Overview
The American Diabetes Association Standards of Care 2024 highlight the significance of personalized, patient-centered approaches to diabetes management. It’s important to recognize that lifestyle modifications, technology integration, and comprehensive education play crucial roles in this journey. Many patients find that tailored strategies, such as community wellness programs and continuous glucose monitors, not only enhance the quality of care but also empower them to take an active role in managing their health. \n\nImagine being supported by a community that understands your struggles and encourages your journey toward better health. This nurturing approach fosters a sense of belonging and motivates individuals to embrace their health challenges with confidence. As you consider these strategies, think about how they can fit into your life and help you thrive. \n\nUltimately, the goal is to create a supportive environment where you feel understood and guided every step of the way. By integrating these practices into your daily routine, you can take meaningful steps toward a healthier, more fulfilling life.
Introduction
As diabetes continues to impact millions, it’s important to recognize that the 2024 American Diabetes Association (ADA) Standards of Care emerge as a beacon of hope. These guidelines offer a robust framework aimed at improving management and outcomes for those living with this chronic condition. They emphasize a patient-centered approach, integrating evidence-based recommendations that encompass everything from screening and diagnosis to lifestyle modifications and innovative technology.
Many patients find that a focus on personalized care resonates deeply with their individual lifestyles and cultural backgrounds, especially in communities like San Marcos, CA. By highlighting the importance of nutrition, exercise, and mental health, alongside advancements in diabetes technology, the ADA sets the stage for transformative changes in diabetes management. This empowers patients to take control of their health journey and encourages healthcare providers to tailor strategies that truly support their patients’ needs.
The journey may be challenging, but with these guidelines, there is a path forward filled with hope and opportunity for healthier living.
Overview of the ADA Standards of Care 2024
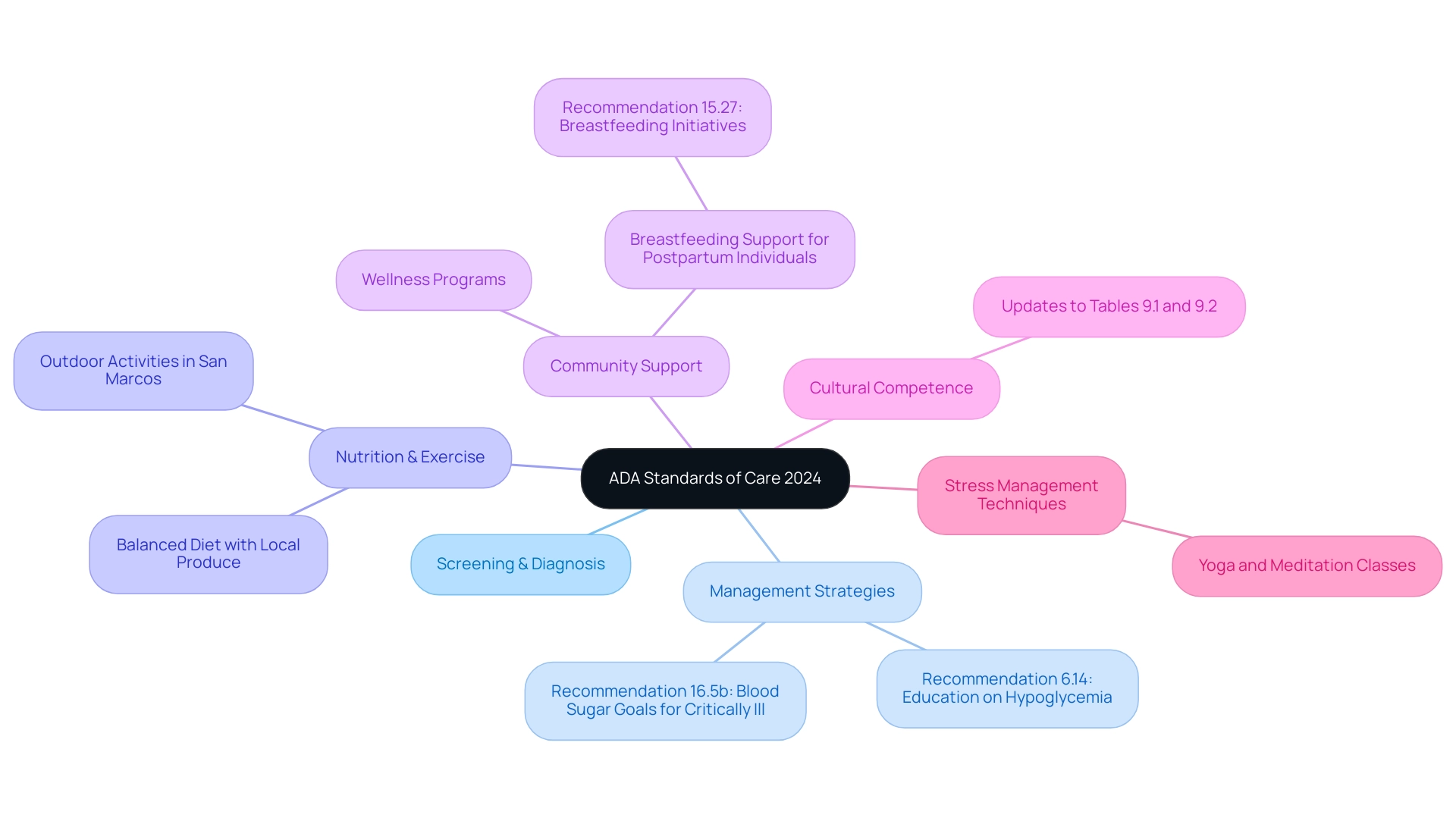
