Overview
The GMI percentage, or Glucose Management Indicator, plays a vital role in diabetes management. It offers a more immediate reflection of blood sugar levels compared to traditional HbA1c measurements. This allows for timely adjustments in treatment plans, which can make a significant difference in your daily life.
It’s important to recognize that understanding your glucose levels can feel overwhelming at times. The article highlights how GMI, calculated from continuous glucose monitoring data, empowers individuals to take charge of their health. Many patients find that this tool helps them better understand their glucose patterns, leading to more informed decisions.
However, it’s crucial to interpret GMI alongside other metrics. There may be discrepancies with HbA1c results, and considering all aspects of your health is essential. Remember, you’re not alone in this journey; many are navigating similar challenges. Together, we can work towards a healthier future.
Introduction
In the journey of managing diabetes, many individuals face challenges that can feel overwhelming. The Glucose Management Indicator (GMI) stands out as a valuable tool, offering real-time insights that can significantly change how you monitor your health. Unlike traditional metrics like hemoglobin A1c (HbA1c), which may hide important fluctuations in glucose levels, GMI provides a more immediate and dynamic picture of your glycemic control.
As continuous glucose monitoring (CGM) systems become more popular among diabetes patients, it’s important to recognize that understanding GMI can empower both patients and healthcare providers. This article will explore the significance of GMI, how it is calculated, and its potential to help you take charge of your health journey. We’ll also discuss its limitations and the importance of a personalized approach to diabetes care. With the right knowledge and tools, you can reclaim your health and enhance your overall well-being.
Understanding the Glucose Management Indicator (GMI)
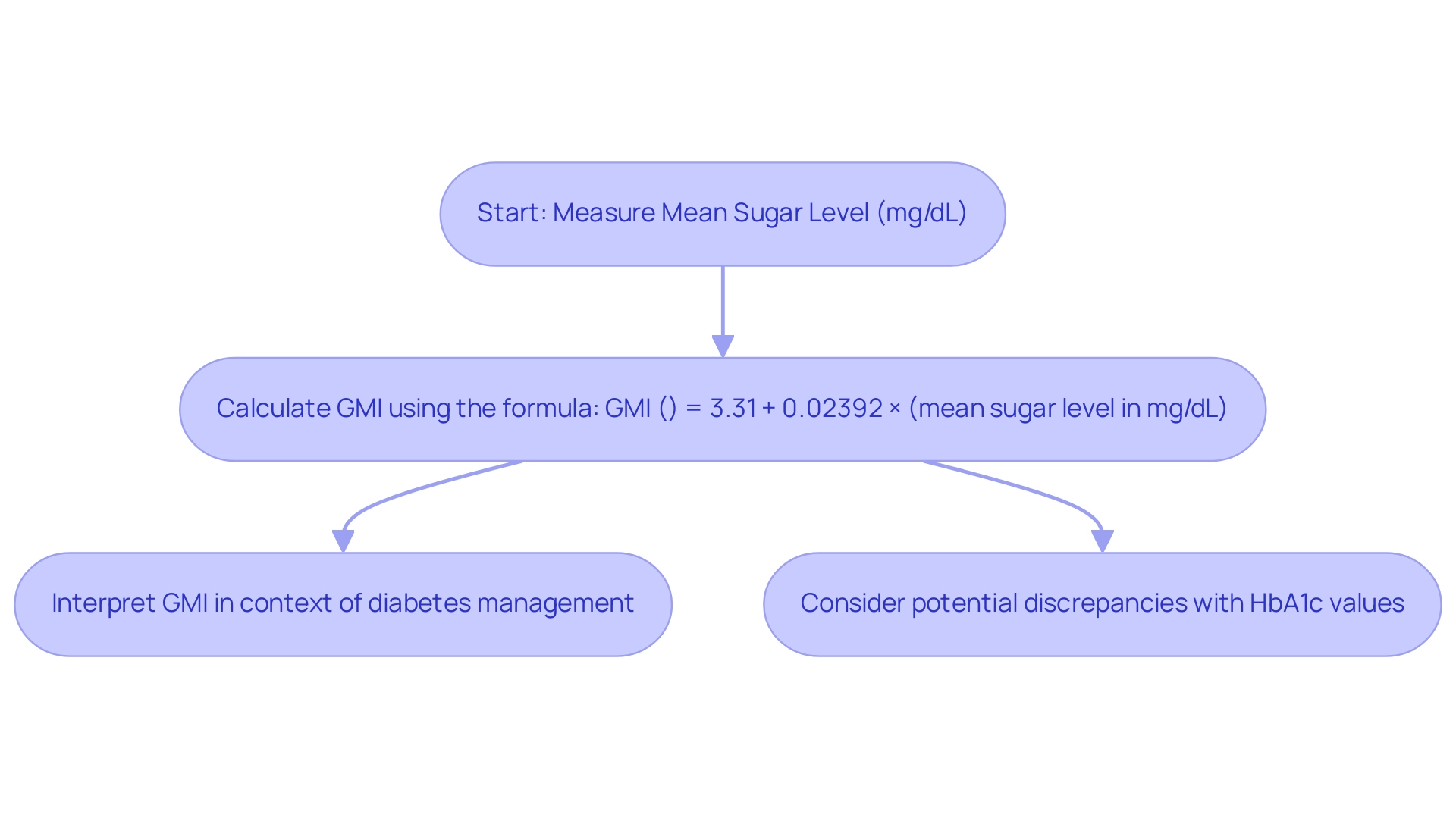
The Glucose Management Indicator (GMI) is an evolving metric that plays a crucial role in understanding blood sugar levels over time. By utilizing data from continuous glucose monitoring (CGM) systems, GMI helps answer the important question of what is GMI percentage. This innovative measure approximates the hemoglobin A1c (HbA1c) level, a traditional benchmark for assessing long-term sugar control. The formula for calculating GMI percentage is straightforward:
GMI (%) = 3.31 + 0.02392 × (mean sugar level in mg/dL).
