Overview
The ADA insulin guidelines provide a vital framework for managing insulin therapy in diabetes care, emphasizing a patient-centered approach that incorporates lifestyle modifications and personalized strategies. The article highlights that adherence to these guidelines not only promotes better glycemic control and quality of life but also significantly reduces healthcare costs associated with non-adherence, thereby underscoring the importance of comprehensive education and support for patients.
Introduction
The management of diabetes, particularly type 2 diabetes, has evolved significantly with the establishment of comprehensive guidelines by the American Diabetes Association (ADA). These guidelines are not merely recommendations; they represent a critical framework designed to standardize insulin therapy practices and improve patient outcomes.
As healthcare providers navigate the complexities of diabetes care, understanding these guidelines is essential, especially in light of the staggering economic implications of nonadherence.
The ADA emphasizes a patient-centered approach that incorporates education, monitoring, and tailored insulin management strategies, ensuring that individuals with diabetes can achieve optimal glycemic control.
This article delves into the key components of the ADA insulin guidelines, exploring their importance, recommendations for effective insulin management, and the vital role of patient education in fostering adherence and improving overall health outcomes.
Overview of ADA Insulin Guidelines and Their Importance
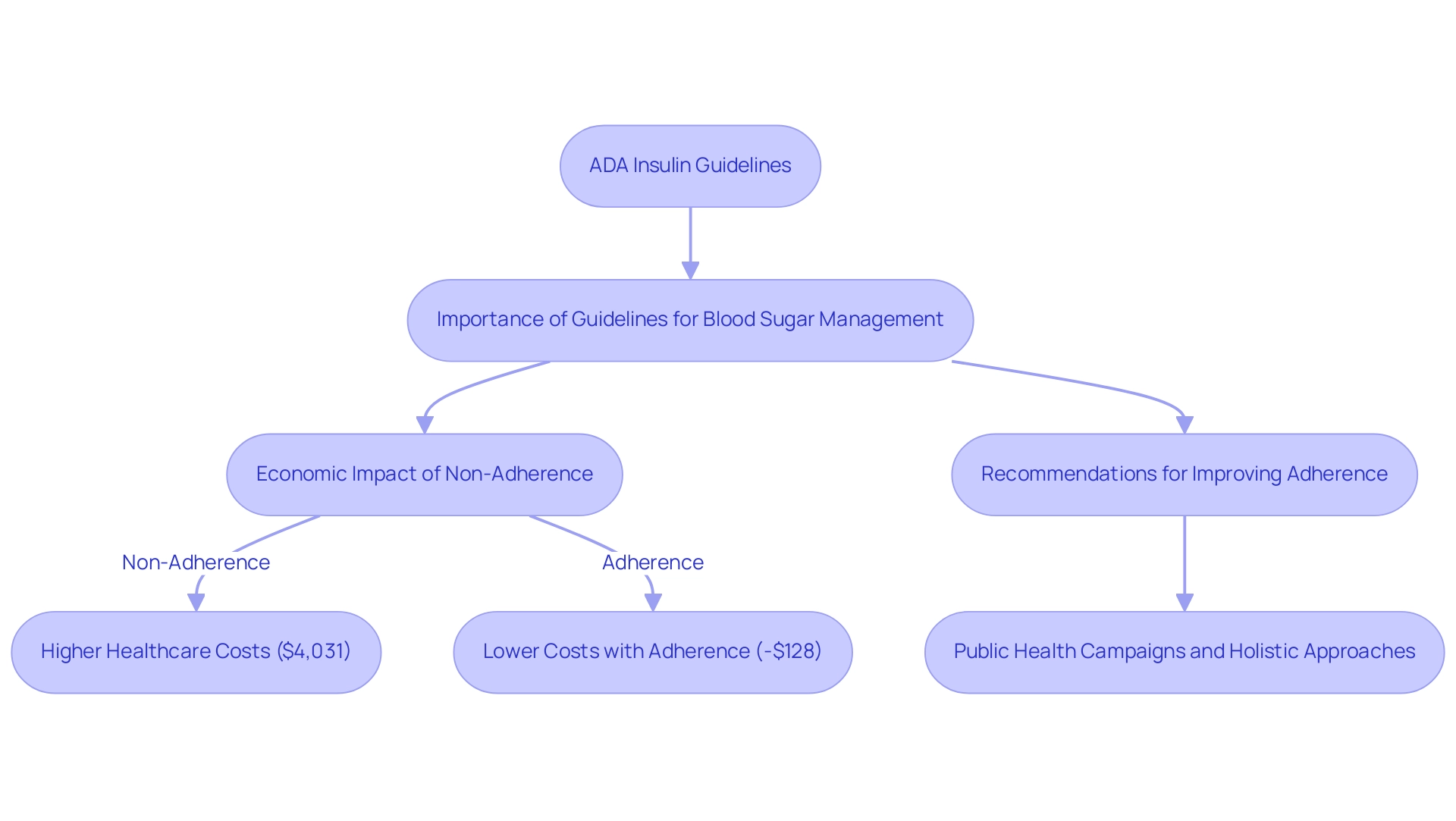
The ADA insulin guidelines for hormone therapy represent a crucial framework for healthcare providers managing blood sugar conditions, particularly type 2. Developed through comprehensive research and expert consensus, the ADA insulin guidelines aim to standardize insulin therapy practices and enhance patient care across diverse healthcare environments. However, it is crucial to recognize that while these guidelines are significant, they should be complemented by a holistic approach that re-examines the source of this condition and addresses health at the root level.