The American Diabetes Association Standards of Care 2024 offers a comprehensive framework of evidence-based recommendations designed to elevate the quality of care for individuals living with diabetes. These guidelines thoughtfully address essential elements such as screening, diagnosis, and management of blood sugar conditions, alongside strategies for preventing complications. A significant focus is placed on patient-centered care, which aligns with holistic lifestyle strategies that encompass nutrition, exercise, community support, and stress management—especially beneficial for those in San Marcos, CA.
It’s important to recognize that embracing the area’s outdoor lifestyle through activities in scenic parks and trails can enhance physical well-being, boost mood, and help manage blood sugar levels. Nutrition plays a pivotal role; therefore, focusing on a balanced diet rich in local produce, such as avocados and berries found at vibrant farmers’ markets, can be instrumental in regulating blood sugar. Community wellness programs provide invaluable support, offering access to education and resources tailored for managing blood sugar.
Many patients find that individual education is crucial in preventing and treating hypoglycemia, as highlighted in Recommendation 6.14. This ensures that individuals are well-informed about their health. Dr. Jason Shumard’s personalized guidance in San Marcos emphasizes how tailored nutrition and functional medicine approaches can empower individuals to effectively manage their condition.
Furthermore, the updated guidelines reflect a commitment to cultural competence, recognizing the diverse backgrounds and experiences of patients. This year’s changes, including updates to Tables 9.1 and 9.2, indicate a proactive strategy for blood sugar control. According to Robert A. Gabbay, a member of the ADA Professional Practice Committee, “the American Diabetes Association standards of care 2024 guidelines represent a significant advancement in the standards of care for blood sugar control, ensuring that all individuals receive comprehensive and culturally sensitive treatment.”
Additionally, Recommendation 16.5b suggests more stringent goals of 110–140 mg/dL (6.1–7.8 mmol/L) for selected critically ill individuals, if achievable without significant hypoglycemia. To illustrate the practical effects of these guidelines, the case study titled ‘Breastfeeding Support for Postpartum Individuals’ emphasizes how Recommendation 15.27 promotes breastfeeding initiatives for all postpartum individuals with blood sugar issues, reinforcing breastfeeding as a crucial aspect of care after childbirth.
Moreover, incorporating stress reduction techniques, such as yoga and meditation classes available in San Marcos, can further enhance overall well-being and support blood sugar control.
