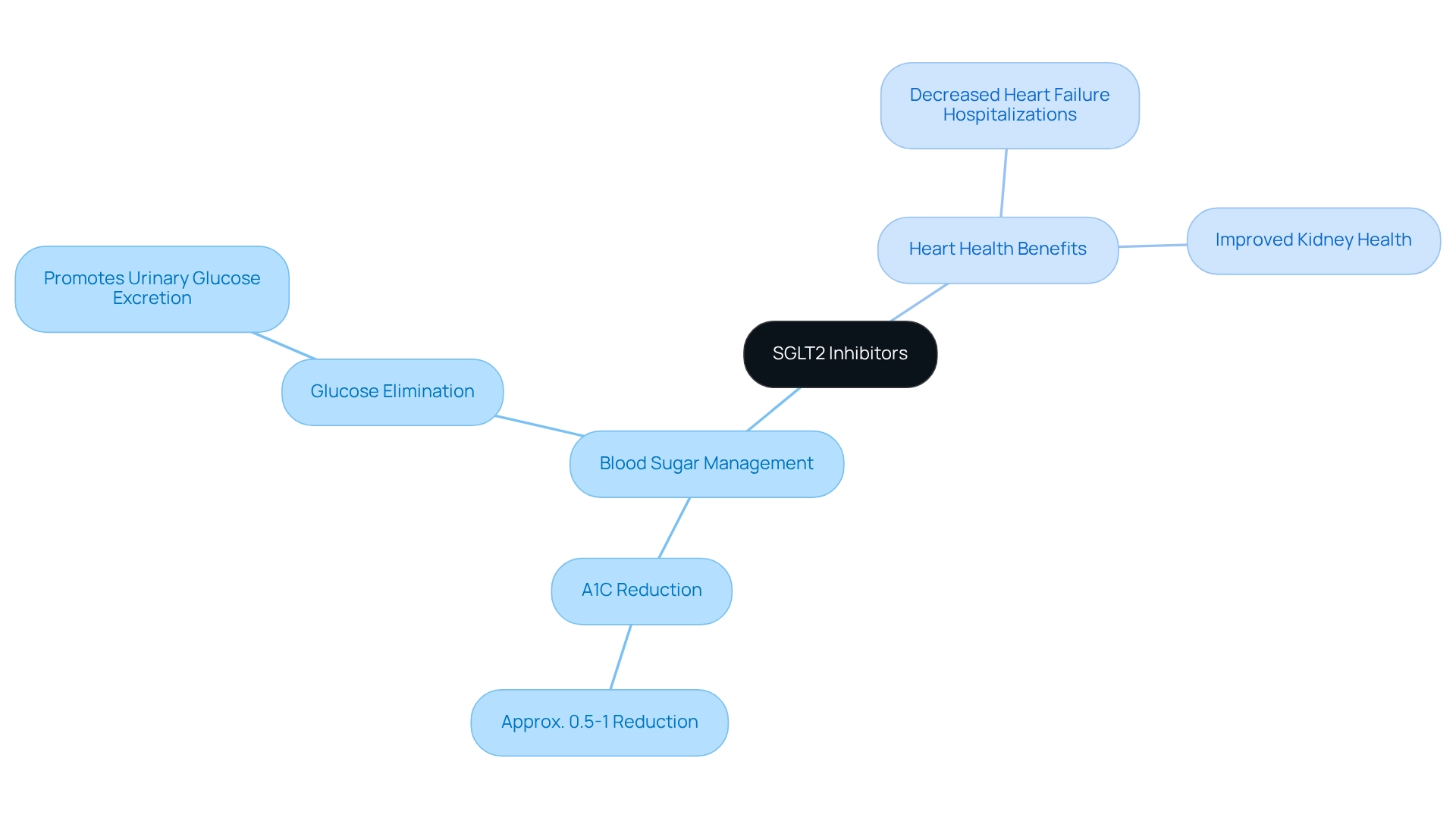
SGLT2 Inhibitors: Dual Benefits for Blood Sugar and Heart Health
Managing diabetes can be a challenging journey, and it’s important to recognize that you’re not alone in this. SGLT2 inhibitors, such as canagliflozin and empagliflozin, are here to help. These medications work by promoting the elimination of glucose through urine, which can lead to a reduction in blood sugar levels. Many patients find that A1C lowering medications can reduce A1C levels by approximately 0.5-1%.
But the benefits of SGLT2 inhibitors extend beyond just lowering glucose. They also offer significant cardiovascular advantages, including a decrease in heart failure hospitalizations and improved kidney health. This dual action makes them a valuable option for individuals with type 2 diabetes, especially those who have existing heart conditions or are at risk for heart complications. Integrating A1C lowering medications into a personalized functional medicine approach can further enhance your diabetes management. This approach involves thorough evaluations and diagnostic exams to better understand your unique medical history, lifestyle choices, and genetic factors. By customizing treatment plans that incorporate SGLT2 inhibitors alongside lifestyle changes and comprehensive health strategies, healthcare providers empower you to achieve improved long-term outcomes.
