Overview
This article addresses the effective management strategies for Type 2 diabetes, recognizing the challenges many face. Understanding insulin resistance is crucial, and adopting lifestyle changes can feel overwhelming at times. However, utilizing educational resources can make a significant difference. It’s important to recognize that improvements in diet, exercise, and glucose monitoring can greatly enhance glycemic control and overall well-being. Many patients find that proactive management empowers them to take charge of their health, fostering a sense of independence and confidence. By embracing these strategies, you can embark on a journey toward a healthier life.
Introduction
Understanding the intricate relationship between insulin and Type 2 diabetes is crucial for effectively managing this prevalent condition. Many individuals face the challenge of insulin resistance, which can feel overwhelming. It’s important to recognize that lifestyle modifications and personalized treatment strategies play a pivotal role in empowering you to take control of your health. With so much information available, you might wonder how to navigate the complexities of insulin management. How can you make meaningful changes that lead to improved outcomes?
By acknowledging these struggles, we can explore how small, manageable steps can lead to significant improvements in your health journey. Many patients find that making simple adjustments to their daily routines can have a profound impact. This journey is not just about managing diabetes; it’s about reclaiming your well-being and feeling more in control. Together, we can uncover the strategies that resonate with you and support you in achieving your health goals.
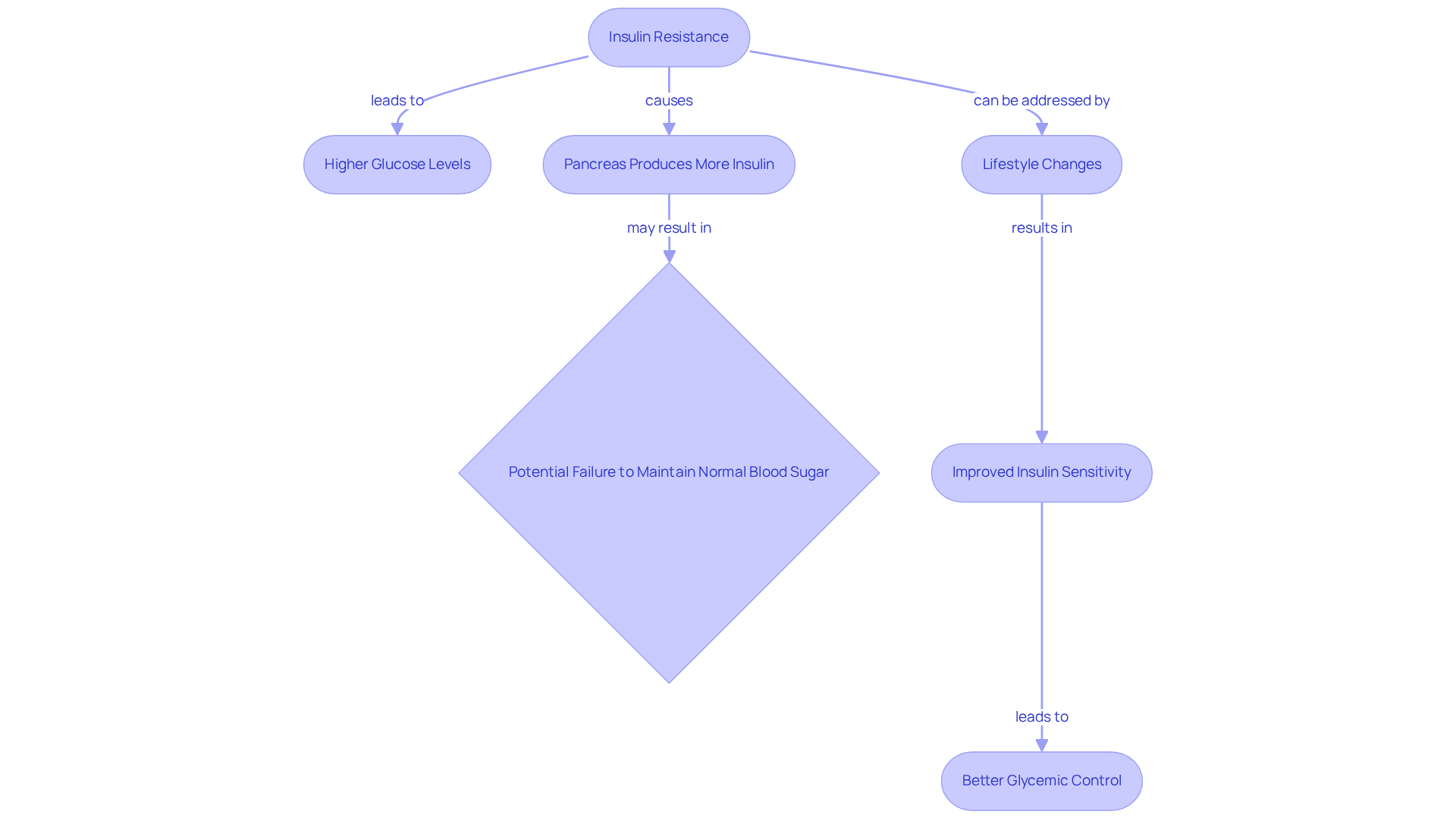
Understand Type 2 Diabetes and Insulin’s Role
Type 2 diabetes often stems from insulin resistance, which is a condition related to insulin and diabetes type 2, where your body’s cells struggle to respond to insulin, leading to higher glucose levels. Insulin, which is produced by the pancreas, is essential for helping your cells absorb glucose, particularly in the context of insulin and diabetes type 2. In the face of glucose intolerance, the pancreas tries to compensate by producing more insulin; however, this increased output may eventually fall short of maintaining normal blood sugar levels.
It’s important to recognize that understanding this mechanism is vital for patients. Efficient hormone management is a key part of your treatment strategy. Many patients find that addressing insulin resistance can improve insulin and diabetes type 2 management through lifestyle changes—such as adopting a healthier diet and increasing physical activity—leading to significant improvements in glycemic control and a reduced risk of complications.
For instance, studies show that individuals who embrace healthier habits often experience remarkable enhancements in their glucose sensitivity. This can help stabilize sugar levels and improve overall well-being. This holistic approach not only empowers you but also encourages a proactive stance toward effectively managing your diabetes. Remember, small changes can lead to meaningful results on your journey to better health.
