Introduction
Understanding A1C is essential for effective diabetes management, as it provides critical insights into an individual’s average blood glucose levels over the past few months. This key metric not only serves as a benchmark for assessing long-term glucose control but also plays a pivotal role in guiding treatment decisions and lifestyle modifications. With the prevalence of diabetes on the rise, recognizing the significance of A1C testing becomes increasingly vital for both patients and healthcare providers.
By exploring the factors that influence A1C levels, the relationship between A1C and daily blood glucose measurements, and the importance of a well-structured diet, this article aims to empower individuals with the knowledge needed to take charge of their health and enhance their diabetes management strategies. Through a comprehensive understanding of A1C, patients can make informed choices that lead to improved health outcomes and a better quality of life.
Understanding A1C: Definition and Importance in Diabetes Management
A1C, commonly referred to as glycated hemoglobin, is an essential blood test that reveals the A1C correlation to blood glucose levels over the past two to three months. Expressed as a percentage, elevated A1C readings suggest A1C correlation to blood glucose management, which can be particularly alarming for individuals diagnosed with type 2. It is generally recommended to maintain an A1C level below 7% to ensure a favorable A1C correlation to blood glucose and reduce the risk of diabetes-related complications.
A1C testing is essential in controlling blood sugar levels as it helps establish A1C correlation to blood glucose, assisting healthcare providers in assessing the effectiveness of treatment strategies and making required adjustments. Regular monitoring is essential; as stated by the National Center for Health Statistics, the age-adjusted prevalence of undiagnosed high blood sugar stands at 4.2% among all adults, with 4.9% for men and 3.5% for women. This highlights the significance of awareness and proactive oversight in the community.
Furthermore, understanding A1C levels can help alleviate the anxiety associated with managing the condition, empowering patients to take control of their health. Type 2 diabetes mellitus is often connected to insulin secretory defects influenced by genetic predisposition, inflammation, and metabolic stress, which highlights the importance of the A1C correlation to blood glucose in understanding and managing the condition. In addition to monitoring A1C, incorporating lesser-known strategies such as:
- Stress reduction techniques
- Personalized nutrition plans
- Community support programs
can significantly enhance health and assist in reversing blood sugar issues.
By understanding the importance of A1C and adopting a holistic approach, patients can take an active part in their condition management, resulting in informed choices that positively influence their health outcomes. The criteria for diagnosing undiagnosed conditions, as noted by the National Center for Health Statistics, include:
- An 8- to 24-hour fasting plasma glucose greater than or equal to 126 mg/dL
- Hemoglobin A1C greater than or equal to 6.5%
highlighting the A1C correlation to blood glucose in individuals who have never received a diagnosis from a healthcare provider. This holistic approach not only empowers patients but also emphasizes the importance of education, nutrition, and support within community wellness programs to enhance health and reverse diabetes effectively.
The Correlation Between A1C Levels and Blood Glucose Measurements
Research consistently demonstrates a strong A1C correlation to blood glucose concentrations. For instance, an A1C level of 6% typically corresponds to an average blood glucose level of approximately 126 mg/dL. This established relationship serves as a standardized framework for assessing the A1C correlation to blood glucose and long-term glucose control.
Notably, the sample sizes in relevant studies include:
- 1,306 men
- 1,632 women
This reinforces the validity of these findings. However, it is essential to recognize that individual variations can influence A1C results. Factors such as anemia, age, and other health conditions may lead to discrepancies, underscoring the necessity of contextual interpretation of A1C measurements.
At the Integrative Wellness Center, we emphasize a holistic approach that addresses the root causes of the condition, empowering patients to reverse their situation through personalized care. For example, one patient, after implementing our recommended lifestyle changes and treatment options, successfully lowered their A1C from 8% to 5.5%. Case studies reveal transformative success stories, showcasing how patients have overcome chronic health issues by integrating lifestyle changes and comprehensive treatment options.
The case study titled ‘Trends in Prevalence of Diabetes (2001–2020)’ highlights that the age-adjusted prevalence of diagnosed conditions significantly increased from 10.3% in 2001–2004 to 13.2% in 2017–2020, underscoring a growing public health concern that emphasizes the importance of A1C monitoring. As a result, while the A1C correlation to blood glucose remains a valuable tool for overseeing blood sugar levels, it should be used alongside regular daily glucose checks to offer a thorough understanding of an individual’s condition. Current research emphasizes this dual approach, reinforcing the Integrative Wellness Center’s commitment to empowering patients through informed, holistic care.