Remember, every small step you take is a step toward better health. It’s about finding what works best for you and your body, and with the right support, you can navigate this journey with confidence.
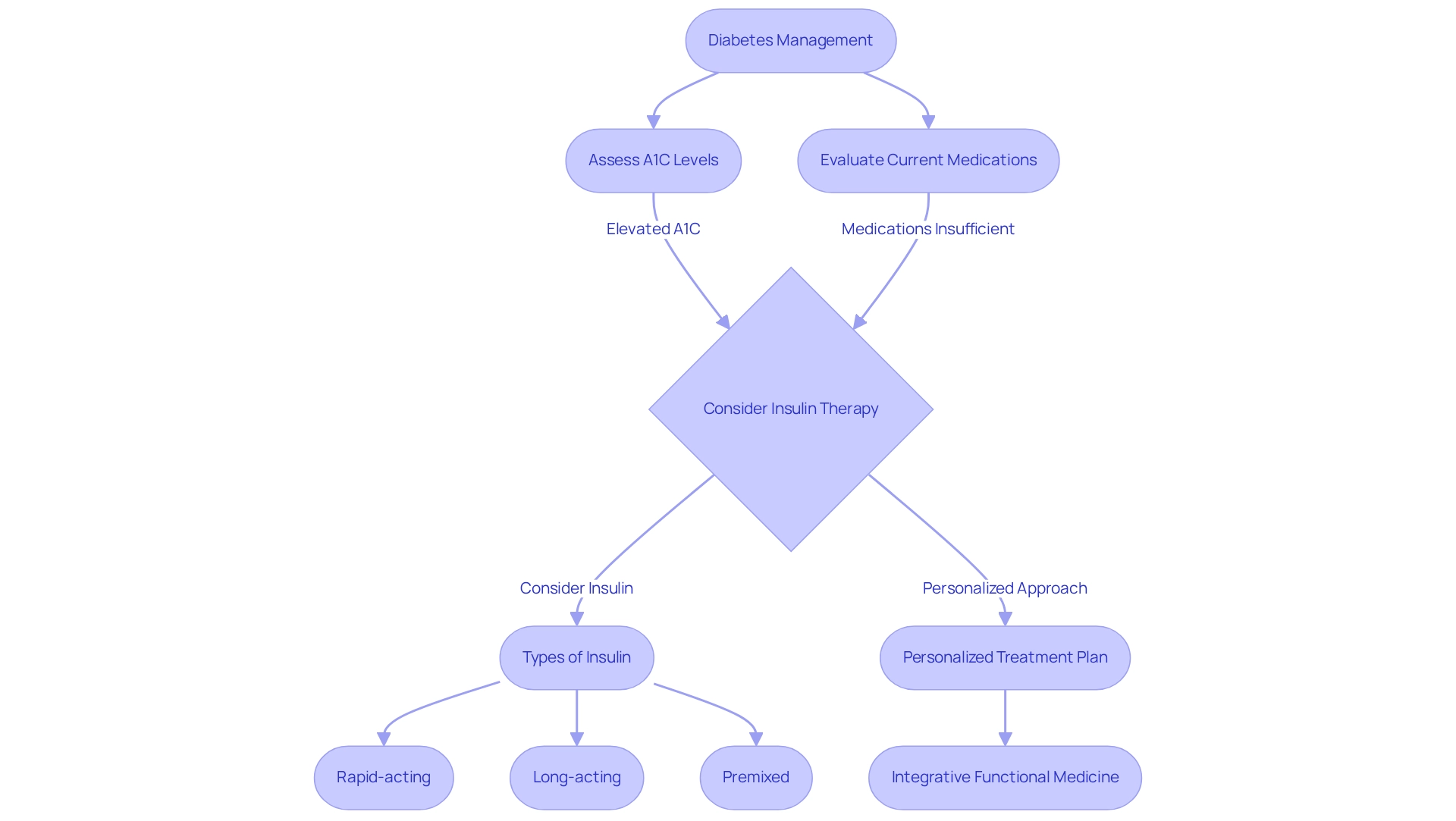
Insulin Therapy: Essential for Managing High A1C Levels
For individuals grappling with type 2 diabetes, insulin treatment is often essential when oral medications alone fall short in achieving adequate glycemic control. If you’re among those with significantly elevated A1C levels, insulin can provide immediate and effective blood sugar regulation, making it a crucial part of your treatment plan. However, it’s important to recognize that insulin therapy should be integrated into a comprehensive, personalized approach to managing diabetes.
Integrative functional medicine takes into account your unique wellness profile, considering elements such as your medical history, lifestyle choices, and genetic factors. This holistic perspective empowers healthcare providers to tailor insulin regimens that meet your individual needs, ultimately enhancing your overall health outcomes.
Functional medicine employs thorough assessments and diagnostic tests to uncover the factors contributing to diabetes. This ensures that your treatment plan addresses not just the symptoms but also the root causes of your condition. There are various types of insulin available, including:
- Rapid-acting
- Long-acting
- Premixed formulations
Each is designed to cater to unique circumstances.
