Overview
Managing blood sugar levels in type 2 diabetes can feel overwhelming at times, but there are effective strategies that can help. A balanced diet, regular exercise, and continuous monitoring of glucose levels are essential components. It’s important to recognize that adopting a holistic approach can make a significant difference.
Utilizing community resources, understanding how hormones affect your body, and engaging in patient education can empower you to take control of your health.
Many patients find that these supportive strategies not only improve their health outcomes but also enhance their confidence in managing their condition. Imagine feeling more in tune with your body and having the knowledge to make informed choices. This journey is about more than just numbers; it’s about your well-being and quality of life.
As you explore these strategies, remember that you’re not alone. Connecting with others who share similar experiences can provide encouragement and motivation. Consider embarking on the 30-Day Diabetes Reset program, where you can find additional resources and support tailored to your needs. Together, we can navigate this path toward healthier living.
Introduction
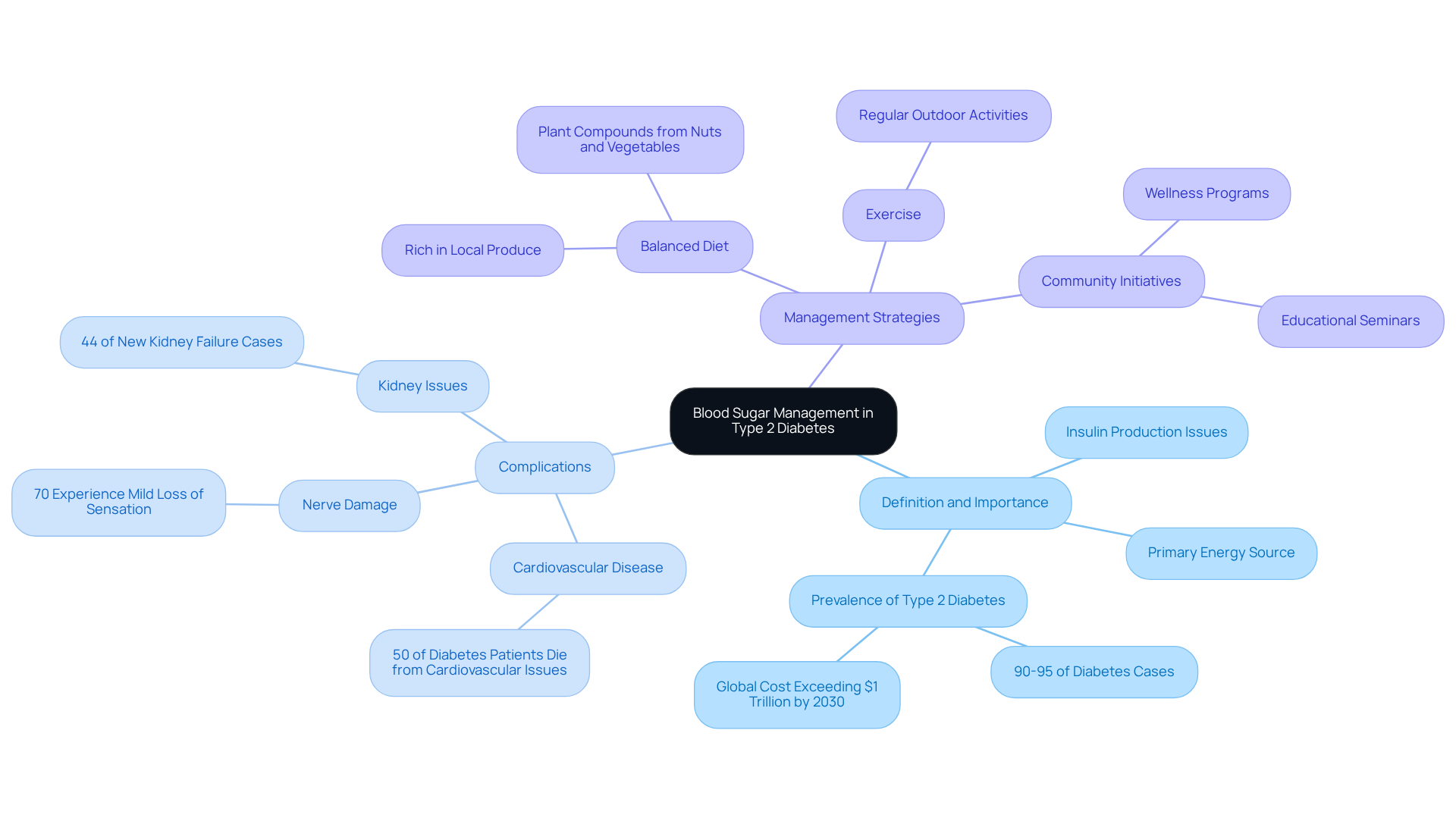
Understanding blood sugar management is crucial for the millions affected by type 2 diabetes, a condition that impacts nearly 90 to 95% of diagnosed cases. Many individuals find themselves overwhelmed by the complexities of controlling their glucose levels. This article delves into essential strategies that empower you to take control, highlighting the significance of:
- Dietary choices
- Effective monitoring techniques
- The vital role of patient education
It’s important to recognize that with so many conflicting methods and overwhelming information available, navigating this journey can feel daunting. How can you reclaim your health amidst the noise? Together, we will explore practical steps to simplify your path toward better health.
