Overview
A normal Glucose Management Indicator (GMI) is crucial for assessing average blood sugar levels, typically calculated from continuous glucose monitoring data, and is essential for effective diabetes management. The article emphasizes that understanding GMI not only aids in personalizing treatment strategies but also empowers patients by providing real-time insights into their glucose patterns, which can lead to significant improvements in health outcomes, such as a reduction in A1C levels by an average of 1.5% within six months.
Introduction
In the realm of diabetes management, the Glucose Management Indicator (GMI) has emerged as a pivotal tool, revolutionizing how individuals monitor and understand their blood glucose levels. By converting continuous glucose monitoring (CGM) data into an estimated A1C percentage, GMI provides a more dynamic and immediate insight into glucose control compared to traditional methods. This innovative approach not only enhances patient engagement but also allows for timely adjustments in treatment and lifestyle, leading to improved health outcomes.
As advancements in CGM technology continue to unfold, the significance of GMI in personalized diabetes care becomes increasingly evident, offering a comprehensive strategy for managing this chronic condition effectively.
Understanding the Glucose Management Indicator (GMI)
The Management Indicator (GMI) serves as a critical metric for estimating an individual’s average blood sugar levels over time, leveraging data gathered from continuous monitoring (CGM) devices. This measurement converts the average sugar readings into a corresponding estimated A1C percentage through a specific calculation formula. In the context of blood sugar management, understanding what is a normal gmi is essential, as it provides a more detailed evaluation of control compared to traditional techniques.
Patients can now experience a transformation in their health management by eliminating inconvenient and costly treatment regimens, as well as avoiding exhausting sugar spikes and crashes. For example, a simulation resembling sugar patterns in 300 patients with type 1 metabolic disorder highlights the dependability of GMI in practical uses. This dynamic approach enables both patients and healthcare professionals to make timely adjustments to treatment plans and lifestyle choices, ultimately enhancing overall management outcomes.
Recent advancements in CGM technology have further solidified GMI’s role in understanding what is a normal gmi as an essential tool in fostering improved patient outcomes and facilitating proactive diabetes care. Additionally, the Poincaré Plot Analysis of BG Stability illustrates how GMI can reflect improvements in sugar management, showing that a smaller, more concentrated plot signifies better stability. As Courtney Green from Dexcom, Inc. observes, ‘GMI is a game changer in understanding sugar patterns and improving treatment outcomes for patients.’