It’s important to recognize that this calculation highlights the GMI’s relevance, as it offers a more immediate reflection of sugar levels compared to HbA1c, which typically represents an average over the preceding two to three months. Many patients find that understanding GMI provides them with a clearer picture of their health.
Recent studies indicate a significant number of patients with blood sugar issues are turning to CGM systems, enhancing their ability to monitor glucose fluctuations in real-time. The HypoDE study, which examined CGM data from 141 individuals with type 1 diabetes over four weeks, underscores the growing reliance on this technology for effective management.
Understanding what is GMI percentage is essential for managing blood sugar levels. It serves as a vital tool for both individuals and healthcare providers, facilitating informed decisions regarding treatment adjustments. However, recent research raises questions about GMI as an accurate estimate of HbA1c, with findings suggesting that a notable percentage of participants exhibit clinically significant discordance between GMI and laboratory HbA1c results.
This discrepancy emphasizes the need for careful interpretation of GMI data in clinical settings, as it may not always align with traditional HbA1c measurements. Experts advocate for the broader adoption of the GMI term within the global diabetes community, highlighting its potential to enhance diabetes management strategies.
By offering actionable insights into glucose levels, GMI empowers individuals to take control of their health. This approach aligns with the holistic philosophy championed by healthcare professionals like Dr. Jason Shumard at Integrative Wellness Center. Dr. Shumard emphasizes the importance of tailored care, stating, “By offering individuals actionable insights and practical tools, the center cultivates an environment where people can reclaim their health and well-being.”
Through education and personalized lifestyle changes, individuals can better understand their conditions and make informed choices that enhance their overall well-being. Remember, taking small steps towards understanding your health can lead to significant improvements in your life.
The Importance of GMI in Diabetes Management
In diabetes management, understanding what GMI percentage is crucial. It offers real-time insights into sugar levels, enabling prompt modifications to treatment plans. Unlike HbA1c, which can obscure fluctuations in blood sugar levels, grasping the concept of GMI percentage provides a more dynamic view of an individual’s glycemic control. This is particularly beneficial for those using continuous monitoring (CGM) devices, as they can consistently track their GMI percentage and make informed decisions regarding diet, exercise, and medication.
Focusing on GMI percentage allows individuals to better comprehend their sugar patterns, helping them keep their levels within the target range. This proactive approach not only leads to better health outcomes but also significantly lowers the risk of complications associated with diabetes. For instance, a retrospective study revealed that individuals transitioning from self-monitoring of blood sugar to CGM experienced a significant reduction in mean HbA1c levels from 11.21% to 7.04%, alongside a decline in average blood sugar levels from 286 mg/dl to 158 mg/dl.
Additionally, the mean System Usability Scale (SUS) score at baseline was 72.4, which improved to 74.8 at 12 weeks, indicating enhanced usability of CGM devices. Such findings highlight the transformative potential of GMI, particularly in managing blood sugar conditions.
Moreover, the ability to monitor glucose levels in real-time empowers individuals to make immediate adjustments to their lifestyle and treatment regimens. This adaptability is essential, as it allows for a personalized approach to health management, ultimately fostering a greater sense of control over their well-being. As Dr. Jason Shumard emphasizes, “By providing individuals with actionable insights and practical tools, the Integrative Wellness Center fosters an environment where people can reclaim their health and well-being.”
This comprehensive focus on GMI percentage not only enhances client engagement but also contributes to a more effective diabetes management strategy. The success stories of patients like A.A., who transformed their health through Dr. Shumard’s 30-Day Diabetes Reset program, illustrate the profound impact of this approach, showcasing significant improvements in energy levels, weight loss, and overall well-being. To learn more about how the Integrative Wellness Center can support your health journey, explore our treatment options today.
How is GMI Calculated?
