Introduction
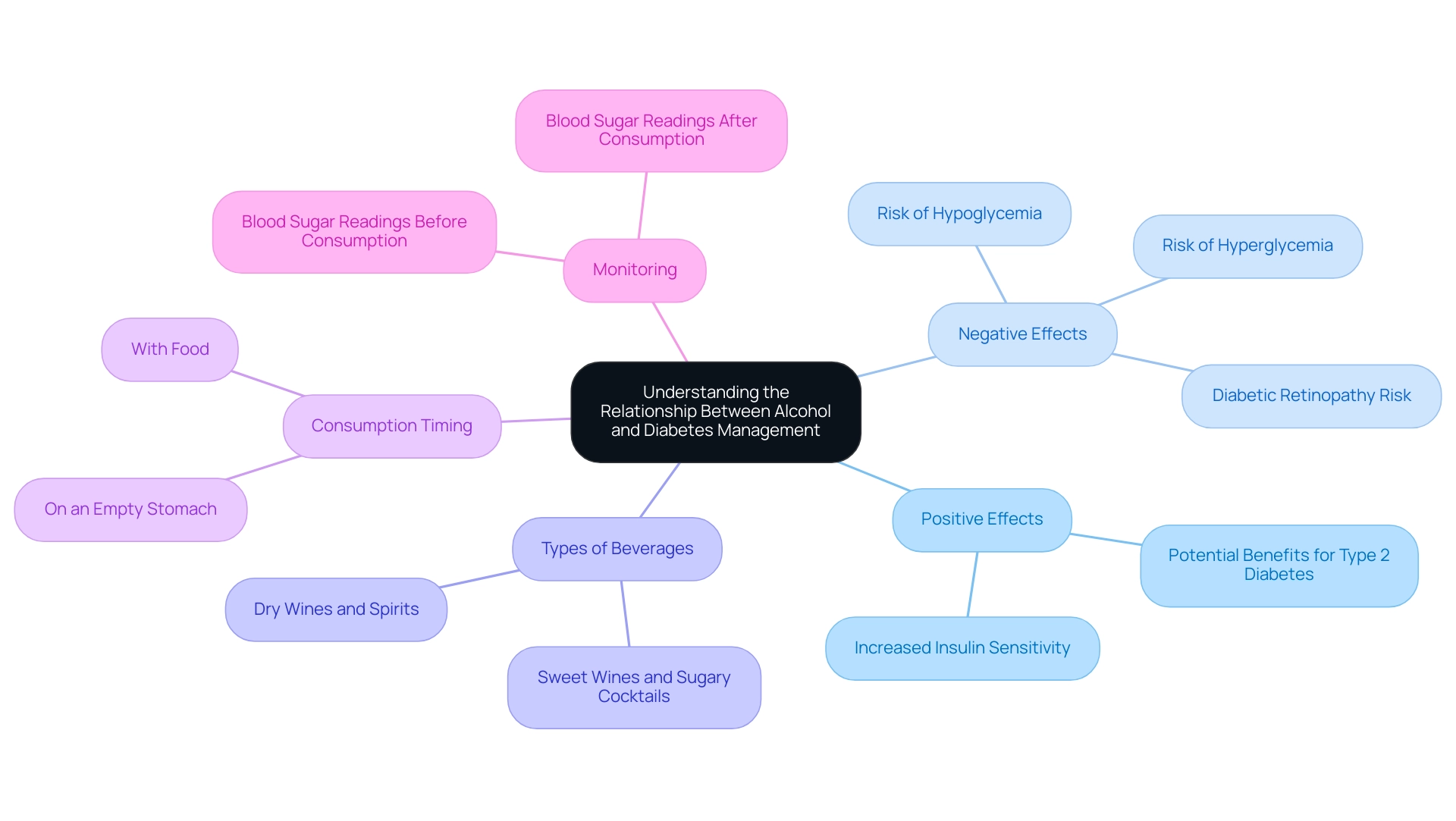
Navigating the complexities of alcohol consumption can be particularly challenging for individuals managing diabetes. The relationship between alcohol and diabetes is multifaceted, presenting both potential benefits and significant risks. While moderate alcohol intake may enhance insulin sensitivity, excessive consumption can lead to harmful fluctuations in blood sugar levels and increase the risk of serious complications.
Understanding the nuances of how different types of alcoholic beverages affect glucose levels and the importance of accompanying food intake is essential for effective diabetes management.
