Overview
Type 2 diabetes is a condition that many individuals face, characterized by insulin resistance and elevated blood sugar levels. Often linked to obesity, sedentary lifestyles, and genetic factors, it affects approximately 589 million adults worldwide. It’s important to recognize that understanding this condition is crucial. Many patients find that effective management strategies, including lifestyle changes and early detection, can significantly improve their health outcomes. By taking proactive steps, they can reduce the risk of severe complications and lead healthier lives.
Have you ever felt overwhelmed by the challenges of managing your health? You’re not alone. Many people share these feelings, and it’s completely understandable. The journey to better health can be daunting, but with the right support and guidance, it becomes much more manageable. Embracing a 30-Day Diabetes Reset program can be a powerful step toward reclaiming your health.
Remember, small changes can lead to significant improvements. By focusing on your lifestyle and making informed choices, you can navigate this journey with confidence. Let’s take this step together, knowing that every effort counts toward a healthier future.
Introduction
Type 2 diabetes is more than just a medical diagnosis; it represents a profound public health challenge affecting millions worldwide. It’s important to recognize that this condition is not just a statistic; it impacts real lives, creating daily struggles for those who face it. With an alarming rise in cases projected to exceed 1.3 billion by 2050, understanding the nuances of this condition becomes imperative for both individuals and healthcare systems. Many patients find that navigating the complexities of type 2 diabetes can be overwhelming, but there is hope and support available.
This article delves into the origins, symptoms, and critical strategies for effective management of type 2 diabetes. What does it truly mean to live with this condition? How can individuals navigate the myriad challenges it presents? Together, we will explore these questions, offering insights and guidance to empower those affected by diabetes to take charge of their health and well-being.
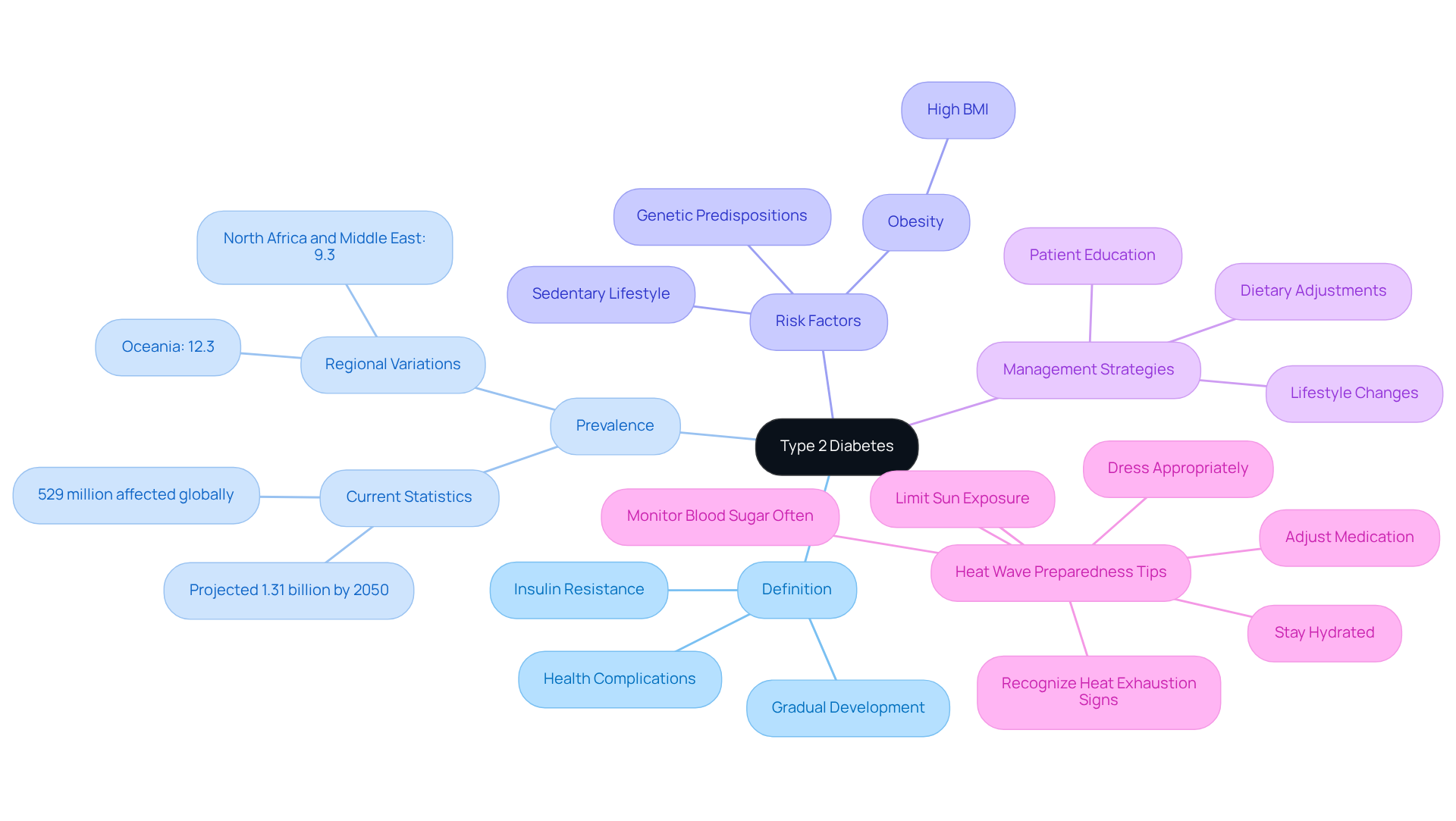
Define Type 2 Diabetes: Understanding the Condition