Understanding what GMI percentage means can feel overwhelming, but it’s essential for managing diabetes effectively. The Management Indicator (GMI) is calculated using average levels obtained from a continuous glucose monitor (CGM) over a period of about 14 days. The formula is:
- GMI (%) = 3.31 + 0.02392 × (mean sugar in mg/dL).
For example, if your mean glucose level is 150 mg/dL, your GMI would be approximately 6.9%.
This calculation is not just a number; it serves as a valuable tool for estimating your expected HbA1c level. By understanding your GMI percentage, you gain a clearer and more immediate reflection of your glycemic control compared to traditional lab tests.
In clinical practice, knowing your GMI percentage is crucial for effective diabetes management. By comparing your current GMI values with past readings, healthcare providers can track your progress and adjust treatment plans as needed. This ongoing evaluation is especially important because time in hyperglycemia (TIHyper) Level 2, which is when sugar levels exceed 250 mg/dL, can significantly impact your overall health.
As Dr. Jason Shumard emphasizes, “By providing individuals with actionable insights and practical tools, the Integrative Wellness Center fosters an environment where people can reclaim their health and well-being.”
Moreover, you can refine your GMI calculation by examining the variability in your sugar levels through statistical measures like standard deviation (SD) and coefficient of variation (CV). Lower SD and CV values indicate more stable blood sugar levels, which are beneficial for managing your condition effectively. These metrics offer a clearer picture of your glucose control, allowing for more personalized interventions.
Comprehending how these variability metrics relate to your GMI percentage can enhance your overall management approach. To effectively monitor and improve your progress, consider using various tracking methods, such as fitness apps, journals, and pedometers. Setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost your focus and motivation. For instance, you might aim to maintain your GMI below a certain level or gradually increase your physical activity.
Research has shown that persistence in goal-setting can positively impact performance; for example, scores improved from 3.4 (SD = 2.0) to 3.8 (SD = 1.9) in specific conditions, highlighting the effectiveness of structured goal-setting. Regularly reviewing your progress not only fosters accountability but also allows you to adapt your goals as your health conditions change. This structured approach, as research suggests, can lead to improved performance and a greater sense of achievement.
Experts emphasize the importance of understanding your GMI percentage in integrating GMI calculations into diabetes management studies. By utilizing CGM data, researchers can gain insights that enhance the understanding of glycemic patterns and guide best practices in care. As methodologies for calculating GMI continue to evolve, staying informed about the latest techniques and expert insights is vital for both you and your healthcare providers.