This article delves into the intricate dynamics of alcohol and diabetes, offering practical strategies and insights to empower individuals in making informed choices about their alcohol consumption while prioritizing their health.
Understanding the Relationship Between Alcohol and Diabetes
Alcohol intake reveals a complex relationship with blood sugar management, showing both positive and negative effects. Moderate intake of alcohol good for diabetes has been associated with increased insulin sensitivity, which could be advantageous for individuals managing type 2 diabetes. However, excessive beverage intake raises significant concerns, as it can lead to fluctuations in blood sugar values, including hypoglycemia and hyperglycemia.
Notably, the substance has been identified as a risk factor for diabetic retinopathy, underscoring the potential dangers associated with its consumption (British Medical Journal, 1984;288:1035–1037). A holistic approach to managing this condition necessitates understanding the type of alcoholic beverage consumed; for instance, sweet wines and sugary cocktails are more likely to elevate blood sugar levels compared to drier options like dry wines or spirits. Furthermore, consuming beverages on an empty stomach significantly increases the risk of hypoglycemia, emphasizing the need for careful monitoring.
This careful approach can help alleviate some of the anxiety that accompanies the worry surrounding potential complications of the condition, particularly in relation to whether alcohol is good for diabetes. A randomized parallel study (Zheng 2012) involving 45 healthy participants demonstrated the impact of beverage consumption on insulin sensitivity and glucose levels, further illustrating the nuanced effects of such beverages on managing blood sugar. As pointed out by Dolly O Baliunas, ‘Because former drinkers may be motivated to refrain due to health concerns, they may actually be at increased risk of developing a certain condition, known as the sick-quitter effect.’
This underscores the significance of comprehending the dynamics of beverage consumption within a comprehensive framework of managing blood sugar. Recent evidence indicates that there may be publication bias in research on beverage intake, with smaller studies demonstrating a significant rise in insulin sensitivity due to beverage intake potentially being neglected. For individuals with type 2, it is advisable to consistently monitor blood sugar readings before and after consuming alcohol to gain insights into their unique responses, facilitating more informed choices regarding alcohol intake.
By reassessing the origin of the illness and addressing health at the fundamental aspect, patients can empower themselves to manage their condition more effectively and lessen anxiety.
Best Practices for Drinking Alcohol with Diabetes
- Choose Lower-Carbohydrate Options: When selecting alcoholic beverages, prioritize lower-carbohydrate choices such as spirits mixed with soda water or dry wines, as these types of alcohol good for diabetes can be beneficial. It is essential to avoid sugary cocktails and sweet wines, as these can lead to significant spikes in blood sugar, complicating diabetes management, and to consider if alcohol good for diabetes.
- Eat Before Drinking: Consuming a well-balanced meal before or while drinking can play a crucial role in stabilizing blood sugar, as understanding whether alcohol is good for diabetes is important. A meal that includes a mix of carbohydrates, proteins, and healthy fats is recommended to mitigate the potential impact of beverages on glucose levels.
- Stay Hydrated: Incorporating water between alcoholic drinks is vital to prevent dehydration, which can adversely affect blood sugar regulation, making it important to understand if alcohol is good for diabetes. Staying hydrated not only supports overall health but also aids in maintaining stable glucose levels during beverage consumption, particularly when considering if alcohol is good for diabetes.
- Limit Beverage Intake: Moderation is essential in drinking, as it raises the question of whether alcohol is good for diabetes. It is advisable for women to limit their intake to one drink per day and for men to restrict it to two drinks, especially considering how alcohol is good for diabetes. This method reduces the dangers linked to excessive drinking, suggesting that moderate alcohol consumption may be alcohol good for diabetes and help avoid various health problems. Significantly, studies indicate that the typical CRP concentration for individuals with no beverage consumption was 0.64 g/mL, emphasizing the possible health consequences of intake.
- Monitor Blood Sugar Levels: Regularly checking blood sugar levels before, during, and after drinking is crucial for understanding how beverages, including if alcohol is good for diabetes, affect individual glucose responses. This practice allows individuals to make informed adjustments to their food intake or medication as needed, while also considering if alcohol is good for diabetes, thereby improving management of the condition.
