Overview
This article seeks to understand nursing diagnoses for Type 2 Diabetes, recognizing the unique challenges faced by patients. It emphasizes the importance of personalized care strategies, which are essential for effective management of this condition. By detailing common nursing diagnoses, assessment strategies, and interventions, healthcare providers can significantly improve patient outcomes. It’s important to recognize that personalized care plays a critical role in managing this chronic condition, fostering a nurturing environment that supports each patient’s journey.
Introduction
In the face of a global health crisis, Type 2 Diabetes has emerged as a significant challenge, affecting millions and reshaping lives. This chronic metabolic disorder, characterized by insulin resistance and elevated blood glucose levels, is not only the most common form of diabetes but also a precursor to serious health complications like cardiovascular disease and neuropathy. It’s important to recognize that as the prevalence of this condition continues to rise, healthcare providers are tasked with understanding its complexities and implementing effective management strategies.
Many patients find that the journey to reclaiming health is multifaceted. From personalized care plans to innovative programs like Dr. Jason Shumard’s 30-Day Diabetes Reset, there are pathways to improve health and well-being. This article delves into the critical nursing diagnoses, assessment strategies, interventions, and evaluation methods that are essential in empowering patients and improving their quality of life amidst the challenges posed by Type 2 Diabetes. Together, we can navigate this journey toward better health.
Overview of Type 2 Diabetes: Definition and Significance
Type 2 Diabetes Mellitus is a chronic metabolic condition characterized by insulin resistance and relative insulin deficiency, resulting in increased blood glucose levels. This condition is the most prevalent form of diabetes, accounting for approximately 90-95% of all diabetes cases worldwide. It’s important to recognize that as of 2025, the occurrence of Type 2 Diabetes continues to rise, with an estimated 537 million adults affected globally. This highlights its critical importance in public well-being.
The implications of Type 2 Diabetes extend far beyond elevated blood sugar levels; it is intricately linked to a range of serious complications, including:
- Cardiovascular disease
- Neuropathy
- Retinopathy
These complications not only pose risks to individuals’ health but also significantly impact their quality of life. Many patients find that they are at a heightened risk for cardiovascular issues, which remain a leading cause of morbidity and mortality among this population.
Grasping these intricacies is crucial for healthcare providers as they develop nursing diagnoses for diabetes type 2 and create care plans tailored to the unique needs of each individual. Effective management strategies, such as those implemented in Dr. Jason Shumard’s 30-Day Diabetes Reset program at the Integrative Wellness Center, empower individuals with actionable insights and practical tools to reclaim their health. Case studies from this program reveal transformative outcomes, with individuals expressing gratitude for the empowerment they feel in managing their condition.
One individual shared, “I lost 55 lbs. My A1C started at 9.1 after 8 months it is now 5.7,” which highlights the effectiveness of personalized care and the program’s impact on their overall well-being.
Moreover, expert opinions emphasize the necessity of a comprehensive approach to Type 2 Diabetes management. Endocrinologists stress that addressing the underlying causes of insulin resistance is crucial for preventing complications and improving patient outcomes. As MD. Jamal Hossain noted, “The corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis,” underscoring the importance of data-driven approaches in managing diabetes.
Additionally, conditions like impaired glucose tolerance (IGT) and impaired fasting glycaemia (IFG) are recognized as high-risk factors for progressing to Type 2 Diabetes, further emphasizing the need for early intervention and education.
In summary, the significance of Type 2 Diabetes in healthcare cannot be overstated. It is essential for healthcare providers to deepen their understanding of this condition, its complications, and effective management strategies, including the nursing diagnosis for diabetes type 2, as presented by Dr. Shumard at the Integrative Wellness Center. By doing so, they can provide optimal care and improve outcomes for those receiving care.