The Integrative Wellness Center’s holistic approach to health, which prioritizes personalized care and education over mere symptom management, underscores the significance of GMI in a comprehensive care strategy.
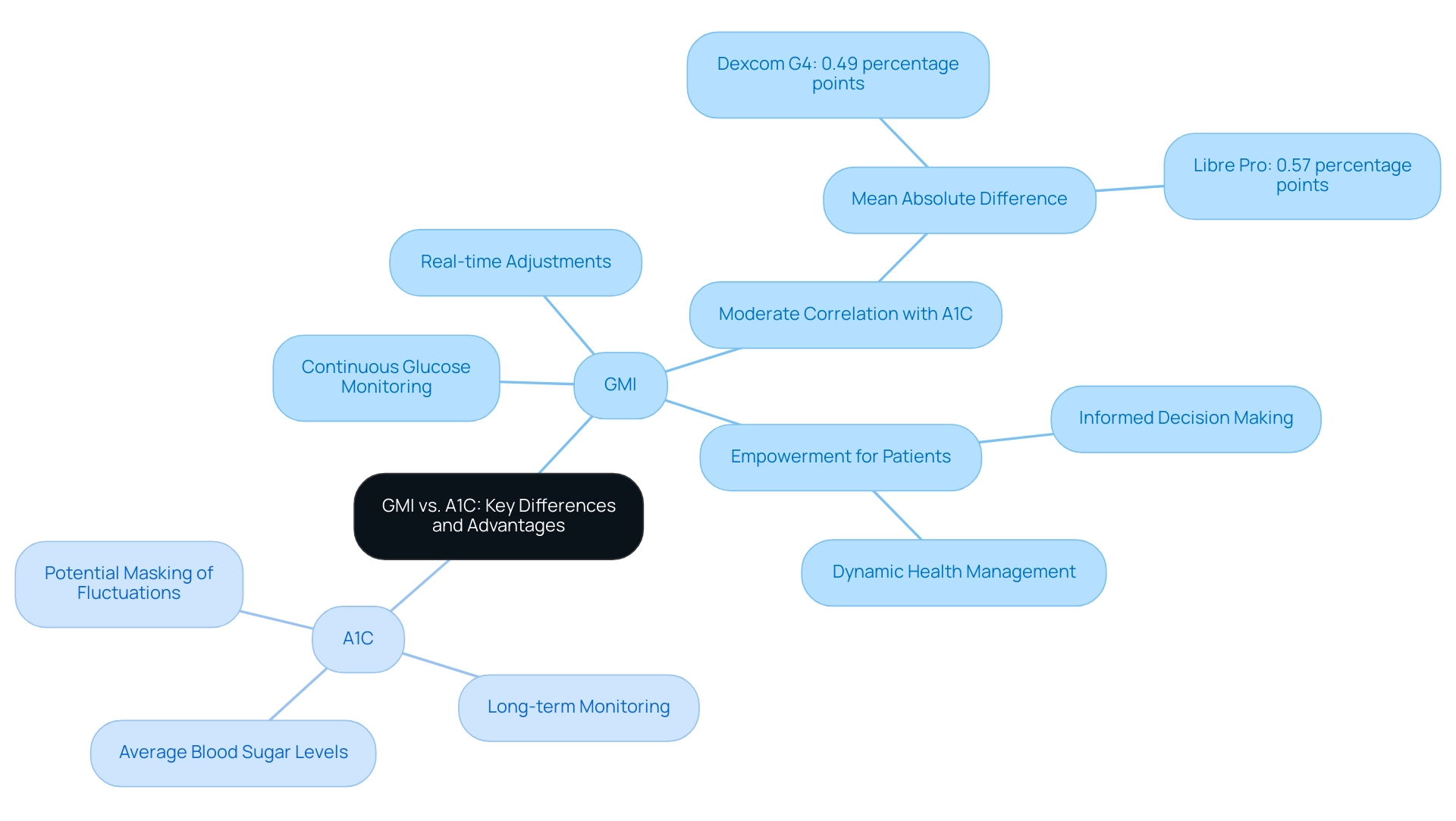
GMI vs. A1C: Key Differences and Advantages
GMI and A1C are crucial metrics in assessing blood sugar control, and understanding what GMI percentage means is essential, especially since they differ significantly in their methodologies and implications for diabetes management. A1C reflects average blood sugar levels over the past two to three months, which can sometimes mask short-term fluctuations that are vital for effective management. In contrast, GMI percentage provides a more immediate estimate derived from recent continuous glucose monitoring (CGM) data, allowing for real-time adjustments to treatment plans.
This capability empowers patients to monitor their sugar levels more frequently and respond to changes promptly, making GMI an invaluable tool for those striving to enhance their condition management.
Recent studies have highlighted the performance of GMI in relation to A1C. For example, a study examining GMI’s effectiveness in adults with type 2 diabetes and obstructive sleep apnea found that GMI was only moderately correlated with A1C, with significant discrepancies noted in over one-third of participants. The mean absolute difference between HbA1c and GMI was found to be 0.49 percentage points for Dexcom G4 and 0.57 percentage points for Libre Pro.
This finding suggests that while GMI can offer timely insights, it is crucial to grasp what GMI percentage entails, as it may not always align perfectly with A1C results. This highlights the importance of using both metrics together for a comprehensive view of glycemic control.
Moreover, the benefits of GMI extend beyond just the frequency of measurement. Patients utilizing GMI can make informed decisions based on their current glucose levels, which is especially beneficial for those facing variable blood sugar patterns. This dynamic nature of GMI empowers individuals to take control of their health, resonating with Dr. Jason Shumard’s dedication to providing actionable insights and practical tools for diabetes management.
Given the concerning statistics regarding hospital safety—such as 7,000 incorrect medications and 80,000 infections acquired in hospitals—Dr. Shumard emphasizes the necessity for personalized functional medicine approaches that prioritize individual safety and well-being. As Dr. Shumard states, “By providing individuals with actionable insights and practical tools, the Integrative Wellness Center fosters an environment where people can reclaim their health and well-being.”
By creating a space where individuals can actively engage with their health information, GMI enhances the overall quality of care for those managing blood sugar issues. Feedback from individuals at the Integrative Wellness Center emphasizes transformative health journeys, illustrating how customized care has led to better management of their condition and overall well-being.