Key Updates in the 2024 Standards of Care
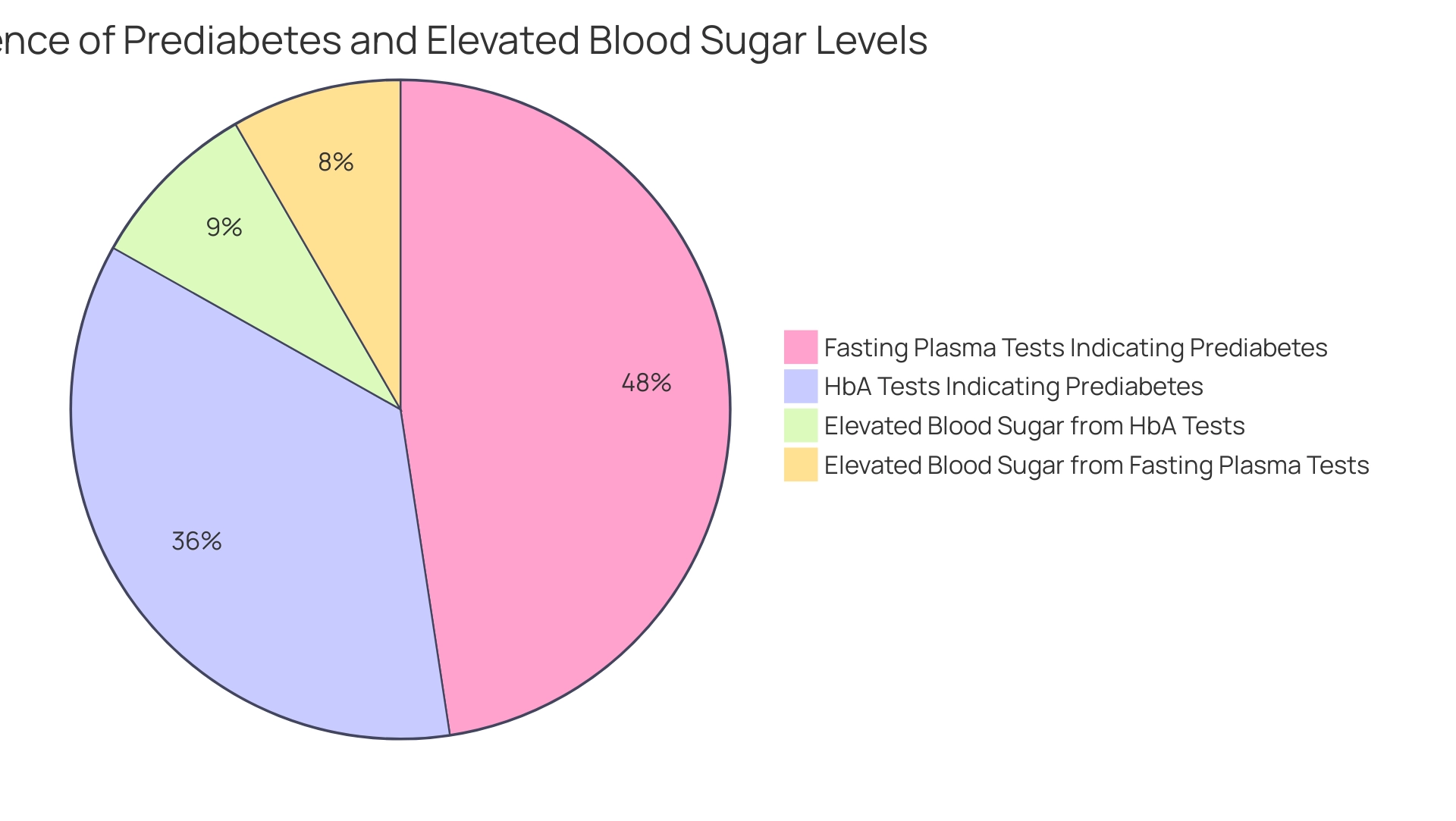
The updates revealed in the American Diabetes Association Standards of Care 2024 are particularly important in the area of obesity control, a significant risk factor for complications associated with blood sugar issues. It’s crucial to understand that these guidelines encourage a more tailored approach to glucose management. This motivates healthcare providers to develop strategies that reflect each individual’s unique circumstances. Given the prevalence of conditions such as prediabetes—approximately 96 million adults in the U.S. are impacted, with significant percentages displaying risk indicators through various testing methods—this approach is more essential than ever.
A recent case study titled ‘Prevalence of Prediabetes and Diabetes in Blood Glucose Tests’ evaluated results from HbA tests and fasting plasma glucose tests, revealing critical statistics:
- 23.0% of HbA tests indicated prediabetes
- 5.5% showed elevated blood sugar levels
- 30.8% of fasting plasma glucose tests indicated prediabetes
- 5.4% showed elevated blood sugar levels
These findings underscore the necessity of tailored management strategies that address individual patient needs and preferences.
Many patients find that integrative functional medicine approaches, like those provided by Dr. Jason Shumard in San Marcos, CA, further improve care for individuals with metabolic conditions. This approach emphasizes comprehensive wellness solutions that involve tailored nutrition, lifestyle changes, and community assistance. It’s not just about dietary changes—like incorporating local produce from vibrant farmers’ markets—but also includes comprehensive assessments and diagnostic tests to identify underlying issues contributing to diabetes.