Living with type 2 diabetes mellitus can be overwhelming, leading many to wonder what does it mean to have type 2 diabetes. Increased blood sugar levels due to insulin resistance and insufficient hormone secretion raise the question of what does it mean to have type 2 diabetes. Unlike type 1 diabetes, where the pancreas produces little to no insulin, individuals with type 2 can produce insulin, but their bodies struggle to use it efficiently. This condition often develops gradually and, if not managed appropriately, raises concerns about what does it mean to have type 2 diabetes and can lead to serious health complications. It’s the most prevalent type of diabetes, affecting around 529 million individuals globally. Alarmingly, forecasts suggest that by 2050, this number may rise to over 1.31 billion.
Many people find that the occurrence of Type 2 diabetes is closely linked to factors such as obesity, sedentary lifestyles, and genetic predispositions. A high body mass index (BMI) is recognized as a significant risk factor, contributing to over 50% of worldwide disability-adjusted life years (DALYs) related to diabetes. Recent studies highlight the critical role of glucose intolerance in the progression of non-insulin-dependent metabolic syndrome. Endocrinologists emphasize that early detection and treatment can significantly impact health outcomes.
Comprehensive treatment approaches, focusing on lifestyle changes, dietary adjustments, and patient education, have shown promising results in reversing insulin resistance and improving overall well-being. Each year, millions are diagnosed with Type 2 diabetes, highlighting the urgent need to understand what does it mean to have type 2 diabetes and to implement effective prevention and management strategies.
For individuals managing Type 2 diabetes, maintaining well-being during extreme weather conditions, such as heat waves, is crucial. Here are some essential heat wave preparedness tips:
- Stay Hydrated: Drink plenty of water throughout the day, even if you don’t feel thirsty. Staying hydrated helps your body sweat and maintain a normal temperature.
- Monitor Blood Sugar Often: Heat can affect your blood sugar levels, so check it more frequently to avoid dangerous highs or lows.
- Proactively Adjust Your Medication: It’s important to consult with your healthcare provider about potential adjustments to insulin and other Type 2 diabetes medications during extreme heat.
- Dress Appropriately: Wear light-colored, loose-fitting clothing to reflect heat and allow your body to cool down efficiently.