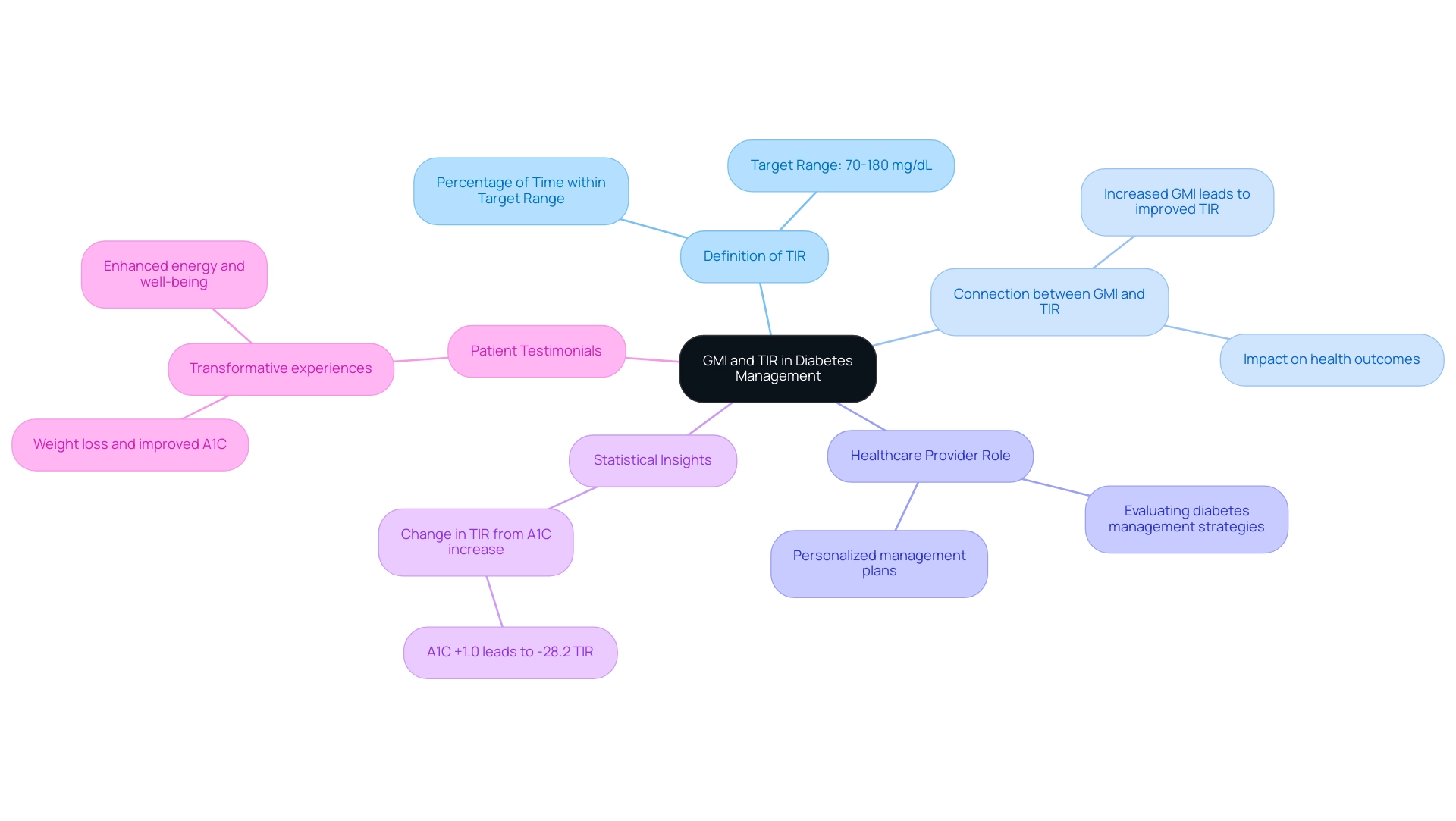
Connecting GMI and Time in Range (TIR)
Time in Range (TIR) is a crucial measure for managing blood sugar levels, reflecting the percentage of time an individual’s sugar levels remain within a target range, typically between 70 and 180 mg/dL. It’s important to recognize that research shows a strong connection between the Glucose Management Indicator (GMI) and TIR. Understanding the GMI percentage often signifies that patients are spending more time within this optimal glucose range. This relationship holds significant importance, as a decrease in GMI can lead to improved TIR, ultimately enhancing health outcomes for those facing blood sugar challenges.
Healthcare providers rely on both GMI and TIR to evaluate the effectiveness of diabetes management strategies. By focusing on these metrics, individuals can cultivate a deeper understanding of their glucose control, which is essential for creating personalized management plans. For instance, a recent analysis revealed that an increase in A1C by just 1.0% could lead to a notable decrease of 28.2% in TIR for individuals with a baseline A1C of 8.0% or higher. This statistic underscores the necessity of monitoring GMI, particularly the GMI percentage, as a means to improve TIR and, consequently, overall health.
Many patients find that understanding Continuous Glucose Monitoring (CGM) reports is vital, especially in the context of telemedicine. Mark Harmel, a Care and Education Specialist for Diabetes, emphasizes that while traditional A1C goals are often highlighted, the new data available in the Ambulatory Glucose Profile (AGP) report allows for a more tailored management plan. This shift towards individualized care resonates with Dr. Jason Shumard’s holistic approach, which champions individual empowerment through actionable insights and practical tools.
Transformative experiences further illustrate the connection between GMI and TIR in diabetes management. One individual shared, “I was in a ‘cookie cutter’ treatment that was not working for me. When I started this program, the Doctor gave great personal attention and care in helping fix my condition. I lost 55 lbs. My A1C started at 9.1 after 8 months it is now 5.7. Fasting glucose was at 133 and now it is at 85.”