Define Blood Sugar and Its Importance in Type 2 Diabetes Management
Glucose, often referred to as plasma glucose, is the main carbohydrate circulating in your body, serving as the primary energy source for your cells. For those facing type 2 conditions, the body may struggle to produce enough insulin or use it effectively, leading to high blood sugar for diabetes type 2. This issue affects around 90 to 95% of all diagnosed cases of sugar-related illnesses in adults, highlighting its significance and prevalence. It’s crucial to maintain blood sugar for diabetes type 2 within a target range to prevent serious complications, such as:
- Cardiovascular disease
- Nerve damage
- Kidney issues
Alarmingly, this condition accounts for 44% of new kidney failure cases, underscoring the urgent need for effective management strategies.
In San Marcos, CA, individuals can effectively control their glucose levels through a holistic approach. This includes:
- Embracing a balanced diet rich in local produce
- Engaging in regular outdoor exercise
- Participating in community wellness initiatives
These programs provide invaluable support and resources aimed at managing blood sugar for diabetes type 2, ultimately enhancing quality of life and reducing the risk of related complications. Research indicates that those who actively regulate their glucose levels experience fewer health issues and improved overall well-being. For instance, patients utilizing continuous glucose monitoring systems often report better management of their condition, leading to fewer hospitalizations and emergency visits.
The importance of glucose regulation becomes evident when considering that nearly 50% of individuals with the illness are unaware of their status, which can lead to serious health consequences. By adopting proactive strategies—like consistent monitoring and lifestyle changes, similar to those recommended by Dr. Jason Shumard—patients can take charge of their blood sugar for diabetes type 2 and mitigate the risks associated with the condition. This holistic approach not only addresses symptoms but also targets the underlying causes of the condition, empowering individuals to reclaim their health and enhance their quality of life.
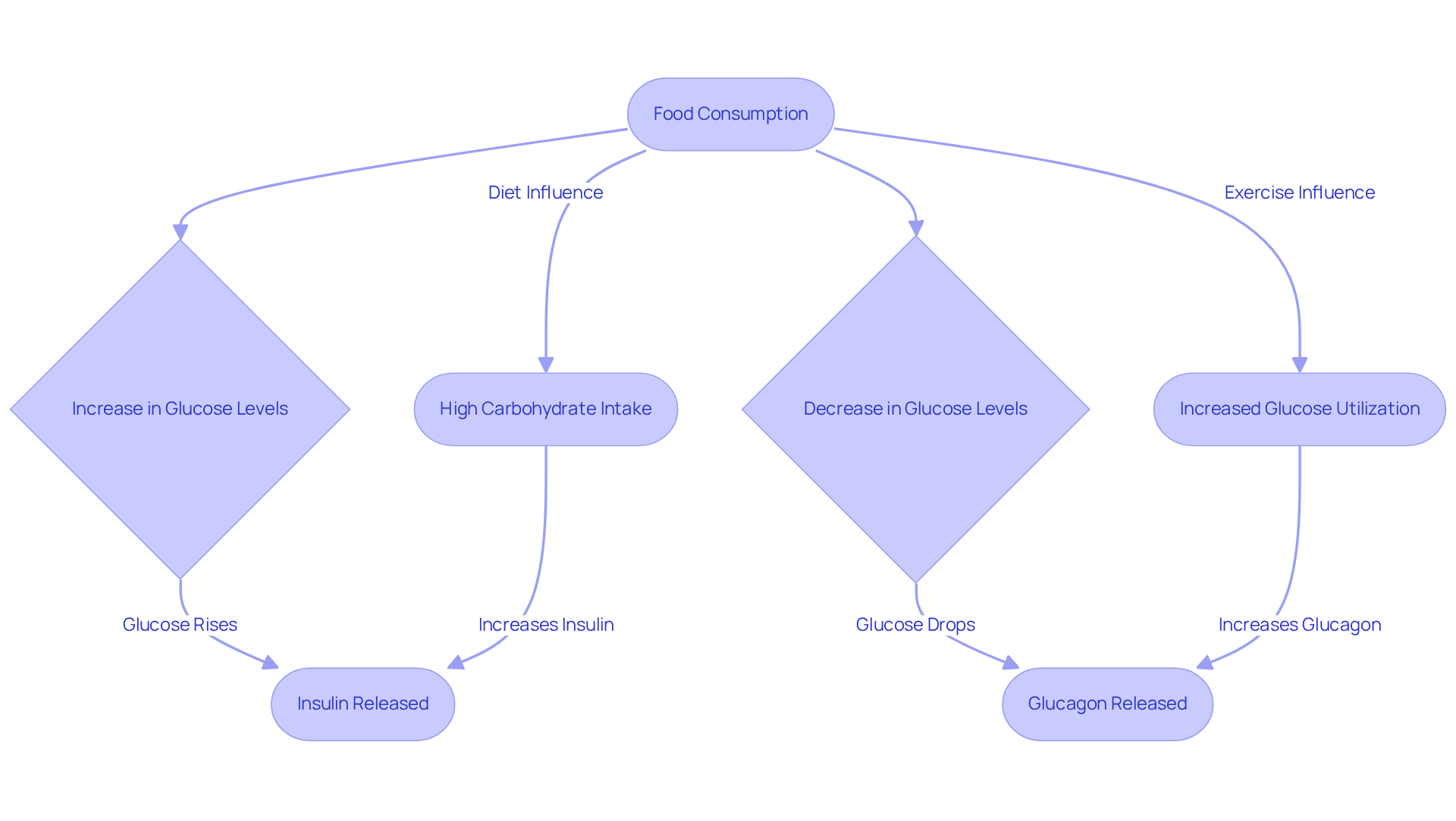
Explain How Blood Sugar Levels Are Regulated in the Body