Factors Influencing A1C Levels
A variety of factors can significantly influence the A1C correlation to blood glucose, such as diet, exercise, stress, and adherence to medication regimens. At the Integrative Wellness Center, we adopt a holistic approach to blood sugar control that emphasizes addressing root causes and empowering patient health. A well-organized diet, emphasizing consistent carbohydrate consumption and balanced meals, is crucial for sustaining stable blood glucose rates, demonstrating A1C correlation to blood glucose, which directly influences A1C control.
Research has shown that a plant-based diet can greatly benefit glycemic control and overall cardiometabolic health. For example, the Mayo Clinic Diet presents a two-phase method that encourages nutritious eating and weight control, offering a structured framework essential for individuals with health issues. Consistent physical activity is also crucial, as it improves insulin sensitivity, aiding in the reduction of blood glucose concentrations.
On the other hand, stress can result in hormonal changes that raise blood glucose, requiring effective stress control methods as part of a comprehensive care strategy. Furthermore, adherence to prescribed medications is critical; non-compliance can lead to an increased A1C correlation to blood glucose readings. In fact, adults with family income exceeding 500% of the federal poverty threshold had the lowest occurrence of diagnosed health issues at 6.3% for men and 3.9% for women, highlighting the significance of socioeconomic factors in health care.
Therefore, it is imperative for individuals to monitor these factors closely and engage in open discussions with their healthcare providers to effectively optimize management of the condition. As H.K. stated, “Our study emphasizes the significant role of diet in managing the A1C correlation to blood glucose, as evidenced by the positive outcomes observed in participants following structured dietary plans.”
Numerous patients, including Sarah, have recounted their experiences: “Since beginning the program, my anxiety regarding my condition has decreased significantly, and there is a noticeable A1C correlation to blood glucose improvement.” By challenging common health myths and embracing a breakthrough approach, patients can experience transformative health improvements at the Integrative Wellness Center. We begin by re-evaluating the origin of your condition, ensuring that every aspect of your health is addressed holistically.
The Role of Diet and Nutrition in Managing A1C Levels
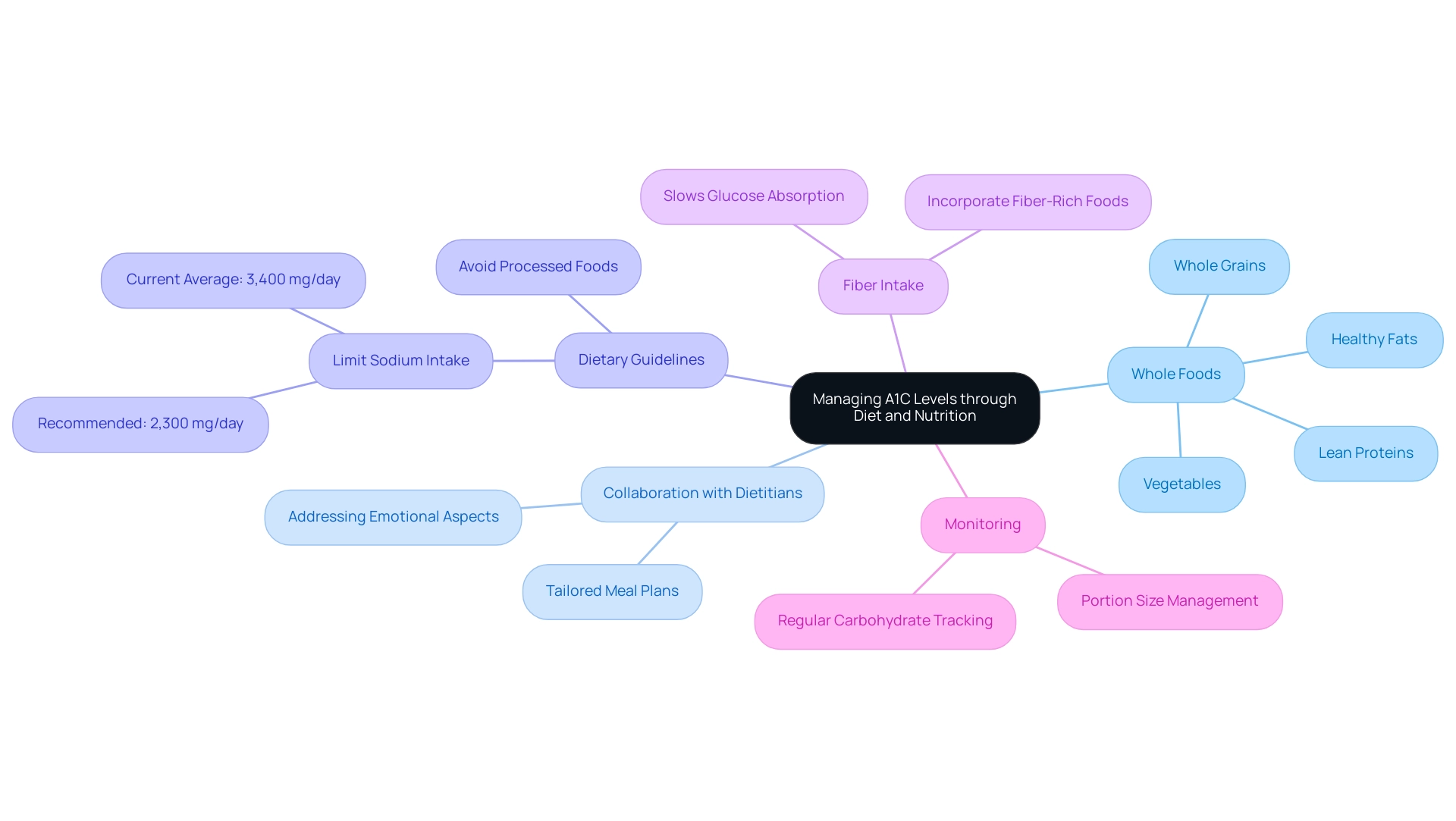