- Limit Exposure: Try to avoid the sun during peak hours from 10 a.m. to 4 p.m. and seek air-conditioned environments during the hottest parts of the day.
- Recognize Heat Exhaustion Signs: Knowing the symptoms can help you react quickly if you or someone else shows signs of heat illness.
These strategies are vital for preserving well-being and safety during heat waves. Remember, you are not alone in this journey, and taking proactive steps can make a significant difference.
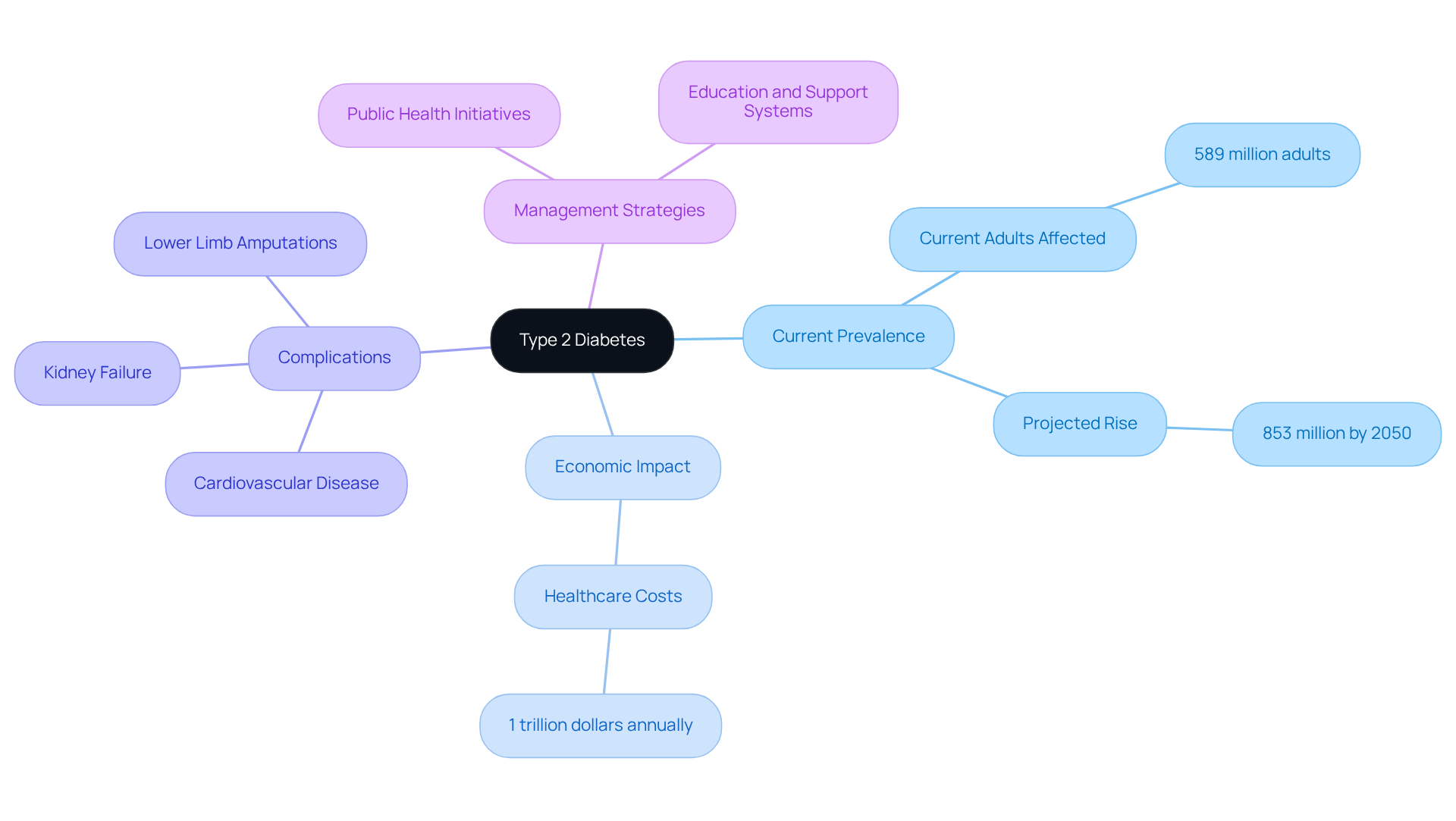
Context and Impact: The Prevalence of Type 2 Diabetes
Type 2 diabetes poses a significant public health challenge, making it crucial to understand what it means to have type 2 diabetes, especially considering that approximately 589 million adults aged 20-79 are currently living with this condition. This number is expected to rise to around 853 million by 2050, highlighting an urgent need for effective management strategies. Many patients find that the increase in sugar-related conditions is particularly noticeable in low- and middle-income nations, where urban growth and lifestyle shifts have led to higher rates of obesity and inactivity.