By understanding personal health history and genetic factors, practitioners can create customized treatment plans. Furthermore, this approach promotes regular physical activity, stress reduction techniques such as yoga and mindfulness, and collaborative care that combines both functional and traditional medicine. It’s important to recognize that the guidelines based on the American Diabetes Association Standards of Care 2024 also highlight advancements in technology for managing blood sugar levels. Tools like continuous glucose monitoring (CGM) and automated insulin delivery systems are vital in enhancing management.
Additionally, the significance of mental well-being is highlighted. Routine assessments for distress linked to metabolic conditions and associated psychological issues ensure a thorough method to care. The endorsement of these guidelines indicates a dedication to enhancing care and results for individuals managing blood sugar issues, aligned with the American Diabetes Association Standards of Care 2024. Together, we can navigate this journey toward better health and well-being.
The Importance of Personalized Diabetes Care
Personalized care for individuals with diabetes has emerged as a fundamental element of effective management, as highlighted by the American Diabetes Association Standards of Care 2024. It’s important to recognize that collective decision-making is vital in this journey. Healthcare professionals are encouraged to collaborate with individuals, taking into account their unique wellness profiles, lifestyles, and values. This nurturing approach not only enhances adherence to treatment plans but also empowers individuals, encouraging them to actively participate in managing their diabetes through effective strategies such as SMART goals and consistent progress tracking.
Many patients find that utilizing fitness apps, journals, and pedometers to set specific targets—like aiming for a daily step count or tracking weight loss—can significantly boost motivation and accountability. The integration of patient-reported outcomes and preferences into treatment decisions is essential, moving away from a one-size-fits-all model. For instance, Dr. Jason Shumard’s 30-Day Diabetes Reset program has transformed numerous experiences, with individuals reporting remarkable health enhancements, including significant weight loss and improved control of blood sugar levels.
As one individual shared, ‘I have lost 55 lbs. My A1C started at 9.1 after 8 months it is now 5.7.’ Such advancements showcase the concrete advantages of customized blood sugar control, illustrating the positive impact of personalized care.
Dr. Savitha Subramanian emphasizes the necessity of addressing psychosocial factors in care, stating, ‘In such a situation, enlisting the help of social workers, arranging for psychological counseling, and allowing some laxity in her glycemic control until her social situation improves become necessary to improve and maintain her compliance.’ As healthcare continues to evolve, the commitment to personalized care models will be paramount in enhancing patient outcomes, particularly in addressing the unique challenges faced by individuals with blood sugar management issues, in accordance with the American Diabetes Association standards of care 2024.