Current trends indicate a growing reliance on A1C lowering medications and insulin therapy, particularly among individuals with elevated A1C readings, as they can significantly improve health outcomes. In fact, almost £3 million has been allocated to research initiatives aimed at developing innovative smart insulins, which may further enhance treatment options for those with blood sugar conditions. One exciting advancement is the development of glucose-responsive insulins (GRIs), which activate in response to blood sugar levels, potentially allowing individuals to require insulin only once a week.
Dr. Elizabeth Robertson, Director of Research at Diabetes UK, expressed optimism, stating, “We are hopeful that this research will lead to transformative progress in type 1 care.” This highlights the potential benefits for everyone managing blood sugar conditions. Collaborating closely with your healthcare provider is essential to determine the most suitable insulin regimen, dosage, and administration techniques. This partnership ensures optimized diabetes management and improves your quality of life through a personalized and integrative approach.
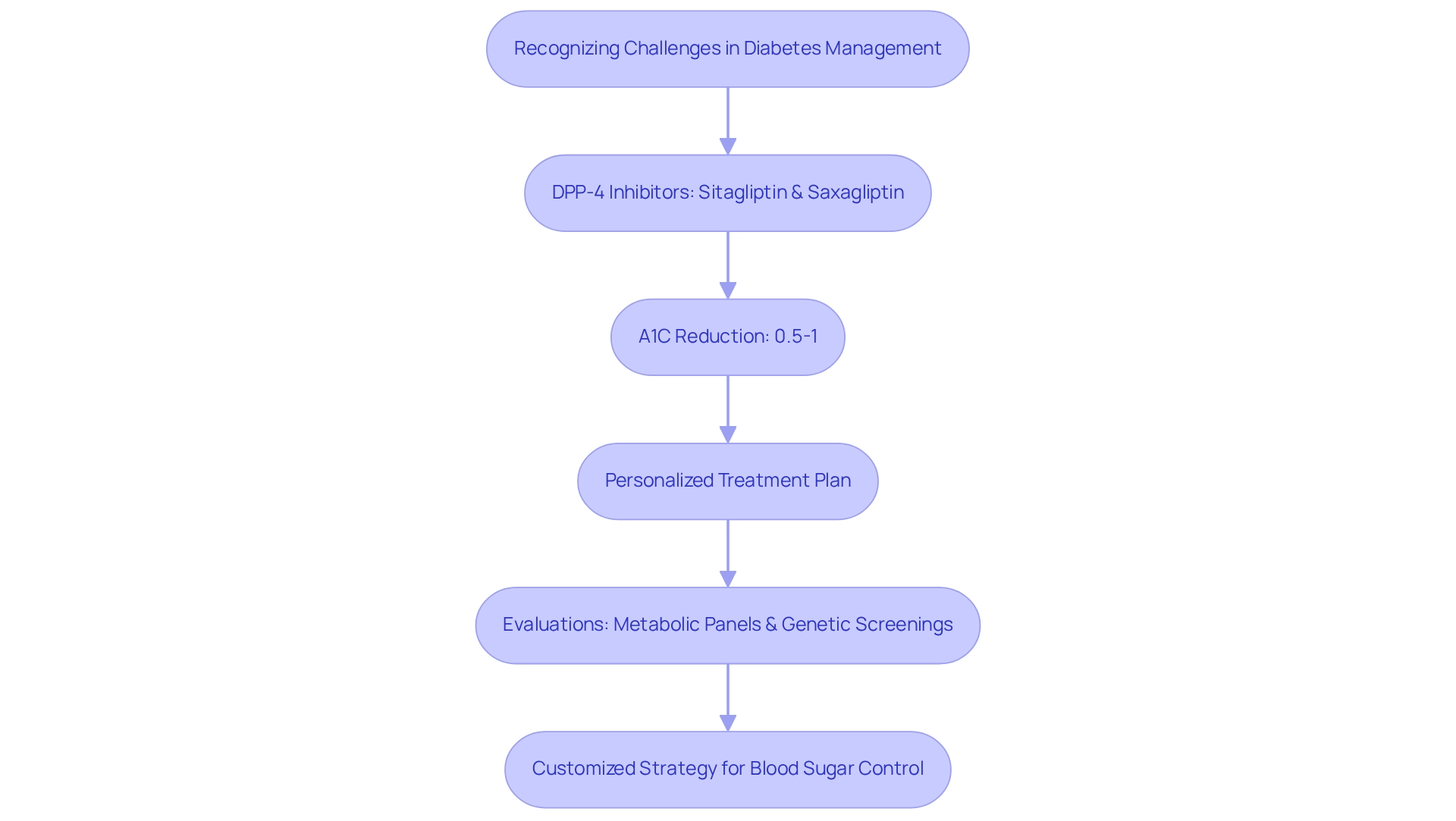
DPP-4 Inhibitors: A Gentle Approach to Lowering A1C
Managing diabetes can feel overwhelming at times, and it’s important to recognize the challenges you face. DPP-4 inhibitors, such as sitagliptin and saxagliptin, offer a gentle, supportive approach to blood sugar regulation. These oral medications work by increasing incretin levels, which play a crucial role in managing your blood sugar levels. Many patients find that A1C lowering medications can reduce A1C levels by about 0.5-1%, providing a sense of progress without the worry of hypoglycemia or weight gain. It’s comforting to know that DPP-4 inhibitors can be integrated into a personalized functional medicine approach. This means that your unique health history, lifestyle choices, and even genetic factors can be considered when creating your treatment plan. You can use these medications on their own or alongside other therapies, allowing for a customized strategy that effectively controls blood sugar levels while addressing the underlying factors of type 2 diabetes.