The economic consequences of Type 2 diabetes are profound, with healthcare costs anticipated to reach 1 trillion dollars each year, alongside considerable declines in productivity. Understanding what it means to have type 2 diabetes is crucial, as this chronic condition is also a major contributor to severe complications, including:
- cardiovascular disease
- kidney failure
- lower limb amputations
These complications further strain healthcare systems globally. Addressing these challenges requires a multifaceted approach. It’s essential to implement public health initiatives, provide education, and establish support systems that empower individuals to manage their health effectively.
By working together and understanding the complexities of this condition, we can foster a supportive environment for those affected. Let’s take action to promote healthier living and provide the necessary resources for everyone to thrive.
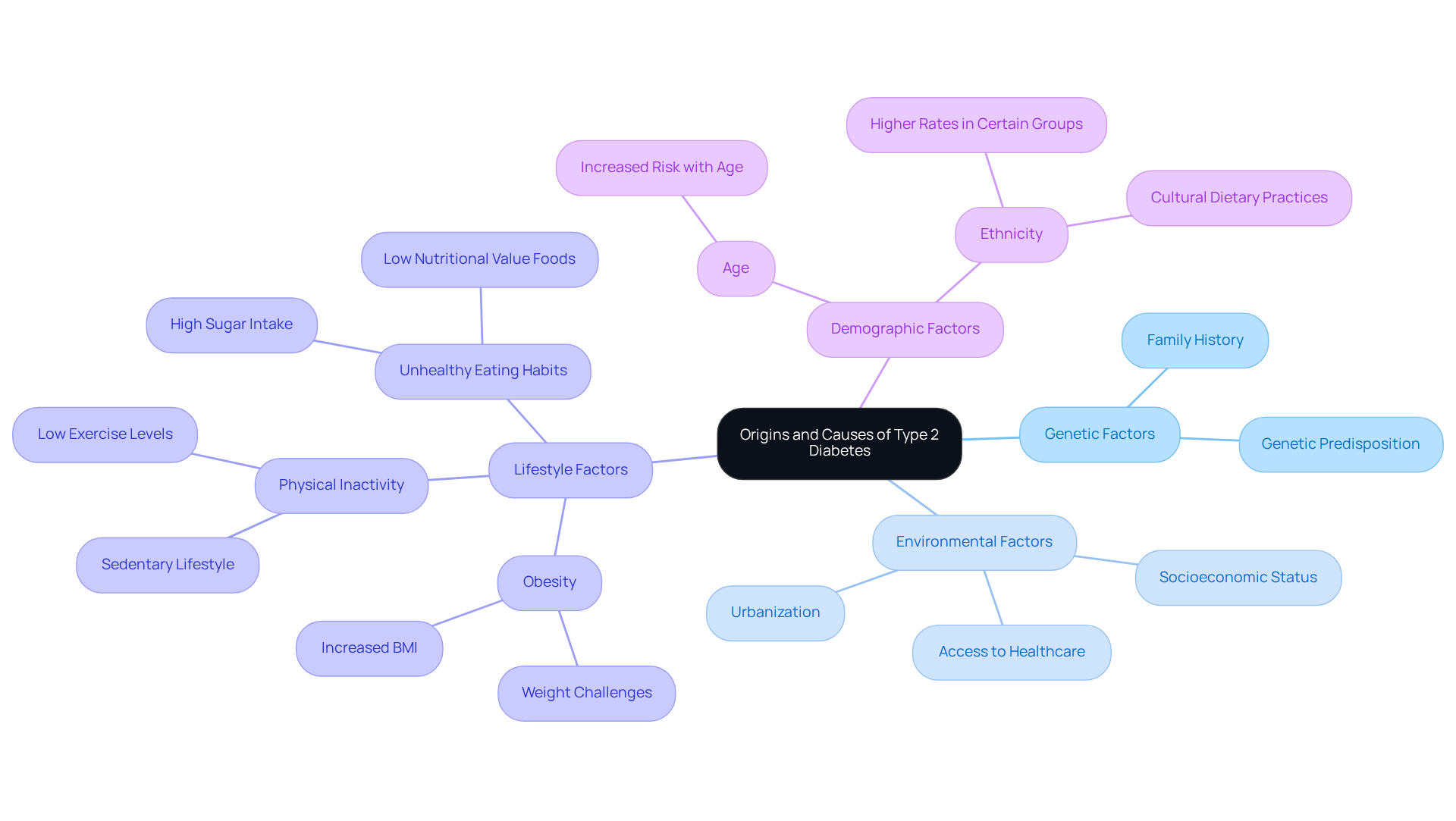
Origins and Causes: What Leads to Type 2 Diabetes?
The emergence of the second form of the condition is influenced by a complex interaction of genetic, environmental, and lifestyle factors. It’s important to recognize what it means to have type 2 diabetes, particularly since obesity is a primary risk factor, with approximately two-thirds of individuals with type 2 diabetes also facing weight challenges. Physical inactivity and unhealthy eating habits further worsen this risk, leading to resistance to a key characteristic of the condition. Insulin resistance occurs when the body’s cells become less responsive to insulin, which raises the question of what does it mean to have type 2 diabetes, prompting the pancreas to work harder to produce sufficient insulin and eventually leading to elevated blood sugar levels.