Furthermore, studies have shown that patients utilizing GMI can reduce their A1C levels by an average of 1.5% within six months, which raises the question of what is a normal gmi and demonstrates its effectiveness in real-world scenarios. This integration of GMI into diabetes management practices is crucial for achieving optimal health results, aligning with Dr. Jason Shumard’s holistic approach to reversing type 2 diabetes and hypothyroidism through functional medicine.
How GMI is Calculated and Interpreted
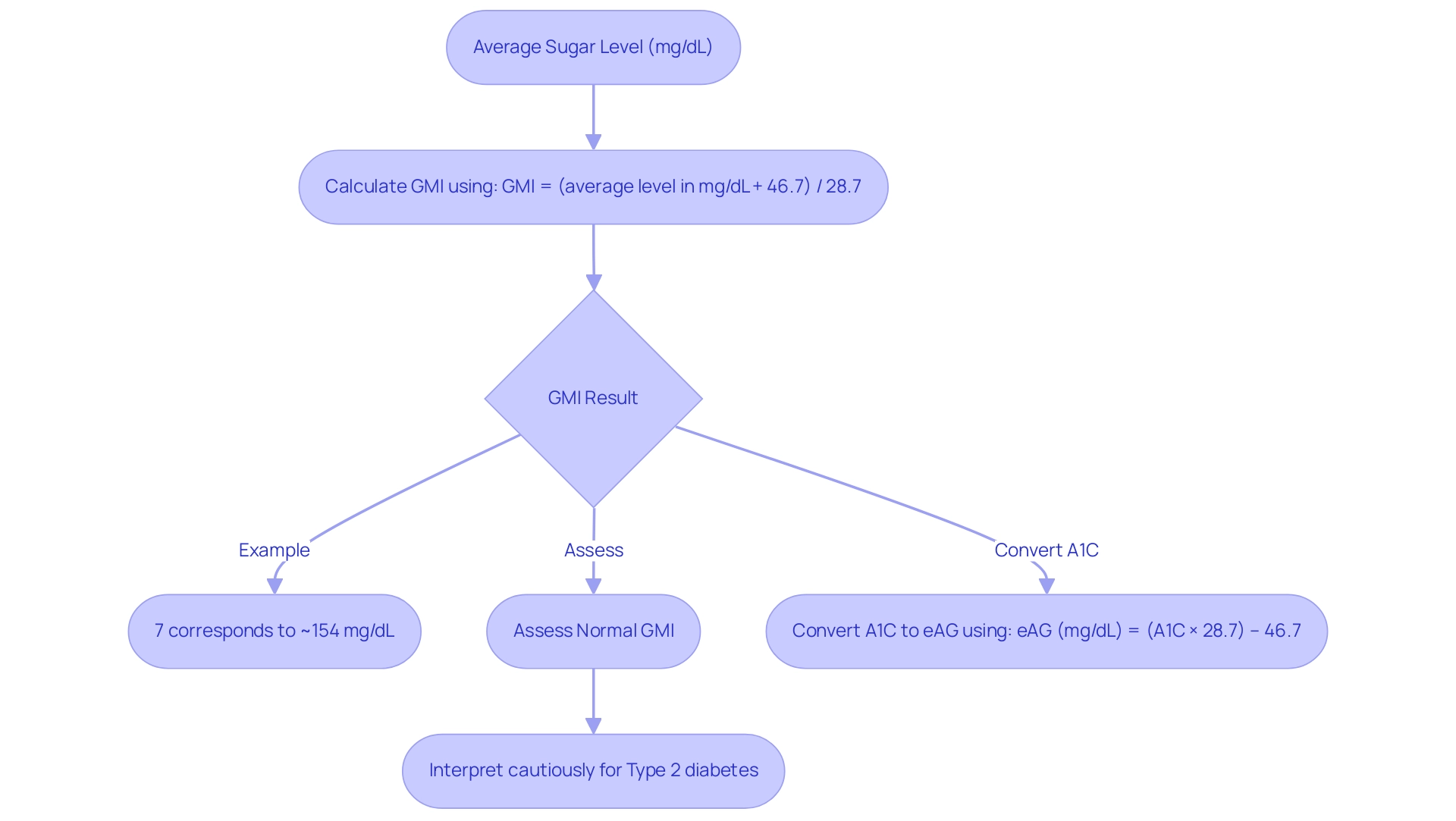
The computation of GMI (Glucose Management Indicator) is obtained from continuous monitoring data using the formula:
GMI = (average level in mg/dL + 46.7) / 28.7
This formula serves to convert the average sugar levels into an A1C-equivalent percentage, thereby facilitating a more comprehensive understanding of glycemic control. For example, a GMI result of 7% corresponds to an average sugar level of approximately 154 mg/dL.
Such a relationship is crucial for patients as it empowers them to interpret their GMI readings effectively and understand what is a normal GMI, linking these values to their overall glucose management strategies. However, it is important to note that what is a normal GMI may not be a reliable measure of glycemic control for patients with type 2 and should be interpreted cautiously in clinical practice. This caution is highlighted by a case study titled ‘GMI and A1C Value Agreement Analysis,’ which examined data from 528 individuals with blood sugar issues, emphasizing the variability between GMI and A1C values.
At the Integrative Wellness Center, we prioritize a comprehensive approach that includes understanding A1C and Estimated Average Glucose (eAG) conversions. The formula for converting A1C to eAG is:
eAG (mg/dL) = (A1C × 28.7) – 46.7
This conversion is essential for empowering patients with type 2 to manage their health effectively.
Our personalized care strategies, including tailored nutrition plans and functional medicine solutions, are designed to meet the unique needs of each individual, enhancing their overall wellness.
Comparing GMI with A1C: Key Differences and Benefits
To understand what is a normal gmi, one can look at how Glycemic Management Indicator (GMI) and Hemoglobin A1c (A1C) serve as essential tools in evaluating long-term sugar control in individuals with diabetes. However, their methodologies and implications differ significantly. A1C is a laboratory-based assessment that indicates average blood sugar levels over the preceding two to three months, providing a retrospective overview of glycemic control.