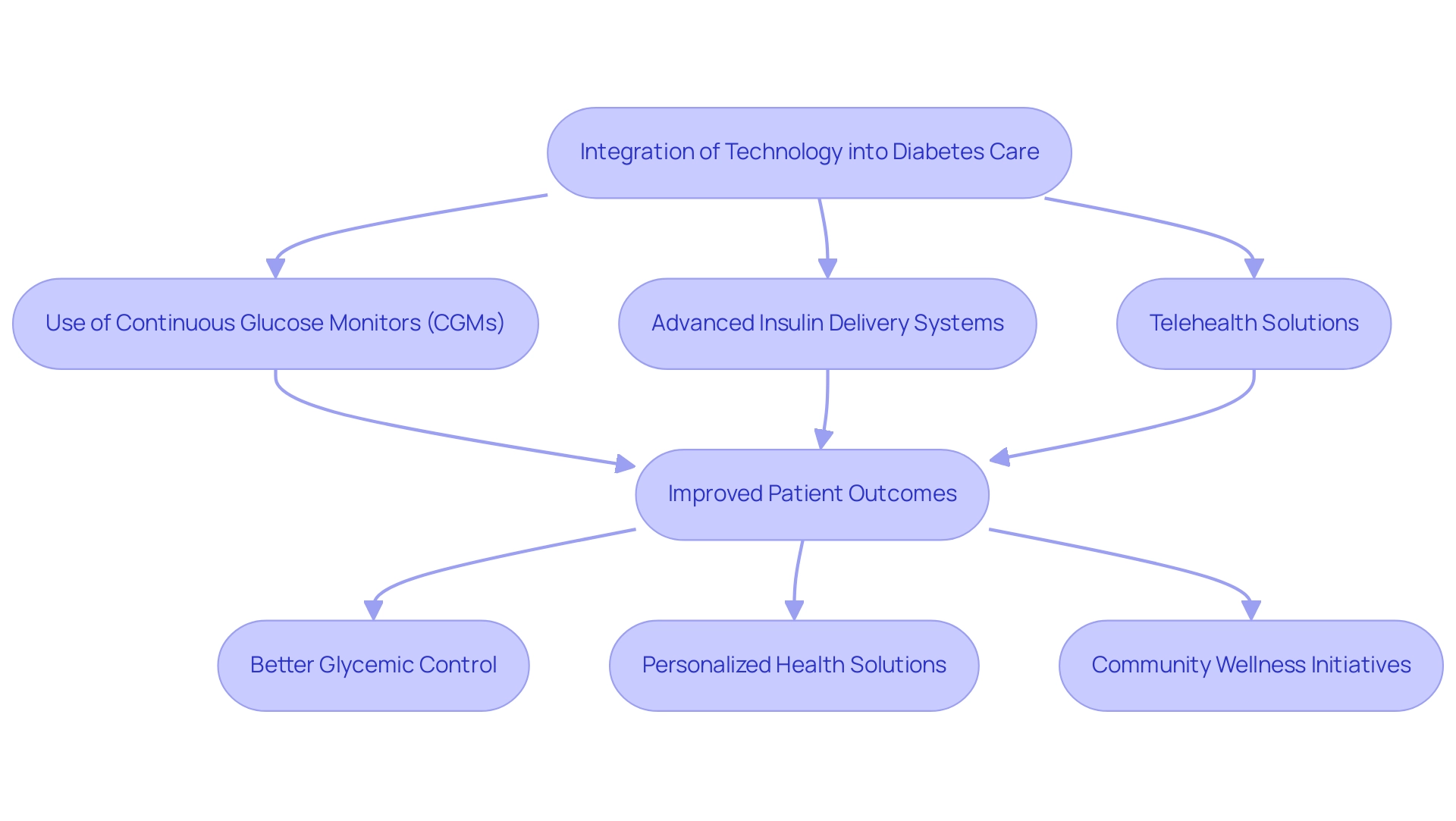
Integrating Technology into Diabetes Care
The integration of technology into blood sugar management has significantly transformed strategies, particularly with the American Diabetes Association Standards of Care 2024 advocating for the use of continuous glucose monitors (CGMs) and advanced insulin delivery systems that respond to real-time glucose data. These innovations not only enhance traditional methods but also align perfectly with integrative functional medicine strategies that focus on personalized health solutions. A notable statistic from a recent study shows a significant improvement in estimated glucose values (EGV) from 205 mg/dL to 172 mg/dL during the unblinded 6-month wear period of CGMs, providing concrete evidence of their effectiveness.
It’s important to recognize that such tools enable individuals to make informed choices regarding their insulin dosing and lifestyle decisions, which is a critical aspect of personalized functional medicine for managing type 2 diabetes. Many patients find that the study titled ‘Impact of Continuous Glucose Monitors on Glycemic Control’ demonstrated that CGM use led to improved glycemic control, evidenced by reductions in A1c levels and increased time in the target glucose range among those receiving the intervention compared to individuals receiving standard care. This reflects the importance of tailored nutrition, comprehensive assessments, and continuous evaluation in achieving better health outcomes.
The principal investigator oversaw the study’s protocol development, data analysis, and manuscript preparation, ensuring a rigorous approach to the research. Furthermore, telehealth solutions have emerged as a vital resource, offering individuals enhanced access to healthcare providers and educational materials. This transition towards digital healthcare encourages increased involvement and self-regulation among individuals, further aiding comprehensive lifestyle approaches such as nutrition, exercise, and stress control in local communities, like those found in San Marcos, CA.
Moreover, community wellness initiatives serve an essential function in providing assistance and resources for blood sugar control, aiding individuals in effectively incorporating these lifestyle adjustments. The American Diabetes Association standards of care 2024 strongly urge healthcare professionals to integrate these advancements into their practice, ensuring that patients benefit from innovative tools designed for effective health control. M.E.L., the guarantor of this work, emphasizes, ‘As the guarantor, I had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis,’ underscoring the commitment to reliable and effective management of blood sugar conditions.
Lifestyle Modifications for Effective Diabetes Management
The American Diabetes Association Standards of Care 2024 highlight the importance of significant lifestyle modifications for effective diabetes management. With the total direct and indirect estimated costs of diagnosed conditions in the United States reaching $413 billion in 2022, the need for impactful lifestyle changes is urgent. A balanced diet plays a crucial role, encouraging the consumption of whole foods like vegetables, fruits, lean proteins, and whole grains, while limiting processed foods and added sugars.