Many patients find that age and ethnicity also play significant roles in the risk of developing the condition. For instance, the occurrence of diagnosed blood sugar conditions differs among various ethnic groups, with rates reaching 13.3% among American Indian/Alaskan Native adults and 11.1% among Hispanic adults. Additionally, specific health issues, such as hypertension, can elevate the risk of developing the second form of the condition.
Recent studies emphasize what does it mean to have type 2 diabetes and the significance of lifestyle changes in preventing such conditions. Nutritionists highlight that adopting a balanced diet rich in whole foods and regular physical activity is crucial for understanding what does it mean to have type 2 diabetes, as it can significantly lower the risk of developing this chronic condition. In San Marcos, CA, individuals can embrace outdoor activities, such as hiking and walking, to enhance their physical fitness while enjoying the area’s natural beauty. Local farmers’ markets provide access to fresh, nutritious produce, which is essential for a diabetes-friendly diet.
Dr. Jason Shumard at the Integrative Wellness Center offers personalized functional medicine approaches that focus on tailored nutrition and lifestyle changes. His expertise in functional endocrinology and clinical nutrition empowers patients to take charge of their well-being through effective management strategies for blood sugar. Preventive actions, such as early diagnosis and focused wellness education, are crucial in reducing the effects of this condition and postponing its complications. Understanding these origins is vital for implementing effective prevention strategies that empower individuals to take control of their health. To learn more about how Dr. Shumard can help you in reversing your condition, consider attending our upcoming events or reaching out to the Integrative Wellness Center for personalized support.