- Plan for Hypoglycemia: It is prudent to always have fast-acting carbohydrates, such as glucose tablets or juice, readily available in case of unexpected low blood sugar episodes, particularly when evaluating whether alcohol is good for diabetes. Being prepared can prevent potential emergencies and ensure safety while enjoying alcohol that is good for diabetes.
- Consult Your Healthcare Provider: Before making any substantial changes to beverage intake, it is highly advised to consult with a healthcare provider. This guarantees that any new drinking habits are in accordance with a person’s overall health management plan, taking into account the latest guidelines for individuals with blood sugar issues concerning beverage consumption. As noted by healthcare experts,
However, more intervention studies with a longer intervention period are necessary to confirm the results,
indicating the need for tailored advice based on personal health profiles. Additionally, discussing moderate drinking with your doctor can provide personalized guidance, ensuring safe practices.
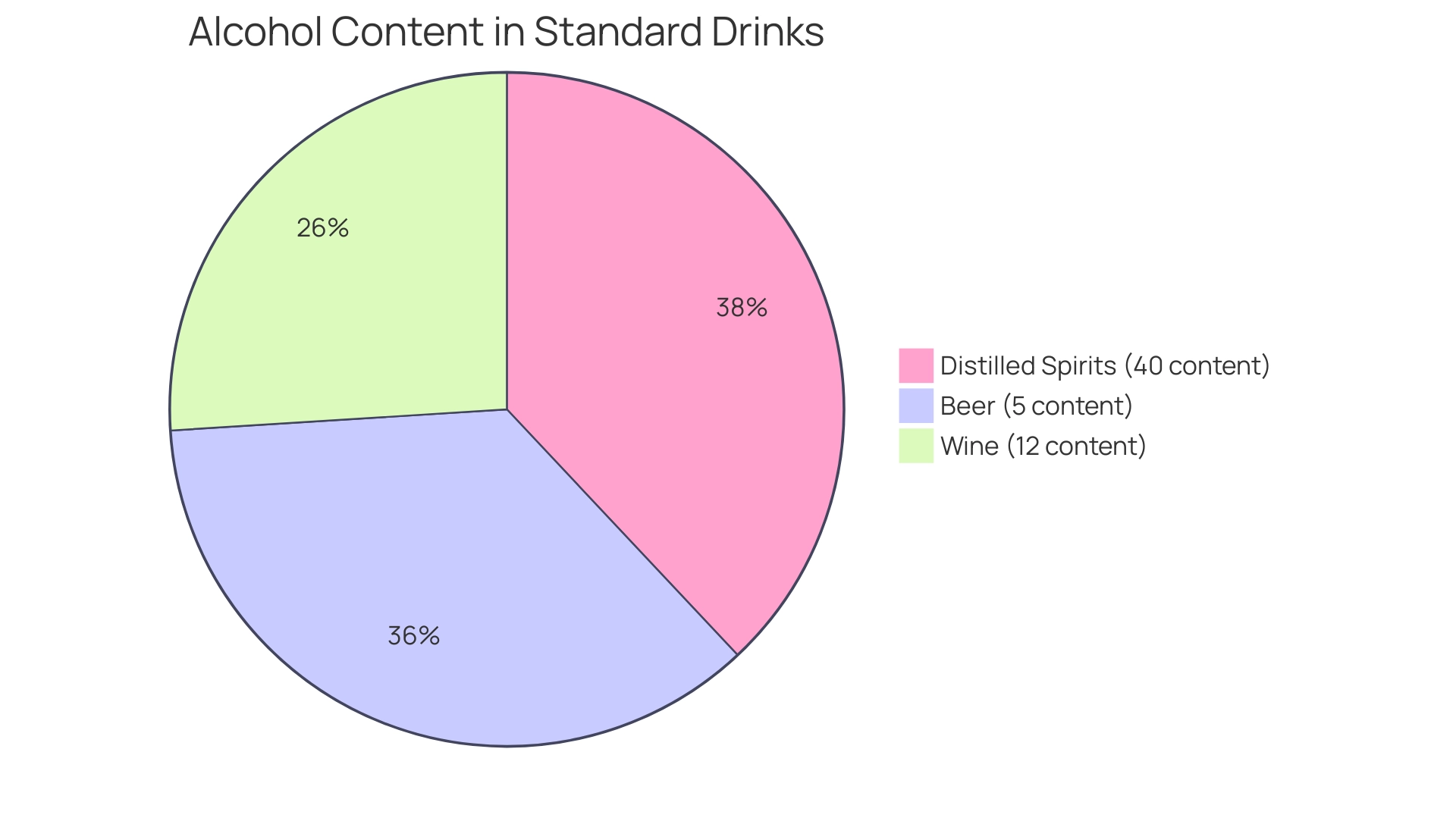
Knowing Your Alcohol Content
Understanding the content of drinks is essential for individuals managing diabetes, especially in determining if alcohol is good for diabetes, as it varies significantly. A standard drink is defined as containing approximately 14 grams of pure ethanol, serving as a benchmark for monitoring consumption. This measurement is typically represented by the following examples:
- 12 ounces of beer (5% content)
- 5 ounces of wine (12% content)
- 1.5 ounces of distilled spirits (40% content)
Knowledge of these measurements allows people with blood sugar issues to effectively monitor their beverage consumption, including whether alcohol is good for diabetes. This knowledge is vital in understanding how alcohol good for diabetes can help mitigate the risks associated with excessive intake, which can cause alarming fluctuations in blood sugar levels. According to the National Health Interview Survey (NHIS), comprehending patterns of beverage consumption in the U.S. population is crucial for tackling health outcomes related to blood sugar issues.