To ensure the best outcomes, thorough evaluations and diagnostic examinations—like metabolic panels and genetic screenings—are essential. These assessments help identify the specific factors contributing to your condition. By understanding your individual needs, we can work together to create a more effective and personalized treatment plan, supporting you on your journey toward better health.
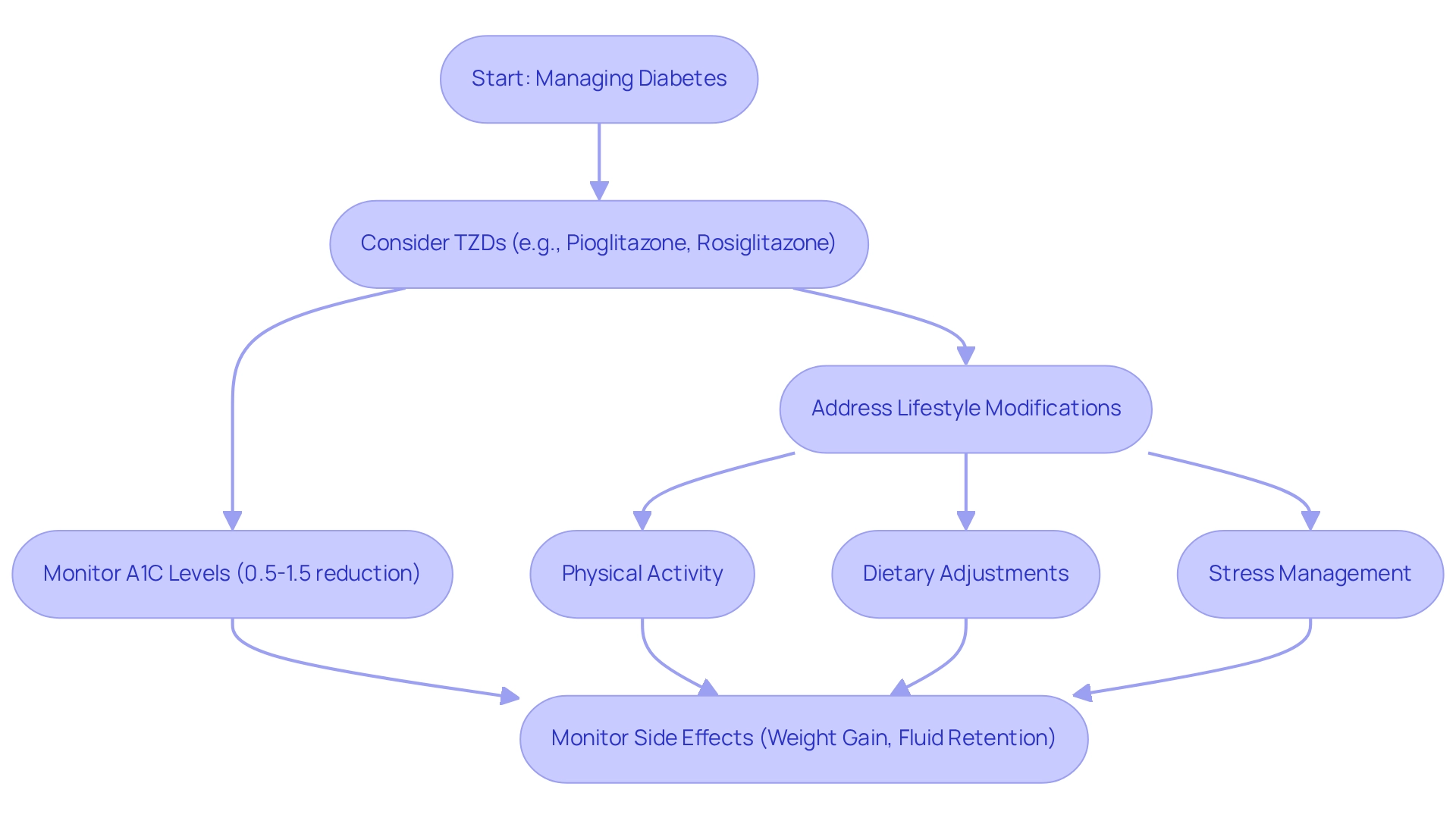
Thiazolidinediones: Enhancing Insulin Sensitivity
Thiazolidinediones (TZDs), such as pioglitazone and rosiglitazone, are medications that can help improve insulin sensitivity in muscle and fat tissues. By activating peroxisome proliferator-activated receptors (PPARs), they play a vital role in how our bodies manage glucose and lipids. Many patients find that TZDs can lower A1C levels by about 0.5-1.5%, making them especially useful for those dealing with insulin resistance, and they are often used as A1C lowering medications.