In contrast, determining what is a normal gmi is derived from real-time data collected via continuous monitoring (CGM) systems, enabling a dynamic assessment of sugar levels throughout the day. This capability to capture fluctuations in sugar levels offers a more nuanced understanding of a patient’s overall management, empowering individuals to take charge of their health. Significantly, during the COVID-19 pandemic, GMI’s role became increasingly essential as virtual consultations restricted access to conventional A1C tests, enabling healthcare providers to participate in meaningful conversations regarding average blood sugar levels.
According to Dr. Andre E. Manov, an expert in Internal Medicine, ‘Our study demonstrates a small but non-significant difference between HbA1c and GMI, which can help in the future to more precisely individualize the insulin management of patients with blood sugar disorders.’ Furthermore, participants with reduced kidney function exhibited a 0.19 percentage point greater difference between A1C and GMI, emphasizing the importance of GMI in this demographic. However, it is important to note the limitations of the study, including a small sample size and the exclusion of certain demographics, which may affect the generalizability of the results.
This real-time insight from GMI facilitates timely and personalized adjustments to treatment plans, ultimately enhancing management of blood sugar levels, particularly for patients with chronic kidney disease (CKD), where A1C may underestimate actual glucose averages. The findings underscore the necessity of using GMI to determine what is a normal GMI, especially when A1C tests are not feasible. Additionally, GMI can play a crucial role in preventing gestational conditions, highlighting the importance of education and personalized care in managing health effectively.
This holistic approach prioritizes empowering type 2 patients to eliminate insulin dependency and prevent complications during pregnancy.
The Role of GMI in Personalized Diabetes Management
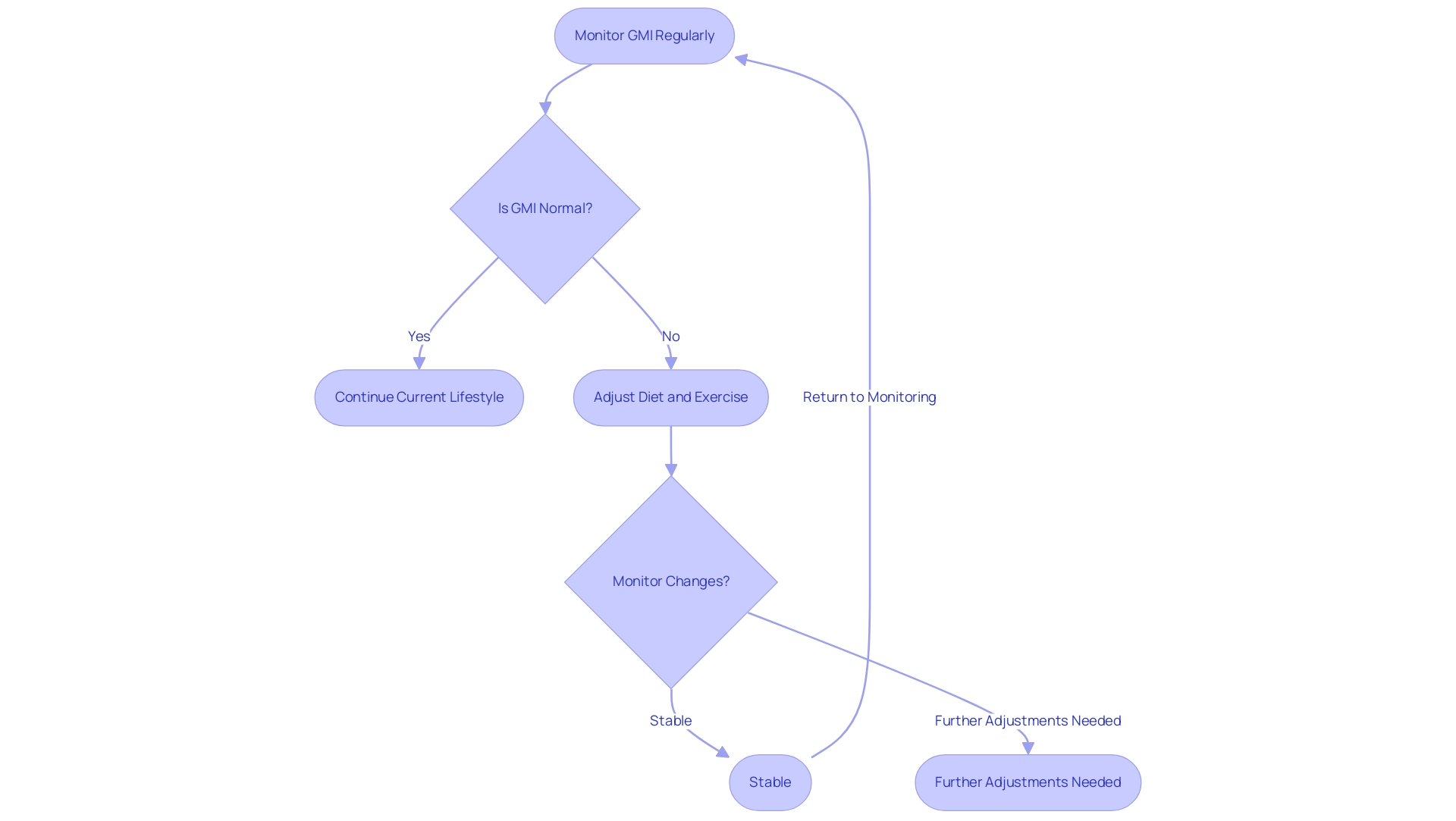
Understanding what is a normal gmi is essential as GMI serves as a cornerstone in the creation of personalized diabetes management strategies. By meticulously analyzing GMI data alongside advanced diagnostic testing, which evaluates biomarkers such as inflammation levels, insulin resistance, and gut health, healthcare professionals can discern patterns in a person’s blood sugar levels. This analysis is instrumental in customizing dietary recommendations, physical activity plans, and medication adjustments.