Managing blood sugar for diabetes type 2 levels can feel overwhelming, but understanding how your body works is a vital first step. Blood glucose concentrations are primarily controlled by hormones from the pancreas, especially insulin and glucagon. When you consume food, and your glucose levels rise, insulin is released to help your cells absorb glucose for energy or storage. Conversely, when glucose levels drop, glucagon steps in, signaling the liver to release stored glucose back into your bloodstream. This delicate balance is essential for maintaining homeostasis and your overall well-being.
It’s important to recognize that several factors can significantly influence these hormonal responses. For instance, your dietary choices play a crucial role. Research indicates that many individuals managing their blood sugar for diabetes type 2 derive 75% to 90% of their daily calories from carbohydrates. This can lead to postprandial hyperglycemia, which is a condition where blood sugar for diabetes type 2 exceeds 180 mg/dl two hours after a meal. Physical activity is another key player; it enhances your body’s ability to use glucose effectively. In San Marcos, CA, you have beautiful parks at your fingertips. Consider hiking at Lake San Marcos or walking the trails at Discovery Lake to incorporate regular exercise into your routine. Additionally, stress can elevate blood sugar levels by triggering hormones that counteract insulin’s effects, making it even more important to find ways to manage stress.
Many patients find that understanding these dynamics is crucial for managing their condition and maintaining healthy blood sugar for diabetes type 2. Did you know that over 100 million Americans live with prediabetes or related conditions? This highlights the importance of effective management strategies. Lifestyle modifications, such as adopting a balanced diet rich in fiber and engaging in consistent physical activity, can positively influence your insulin and glucagon responses, resulting in better management of blood sugar for diabetes type 2. Local farmers’ markets in San Marcos offer fresh produce like avocados and berries, which are excellent choices for a diabetes-friendly diet. By recognizing how your choices impact hormonal balance and utilizing nearby resources, you can take proactive steps toward effectively managing your condition. Remember, you are not alone on this journey, and small changes can lead to significant improvements.