Another individual noted, “I feel so much better… I lost a lot of weight, have more energy and feel great. I am not depressed anymore and I don’t need my meds anymore!!!” These heartfelt testimonials highlight how understanding and managing GMI and TIR can lead to significant improvements in health and well-being, aligning with Dr. Shumard’s commitment to holistic care and the success of the 30-Day Diabetes Reset program.
In summary, grasping the GMI percentage and its relationship with TIR is vital for effective management of diabetes. By prioritizing these metrics, individuals can achieve better health outcomes and reclaim their well-being, reflecting the holistic philosophy championed by Dr. Jason Shumard.
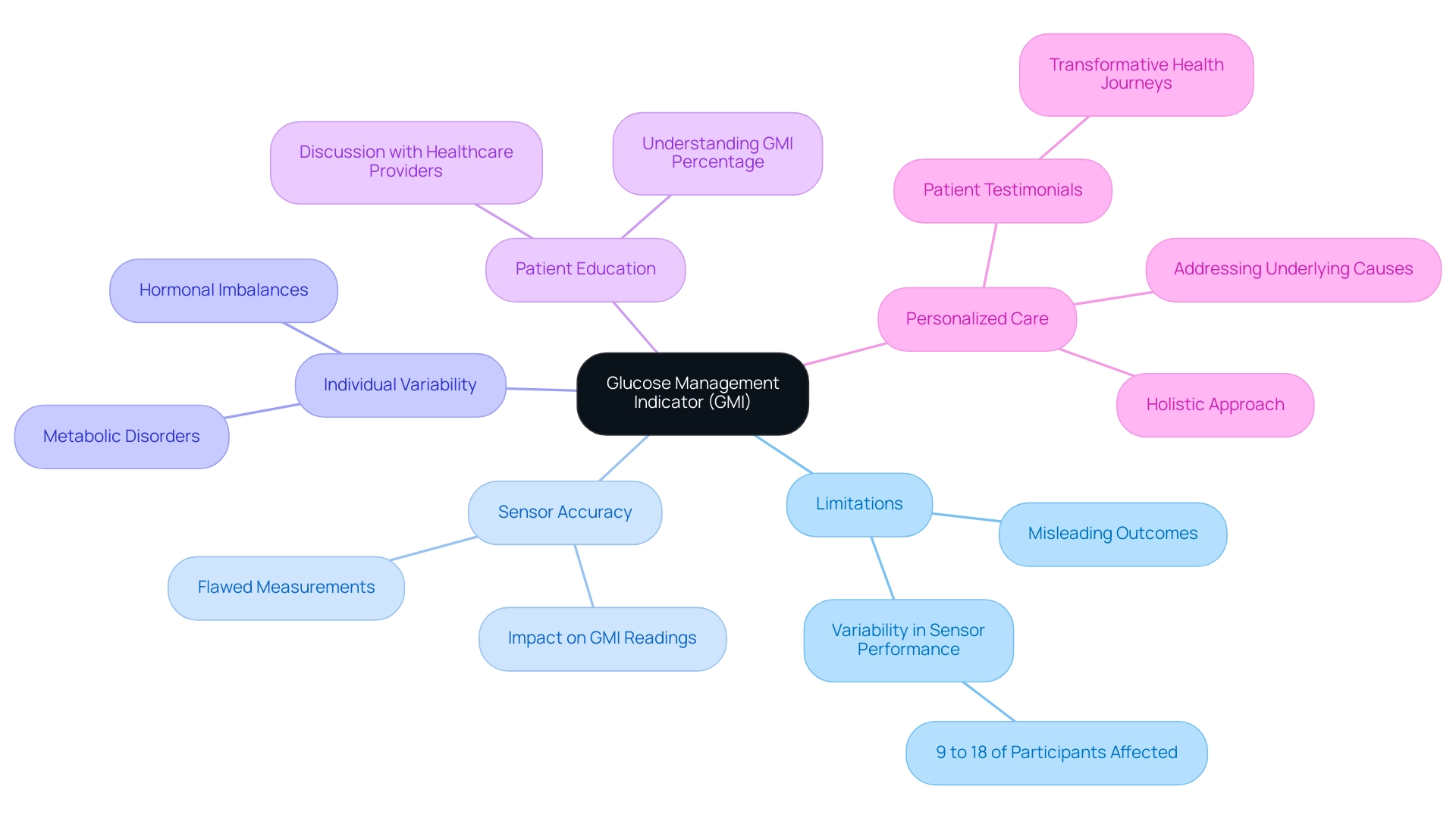
Limitations and Considerations of GMI
While the Glucose Management Indicator (GMI) provides valuable insights into diabetes management, it’s important to understand what the GMI percentage is and its limitations. GMI is derived from Continuous Glucose Monitoring (CGM) data, which can be significantly affected by sensor accuracy. Flawed measurements can lead to misleading GMI outcomes, complicating the analysis of a person’s sugar management.