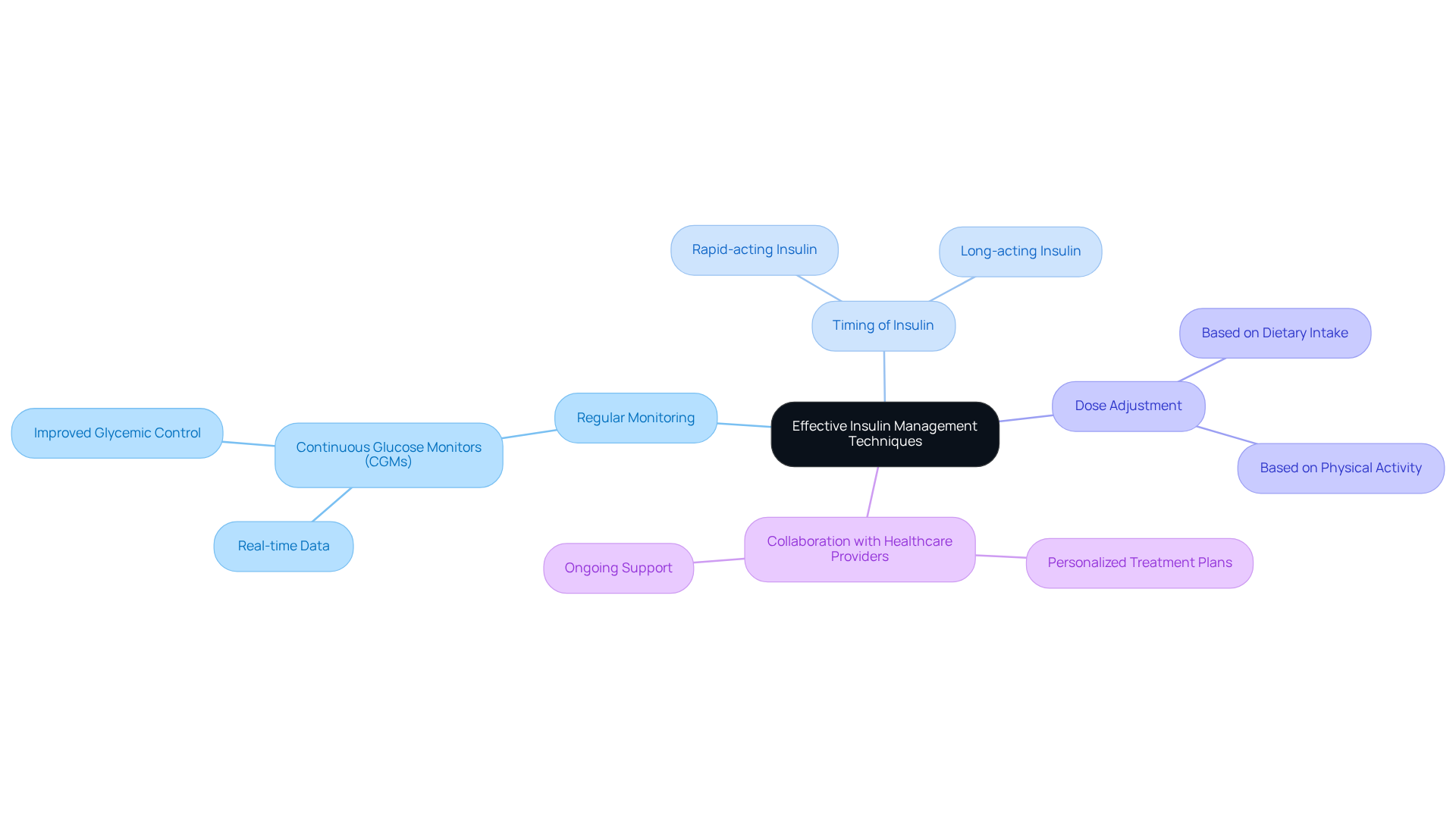
Implement Effective Insulin Management Techniques
Managing glucose levels can be a challenging journey, filled with ups and downs. It’s essential to recognize that effective glucose management for insulin and diabetes type 2 encompasses various strategies, including:
- Regular monitoring of glucose levels
- Understanding the timing of insulin administration
- Adjusting doses based on dietary intake and physical activity
Collaborating closely with healthcare providers is vital in crafting a personalized treatment plan that meets your unique needs.
Many patients find that continuous glucose monitors (CGMs) are invaluable tools in this process. By providing real-time data on blood sugar fluctuations, CGMs enable timely adjustments to insulin and diabetes type 2 doses, making it easier to stay on track. Moreover, understanding the different types of insulin and diabetes type 2—such as rapid-acting and long-acting—empowers you to take charge of your health more effectively.
Research has shown that using CGMs can lead to significant improvements in glycemic control, resulting in lower HbA1c levels and fewer instances of hypoglycemia. This underscores the importance of these devices in modern diabetes management. Remember, you’re not alone in this journey; with the right support and tools, you can navigate the complexities of glucose management with confidence.