Common Nursing Diagnoses for Type 2 Diabetes Patients
Common nursing diagnoses for patients with Type 2 Diabetes encompass several critical areas that require attention and intervention:
- Risk for Unstable Blood Glucose Levels: Fluctuations in blood sugar levels can be challenging for many individuals. Factors such as dietary choices, medication adherence, and physical activity play a significant role. It’s important to recognize that effective interventions involve ongoing monitoring and thorough education on self-management strategies. This empowers individuals to maintain stable glucose levels. Notably, the SITA-HOSPITAL trial involving 279 individuals with type 2 diabetes highlights the importance of tailored interventions in managing these fluctuations. Utilizing tools like fitness apps and journals can enhance tracking efforts. Setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost focus and motivation.
- Imbalanced Nutrition: More than Body Requirements: Many individuals with Type 2 Diabetes face challenges related to obesity and excessive caloric intake. Nursing interventions should prioritize dietary education, emphasizing balanced nutrition and the adoption of healthy eating habits to support weight management and overall health. Dr. Jason Shumard’s holistic approach includes personalized guidance on nutrition, empowering individuals to make informed dietary choices that resonate with their personal health journeys.
- Deficient Knowledge Related to Diabetes Management: It’s common for patients to lack essential knowledge about their condition, which can impede effective self-management. Providing education on blood glucose monitoring techniques, medication administration, and necessary lifestyle modifications is crucial. As noted by Matt Vera, BSN, R.N., “Thank you for your kind words! We’re delighted to hear that you found the care plan useful,” underscoring the significance of effective care plans in diabetes management. Dr. Shumard’s 30-Day Reset program exemplifies this by providing patients with the tools and knowledge necessary to reverse their condition.
- Risk for Infection: Patients with diabetes are at an elevated risk for infections due to potential skin integrity issues and compromised immune function. Regular assessments and the implementation of preventive measures, such as proper hygiene practices and timely vaccinations, are vital to mitigate this risk.
- Impaired Skin Integrity: Diabetes can lead to various skin complications, particularly in the lower extremities. Nurses should perform regular skin evaluations and inform individuals about appropriate foot care methods to avert serious problems such as ulcers, which can greatly affect their quality of life.