As Peter Boersma, M.P.H., states, ‘Heavy drinking is defined as the average intake of more than 7 drinks per week for women and more than 14 drinks per week for men in the past year.’ This definition assists individuals in identifying the potential risks of excessive beverage intake and emphasizes the significance of moderation, particularly in evaluating whether alcohol is good for diabetes while effectively managing blood sugar levels. In addition to tracking alcohol intake, it is important to recognize that alcohol can be good for diabetes, while also maintaining hydration as a key factor in managing blood sugar levels.
In San Marcos, residents can select from a range of local drink choices that can assist hydration without affecting blood sugar. Opt for refreshing infused water with local fruits, herbal teas, or natural, no-sugar-added beverages available at local markets. These strategies not only promote hydration but also aid in overall health and energy regulation, helping to maintain blood sugar stability and enabling individuals to manage their condition more effectively.
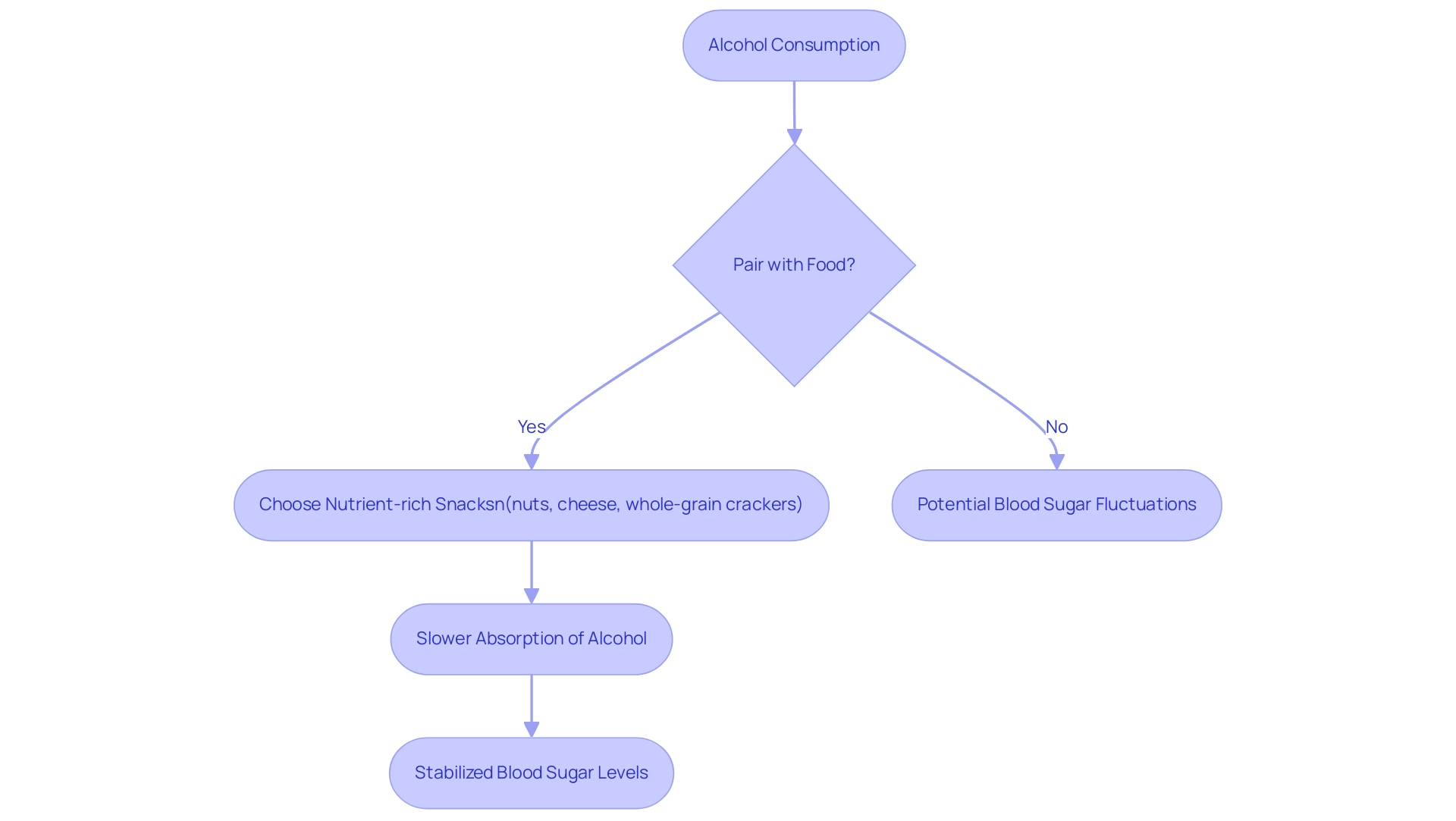
The Importance of Pairing Alcohol with Food
For individuals managing diabetes, pairing beverages with food emerges as a crucial strategy for mitigating potential blood sugar fluctuations. Eating while drinking can effectively slow the absorption of spirits, thereby promoting more stable blood sugar readings. A balanced meal incorporating fiber, protein, and healthy fats is essential, as these nutrients can counteract the effects of spirits.
For instance, pairing a moderate drink with snack options such as nuts, cheese, or whole-grain crackers not only enhances the drinking experience but also provides vital nutrients that help stabilize blood sugar levels. Recent studies, especially the results from the China Health and Nutrition Survey, which examined long-term drinking patterns and their link to the risk of type 2 sugar-related illness, emphasize the importance of dietary habits in drinking. This research uncovered important links between beverage intake patterns and the likelihood of developing type 2 metabolic disorder.