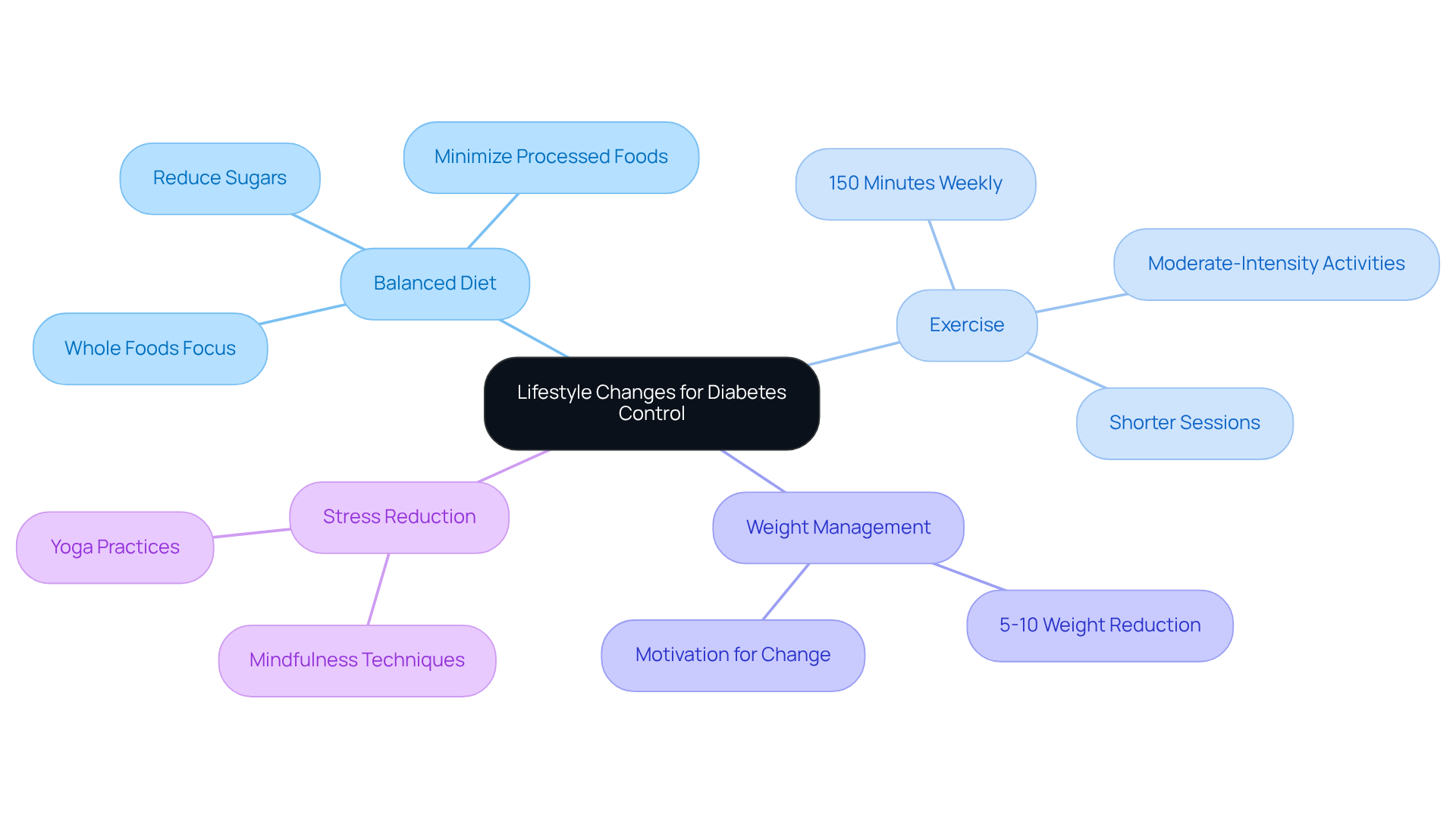
Adopt Lifestyle Changes for Optimal Diabetes Control
Adopting lifestyle changes is essential for optimal diabetes control, especially considering that treatment cannot be a one-size-fits-all approach. It’s important to recognize that many individuals face challenges in managing their condition, and there are key strategies that can make a significant difference:
- Balanced Diet: Maintaining a diet rich in whole foods—such as fruits, vegetables, whole grains, and lean proteins—while minimizing processed foods and sugars can lead to better health outcomes.
- Exercise: Many health organizations recommend at least 150 minutes of moderate-intensity exercise per week. This can improve insulin sensitivity and aid in weight management, which is crucial for those living with insulin and diabetes type 2.
- Weight Management: Studies show that even a modest weight reduction of 5-10% can lead to notable enhancements in glucose levels and overall health. This can be a powerful motivator for individuals seeking to improve their condition.
- Stress Reduction: Engaging in stress-reduction techniques, such as mindfulness and yoga, can also positively impact blood sugar control. It’s incredible how much our mental well-being can influence our physical health.