The effectiveness of these nursing diagnoses and interventions is illustrated through Dr. Jason Shumard’s Functional Medicine Approach, which emphasizes a holistic strategy in managing diabetes. His 30-Day Reset program has proven to enable individuals, resulting in transformative outcomes and enhanced wellness management.
By identifying these typical nursing diagnoses for Type 2 Diabetes, healthcare professionals can create focused care strategies that effectively meet the distinct requirements of individuals with this condition. This ultimately enhances their health results and quality of life. Furthermore, the ongoing challenge of determining the optimal blood glucose concentration for ICU individuals highlights the necessity for personalized nursing interventions.
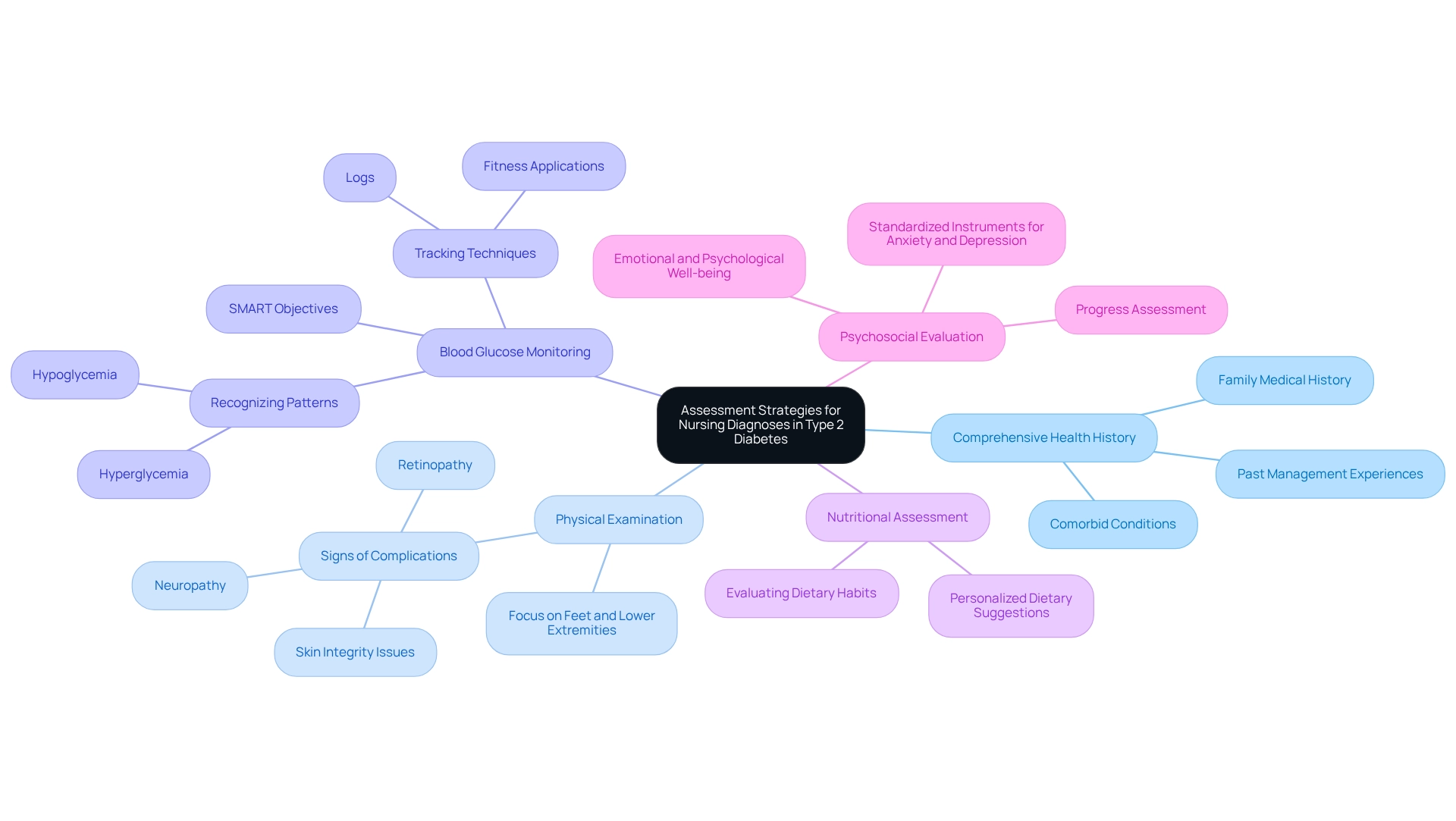
Assessment Strategies for Nursing Diagnoses in Type 2 Diabetes
Effective assessment strategies for nursing diagnoses in Type 2 Diabetes encompass several critical components that can truly make a difference in the lives of individuals facing this challenge.
- Comprehensive Health History: It is vital to collect thorough information regarding the individual’s medical background. This includes past management experiences with blood sugar issues, family medical history related to such conditions, and any comorbid conditions. By understanding these aspects, we can tailor our approach to care, in accordance with the principles of Dr. Jason Shumard‘s 30-Day Diabetes Reset program. This program equips individuals with the resources and understanding required for effective wellness management.
- Physical Examination: A thorough physical examination should focus on identifying signs of complications associated with diabetes, such as neuropathy, retinopathy, and skin integrity issues. Special attention must be given to the feet and lower extremities, as these areas are particularly vulnerable to complications. Many patients find that addressing these concerns early can significantly improve their quality of life.
- Blood Glucose Monitoring: Regular monitoring of blood glucose levels is vital for recognizing patterns of hyperglycemia or hypoglycemia. This information is essential for modifying treatment strategies and empowering individuals to take an active role in managing their well-being. Employing tracking techniques like fitness applications or logs can enhance this process, enabling individuals to establish SMART objectives—specific, measurable, attainable, relevant, and time-bound—to improve their outcomes.