As mentioned by Dr. Robert H. Eckel, a leading authority in the field, grasping the connection between food and beverage absorption is crucial for effective management of blood sugar. Furthermore, it is important to recognize that stratified analyses did not find significant interactions between habitually consuming beverages with meals and various risk factors for incident type 2 diabetes, highlighting the complexity of this relationship. This approach not only encourages responsible drinking but also supports overall metabolic health, aligning with the principles emphasized by the American Heart Association’s Epidemiology and Prevention | Lifestyle Cardiometabolic Health.
Recognizing Symptoms of Hypoglycemia
The consumption of alcohol poses a significant risk of hypoglycemia, particularly when ingested without accompanying food. Symptoms of hypoglycemia can manifest as:
- Shakiness
- Sweating
- Confusion
- Irritability
- Faintness
It is imperative for individuals who experience any of these symptoms while drinking to respond swiftly.
Prompt intake of fast-acting carbohydrates, such as glucose tablets or fruit juice, can effectively raise blood sugar. According to recent observations, one participant in a related study recorded a plasma glucose level as low as 33 mg/dL at the 120-minute mark, emphasizing the severity of potential drops in blood sugar. The mean ± standard deviation for all measurements indicates variability in these responses, further underscoring the need for vigilance.
Understanding and instruction regarding identifying these symptoms are essential, as they allow individuals to create a proactive management strategy to avert serious complications during social situations involving beverage intake. As highlighted in recent discoveries, low blood sugar can rise after drinking; therefore, individuals with blood sugar issues should be especially cautious and consult their healthcare professionals about whether alcohol is good for diabetes and its interaction with medication.
In summary, we have demonstrated that in individuals with type 1 condition, evening intake of beverages can lead to a decrease in blood glucose the following morning and heightens the risk of hypoglycemia after breakfast.