It’s important to recognize that managing diabetes is not just about medication; it’s about a comprehensive, personalized approach. This means considering TZDs as part of a broader functional medicine strategy. By understanding your unique wellness profile, including your lifestyle choices and genetic factors, we can work together to optimize your treatment outcomes.
For instance, incorporating regular physical activity, making dietary adjustments, and practicing stress management techniques can significantly enhance the effectiveness of TZDs. While these medications can be beneficial, some individuals may experience weight gain and fluid retention. This highlights the importance of careful monitoring and making necessary adjustments alongside these lifestyle modifications.
Remember, you are not alone on this journey. Many patients have found success by integrating these strategies into their daily lives. As you consider the path ahead, think about how these changes can lead to a healthier, more fulfilling life. Your commitment to this process can make a meaningful difference in managing your diabetes.
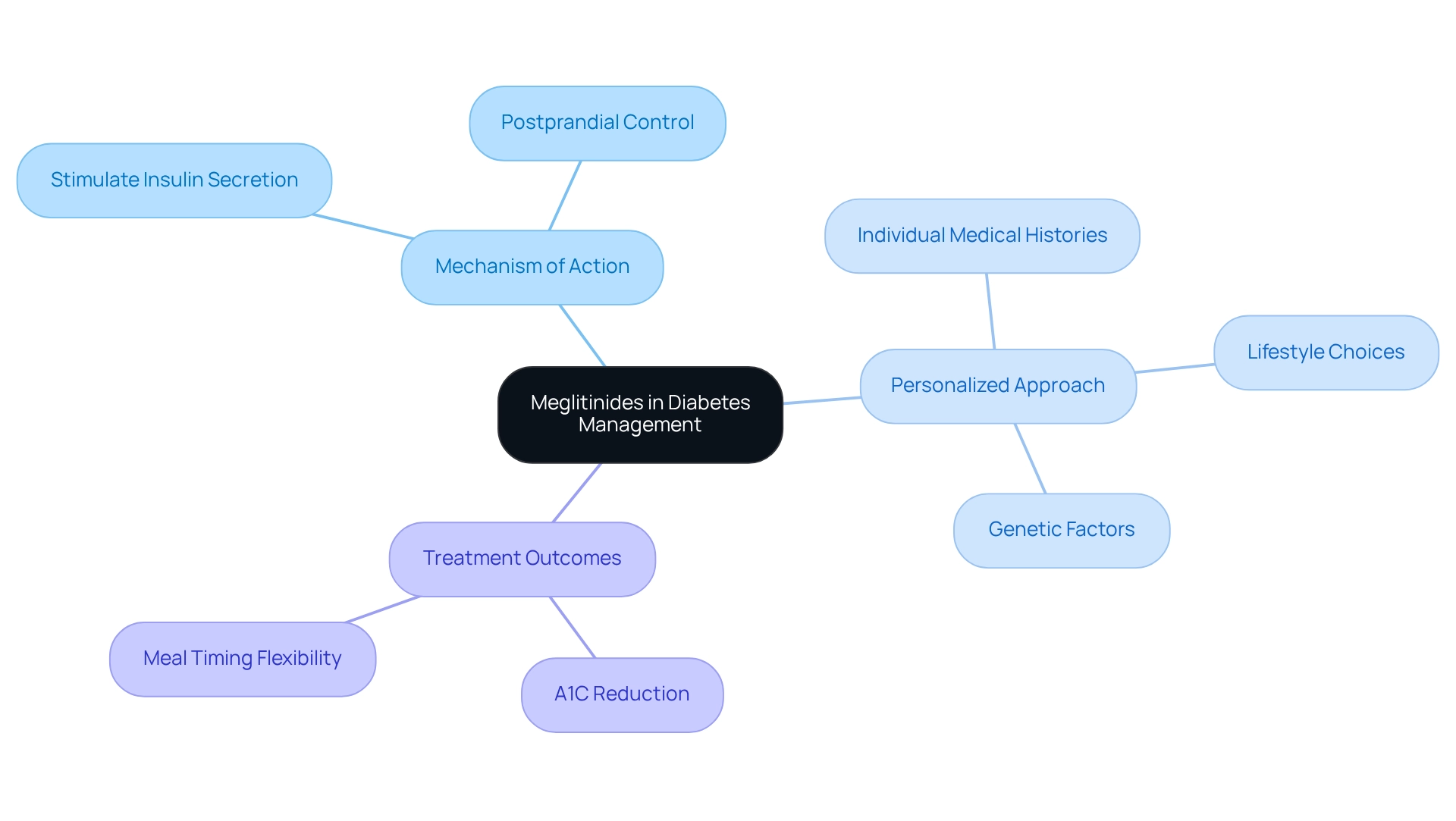
Meglitinides: Quick Action for Post-Meal Blood Sugar Control
Managing diabetes can feel overwhelming, especially when it comes to controlling blood sugar levels. Meglitinides, like repaglinide and nateglinide, offer a supportive option for many individuals. These fast-acting oral medications stimulate insulin secretion from the pancreas in response to meals, helping to control those pesky postprandial blood sugar spikes. This can be particularly valuable for patients who experience significant fluctuations after eating.