- Nutritional Assessment: Evaluating dietary habits and nutritional intake is key to identifying imbalances that may impact blood sugar management. Instructing individuals on nutritious eating habits can greatly enhance their overall well-being and blood sugar control. A personalized approach, as promoted by functional medicine, can assist in adapting dietary suggestions to personal needs, addressing the underlying issues of blood sugar disorders rather than merely the symptoms.
- Psychosocial Evaluation: Comprehending the individual’s emotional and psychological well-being is essential, as stress and mental wellness concerns can significantly affect diabetes management. Utilizing standardized instruments to evaluate anxiety and depression levels can offer valuable insights into the individual’s overall well-being. Consistently assessing progress and adjusting objectives can enhance accountability and encouragement, further empowering individuals in their wellness journey.
By employing these thorough evaluation methods, nurses can effectively recognize the nursing diagnosis for Type 2 diabetes and create care plans that meet the varied needs of individuals. This approach not only improves outcomes for individuals but also fosters a supportive atmosphere where people feel capable of taking charge of their well-being proactively. As Dr. Jason Shumard states, “By providing individuals with actionable insights and practical tools, the Integrative Wellness Center fosters an environment where they can reclaim their health and well-being.”
Incorporating case studies that illustrate the life-altering results reported by individuals further emphasizes the effectiveness of these assessment strategies, showcasing the success of the groundbreaking program offered by the Integrative Wellness Center.
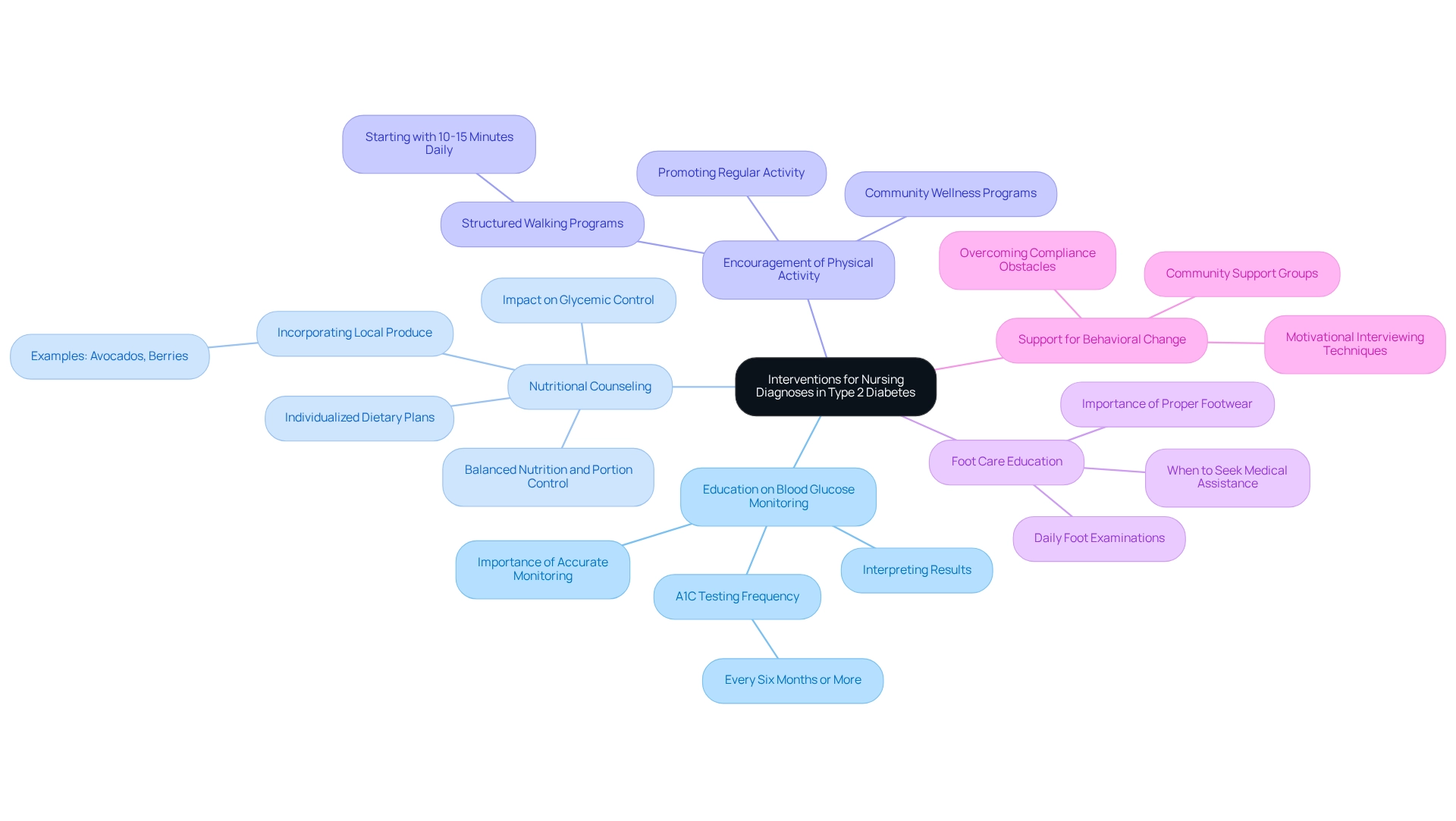
Interventions for Nursing Diagnoses in Type 2 Diabetes
Nursing interventions for common diagnoses in Type 2 Diabetes encompass a range of strategies aimed at improving patient outcomes and empowering individuals to manage their condition effectively.
- Education on Blood Glucose Monitoring: It’s important to recognize that nurses play a crucial role in instructing individuals on how to accurately monitor their blood glucose levels. This includes interpreting results and understanding when to seek medical advice. Regular monitoring is essential; individuals should plan to get an A1C test every six months or more frequently, as advised by their healthcare team.