Additionally, it is important to recognize that the study faced limitations, including a small sample size and lack of randomization, highlighting the need for more comprehensive research on the effects of substances on glucose fluctuations.
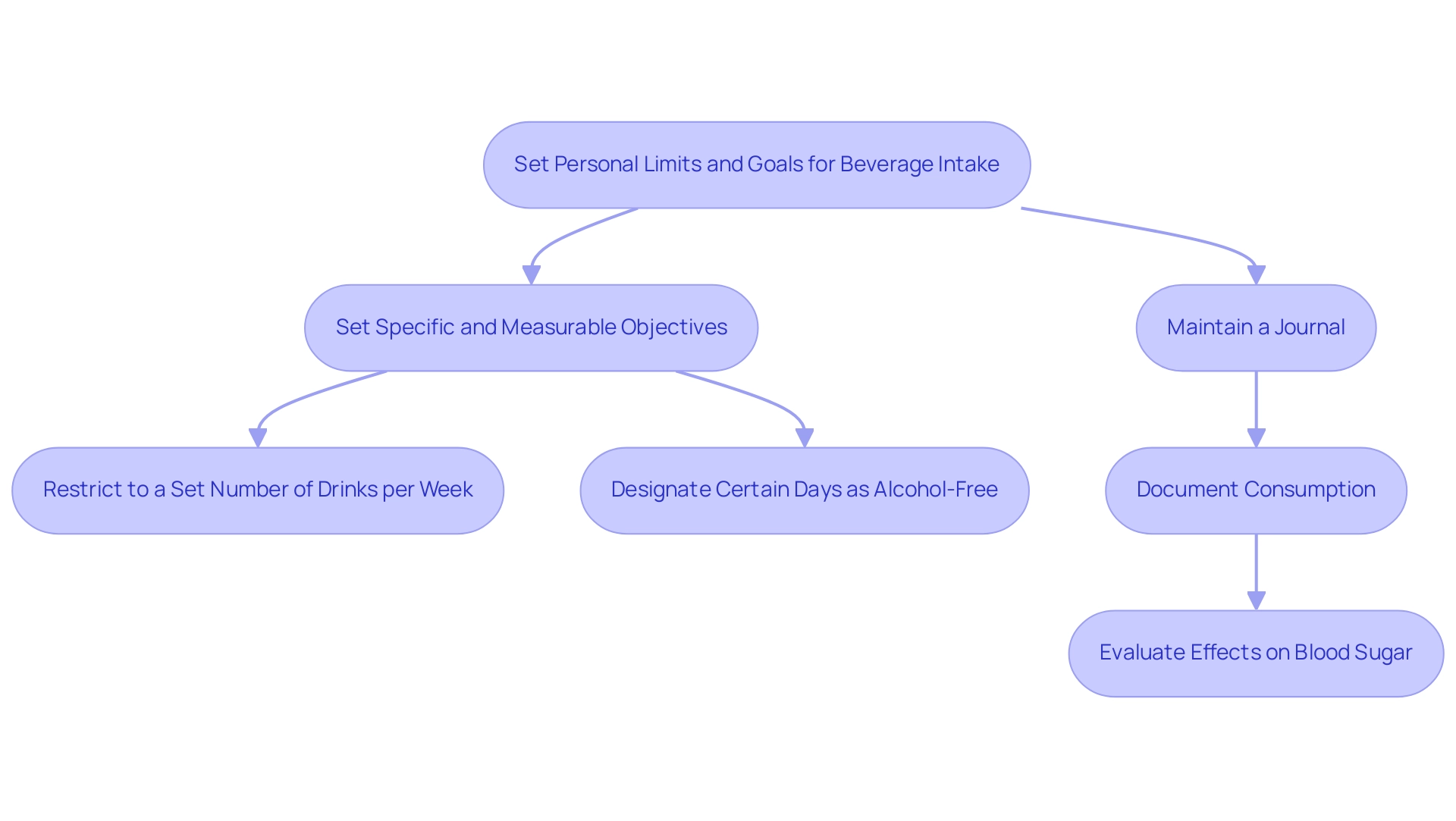
Setting Personal Limits and Goals
Setting personal limits and objectives for beverage intake is a crucial tactic in managing diabetes effectively. It is essential to evaluate how beverages influence personal blood glucose amounts and general well-being. Begin by setting specific and measurable objectives, such as:
- Restricting beverage intake to a predetermined number of drinks per week
- Designating certain days as free from consumption
For example, research has classified beverage intake from teetotaler to ≥210 g/week, suggesting that even moderate usage can affect glucose amounts. A notable case study is Wei (2000), which involved a U.S. study of men aged 30-79, tracking 8,633 participants. This research discovered that alcohol intake, measured in grams per week, had significant implications for blood sugar diagnoses, indicating that there may be cases where alcohol good for diabetes could be considered based on glucose levels or history.