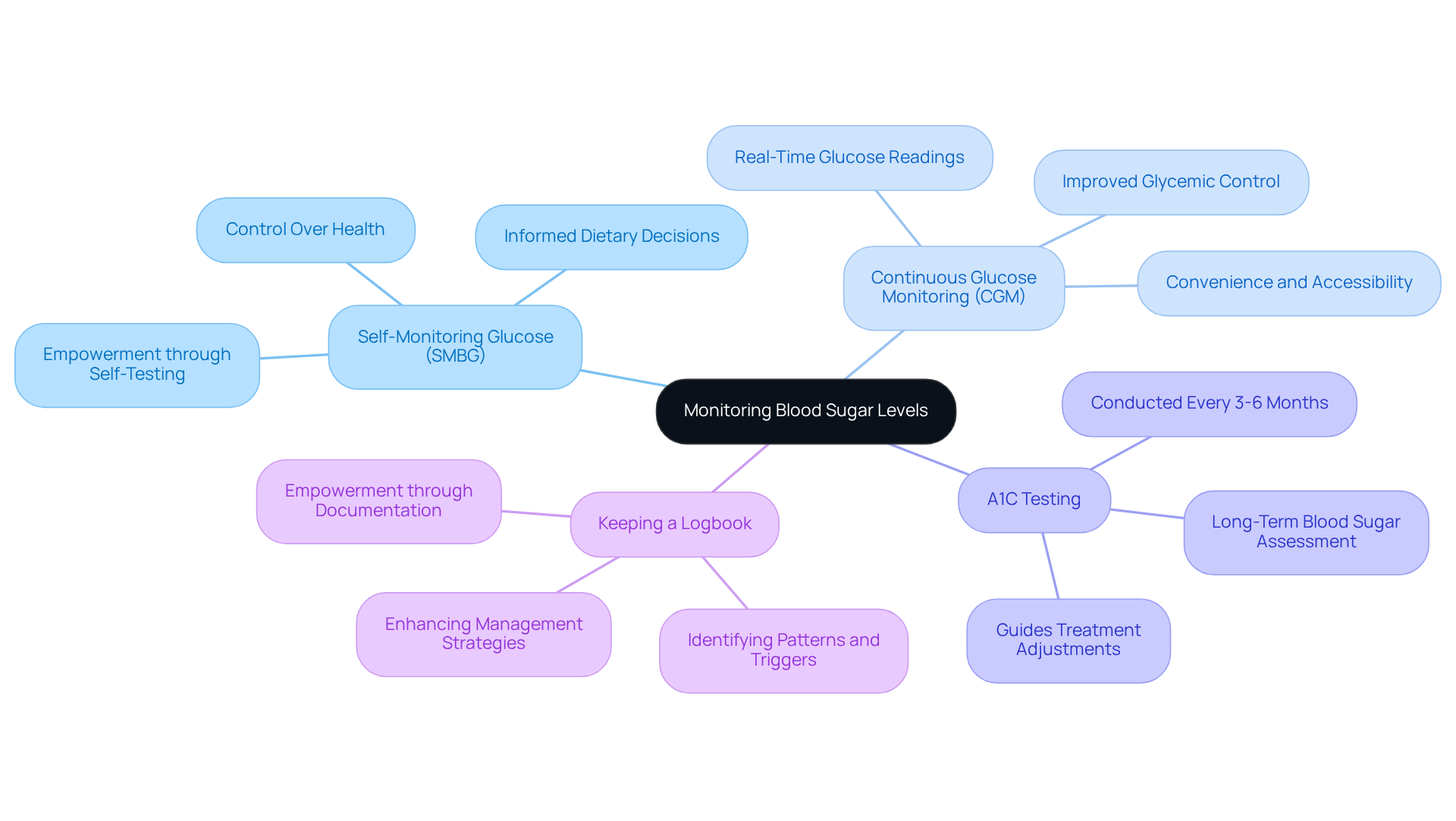
Outline Effective Methods for Monitoring Blood Sugar Levels
Managing type 2 diabetes can be challenging, but effective monitoring of blood sugar for diabetes type 2 levels is crucial for maintaining your health. There are several methods you can consider to help you on this journey:
- Self-Monitoring Glucose (SMBG): Have you ever thought about how empowering it is to check your own glucose levels? Using a glucose meter, you can monitor your readings at home, typically before meals and at bedtime. This method allows you to track fluctuations in blood sugar for diabetes type 2 and make informed decisions about your diet and medication, putting you in control.