- Nutritional Counseling: Many patients find that providing individualized dietary plans is essential for managing blood sugar levels. These plans should emphasize balanced nutrition, portion control, and carbohydrate counting. Research suggests that effective nutritional guidance can result in significant enhancements in glycemic control, with individuals experiencing improved management of their diabetes through customized dietary strategies. Incorporating local produce, such as avocados and berries, can enhance these plans, especially for those living in areas like San Marcos, CA.
- Encouragement of Physical Activity: Promoting regular physical activity is critical for enhancing insulin sensitivity and overall health. Nurses should motivate individuals to participate in physical activities that suit their abilities and preferences, such as walking in local parks or joining community wellness programs. This can lead to improved metabolic outcomes and a better quality of life. A structured walking program, as detailed in the user guide, can assist individuals in gradually raising their activity levels, beginning with achievable objectives like 10-15 minutes of walking each day. The walking program PDF offers specific guidelines to help individuals in creating a consistent routine.
- Foot Care Education: Proper foot care is vital for individuals with diabetes to prevent complications. Nurses should guide individuals on daily foot examinations, the significance of using suitable footwear, and identifying when to seek medical assistance for foot problems. This proactive approach can significantly reduce the risk of serious complications.
- Support for Behavioral Change: Utilizing motivational interviewing techniques can help nurses assist individuals in making necessary lifestyle changes. By tackling obstacles to compliance and establishing attainable objectives, nurses can enable patients to take charge of their well-being. Engaging in community support, such as walking groups, can enhance accountability and motivation.
The effectiveness of these interventions is underscored by case studies demonstrating the positive impact of continuous glucose monitoring (CGM) devices. For instance, a study revealed that transitioning from self-monitoring of blood glucose to CGM resulted in a significant decrease in mean HbA1c levels from 11.21% to 7.04%, with average blood glucose levels dropping from 286 mg/dl to 158 mg/dl, and a notable reduction in hypoglycemic events. This highlights the significance of continuous education and oversight in managing blood sugar conditions.