This comprehensive perspective can help mitigate the staggering annual burden of non-adherent care for blood sugar management, estimated to reach as high as $16 billion. Dr. Kaul, Heart & Stroke Foundation Chair in Cardiovascular Research, emphasizes, ‘Adherence to the ADA insulin guidelines is crucial for promoting optimal glycemic control and improving the quality of life for individuals living with diabetes.’ Evidence from a recent study on the economic impact of nonadherence indicates that patients who do not follow ADA recommendations incur healthcare expenditures that are $4,031 higher compared to their baseline year, while those who adhere to the guidelines experience lower costs by $128.
Such findings highlight the critical need for healthcare professionals to initiate and manage insulin therapy in accordance with the ADA insulin guidelines. Additionally, incorporating public health campaigns aimed at young males for glucose screening and annual check-ups is recommended to enhance adherence rates. Ultimately, these strategies, when combined with a holistic regimen, lead to enhanced patient outcomes and increased adherence to treatment protocols.
Key Recommendations for Insulin Initiation and Management
The ADA insulin guidelines provide critical recommendations for hormone initiation and management, emphasizing a patient-centered and holistic approach to blood sugar regulation. Insulin therapy should be considered when lifestyle modifications and oral medications are insufficient to achieve adequate glycemic control, in accordance with the ADA insulin guidelines that emphasize addressing the root causes of diabetes. Tailored initiation of therapy takes into account individual patient factors, such as treatment goals, personal preferences, and any existing comorbid conditions.
It is recommended that doses of the hormone be titrated gradually to mitigate the risk of hypoglycemia while effectively reaching target blood glucose levels. Regular monitoring of blood glucose is essential to assess the effectiveness of the treatment plan and to make necessary adjustments. Instruction on carbohydrate counting and comprehending the action profiles of different types of hormone further empowers individuals, enhancing their ability to manage their condition effectively.