As noted by Deepak Hiwale, ‘Exercise and diet can help prevent or even completely reverse metabolic conditions such as high blood sugar and cardiovascular disease.’ Real-world examples demonstrate that individuals who adopt these dietary and exercise strategies often experience remarkable improvements in their management of insulin and diabetes type 2. This reinforces the critical role of personalized lifestyle changes in controlling insulin and diabetes type 2 effectively. These changes not only enhance blood sugar regulation but also contribute to improved quality of life and reduced reliance on conventional medical interventions, highlighting the transformative potential of holistic care.
Furthermore, numerous patients at Integrative Wellness Center have shared their success stories, showcasing how personalized lifestyle changes have led to significant advancements in their condition management. Our breakthrough method for type 2 blood sugar condition patients empowers individuals to take control of their health and achieve lasting results. Remember, you are not alone on this journey—support is available, and positive change is possible.
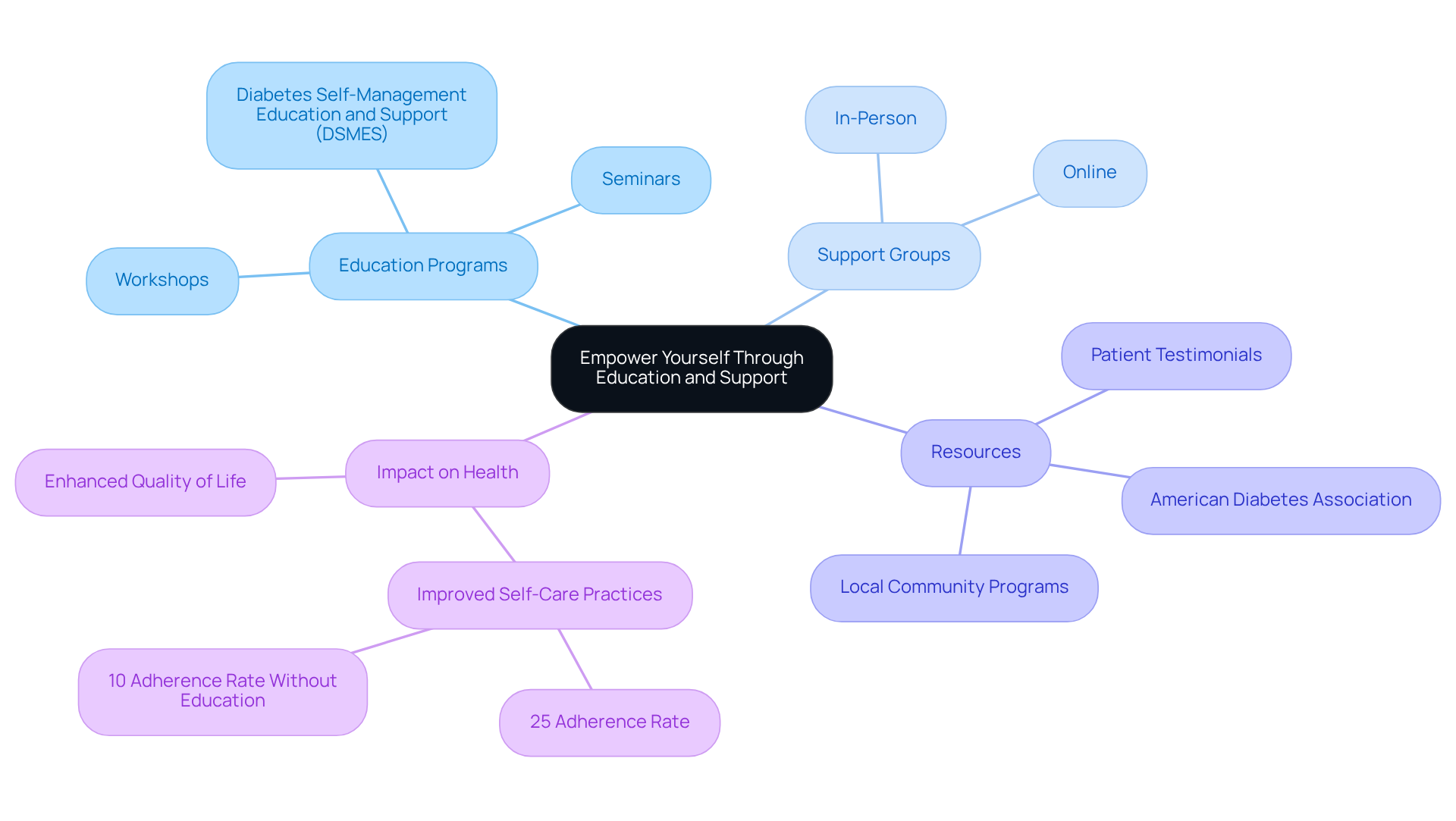
Empower Yourself Through Education and Support
Empowering oneself through education is essential for effectively managing your health. It’s important to recognize that patients often face numerous challenges, and participating in education programs can provide valuable insights into navigating these difficulties. Support groups, whether in-person or online, offer not only emotional support but also practical advice from peers who understand what you’re going through. Resources such as the American Diabetes Association and local community programs can be invaluable for accessing tools and information tailored to managing insulin and diabetes type 2.