A CGM user shared their experience: “I woke up in the middle of the night to my CGM warning me about a severe low blood glucose. It said I was in the 40s and trending down… I was grateful my CGM woke me up and that I had my handheld blood glucose monitor nearby to double check my numbers.”
This personal narrative emphasizes the essential function of ongoing glucose monitoring in effectively managing the condition and aligns with the functional medicine approach that incorporates various strategies for comprehensive wellness management.
By applying these thorough nursing strategies, healthcare professionals can greatly improve the nursing diagnosis for diabetes type 2, thereby creating a setting where individuals feel enabled to take control of their health and enhance their overall quality of life. Future studies should also consider the constraints of CGM devices and investigate their wider relevance in managing blood sugar.
Evaluation of Nursing Diagnoses and Patient Outcomes
Evaluating nursing diagnoses and patient outcomes in Type 2 Diabetes involves several critical components:
- Monitoring Blood Glucose Levels: Regular assessment of blood glucose levels is essential for determining the effectiveness of interventions. This continuous oversight enables healthcare practitioners to make prompt modifications to the care strategy, ensuring optimal management of the condition. Research suggests that efficient blood glucose monitoring greatly improves outcomes for individuals, with participants noting better control over their condition. Significantly, individuals with diabetes for over 15 years had a confidence score of 7.95 ± 1.30, highlighting the importance of monitoring in enhancing confidence.
- Reviewing Dietary Adherence: Assessing an individual’s compliance with dietary recommendations is essential. This includes evaluating changes in weight and nutritional status, which can directly impact blood glucose levels. In San Marcos, CA, individuals can benefit from local farmers’ markets that offer fresh, seasonal produce, such as avocados and berries, which are rich in fiber and nutrients essential for regulating blood sugar levels. Statistics indicate that dietary adherence rates among individuals with Type 2 diabetes can differ, emphasizing the necessity for tailored dietary approaches that align with personal lifestyles and preferences. Furthermore, individuals released on steroids should obtain clear strategies for managing potential hyperglycemia, which is essential for maintaining stable blood glucose levels.
- Assessing Physical Activity Levels: Monitoring engagement in physical activity is vital, as it plays a significant role in blood glucose control and overall health. Consistent physical activity, like hiking at Lake San Marcos or strolling the paths at Discovery Lake, has been associated with enhanced insulin sensitivity and better control of blood sugar, making it a crucial component of patient assessments. Many patients find that using technology, such as insulin pumps, significantly assists in managing their condition. One participant remarked, “My insulin pump certainly assists, so the best method I’ve used to manage my condition is through the insulin pump,” demonstrating the influence of technology on physical activity and management of the illness. Highlighting the outdoor lifestyle in San Marcos, participating in these activities not only promotes physical fitness but also improves mental well-being.
- Client Feedback: Actively seeking input from individuals regarding their comprehension of diabetes management and contentment with care is invaluable. This feedback not only assists in recognizing difficulties encountered by individuals but also enables them to take an active role in their health journey. Involving individuals in their care promotes a sense of ownership and can result in improved adherence to treatment plans. Community wellness initiatives in San Marcos can offer extra assistance and resources designed for managing diabetes, improving engagement. Dr. Jason Shumard’s tailored support can further empower individuals in their management journey.
- Adjusting Care Plans: Based on evaluation findings, healthcare providers should be prepared to modify care plans to better meet the individual’s needs. This adaptability ensures that interventions stay pertinent and effective, ultimately resulting in enhanced outcomes for individuals. For example, participants in a recent case study titled ‘Use of Technology in Diabetes Self-Management’ reported that utilizing mobile applications, insulin pumps, and continuous glucose monitors (CGM) enhanced their ability to manage their condition effectively, providing better data access and reminders for medication.