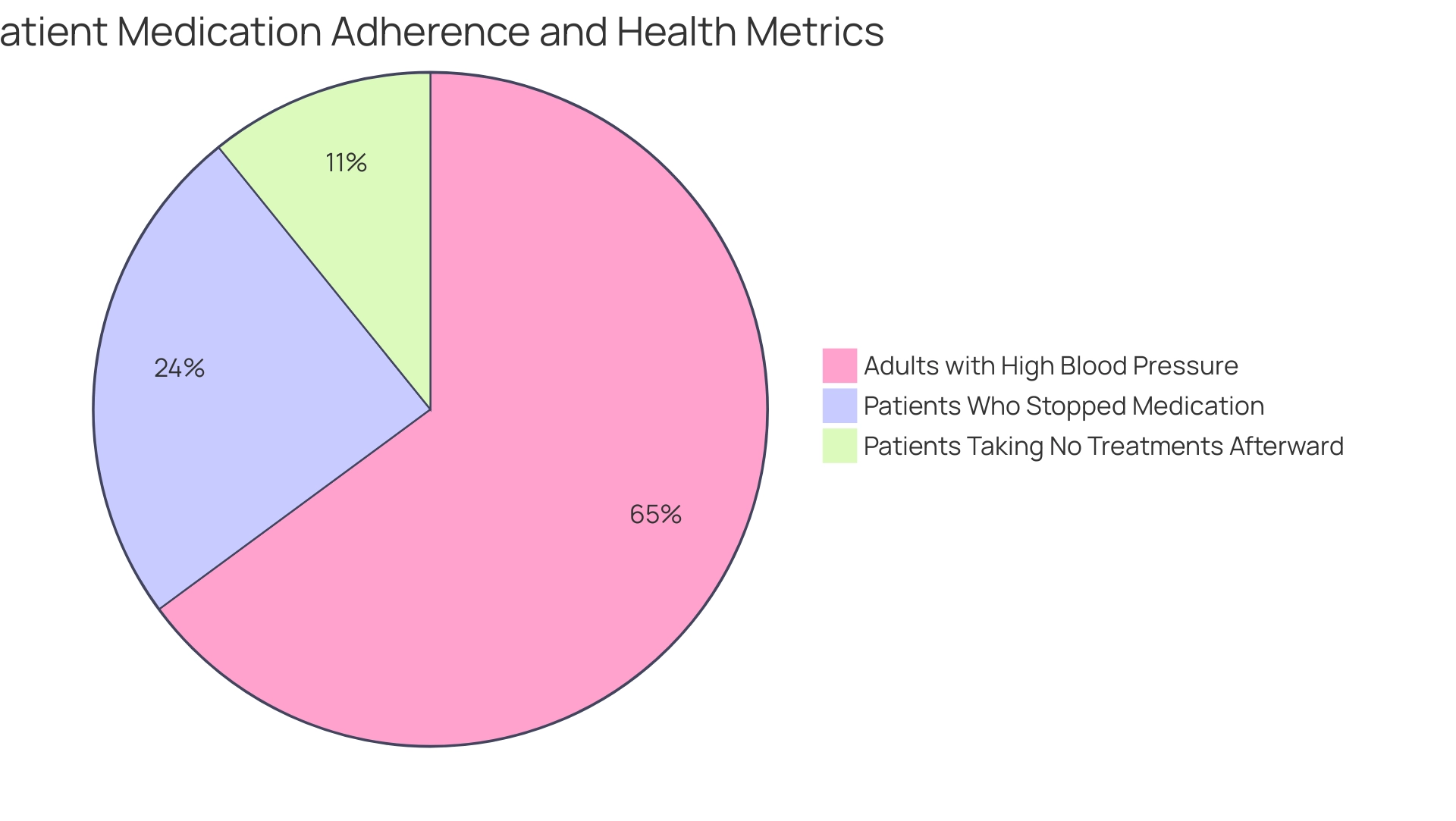
Significantly, recent statistics indicate that:
- 26.5% of patients stopped using their medication completely.
- 11.8% of those taking no treatments for managing blood sugar levels afterward, emphasizing the significance of adhering to management strategies.
Additionally, considering that 70.8% of U.S. adults with diagnosed diabetes had a systolic blood pressure of 140 mmHg or higher or diastolic blood pressure of 90 mmHg or higher, highlights the additional health challenges faced by this population. As highlighted by Dr. G. Caleb Alexander, ‘These findings provide not only updated data characterizing hormone trends but also greater detail regarding the use of different molecules and types of this hormone, including delivery devices.’
This highlights the necessity for thorough education and assistance in blood sugar control. Moreover, recognizing the significant financial impact of this condition, with direct and indirect expenses totaling $413 billion in 2022, highlights the importance of effective treatment strategies that correspond with a comprehensive and integrative approach. Importantly, addressing the anxiety that accompanies the worry surrounding potential complications of this condition is crucial for patient well-being, as it can significantly impact adherence to treatment plans.