Maintaining a detailed journal to document both consumption and its effects on blood sugar can significantly enhance self-awareness, reinforcing positive habits. This approach not only assists in navigating social situations but also aligns with personal health management plans. Dr. Ameena T. Ahmed underscores this point, mentioning that,
These findings underscore the significance of regular evaluation of beverage consumption in individuals with blood sugar issues, especially as half of adults with such conditions partake in drinks.
By setting clear goals for alcohol consumption and monitoring progress, individuals can create a sustainable framework for managing their health, particularly because some studies suggest that alcohol is good for diabetes, especially in light of the variability in diabetes diagnosis reported across studies.
Conclusion
Understanding the intricate relationship between alcohol and diabetes is essential for individuals looking to manage their health effectively. While moderate alcohol consumption may offer some benefits, such as improved insulin sensitivity, the risks associated with excessive intake cannot be overlooked. Fluctuations in blood sugar levels and the potential for serious complications highlight the need for careful consideration of both the type and quantity of alcohol consumed.
Implementing best practices, such as:
- Choosing lower-carbohydrate options
- Eating before drinking
- Staying hydrated
can significantly mitigate the risks. Monitoring blood sugar levels before, during, and after consumption provides valuable insights into personal responses to alcohol, empowering individuals to make informed decisions. Additionally, recognizing the symptoms of hypoglycemia and preparing accordingly can enhance safety during social situations.
Establishing personal limits and setting clear goals for alcohol consumption are vital steps in fostering a sustainable approach to diabetes management. By documenting consumption patterns and their effects on blood sugar, individuals can cultivate a greater awareness of their health. Ultimately, prioritizing informed choices and maintaining open communication with healthcare providers can lead to a balanced lifestyle that accommodates both social enjoyment and effective diabetes care.
Frequently Asked Questions
How does alcohol intake affect blood sugar management?
Alcohol intake has a complex relationship with blood sugar management, showing both positive and negative effects. Moderate alcohol consumption can increase insulin sensitivity, which may benefit individuals with type 2 diabetes. However, excessive intake can lead to fluctuations in blood sugar levels, resulting in hypoglycemia or hyperglycemia.
What are the risks associated with alcohol consumption for diabetics?
Alcohol is identified as a risk factor for diabetic retinopathy and can lead to significant blood sugar fluctuations. Sweet wines and sugary cocktails tend to elevate blood sugar levels more than drier options like dry wines or spirits. Additionally, drinking on an empty stomach increases the risk of hypoglycemia.
What should individuals with diabetes consider when choosing alcoholic beverages?
Individuals with diabetes should opt for lower-carbohydrate options, such as spirits mixed with soda water or dry wines, and avoid sugary cocktails and sweet wines. It is also important to monitor how different beverages affect blood sugar levels.
How can one stabilize blood sugar levels when consuming alcohol?
Consuming a well-balanced meal that includes carbohydrates, proteins, and healthy fats before or while drinking can help stabilize blood sugar levels. Staying hydrated by drinking water between alcoholic drinks is also crucial.
What is the recommended limit for alcohol intake for individuals with diabetes?
It is advisable for women to limit their alcohol intake to one drink per day and for men to two drinks per day to reduce the risks associated with excessive drinking.
Why is it important to monitor blood sugar levels when drinking alcohol?
Regularly checking blood sugar levels before, during, and after drinking helps individuals understand how alcohol affects their glucose responses. This practice enables them to make informed adjustments to their food intake or medication as needed.
What should individuals do in case of hypoglycemia while drinking?
It is prudent to have fast-acting carbohydrates, such as glucose tablets or juice, readily available to address unexpected low blood sugar episodes while consuming alcohol.
Should individuals with diabetes consult healthcare providers about alcohol consumption?
Yes, it is highly advised to consult with a healthcare provider before making changes to alcohol intake. This ensures that drinking habits align with overall health management plans and personal health profiles.