- Continuous Glucose Monitoring (CGM): Many patients find that CGM devices offer real-time glucose readings and trends, making it easier to manage your glucose levels dynamically. Research shows that CGM can lead to a modest decrease in HbA1c values by about 0.32%, indicating improved glycemic control, which helps in managing blood sugar for diabetes type 2. As this technology becomes more popular, its convenience and effectiveness are helping more individuals take charge of their health.
- A1C Testing: It’s important to recognize that regular A1C testing, which assesses average blood sugar for diabetes type 2 levels over the past 2-3 months, plays a vital role in your diabetes management. Typically conducted every 3-6 months, this laboratory examination helps you understand your long-term control and informs any necessary adjustments to your treatment plan.
- Keeping a Logbook: Have you considered keeping a logbook? Documenting your blood sugar for diabetes type 2 readings, along with food intake and physical activity, can help you identify patterns and triggers. This practice not only enhances your management strategies but also empowers you to take control of your health journey.
Recent advancements in CGM technology, like the Abbott FreeStyle Libre 3, now provide minute-by-minute glucose readings and alerts for high and low levels. This innovation enhances the user experience and encourages more people to adopt these tools. Furthermore, with around 37.3 million individuals affected by diabetes in the U.S., efficient monitoring techniques are more important than ever.
Integrating these strategies into your daily routine can significantly enhance the management of blood sugar for diabetes type 2. Remember, every small step can lead to improved health outcomes and a better quality of life. You are not alone in this journey, and there are resources and support available to help you thrive.
Discuss Dietary Guidelines and Lifestyle Changes for Blood Sugar Control
Managing blood sugar for diabetes type 2 levels can feel overwhelming at times, but there are practical dietary guidelines and lifestyle changes that can make a significant difference in your journey toward better health. Here are some compassionate suggestions to consider:
-
Balanced Meals: Aim for meals that combine carbohydrates, proteins, and healthy fats. This balance can help stabilize your glucose levels, preventing those frustrating spikes and crashes. Remember, personalized nutrition plans are essential, as they cater to your unique needs, enhancing the effectiveness of these strategies.
-
Carbohydrate Counting: Understanding the carbohydrate content in your meals is crucial for effective meal planning. Have you ever noticed how certain foods can cause your glucose levels to rise? Research shows that mastering carbohydrate counting can lead to improved glycemic control and better management of blood sugar for diabetes type 2. This method is often complemented by functional medicine approaches that consider your lifestyle and eating habits as a whole.
-
Boost Fiber Consumption: Incorporating fiber-rich foods like whole grains, fruits, and vegetables can be a game changer. These foods slow down glucose absorption, which results in better regulation of blood sugar for diabetes type 2. Studies indicate that increasing your fiber intake can significantly lower HbA1c values, with many participants achieving readings under 7% when following a high-fiber diet.
-
Consistent Physical Activity: Regular exercise can enhance your insulin responsiveness and help lower glucose levels. Have you thought about starting a walking program? It’s a gentle way to increase your activity levels gradually, while also making it enjoyable and accountable. This step-by-step approach aligns beautifully with your journey toward better health.
-
Stay Hydrated: Never underestimate the power of hydration. Drinking plenty of water is vital for supporting your metabolism and blood sugar regulation. It’s easy to overlook, but staying hydrated plays an essential role in your overall health. Functional medicine emphasizes the importance of hydration in effectively managing blood sugar for diabetes type 2.
-
Consider Targeted Supplements: If you’re open to it, incorporating specific supplements under the guidance of a healthcare provider can support your metabolic health. These may include nutrients that enhance insulin sensitivity and overall wellness.
-
Stress Management Techniques: Have you considered how stress affects your glucose levels? Techniques like mindfulness or yoga can be incredibly beneficial. Managing stress is crucial, as it can significantly impact your blood sugar control.
By embracing these strategies, you can take proactive steps toward managing blood sugar for diabetes type 2 and improving your overall well-being. Remember, you are not alone on this journey, and with the principles of integrative functional medicine, you can find the support you need to thrive.