It’s important to recognize that every patient’s journey is unique. In a personalized approach to diabetes management, incorporating meglitinides into a comprehensive treatment plan can make a real difference. By considering individual medical histories, lifestyle choices, and even genetic factors, healthcare practitioners can tailor the use of these medications effectively. Comprehensive assessments and diagnostic tests guide this personalized strategy, ensuring that each person receives the care they truly need, and many patients find that A1C lowering medications, such as meglitinides, can reduce A1C values by approximately 0.5-1%. Typically taken right before meals, their rapid action provides meal timing flexibility—a crucial aspect for those with varying schedules. This adaptability can be beneficial, especially when the medication is tailored to fit individual health profiles. Keep in mind that you are not on this journey by yourself; there are resources available to assist you in managing your diabetes more efficiently.
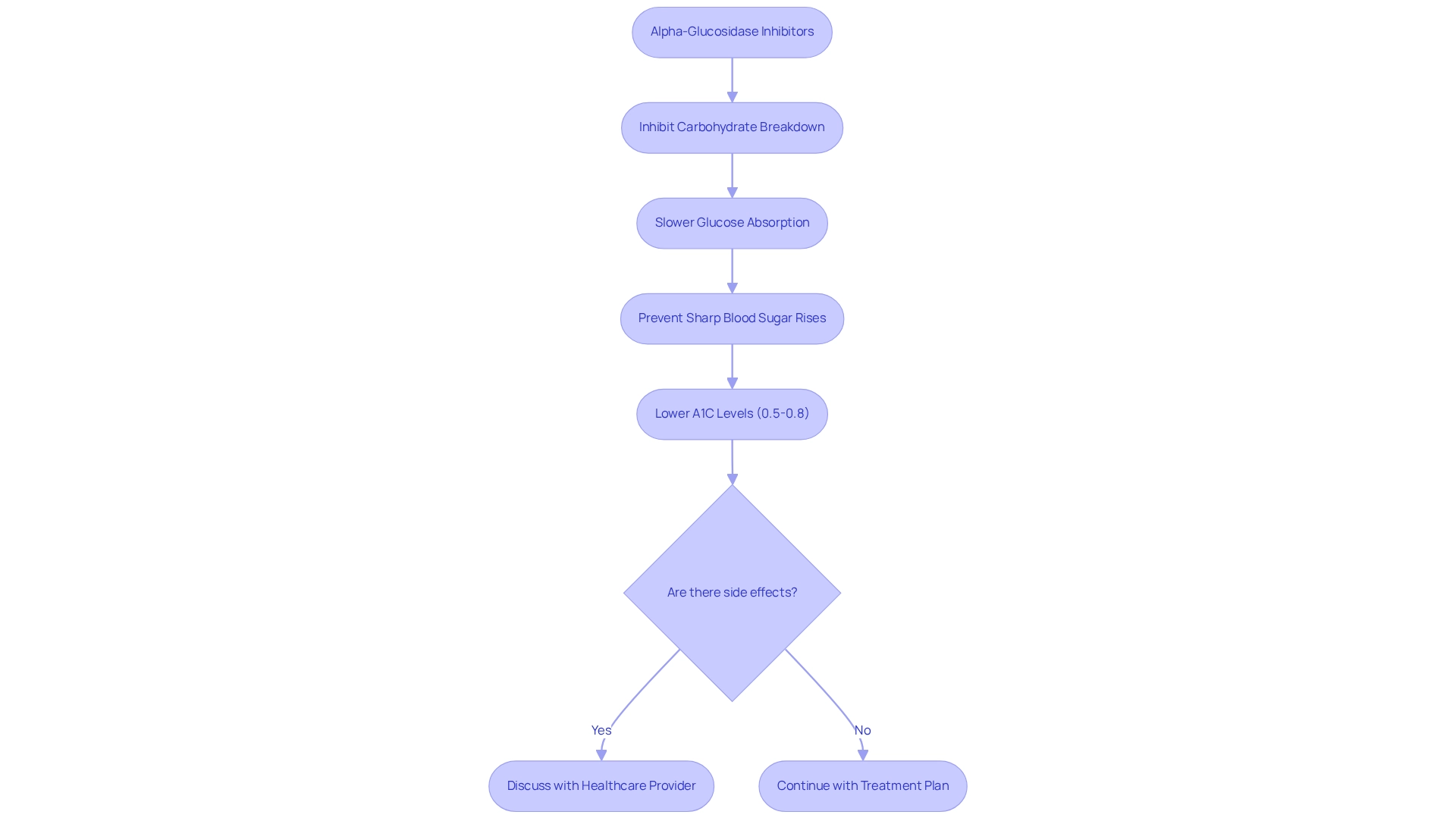
Alpha-Glucosidase Inhibitors: Slowing Carbohydrate Absorption
Managing blood sugar levels can be a challenging journey, and medications like alpha-glucosidase inhibitors—such as acarbose and miglitol—offer valuable support. These medications work by inhibiting enzymes that break down carbohydrates in the intestines, which helps slow the absorption of glucose. This mechanism is particularly helpful in preventing sharp rises in blood sugar concentrations after meals, allowing for a more stable experience throughout the day. Many patients find that A1C lowering medications can lower their A1C levels by approximately 0.5-0.8%, typically taken with the first bite of a meal.