Understanding the Types of Insulin Recommended
The guidelines provided by the ADA insulin guidelines outline various types of insulin that are essential for effective health control, each having distinct features designed for specific needs. However, it is crucial to challenge the prevailing myths surrounding the treatment of this condition, such as the misconception that it is solely inherited and that the only options for control involve strict adherence to medication and lifestyle changes. In contrast, a breakthrough approach at the Integrative Wellness Center offers hope for reversing type 2 diabetes, emphasizing that a happy, healthy, and diabetes-free life may be attainable.
This innovative process not only emphasizes management of glucose but also incorporates lifestyle modifications and personalized strategies that differ significantly from traditional methods. Rapid-acting medications, such as lispro and aspart, are particularly effective in managing postprandial blood glucose spikes, allowing for better control following meals. In contrast, long-acting formulations, including glargine and detemir, are designed to provide consistent basal coverage throughout the day, ensuring stable glucose levels.
The choice of a suitable type of hormone therapy and regimen should be personalized, taking into account factors such as the individual’s lifestyle, eating habits, and overall treatment goals. Furthermore, informing individuals about the pharmacokinetics of various types of glucose-lowering medications is essential. Understanding how these medications work can significantly enhance their effectiveness and improve adherence to treatment protocols.
Considering the rising occurrence of type 2 conditions, as shown by the diagnosis of 5,293 children and adolescents aged 10 to 19 years in 2017-2018, such education is crucial for enhancing control strategies and improving patient outcomes. Moreover, comprehending insulin usage patterns is crucial to guide health policy and the ADA insulin guidelines for addressing blood sugar conditions. A case study shows that among adults with high blood sugar, 47.4% had an A1C value of 7.0% or above, emphasizing the significant percentage of individuals not reaching optimal glycemic control, which requires enhanced treatment strategies.
As Dr. Sudipa Sarkar from Johns Hopkins University emphasizes, ‘Effective control of the condition depends on a tailored strategy that takes into account individual needs and the changing array of treatment options.
Monitoring and Adjusting Insulin Therapy
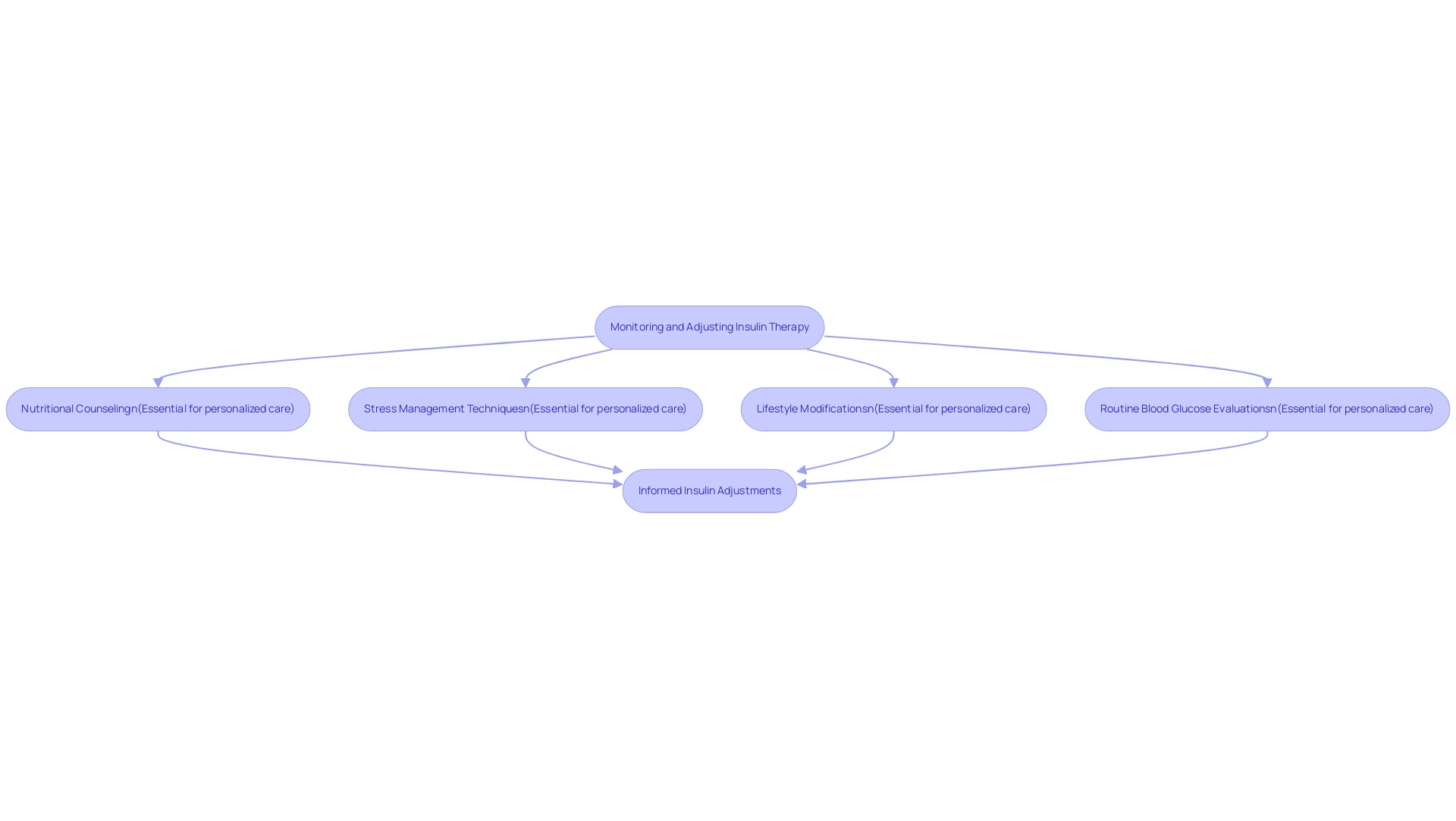
Efficient hormone treatment requires constant observation and customized modifications according to unique individual situations. At the Integrative Wellness Center, we promote a holistic approach that not only empowers individuals to eliminate anxiety about potential diabetes complications but also incorporates specific practices such as:
- Nutritional counseling
- Stress management techniques
- Lifestyle modifications