Many patients find that engaging in educational opportunities makes a significant difference. In fact, research indicates that almost 25% of individuals who received education on managing their condition adhered to at least 9 out of 10 recommended self-care practices, compared to only 10% of those who did not receive such instruction. Attending seminars and workshops further enhances knowledge and fosters a sense of community among individuals with diabetes.
Testimonials from patients highlight the transformative impact of these educational resources and support networks. They reinforce the notion that when you are informed and connected, you are better equipped to manage your health effectively. Remember, you are not alone on this journey, and there are many resources available to support you every step of the way.
Conclusion
Understanding and managing type 2 diabetes, especially through the lens of insulin, is vital for achieving better health outcomes. It’s important to recognize the challenges many face with insulin resistance and its impact on glucose levels. Effective management involves a blend of lifestyle changes, education, and support. By taking a proactive approach to insulin management, individuals can significantly enhance their overall well-being and reduce the risk of complications associated with diabetes.
Key strategies include:
- Adopting a balanced diet
- Engaging in regular physical activity
- Utilizing continuous glucose monitors to improve glycemic control
Each of these components plays a crucial role in managing insulin levels and enhancing the body’s response to glucose. Many patients find that education and support networks are invaluable, empowering them to take charge of their health and make informed decisions about their treatment plans.
Ultimately, the journey of managing type 2 diabetes does not have to be faced alone. By embracing personalized lifestyle changes and seeking out educational resources and support, individuals can transform their approach to diabetes management. This holistic strategy not only fosters better health outcomes but also enhances quality of life. Remember, with the right tools and knowledge, meaningful change is within reach. You are not alone on this journey—support is available, and together we can navigate the path to better health.
Frequently Asked Questions
What is Type 2 diabetes and how is it related to insulin?
Type 2 diabetes often arises from insulin resistance, where the body’s cells have difficulty responding to insulin, resulting in elevated glucose levels. Insulin, produced by the pancreas, is crucial for helping cells absorb glucose.
What happens when the body experiences insulin resistance?
When insulin resistance occurs, the pancreas attempts to compensate by producing more insulin. However, this increased insulin output may eventually be insufficient to maintain normal blood sugar levels.
Why is understanding insulin’s role important for patients with Type 2 diabetes?
Understanding the mechanism of insulin resistance is vital for patients as it is essential for effective hormone management, which is a key part of their treatment strategy.
How can lifestyle changes impact the management of Type 2 diabetes?
Many patients find that addressing insulin resistance through lifestyle changes, such as a healthier diet and increased physical activity, can improve insulin management, leading to better glycemic control and a reduced risk of complications.
What benefits can healthier habits provide for individuals with Type 2 diabetes?
Studies indicate that individuals who adopt healthier habits often see significant improvements in their glucose sensitivity, which can stabilize sugar levels and enhance overall well-being.
What is the overall approach recommended for managing Type 2 diabetes?
A holistic approach that includes lifestyle changes empowers patients and encourages a proactive stance toward effectively managing diabetes, with the understanding that small changes can lead to meaningful health improvements.