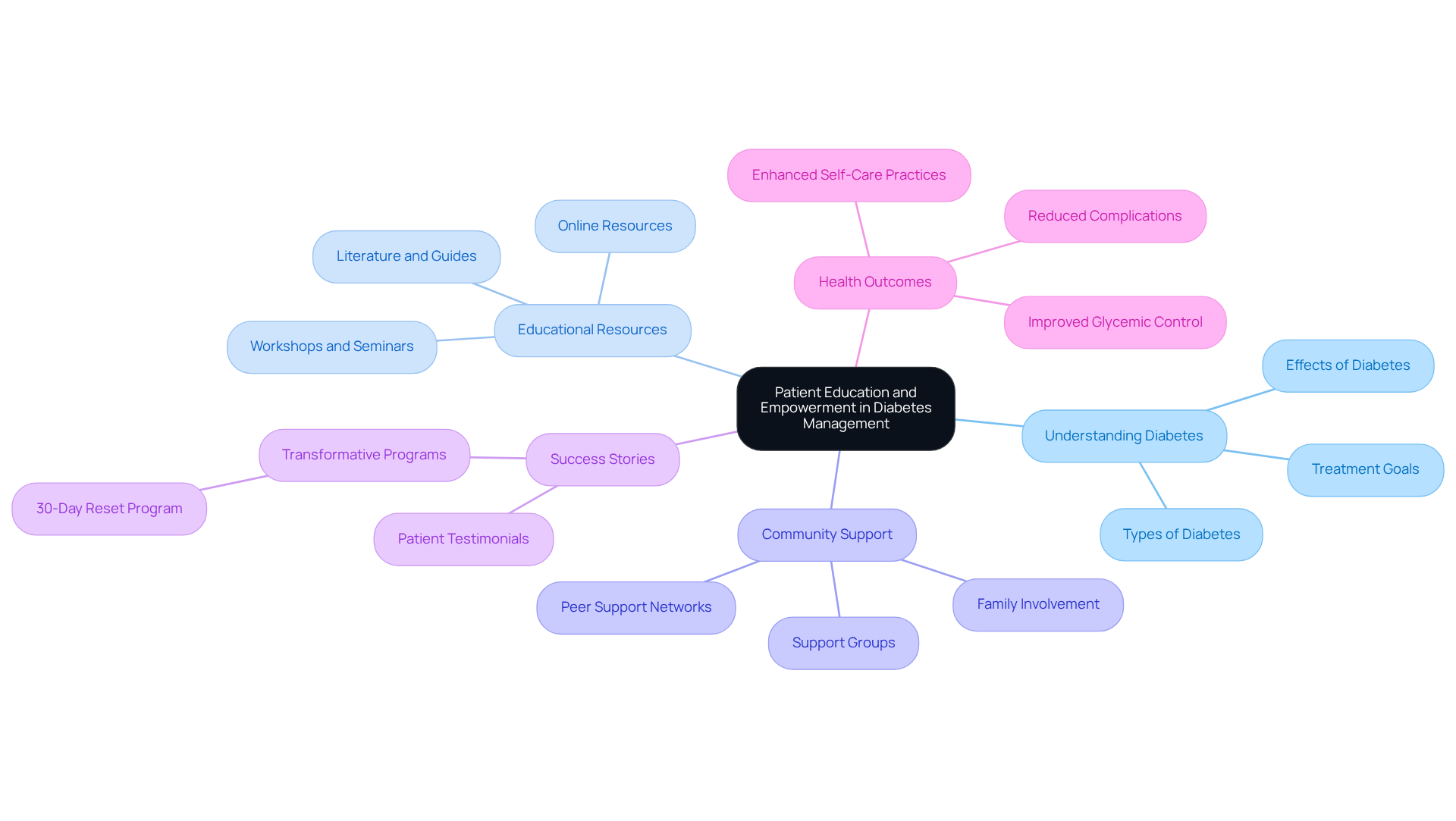
Highlight the Role of Patient Education and Empowerment in Diabetes Management
Managing blood sugar for diabetes type 2 can be a challenging journey, but patient education and empowerment are essential in navigating this path. By truly understanding their condition, individuals can make informed choices about their diet, exercise, medication, and how to manage their blood sugar for diabetes type 2. At Integrative Wellness Center, we believe in a holistic approach that goes beyond typical lab work. We offer comprehensive testing and personalized plans tailored to each individual’s unique needs.