For instance, studies have shown that between 9% and 18% of participants experienced an absolute difference greater than 1 percentage point (>11 mmol/mol), highlighting the variability in sensor performance. Many patients find that this inconsistency can be frustrating and confusing.
Moreover, individual differences in sugar metabolism can further complicate the reliability of GMI. Certain medical conditions, such as hormonal imbalances or metabolic disorders, may distort sugar levels, making GMI less relevant for some individuals. Therefore, it is crucial for individuals to engage in discussions with their healthcare providers about what the GMI percentage means for them.
This dialogue should encompass a comprehensive understanding of glucose management, including the GMI percentage alongside other metrics like A1C and Time in Range (TIR). It’s important to recognize that every patient’s journey is unique, and understanding these metrics can empower them to take control of their health.
Real-world examples illustrate the challenges faced in interpreting GMI data. Patients may find themselves confused by fluctuating GMI readings that do not align with their daily experiences or symptoms. This highlights the necessity for personalized care, as emphasized by Dr. Jason Shumard, who advocates for actionable insights and practical tools to empower individuals in their health journeys.
Dr. Shumard’s holistic approach, which focuses on treating the underlying causes of chronic conditions, enhances the effectiveness of management strategies for this illness. His dedication to addressing the dangers of traditional treatments for blood sugar conditions, including the risks of elevated insulin levels, is vital in promoting a safer healthcare environment. This is especially important considering concerning statistics related to hospital safety, such as the 7,000 incorrect medications administered to individuals and 80,000 infections contracted in healthcare facilities.
Patient testimonials reflect transformative health journeys at Dr. Shumard’s Functional Medicine Center, showcasing the positive impact of personalized functional medicine approaches to managing blood sugar. For instance, one individual shared, “Dr. Shumard’s guidance helped me understand my condition better and take control of my health.” By fostering an environment of education and support, patients can better navigate the complexities of managing their condition.
In summary, while GMI serves as a useful tool, understanding the GMI percentage and its limitations necessitates a cautious approach. Sensor accuracy, individual variability, and the need for comprehensive discussions with healthcare providers are critical considerations for effective management of the condition. Future research should also record the cost-effectiveness of CGM and its effect on health outcomes for various populations, emphasizing the significance of a comprehensive and individualized approach to managing this condition.
Practical Applications of GMI in Daily Diabetes Management
To effectively integrate your understanding of what GMI percentage means into the daily management of your condition, it’s essential to regularly track your continuous glucose monitoring (CGM) data and compute your GMI at least every two weeks. Maintaining a detailed log of GMI values alongside your dietary choices and physical activity can reveal patterns and triggers that influence your glucose levels. This practice not only helps you understand your individual responses but also empowers you to make informed adjustments to your diabetes care plan.
Implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly enhance this process. For instance, you might set a goal to keep your GMI within a specific range over the next month or to gradually increase your physical activity each week. It’s important to collaborate with your healthcare providers; working together with your doctor to establish personalized glucose targets based on your GMI percentage and time in range (TIR) data is vital.
This tailored approach ensures that your management strategies align with your individual health goals. Furthermore, engaging in educational resources—such as seminars, workshops, and Dr. Shumard’s insightful publications—can greatly enhance your understanding of what GMI percentage entails and how it can be practically applied in your diabetes management. By actively participating in these educational opportunities, you can gain valuable insights that foster a proactive approach to your health.
Additionally, consider utilizing various tracking methods, including fitness apps, journals, and pedometers, to effectively monitor your progress. A major manufacturer has even introduced a semi-quantitative system that uses a smartphone camera to estimate glucose levels without requiring a meter, which can further assist you in understanding what GMI percentage means. Dr. Jason Shumard emphasizes, “By providing individuals with actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being.”
It’s also important to recognize that a recent case study titled “Evaluation of Glucose Management Indicator (GMI) in Type 2 Diabetes” found significant variability and discordance, raising questions about what GMI percentage means in relation to HbA1c. This suggests that patients should interpret GMI data with caution in clinical practice. This balanced perspective highlights the significance of understanding what GMI percentage is as a component of a comprehensive management strategy for blood sugar. For personalized support and to explore how we can assist you in achieving your health goals, please contact us today at DrShumard.com or call (858) 564-7081.
Key Takeaways: Embracing GMI for Better Health
The Glucose Management Indicator (GMI) is a vital metric for those managing their blood sugar levels. It offers a more immediate and accurate reflection of control compared to traditional A1C tests. GMI is derived from continuous glucose monitoring (CGM) systems, which have shown remarkable improvements in glycemic control. These improvements include decreases in HbA1c levels, average blood glucose levels, and the frequency of hypoglycemic events. As such, GMI is an essential tool in effective management strategies.