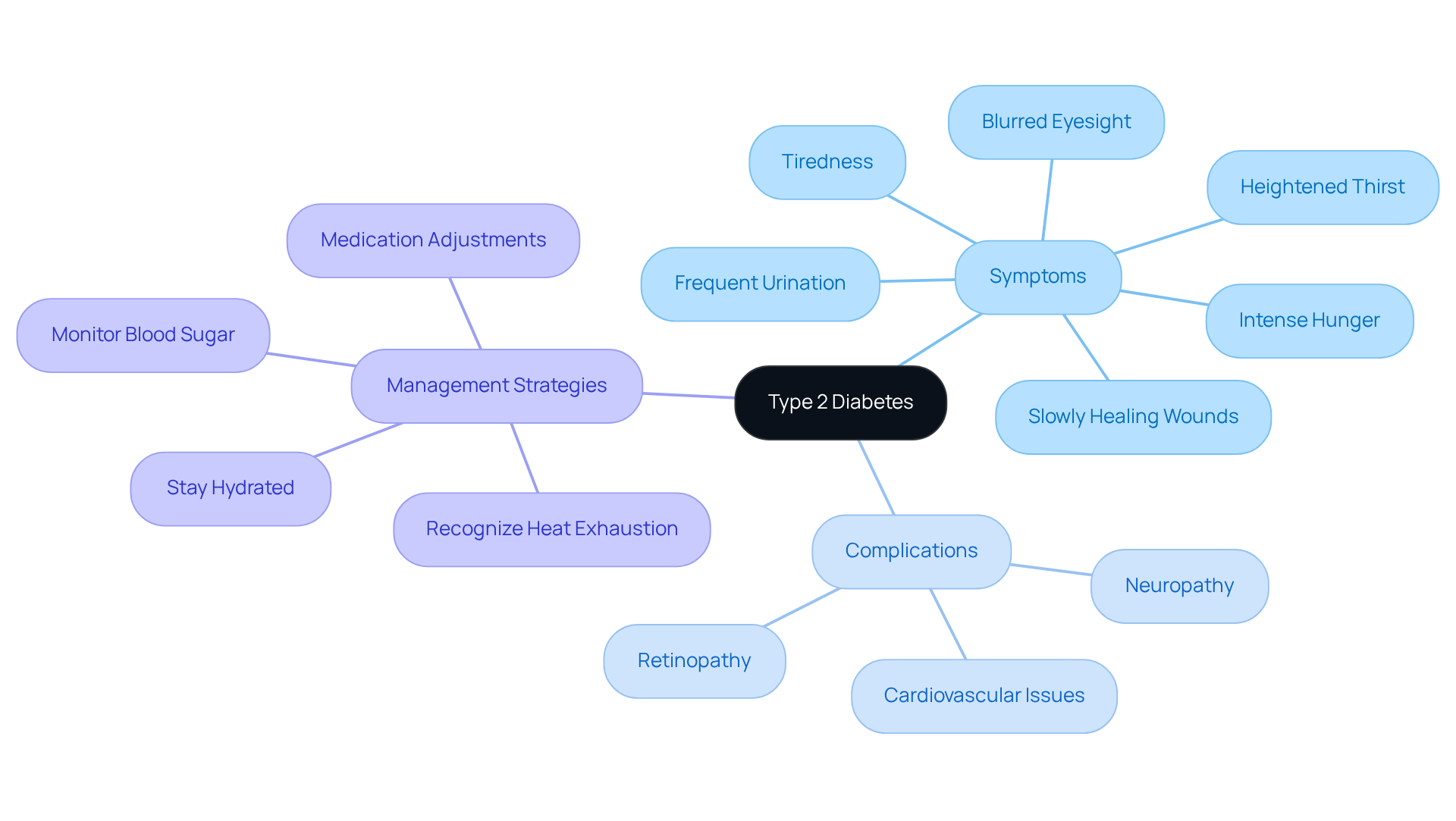
Key Characteristics and Symptoms: Recognizing Type 2 Diabetes
If you’re experiencing heightened thirst, frequent urination, intense hunger, tiredness, blurred eyesight, or slowly healing wounds, these may be typical signs of what does it mean to have type 2 diabetes. It’s important to recognize that many individuals may not notice symptoms in the early stages, which can lead to a delay in diagnosis and treatment. As this condition progresses, complications such as neuropathy, retinopathy, and cardiovascular issues may arise. Acknowledging these symptoms early is vital, as it empowers individuals to seek medical advice and begin appropriate management strategies. This proactive approach can significantly improve quality of life and reduce the risk of severe complications.