The ADA insulin guidelines emphasize the significance of routine blood glucose evaluations, which are essential for directing necessary adjustments in medication dosing.
Significantly, the occurrence of hypoglycemia during follow-up episodes is around 4.8%, highlighting the necessity of careful monitoring practices to reduce risks linked to therapy, such as modifying monitoring frequency according to individual needs. Healthcare providers play a vital role in collaborating with patients to establish monitoring routines that fit seamlessly into their daily lives. Factors such as diet, exercise, and stress significantly influence blood glucose levels, and understanding these elements is essential for making informed insulin adjustments.
In this context, Prasanna Tadi emphasizes,
Blood glucose monitoring is a crucial aspect of care in clients with blood sugar issues.
By cultivating a setting of transparent dialogue and learning, healthcare professionals can enable individuals to actively participate in their health care, reducing fears and improving compliance. For instance, the variety of blood glucose meters available today—each offering unique features for better data tracking and trend identification—supports personalized management of the condition and has been shown to improve glycemic control outcomes.
Moreover, the ratio of individuals checking their blood glucose rises with elevated HbA(1c) values, emphasizing the significance of consistent monitoring for effective therapy modifications. Ultimately, these practices can lead to improved health outcomes and a more efficient, integrative strategy for glucose management in accordance with ADA insulin guidelines, alleviating concerns about developing severe complications.
The Role of Patient Education in Insulin Management
Patient education acts as a crucial element of effective glucose control, as highlighted by the ADA insulin guidelines. At the Integrative Wellness Center, we empower patients to eliminate anxiety over potential diabetes complications through holistic care and education, helping them find new peace in life – eliminating worry about developing traumatic and debilitating diabetes complications. Comprehending resistance to this hormone is vital; conventional therapies may neglect the underlying factors, resulting in poor management.
Informing individuals about their condition, the essential role of hormone treatment, and strategies for managing blood glucose levels empowers them to take control of their health. The ADA insulin guidelines advocate for healthcare providers to engage in continuous educational initiatives, which should include discussions about:
- The mechanics of insulin action
- The implications of lifestyle choices
- The potential side effects associated with insulin therapy
A systematic review of community-based Diabetes Self-Management Education (DSME) programs, including the Community-Based DSME Empowerment Program with 516 participants, demonstrated that such initiatives can significantly enhance mental health-related quality of life and lead to better health outcomes.