A well-balanced diet is essential for effectively managing the a1c correlation to blood glucose in individuals with blood sugar issues, particularly through a holistic approach that addresses root causes. Focusing on whole foods—including a variety of vegetables, lean proteins, whole grains, and healthy fats—can significantly help stabilize blood glucose levels and reduce the anxiety related to potential complications of this condition. It is advisable to limit the intake of processed foods, sugary beverages, and high-glycemic index foods that tend to cause sharp spikes in blood sugar.
Additionally, incorporating fiber-rich foods plays a crucial role in blood sugar control, as fiber can slow down glucose absorption. The American Diabetes Association (ADA) claims that, ‘The objective for most adults with the condition is an A1C of less than 7%,’ which underscores the a1c correlation to blood glucose and the significance of dietary control in achieving this goal. Patients are encouraged to collaborate with a registered dietitian and other healthcare professionals to create a tailored meal plan that aligns with their health objectives and lifestyle preferences.
This collaboration is vital for addressing both the physical and emotional aspects of diabetes management. Regular monitoring of carbohydrate intake and portion sizes is essential for maintaining optimal values in the A1C correlation to blood glucose. In 2024, recent dietary guidelines recommend limiting sodium intake to 2,300 mg per day, as current averages soar around 3,400 mg, primarily due to processed foods.
Moreover, approaches like physical activity, diet, and medication can collectively assist in effectively managing the a1c correlation to blood glucose values. An analysis of 29 randomized controlled trials regarding artificial sweeteners suggests that they do not increase blood sugar concentrations; however, the overall composition of the food or beverage should be taken into account, particularly for individuals with insulin sensitivity. By addressing anxiety associated with complications of blood sugar issues and incorporating these strategies into a comprehensive approach, patients can attain better glucose control and improved overall well-being.
Regular Monitoring of A1C Levels: Best Practices
Tracking the A1C correlation to blood glucose is essential for the efficient management of blood sugar conditions, particularly for older individuals with such conditions and additional health issues. For individuals with well-managed blood sugar levels, it is recommended to perform A1C testing at least twice a year. In contrast, those whose treatment has changed or who are struggling to meet their glycemic targets should have their A1C readings evaluated quarterly.