For instance, if a patient’s GMI consistently indicates elevated sugar levels after meals, healthcare providers may propose specific dietary modifications or recommend increased physical activity post-meal. This tailored approach not only promotes patient engagement but also fosters adherence to management strategies, culminating in improved health outcomes. Success stories, such as those from Dr. Jason Shumard’s 30-Day Diabetes Reset program, reveal transformative health improvements; patients like M.L. reported significant weight loss and substantial reductions in A1C levels, from 9.1 to 5.7, and fasting glucose levels, from 133 to 85. Significantly, 82% of Class 3 participants indicated experiencing hypertension, emphasizing the increased cardiovascular risks linked to managing diabetes-related conditions.
Dimitris Bertsimas, a prominent figure in research on blood sugar regulation, stated, ‘To our knowledge, we present the first prescriptive method for personalized type 2 care,’ emphasizing the importance of individualized treatment.
Furthermore, insights from case studies indicate that demographic factors significantly influence patient preferences, suggesting that tailored strategies must consider individual health attributes. Additionally, recent research suggests that more frequent, bidirectional communication with healthcare providers could lead to more effective improvements in HbA1c levels for managing blood sugar. Thus, leveraging GMI data is crucial for informing dietary choices and activity recommendations, which helps determine what is a normal gmi and leads to more effective management of blood sugar.
Implications of GMI for Daily Diabetes Management
The implications of Glucose Management Indicator (GMI), particularly in understanding what is a normal gmi, for daily blood sugar management are substantial. Regular monitoring of what is a normal gmi, which is approximately 17 hours out of a 24-hour day (70% of the time), allows individuals to make informed decisions regarding their dietary choices, exercise routines, and medication adherence. A GMI reading that reveals a trend of increasing glucose levels may prompt an individual to reduce carbohydrate intake or enhance physical activity to mitigate these fluctuations.
A study titled ‘Frequency of GMI and A1C Discrepancies,’ involving 528 individuals with blood sugar issues, showed that GMI and laboratory A1C values often do not match, with 51% differing by 0.3% or more. This emphasizes the necessity for clinicians to utilize both GMI and A1C together to refine management strategies for the condition. Additionally, understanding what is a normal gmi serves as a valuable tool for patient empowerment, providing insights into how daily actions influence glucose levels.
This understanding encourages a proactive strategy for managing the condition, essential for sustaining long-term health and well-being. Richard M Bergenstal, a prominent voice in research on blood sugar management, stated, ‘It is the hope of the authors that the term GMI, particularly what is a normal gmi and its calculation, will be adopted by the global community,’ highlighting the significance of GMI in fostering informed patient engagement in their care. Furthermore, a calculator for computing what is a normal gmi is available online, allowing users to estimate their GMI based on CGM data.