With a mean triglycerides (TG) decrease of 0.009, this underscores the effectiveness of these educational programs. Although the study faced limitations, such as a small sample size and minimal generalizability, it highlights the necessity for larger randomized controlled trials to further explore these benefits. By fostering a supportive and informative atmosphere through community wellness programs in San Marcos, individuals are more likely to adhere to their treatment regimens, resulting in improved glycemic control and enhanced quality of life.
As noted by health educators, informed patients are more likely to make choices that lead to better health and fewer complications. Discover real solutions and get your life back with the support of our programs, as 1 out of every 3 people you meet will develop some form of diabetes in his or her lifetime, and 10% of women have a sub-optimally functioning thyroid.
Conclusion
The American Diabetes Association (ADA) insulin guidelines provide a vital framework for managing type 2 diabetes, emphasizing the importance of patient-centered care and comprehensive education. By standardizing insulin therapy practices, these guidelines aim to improve patient outcomes and reduce the economic burden associated with nonadherence. The staggering costs related to inadequate management underscore the necessity for healthcare providers to initiate and manage insulin therapy in alignment with these guidelines.
Key recommendations highlight the need for tailored insulin initiation and management strategies that consider individual patient circumstances, preferences, and comorbidities. Regular monitoring and gradual titration of insulin doses are essential to minimize the risks of hypoglycemia while achieving optimal glycemic control. Effective patient education plays a critical role in empowering individuals to manage their diabetes, enhancing adherence to treatment protocols.
Understanding the various types of insulin and their specific uses is crucial for effective diabetes management. Addressing misconceptions about diabetes treatment can open pathways to innovative approaches that go beyond traditional management strategies. A holistic perspective that includes lifestyle modifications, nutritional counseling, and stress management can significantly enhance patient engagement and adherence to therapy.
In conclusion, adherence to the ADA guidelines not only facilitates better health outcomes but also mitigates the financial implications of diabetes care. By fostering a supportive environment through continuous education and personalized strategies, healthcare providers can empower individuals with diabetes to take control of their health, ultimately leading to improved quality of life and reduced complications. Embracing these guidelines is essential for advancing diabetes management and ensuring a healthier future for individuals living with this chronic condition.
Frequently Asked Questions
What are the ADA insulin guidelines?
The ADA insulin guidelines are a set of recommendations developed through research and expert consensus to standardize insulin therapy practices for managing blood sugar conditions, particularly type 2 diabetes.
Why are the ADA insulin guidelines important?
They are crucial for promoting optimal glycemic control, improving the quality of life for individuals with diabetes, and helping healthcare providers manage insulin therapy effectively.
How do the ADA insulin guidelines suggest initiating insulin therapy?
Insulin therapy should be considered when lifestyle changes and oral medications do not provide adequate glycemic control, taking into account individual patient factors such as treatment goals and personal preferences.
What is the recommended approach to dosing insulin according to the guidelines?
The guidelines recommend that insulin doses be titrated gradually to reduce the risk of hypoglycemia while effectively reaching target blood glucose levels.
What role does patient education play in managing diabetes according to the guidelines?
Education on carbohydrate counting and understanding the action profiles of different types of insulin empowers individuals to manage their condition more effectively.
What is the economic impact of non-adherence to the ADA insulin guidelines?
Patients who do not follow the guidelines incur healthcare costs that are $4,031 higher compared to their baseline year, while those who adhere to the guidelines experience lower costs by $128.
How does non-adherence affect diabetes management?
A significant percentage of patients stop using their medication completely, which emphasizes the importance of adherence to management strategies for effective blood sugar control.
What additional health challenges do individuals with diabetes face?
Many adults with diagnosed diabetes also have high blood pressure, which adds to the complexity of their health management.
What recommendations are made for improving adherence to treatment?
Incorporating public health campaigns aimed at young males for glucose screening and annual check-ups is recommended to enhance adherence rates.
Why is a holistic approach important in managing diabetes?
A holistic approach addresses the root causes of diabetes and supports overall health, which can lead to better patient outcomes and increased adherence to treatment protocols.