It’s important to recognize that many individuals face challenges in making these changes. Research shows that participants in the Diabetes Prevention Program achieved an average weight loss of 7.6 kg, or about 8% of their initial body weight, by following a 500-700 kcal/day deficit during a 12-week intervention. Regular physical activity is another cornerstone of these recommendations, with guidelines suggesting at least 150 minutes of moderate-intensity exercise each week. For those with type 2 diabetes, a step-by-step guide to starting a walking program can significantly enhance wellness and vitality.
Many patients find that beginning their journey involves evaluating their current fitness level and setting realistic goals, such as committing to a daily walk of 10-15 minutes. Selecting a comfortable environment is crucial; whether indoors or outdoors, ensure it aligns with your safety preferences. Developing a consistent schedule and gradually increasing both the duration and frequency of walks is essential for success.
Tracking progress through a journal or app can help maintain motivation. Additionally, the support of a hiking group or companion can enhance accountability and enjoyment. This holistic approach, as illustrated by patient testimonials like that of A.A., demonstrates how organized programs can align with the American Diabetes Association standards of care 2024, leading to transformative experiences. A.A.’s journey showcases the effectiveness of these structured guidelines in achieving significant wellness improvements.
Furthermore, aerobic exercise should be incorporated at least three days each week, with no more than two consecutive days off. Targeting moderate intensity can enhance insulin action and promote long-term benefits. Research indicates that organized walking initiatives can lead to substantial health improvements, with a success rate of 89.5% among experts at the Primary Health Care Center recognizing the advantages of similar efforts.
Key Tips for Starting Your Walking Program:
- Begin with short walks, gradually increasing duration.
- Choose a safe and comfortable environment.
- Track your progress to stay motivated.
- Consider joining a walking group for support and companionship.
Remember, every small step counts toward a healthier you!
Addressing Comorbidities and Mental Health in Diabetes Care
The American Diabetes Association Standards of Care 2024 present a holistic framework for managing diabetes, emphasizing essential lifestyle strategies that complement medical treatment. Living with type 2 diabetes in San Marcos, CA, can be effectively managed through tailored nutrition, regular exercise, community support, and stress management—elements that resonate deeply with the local lifestyle. It’s important to recognize the significance of a balanced diet rich in local produce, such as avocados and berries. These guidelines advocate for engaging with vibrant farmers’ markets to incorporate fresh, nutritious options into daily meals.
Many patients find that exercise is equally crucial; the area’s parks and trails offer ample opportunities for physical activity, enhancing insulin sensitivity and helping manage blood sugar levels. Additionally, community wellness initiatives provide essential resources designed to support blood sugar management, such as nutrition education, fitness classes, and peer support groups. This highlights the importance of social connections in achieving wellness objectives. Mental well-being is another vital aspect, with the American Diabetes Association standards suggesting regular assessments for conditions like depression and anxiety—common concerns among individuals managing blood sugar issues.
Studies show that nearly 40% of individuals with diabetes face mental wellness challenges, making combined care approaches that address both physical and emotional wellness crucial. This comprehensive strategy not only seeks to enhance overall wellness but also improves the quality of life for those navigating the complexities of a chronic condition. By focusing on customized functional medicine strategies, which emphasize individualized nutrition and testing, healthcare providers can better meet the diverse needs of their patients.
As illustrated by the case study titled ‘Blood Glucose Lowering Treatment in Older Adults,’ individualized treatment plans are increasingly essential, especially as the older adult population grows and the prevalence of diabetes-related complications rises. Incorporating these holistic lifestyle strategies alongside medical interventions can lead to improved health outcomes and a better quality of life for those managing type 2 diabetes.
Are you ready to take the first step toward a healthier you? Embrace these strategies and consider joining the 30-Day Diabetes Reset program to support your journey.