During heat waves, it becomes especially crucial for those with type 2 diabetes to remain hydrated. Consuming ample water throughout the day is essential, even if you do not feel thirsty. Many patients find that monitoring blood sugar levels more frequently is necessary, as heat can affect these levels, potentially leading to dangerous highs or lows. Additionally, discussing potential modifications to medications for blood sugar control with medical professionals during intense heat can help in managing your wellbeing effectively. It’s vital to recognize the signs of heat exhaustion early, as timely intervention can prevent serious health issues. Furthermore, understanding the risks associated with conventional diabetes treatments, including the potential for increased insulin resistance, underscores the importance of a holistic approach to care. Remember, you’re not alone on this journey, and taking these steps can lead to a healthier, more fulfilling life.
Conclusion
Living with type 2 diabetes can be a challenging journey, filled with complexities that require understanding and proactive management. This chronic condition, marked by insulin resistance and elevated blood sugar levels, extends beyond personal health; it represents a significant public health concern impacting millions around the world. It’s important to recognize the implications of this condition, as they are crucial for fostering better health outcomes and preventing serious complications.
Many individuals find that type 2 diabetes is closely linked to lifestyle factors such as obesity and inactivity. Early detection and comprehensive treatment strategies are vital in reversing its progression. The importance of education, lifestyle modifications, and community support cannot be overstated; these elements empower individuals to take control of their health. Furthermore, awareness of symptoms and the need for regular monitoring—especially during extreme weather conditions—highlights the necessity of a proactive approach to care.
Addressing the challenges posed by type 2 diabetes calls for collective action. By promoting healthier lifestyles, enhancing public health initiatives, and ensuring access to resources, we can significantly impact the trajectory of this condition. Engaging in preventive measures and supporting those affected can lead to a healthier future. This reinforces the message that understanding and managing type 2 diabetes is essential for both individual well-being and public health. Together, we can navigate this journey toward better health.
Frequently Asked Questions
What is type 2 diabetes?
Type 2 diabetes is a condition characterized by increased blood sugar levels due to insulin resistance and insufficient insulin secretion. Unlike type 1 diabetes, individuals with type 2 can produce insulin but struggle to use it effectively.
How common is type 2 diabetes?
Type 2 diabetes is the most prevalent type of diabetes, currently affecting around 529 million individuals globally, with projections suggesting this number may rise to over 1.31 billion by 2050.
What factors contribute to the development of type 2 diabetes?
The development of type 2 diabetes is closely linked to factors such as obesity, sedentary lifestyles, and genetic predispositions. A high body mass index (BMI) is a significant risk factor.
What are the health risks associated with type 2 diabetes?
If not managed appropriately, type 2 diabetes can lead to serious health complications, including a significant contribution to worldwide disability-adjusted life years (DALYs) related to diabetes.
How can type 2 diabetes be managed?
Comprehensive treatment approaches focusing on lifestyle changes, dietary adjustments, and patient education can help reverse insulin resistance and improve overall well-being.
What should individuals with type 2 diabetes do during extreme heat?
Individuals managing type 2 diabetes should stay hydrated, monitor blood sugar levels more frequently, consult their healthcare provider about medication adjustments, dress appropriately for the heat, limit sun exposure during peak hours, and recognize signs of heat exhaustion.
Why is early detection important in type 2 diabetes?
Early detection and treatment of type 2 diabetes can significantly impact health outcomes and help prevent serious complications.