However, it’s important to recognize that some individuals may experience gastrointestinal side effects, such as gas and bloating. Discussing these concerns with a healthcare provider is crucial, as they can provide guidance and support tailored to your needs.
In the context of a personalized approach to managing blood sugar levels, it’s essential to consider how A1C lowering medications can be integrated into a customized treatment plan. Each individual has a unique health profile, lifestyle choices, and underlying factors contributing to their condition. This holistic perspective encompasses thorough evaluations and diagnostic examinations, which assist in recognizing your specific requirements and circumstances.
Together, we can ensure an effective management approach that truly supports your journey toward better health.
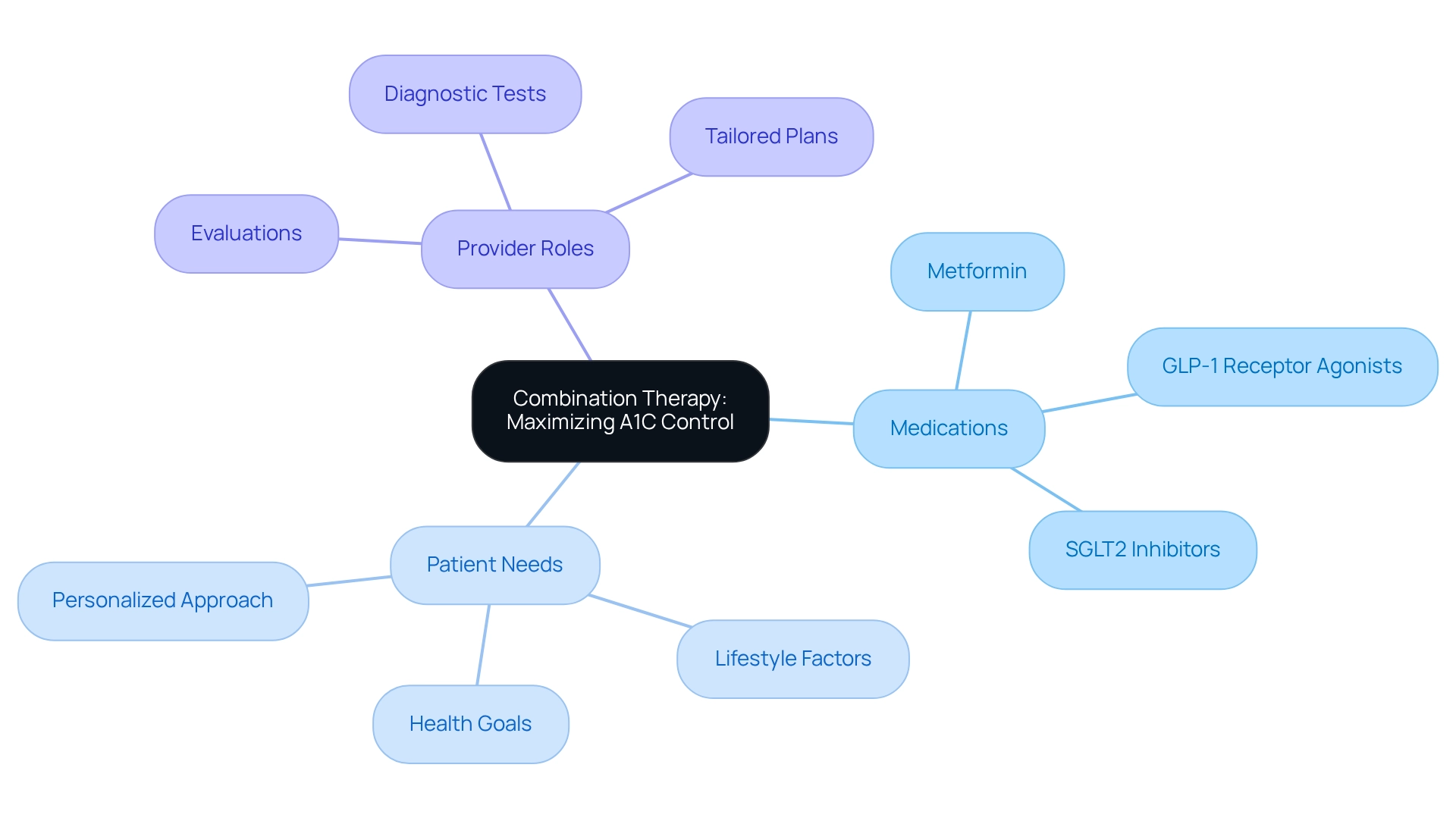
Combination Therapy: Maximizing A1C Control
Combination therapy can be a game-changer for those managing diabetes. Have you ever felt frustrated when a single medication just doesn’t seem to do the trick? This approach, which involves using two or more A1C lowering medications, aims to achieve better glycemic control than what one agent can provide. It’s especially beneficial for patients who haven’t yet reached their A1C goals with monotherapy, as many patients find that pairing metformin with a GLP-1 receptor agonist or an SGLT2 inhibitor, which are A1C lowering medications, not only improves blood sugar regulation but also helps with weight management and cardiovascular health. It’s important to recognize that this strategy aligns beautifully with the principles of integrative functional medicine, which emphasizes a personalized approach to managing blood sugar conditions.