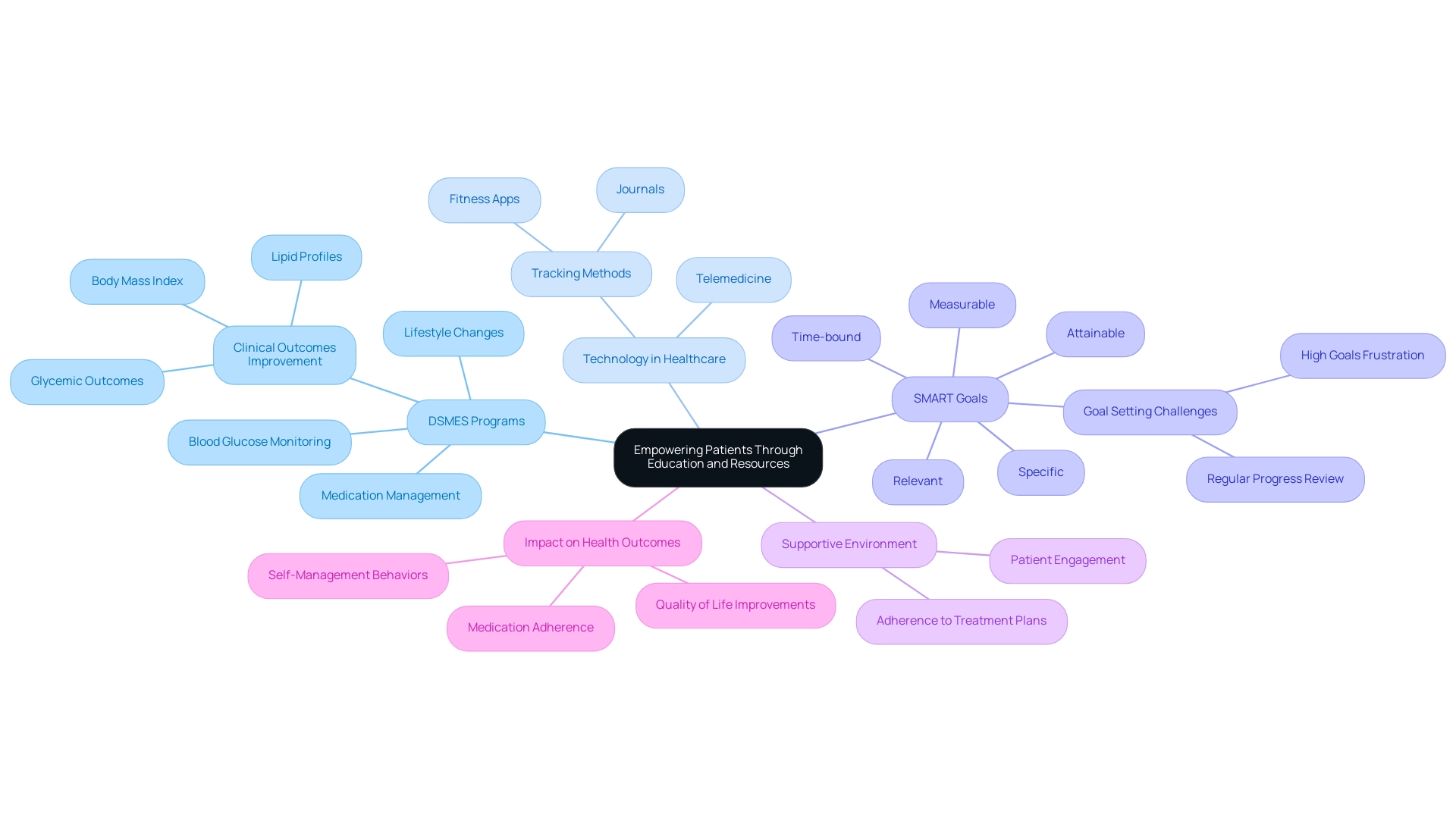
Empowering Patients Through Education and Resources
The American Diabetes Association Standards of Care 2024 highlight the crucial importance of individual education in effectively managing diabetes. By empowering individuals with Type 2 Diabetes through comprehensive knowledge and resources, we enable them to take an active role in their healthcare decisions. The guidelines strongly advocate for the implementation of self-care education and support (DSMES) programs, which align with the American Diabetes Association standards of care 2024. These programs equip patients with essential skills for effective condition oversight.
These initiatives cover vital topics such as blood glucose monitoring, medication management, and necessary lifestyle changes. A systematic review of DSME programs, particularly in Middle Eastern countries, revealed significant improvements in clinical glycemic outcomes, lipid profiles, and body mass index in over 60% of the studies reviewed, with follow-up durations ranging from 4.5 to 37.5 months. Additionally, patients reported improvements in medication adherence, self-management behaviors, and overall quality of life.
Many patients find that ‘the application of technology and telemedicine can help deliver care at a distance for rural communities,’ as emphasized by Mendez I. This enhances the accessibility of educational resources. Individuals are also encouraged to utilize various tracking methods, such as fitness apps and journals, to monitor their progress. Implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost focus and motivation in managing blood sugar.
However, it’s important to recognize that setting goals too high can lead to frustration and decreased motivation. Understanding the systematic negative relationships between goal achievement and goal difficulty is crucial for realistic goal-setting. Regularly reviewing one’s progress not only fosters accountability but also allows for the adaptation of goals as fitness levels change. While conventional diabetes treatments are prevalent, they may pose risks such as increased insulin resistance, underscoring the need for a more holistic approach to care.