It’s important to recognize that educational resources, such as workshops, seminars, and literature, provide valuable insights into effective self-management strategies, particularly for controlling blood sugar for diabetes type 2. These resources empower patients to take charge of their health and well-being by effectively managing blood sugar for diabetes type 2. Many patients find that fostering a supportive community allows them to share experiences and challenges, enhancing motivation and accountability.
Our patients have achieved transformative results through Dr. Jason Shumard’s 30-Day Reset program. This program empowers individuals to conquer their condition through lifestyle changes and education. For instance, one patient shared, ‘I never thought I could manage my diabetes without medication, but this program changed my life.’ Such stories illustrate the power of empowerment and education.
Empowered patients are not only more likely to adhere to treatment plans but also actively monitor their health, including their blood sugar for diabetes type 2. By taking these proactive steps, they can ultimately achieve better health outcomes, including improved blood sugar for diabetes type 2. If you’re ready to take control of your diabetes journey, consider joining our 30-Day Reset program and discover the possibilities for a healthier future.
Conclusion
Understanding and managing blood sugar levels is vital for individuals navigating the challenges of type 2 diabetes. This article has explored essential strategies that empower you to take control of your health. By emphasizing dietary choices, effective monitoring techniques, and the critical role of patient education, we aim to support your journey. Integrating these elements into your daily life can significantly enhance your management of blood sugar levels and overall well-being.
Key insights discussed include:
- The necessity of a balanced diet rich in fiber
- The benefits of regular physical activity
- The importance of self-monitoring glucose levels
Many patients find that fostering a supportive community through patient education leads to better health outcomes. With the right tools and knowledge, you can navigate your diabetes journey more effectively and confidently.
It’s important to recognize that embracing a proactive approach to managing blood sugar for diabetes type 2 is not only possible but essential. By implementing the strategies outlined, you can enhance your quality of life, reduce the risk of complications, and ultimately reclaim your health. Stay informed about the latest research and advancements in diabetes management, as this knowledge empowers you to make informed choices on your journey.
Frequently Asked Questions
What is blood sugar and why is it important in managing type 2 diabetes?
Blood sugar, or plasma glucose, is the main carbohydrate in the body and serves as the primary energy source for cells. In type 2 diabetes, the body may not produce enough insulin or use it effectively, leading to high blood sugar levels. Maintaining blood sugar within a target range is crucial to prevent serious complications, including cardiovascular disease, nerve damage, and kidney issues.
What complications can arise from poorly managed blood sugar in type 2 diabetes?
Poorly managed blood sugar can lead to serious complications such as cardiovascular disease, nerve damage, and kidney issues, with type 2 diabetes accounting for 44% of new kidney failure cases.
How can individuals in San Marcos, CA, manage their blood sugar levels effectively?
Individuals in San Marcos can manage their blood sugar levels through a holistic approach that includes a balanced diet rich in local produce, regular outdoor exercise, and participation in community wellness initiatives.
What role does continuous glucose monitoring play in managing diabetes?
Continuous glucose monitoring systems help patients better manage their condition, leading to fewer hospitalizations and emergency visits by providing real-time data on glucose levels.
How are blood sugar levels regulated in the body?
Blood sugar levels are primarily controlled by hormones from the pancreas, especially insulin and glucagon. Insulin helps cells absorb glucose when levels rise after eating, while glucagon signals the liver to release stored glucose when levels drop.
What factors can influence blood sugar regulation?
Dietary choices significantly influence blood sugar regulation, as many individuals derive 75% to 90% of their daily calories from carbohydrates, which can lead to postprandial hyperglycemia. Physical activity enhances the body’s ability to use glucose effectively, and stress can elevate blood sugar levels by triggering hormones that counteract insulin’s effects.
What lifestyle changes can help manage blood sugar levels?
Lifestyle changes such as adopting a balanced diet rich in fiber, engaging in consistent physical activity, and managing stress can positively influence insulin and glucagon responses, leading to better blood sugar management.
Why is it important to monitor blood sugar levels regularly?
Regular monitoring of blood sugar levels is important because nearly 50% of individuals with type 2 diabetes are unaware of their condition, which can lead to serious health consequences. Proactive strategies can help manage blood sugar effectively and mitigate risks associated with the condition.