Healthcare providers play a crucial role here. By performing thorough evaluations and diagnostic tests, they can gain a deeper understanding of individual wellness profiles. This includes recognizing how lifestyle choices and genetic factors impact blood sugar management. By working closely with patients, providers can develop a tailored combination therapy plan that considers unique health needs, potential side effects, and the use of A1C lowering medications. Ultimately, this comprehensive strategy addresses both the symptoms and the underlying causes of type 2 diabetes, offering hope and support to those on this journey. Remember, you’re not alone in this; there are effective strategies available that can truly make a difference in your health.
Conclusion
Managing diabetes can feel overwhelming, but it’s important to recognize that you’re not alone on this journey. The Integrative Wellness Center’s 30-Day Diabetes Reset Program is designed with you in mind, combining dietary education, physical activity, and behavioral coaching to empower you to take control of your health. Many participants find that by fostering sustainable lifestyle changes, they can stabilize their glucose levels and reduce reliance on medications, leading to a greater sense of well-being.
Medications like metformin, GLP-1 receptor agonists, and SGLT2 inhibitors play crucial roles in diabetes management. Each treatment offers unique benefits, from lowering A1C levels to providing cardiovascular support. When integrated into a functional medicine framework, these options become part of a comprehensive strategy tailored to your individual health profile, lifestyle choices, and genetic factors. This holistic approach not only addresses symptoms but also targets the root causes of diabetes, paving the way for long-term health improvements.
Ultimately, successful diabetes management hinges on collaboration between you and your healthcare providers. By embracing a personalized, integrative approach that incorporates both lifestyle modifications and advanced treatment options, you can navigate your diabetes journey with confidence. This empowers you to make informed decisions that lead to better health outcomes and a brighter future. As knowledge and resources continue to expand, it is essential to stay informed and proactive in your care, ensuring you are equipped to thrive in your health journey.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program?
The 30-Day Diabetes Reset Program is a transformative initiative at the Integrative Wellness Center designed to support individuals in managing their diabetes. It combines dietary education, physical activity, and behavioral coaching to foster sustainable lifestyle changes.
What are the main components of the program?
The program includes dietary education, physical activity, and behavioral coaching, which together equip participants with the tools and knowledge needed for effective diabetes management.
How does the program help individuals manage their blood sugar levels?
The program teaches participants to recognize and eliminate foods that raise blood sugar levels, encourages consistent exercise, and helps create a customized action plan for long-term well-being.
Can participants expect to reduce their reliance on medication?
Many participants envision a life where they maintain glucose balance without relying heavily on insulin and medication, making this a reachable goal through the program.
What medication is commonly prescribed for managing type 2 diabetes?
Metformin is often the first choice for new patients managing type 2 diabetes as it reduces hepatic glucose production and enhances insulin sensitivity.
What are the benefits of taking Metformin?
Metformin can lower A1C levels by approximately 1-2% and has a favorable safety profile with minimal risk of hypoglycemia when used alone.
What other resources are available for diabetes management?
Dr. Jason Shumard offers comprehensive resources, including a book on functional medicine strategies for type 2 diabetes and thyroid dysfunction, which many patients have found helpful.
What are GLP-1 receptor agonists and how do they work?
GLP-1 receptor agonists, such as liraglutide and semaglutide, are A1C lowering medications that stimulate insulin secretion after meals, suppress glucagon release, and slow gastric emptying.
What additional benefits do GLP-1 receptor agonists provide?
These medications can reduce A1C levels by 1-2%, promote weight loss, and lower the risk of cardiovascular events, making them beneficial for individuals with type 2 diabetes.
How does functional medicine approach diabetes management?
Functional medicine considers a patient’s unique medical history, lifestyle choices, and genetic factors to create tailored treatment plans, often utilizing assessments like metabolic panels and genetic testing for sustainable diabetes management.