It’s important to note that treatment plans for older adults should include agents that reduce cardiorenal risk, regardless of glycemia. Understanding the A1C correlation to blood glucose is crucial; an A1C level below 5.7% is categorized as normal, while levels ranging from 5.7% to 6.4% suggest prediabetes, and an A1C of 6.5% or above confirms a diagnosis of the condition. Continuous dialogue with healthcare providers concerning A1C results enables personalized modifications to care plans as required.
Furthermore, keeping a detailed record of A1C results over time not only helps in tracking progress but also acts as a motivational tool for patients to follow their strategies. Furthermore, regulation of blood pressure and cholesterol reduction with statins have been linked to a lower risk of developing dementia, emphasizing the interrelation of these factors in health care. It is crucial to acknowledge that insulin resistance can complicate the control of blood sugar levels and that conventional therapies may present hazards, especially for elderly individuals.
Roopa Naik emphasizes the importance of regular monitoring, stating, ‘Disclosure: Roopa Naik declares no relevant financial relationships with ineligible companies.’ Moreover, recognizing overtreatment in older adults, as discussed in the case study on overtreatment and its implications, is essential for preventing unnecessary medication burden. These practices align with the latest recommendations for A1C monitoring and reflect the consensus among care experts on the A1C correlation to blood glucose as a best practice for maintaining optimal glycemic control.
Integrating considerations about Alzheimer’s and dementia into diabetes management strategies is also crucial, as these conditions can significantly impact hospitalization rates and overall health outcomes for older adults.
Conclusion
Understanding A1C levels is fundamental for effective diabetes management, as it provides insights into average blood glucose levels and influences treatment decisions. The correlation between A1C levels and daily blood glucose measurements underscores the importance of regular monitoring. This dual approach, combined with a well-structured diet and lifestyle modifications, empowers individuals to take control of their health and improve their outcomes.
Various factors, including diet, exercise, stress management, and medication adherence, play a pivotal role in influencing A1C levels. Emphasizing a balanced diet rich in whole foods and fiber can stabilize blood glucose and reduce anxiety related to diabetes complications. Collaborating with healthcare professionals to create personalized meal plans further enhances the ability to manage A1C effectively.
Regular A1C testing is essential, particularly for those with changing treatment plans or difficulties in achieving glycemic targets. Maintaining open communication with healthcare providers and keeping detailed records of A1C results can motivate individuals to adhere to their management strategies. By integrating these best practices, individuals can navigate their diabetes journey more effectively, fostering better health and quality of life.
Frequently Asked Questions
What is A1C and why is it important?
A1C, or glycated hemoglobin, is a blood test that indicates the correlation between A1C levels and blood glucose over the past two to three months. It is important for managing blood sugar levels, particularly for individuals diagnosed with type 2 diabetes, as elevated A1C readings can indicate poor blood glucose management.
What is the recommended A1C level for individuals with diabetes?
It is generally recommended to maintain an A1C level below 7% to ensure effective blood glucose management and reduce the risk of diabetes-related complications.
How does A1C testing assist healthcare providers?
A1C testing helps healthcare providers assess the effectiveness of treatment strategies and make necessary adjustments to improve blood sugar control.
What are the prevalence rates of undiagnosed high blood sugar among adults?
According to the National Center for Health Statistics, the age-adjusted prevalence of undiagnosed high blood sugar is 4.2% among all adults, with 4.9% for men and 3.5% for women.
How can understanding A1C levels help patients with diabetes?
Understanding A1C levels can alleviate anxiety related to managing the condition and empower patients to take control of their health through informed decision-making.
What factors can complicate A1C results?
Factors such as anemia, age, and other health conditions can influence A1C results, highlighting the need for contextual interpretation of these measurements.
What strategies can enhance health and assist in reversing blood sugar issues?
Strategies include stress reduction techniques, personalized nutrition plans, and community support programs.
What are the diagnostic criteria for undiagnosed diabetes?
The diagnostic criteria include a fasting plasma glucose level greater than or equal to 126 mg/dL or a hemoglobin A1C level greater than or equal to 6.5%.
How does A1C correlate with average blood glucose levels?
An A1C level of 6% typically corresponds to an average blood glucose level of approximately 126 mg/dL, establishing a standardized framework for assessing blood glucose control.
What is the trend in the prevalence of diagnosed diabetes?
The age-adjusted prevalence of diagnosed diabetes has increased from 10.3% in 2001–2004 to 13.2% in 2017–2020, indicating a growing public health concern.