By performing comprehensive assessments that include these components, healthcare providers can guarantee that the nursing diagnosis for diabetes type 2 leads to favorable outcomes for individuals and ongoing enhancement in managing blood sugar conditions. This holistic approach not only addresses the symptoms of diabetes but also empowers patients to reclaim their health and well-being through personalized guidance and community support, including the functional medicine strategies offered by Dr. Jason Shumard.
Conclusion
Type 2 Diabetes is more than just a health condition; it represents a significant public health challenge that impacts millions of lives worldwide. Many individuals struggle with serious complications that can greatly affect their quality of life. It’s important to recognize that a comprehensive understanding of this condition, along with effective nursing diagnoses and interventions, is crucial for promoting better health outcomes. By addressing common issues such as unstable blood glucose levels, nutritional imbalances, and the need for patient education, healthcare providers can empower individuals to take control of their health.
Assessment strategies play a vital role in identifying the unique needs of each patient. This personalized approach allows for tailored care plans that enhance self-management. Regular monitoring of blood glucose, dietary adherence, and physical activity levels are essential components in evaluating the effectiveness of interventions. Many patients find that these evaluations foster a supportive environment where they feel engaged and motivated to manage their diabetes effectively.
Through innovative programs like Dr. Jason Shumard’s 30-Day Diabetes Reset, patients gain access to the resources and knowledge necessary to reclaim their health. The integration of educational initiatives, behavioral support, and community engagement highlights the importance of a holistic approach in diabetes management. As healthcare providers continue to adapt and refine their strategies, the potential for improved patient outcomes remains promising. Ultimately, prioritizing personalized care and empowering patients can lead to transformative changes in the lives of those living with Type 2 Diabetes. Together, we can navigate this journey toward better health.
Frequently Asked Questions
What is Type 2 Diabetes Mellitus?
Type 2 Diabetes Mellitus is a chronic metabolic condition characterized by insulin resistance and relative insulin deficiency, which leads to increased blood glucose levels. It accounts for approximately 90-95% of all diabetes cases worldwide.
How many adults are estimated to be affected by Type 2 Diabetes by 2025?
By 2025, it is estimated that approximately 537 million adults globally will be affected by Type 2 Diabetes.
What are the serious complications associated with Type 2 Diabetes?
The complications associated with Type 2 Diabetes include cardiovascular disease, neuropathy, and retinopathy, which can significantly impact individuals’ health and quality of life.
What is the significance of understanding Type 2 Diabetes for healthcare providers?
Understanding Type 2 Diabetes is crucial for healthcare providers as it helps them develop appropriate nursing diagnoses and care plans tailored to the unique needs of individuals with the condition.
What management strategies are mentioned for Type 2 Diabetes?
Effective management strategies include personalized care and education, as exemplified by Dr. Jason Shumard’s 30-Day Diabetes Reset program, which provides actionable insights and practical tools for individuals to manage their condition.
What are common nursing diagnoses for patients with Type 2 Diabetes?
Common nursing diagnoses include: 1. Risk for Unstable Blood Glucose Levels 2. Imbalanced Nutrition: More than Body Requirements 3. Deficient Knowledge Related to Diabetes Management 4. Risk for Infection 5. Impaired Skin Integrity
How can healthcare professionals address the risk for unstable blood glucose levels?
Healthcare professionals can address this risk through ongoing monitoring, education on self-management strategies, and utilizing tools like fitness apps and journals to track blood glucose levels.
Why is dietary education important for individuals with Type 2 Diabetes?
Dietary education is important to help individuals manage obesity and caloric intake, promoting balanced nutrition and healthy eating habits that support weight management and overall health.
What role does education play in diabetes management?
Education is critical for helping patients understand blood glucose monitoring, medication administration, and necessary lifestyle modifications, which empowers them to manage their condition effectively.
What preventive measures can be taken to reduce the risk of infection in diabetes patients?
Preventive measures include regular assessments, proper hygiene practices, and timely vaccinations to mitigate the risk of infections due to potential skin integrity issues and compromised immune function.