Adjusting lifestyle based on what is a normal gmi trends not only enhances health management but also reinforces the significance of personalized strategies tailored to individual health goals. The formula for converting A1C to Eat is:
Eat (mg/dL) = [(A1C × 28.7)](https://healthline.com/health/diabetes/what-is-gmi) – 46.7
In San Marcos, CA, incorporating local resources such as educational programs at the Integrative Wellness Center, engaging in community wellness initiatives, and embracing outdoor activities can further support effective management of blood sugar levels.
For personalized guidance, consider reaching out to local support programs that provide resources and education tailored to managing type 2 diabetes, ultimately leading to improved health outcomes.
Conclusion
The Glucose Management Indicator (GMI) is transforming diabetes management by providing a real-time, nuanced understanding of blood glucose levels. By utilizing data from continuous glucose monitoring (CGM) devices, GMI enables patients and healthcare providers to make informed decisions about treatment and lifestyle adjustments, ultimately leading to improved health outcomes. Its ability to reflect average glucose levels through a straightforward calculation makes it a vital tool in personalizing diabetes care, especially when traditional methods may fall short.
The comparison between GMI and A1C highlights significant differences that underscore the importance of incorporating both metrics into diabetes management strategies. While A1C offers a retrospective view of glucose control, GMI provides dynamic insights that empower patients to take proactive steps in managing their health. This is particularly crucial in situations where access to laboratory testing is limited, as seen during the COVID-19 pandemic.
As advancements in CGM technology continue to evolve, the role of GMI in personalized diabetes management becomes increasingly essential. Tailored strategies based on GMI data not only enhance patient engagement but also foster adherence to treatment plans. Through comprehensive analysis and individualized care, healthcare professionals can better support their patients in achieving optimal health outcomes. The ongoing integration of GMI into diabetes care is not just a trend; it represents a fundamental shift towards a more patient-centered approach in managing this complex chronic condition.
Frequently Asked Questions
What is the Glucose Management Indicator (GMI)?
The GMI is a critical metric that estimates an individual’s average blood sugar levels over time, using data from continuous glucose monitoring (CGM) devices. It converts average sugar readings into an estimated A1C percentage through a specific calculation.
Why is understanding a normal GMI important?
Understanding a normal GMI is essential for evaluating blood sugar control more effectively than traditional techniques, allowing patients and healthcare professionals to make timely adjustments to treatment plans and lifestyle choices.
How does GMI benefit patients with diabetes?
GMI helps patients eliminate inconvenient and costly treatment regimens, avoid sugar spikes and crashes, and enhances overall management outcomes by providing reliable data for informed decision-making.
What advancements have been made in CGM technology related to GMI?
Recent advancements in CGM technology have solidified GMI’s role as a vital tool for improving patient outcomes and facilitating proactive diabetes care.
What does the Poincaré Plot Analysis indicate about GMI?
The Poincaré Plot Analysis shows that a smaller, more concentrated plot signifies better stability in blood sugar management, reflecting improvements in glucose control through GMI.
How does GMI impact A1C levels in patients?
Studies indicate that patients utilizing GMI can reduce their A1C levels by an average of 1.5% within six months, demonstrating its effectiveness in real-world scenarios.
How is GMI calculated?
GMI is calculated using the formula: GMI = (average level in mg/dL + 46.7) / 28.7, which converts average sugar levels into an A1C-equivalent percentage.
What should patients understand about interpreting their GMI readings?
Patients should interpret their GMI readings in the context of their overall glucose management strategies, noting that what is considered a normal GMI may not be a reliable measure of glycemic control for individuals with type 2 diabetes.
What is the formula for converting A1C to estimated average glucose (eAG)?
The formula for converting A1C to eAG is: eAG (mg/dL) = (A1C × 28.7) – 46.7, which helps patients manage their health effectively.
What approach does the Integrative Wellness Center take regarding GMI and diabetes management?
The Integrative Wellness Center prioritizes a comprehensive approach that includes understanding A1C and eAG conversions, along with personalized care strategies such as tailored nutrition plans and functional medicine solutions.