By creating a supportive environment and equipping patients with essential tools, healthcare providers can significantly enhance patient engagement and adherence to treatment plans, ultimately leading to better health outcomes.
Conclusion
The 2024 American Diabetes Association (ADA) Standards of Care offer a transformative framework for managing diabetes, placing a strong emphasis on a patient-centered approach. This approach incorporates personalized care, lifestyle modifications, and advanced technology, all tailored to meet individual needs. It’s important to recognize that for those living with prediabetes and diabetes, these guidelines empower individuals to take charge of their health journey. By fostering a collaborative relationship between healthcare providers and patients, informed decision-making and goal-setting become attainable goals.
Many patients find that integrating lifestyle modifications, such as nutrition and exercise, is paramount for effective diabetes management. The guidelines encourage adopting a balanced diet rich in whole foods and engaging in regular physical activity, which can significantly improve health outcomes. Community support and wellness programs further enhance this approach, providing valuable resources and encouragement for individuals navigating the challenges of diabetes.
Moreover, the integration of technology, including continuous glucose monitoring and telehealth solutions, represents a significant advancement in diabetes care. These tools not only improve glycemic control but also foster greater patient engagement and self-management. Additionally, addressing mental health and comorbidities is essential, as the guidelines advocate for holistic care strategies that encompass both physical and emotional well-being.
In summary, the 2024 ADA Standards of Care illuminate a hopeful path forward for diabetes management. By prioritizing personalized care, lifestyle changes, and technological advancements, patients are better equipped to manage their condition and improve their quality of life. As these guidelines take effect, they herald a new era of diabetes care that is both comprehensive and culturally sensitive. This ultimately fosters healthier communities and empowers individuals to thrive. So, are you ready to embrace this journey towards a healthier you?
Frequently Asked Questions
What is the purpose of the American Diabetes Association Standards of Care 2024?
The purpose of the American Diabetes Association Standards of Care 2024 is to provide a comprehensive framework of evidence-based recommendations aimed at improving the quality of care for individuals living with diabetes, addressing screening, diagnosis, management of blood sugar conditions, and prevention of complications.
How does the 2024 guidelines emphasize patient-centered care?
The guidelines emphasize patient-centered care by aligning with holistic lifestyle strategies that include nutrition, exercise, community support, and stress management, which are particularly beneficial for patients in areas like San Marcos, CA.
What role does nutrition play in managing diabetes according to the guidelines?
Nutrition plays a pivotal role in managing diabetes, with recommendations to focus on a balanced diet rich in local produce, such as avocados and berries, to help regulate blood sugar levels.
What is the significance of individual education in diabetes management?
Individual education is crucial in preventing and treating hypoglycemia, ensuring that individuals are well-informed about their health and management strategies.
How do the updated guidelines reflect cultural competence?
The updated guidelines reflect cultural competence by recognizing the diverse backgrounds and experiences of patients, ensuring that care is comprehensive and culturally sensitive.
What are the recommended blood sugar control goals for critically ill individuals?
The guidelines suggest more stringent blood sugar control goals of 110–140 mg/dL (6.1–7.8 mmol/L) for selected critically ill individuals, if achievable without significant hypoglycemia.
What does Recommendation 15.27 promote regarding postpartum care?
Recommendation 15.27 promotes breastfeeding initiatives for all postpartum individuals with blood sugar issues, emphasizing breastfeeding as an important aspect of care after childbirth.
What are some lifestyle strategies recommended for diabetes management?
Recommended lifestyle strategies include engaging in outdoor activities, incorporating stress reduction techniques like yoga and meditation, and participating in community wellness programs.
What are the statistics related to prediabetes and diabetes from the recent case study?
The case study revealed that 23.0% of HbA tests indicated prediabetes, 5.5% showed elevated blood sugar levels, 30.8% of fasting plasma glucose tests indicated prediabetes, and 5.4% showed elevated blood sugar levels.
How do integrative functional medicine approaches improve care for metabolic conditions?
Integrative functional medicine approaches improve care by emphasizing tailored nutrition, lifestyle changes, community assistance, and comprehensive assessments to identify underlying issues contributing to diabetes.
What advancements in technology for managing blood sugar levels are highlighted in the guidelines?
The guidelines highlight advancements such as continuous glucose monitoring (CGM) and automated insulin delivery systems as vital tools for enhancing blood sugar management.
Why is mental well-being important in diabetes care?
Mental well-being is important in diabetes care as routine assessments for distress linked to metabolic conditions ensure a thorough and holistic approach to health management.