It’s important to recognize that while laboratory HbA tests typically cost around $10 each, CGM systems can accumulate costs of several hundred dollars monthly. This highlights the financial implications of diabetes management tools.
Understanding the GMI percentage and its connection to other metrics, like Time in Range (TIR), empowers individuals to take a proactive approach to their health. By embracing GMI, people can significantly enhance their ability to monitor and manage glucose levels, ultimately leading to better health outcomes. Many individuals at Dr. Jason Shumard’s center have reported substantial improvements in their overall well-being and quality of life.
For instance, one individual shared, “Since starting the GMI monitoring, I’ve felt more in control of my diabetes than ever before. My energy levels have improved, and I can enjoy activities with my family again.” Another expert noted, “CGM devices lead to significant improvements in glycemic control compared to SMBG, including reductions in HbA1c levels, average blood sugar levels, and hypoglycemic events.”
Key takeaways for patients regarding GMI include:
- GMI provides a more immediate assessment of glucose control, allowing for timely adjustments in management strategies.
- Regular discussions with healthcare providers about GMI can facilitate a more personalized approach to managing blood sugar.
- Understanding GMI can lead to improved adherence to treatment plans and better health outcomes.
The significance of GMI in health outcomes is underscored by the holistic approach at Dr. Shumard’s center, which prioritizes personalized care and education over mere symptom management. This methodology creates an environment where individuals can reclaim their health and well-being, reducing reliance on conventional medical interventions. Given the alarming statistics of 7,000 incorrect medications and 80,000 infections acquired in hospitals, the need for a more holistic and personalized approach to managing blood sugar levels is even more critical.
As individuals become more informed about GMI and its implications, they are better equipped to navigate their diabetes management journey, leading to enhanced health outcomes in 2025 and beyond. However, it is essential to note that long-term studies are needed to document the cost-effectiveness of CGM and its impact on patient health.
Conclusion
The Glucose Management Indicator (GMI) represents a meaningful step forward in diabetes management, providing a real-time and accurate insight into glucose control that goes beyond traditional A1C tests. By utilizing data from continuous glucose monitoring (CGM) systems, GMI empowers patients to make informed treatment decisions. This can lead to significant improvements in glycemic control, including reductions in HbA1c and average blood glucose levels.
It’s important to recognize that understanding GMI and its link to Time in Range (TIR) can help individuals take a more proactive approach to their health. Many patients from Dr. Jason Shumard’s center have shared their positive experiences, noting how this strategy has enhanced their energy levels and overall quality of life.
While GMI offers valuable insights, we must also consider its limitations, such as potential sensor inaccuracies and individual differences in glucose metabolism. Ongoing conversations with healthcare providers about GMI results are crucial for developing personalized diabetes management strategies.
In essence, as patients learn more about GMI, they become better equipped to manage their health. By integrating GMI into daily diabetes management, individuals can foster greater engagement and achieve more effective, personalized care. Prioritizing GMI can help patients reclaim their health and improve outcomes on their diabetes management journey.
Frequently Asked Questions
What is the Glucose Management Indicator (GMI)?
The GMI is a metric that helps understand blood sugar levels over time by utilizing data from continuous glucose monitoring (CGM) systems. It approximates the hemoglobin A1c (HbA1c) level, which is a traditional benchmark for assessing long-term sugar control.
How is the GMI percentage calculated?
The GMI percentage is calculated using the formula: GMI (%) = 3.31 + 0.02392 × (mean sugar level in mg/dL).
Why is GMI considered important in diabetes management?
GMI provides a more immediate reflection of sugar levels compared to HbA1c, which represents an average over the preceding two to three months. This helps individuals and healthcare providers make informed decisions regarding treatment adjustments.
What recent studies highlight the use of CGM systems?
The HypoDE study examined CGM data from 141 individuals with type 1 diabetes over four weeks, demonstrating the growing reliance on CGM technology for effective blood sugar management.
Are there any concerns regarding the accuracy of GMI as an estimate of HbA1c?
Yes, recent research indicates that there may be clinically significant discordance between GMI and laboratory HbA1c results, emphasizing the need for careful interpretation of GMI data in clinical settings.
How does understanding GMI empower individuals in managing their health?
By offering actionable insights into glucose levels, GMI empowers individuals to take control of their health, facilitating informed choices regarding diet, exercise, and medication.
What benefits have been observed from using CGM systems?
Individuals transitioning from self-monitoring of blood sugar to CGM have experienced significant reductions in mean HbA1c levels and average blood sugar levels, indicating improved health outcomes.
How does GMI contribute to a personalized approach to health management?
GMI allows individuals to monitor their glucose levels in real-time, enabling immediate adjustments to their lifestyle and treatment regimens, fostering a greater sense of control over their well-being.
What is the significance of tailored care in diabetes management?
Tailored care, as emphasized by healthcare professionals, provides individuals with practical tools and insights that help them reclaim their health and well-being through personalized lifestyle changes.