Overview
This article offers a compassionate overview of the American Diabetes Association Standards of Care 2025, recognizing the challenges faced by those living with diabetes. It emphasizes the importance of patient-centered and holistic approaches in diabetes management, acknowledging that each individual’s journey is unique and deserving of understanding. \n\nKey updates are highlighted, such as the integration of continuous glucose monitoring, which can empower patients to take charge of their health. The role of GLP-1 receptor agonists is also discussed, along with the necessity of education and lifestyle interventions. These elements are not just clinical updates; they represent vital tools that can help individuals manage their diabetes effectively and improve their health outcomes. \n\nIt’s important to recognize that managing diabetes can be overwhelming, but with the right support and resources, individuals can feel more in control. This article aims to provide guidance and encouragement, inviting readers to explore how these standards can positively impact their lives and inspire a healthier future.
Introduction
Navigating the complexities of diabetes management can be overwhelming, and it’s crucial to recognize the emotional toll it can take. As the American Diabetes Association (ADA) unveils its 2025 Standards of Care, there is a transformative opportunity to reshape how diabetes is diagnosed, treated, and managed. These guidelines emphasize the importance of personalized care, integrating innovative strategies, technology, and lifestyle modifications to better support individuals on their journey.
Have you ever felt lost in the sea of information about diabetes? You’re not alone. The role of continuous glucose monitoring and the significance of holistic care, which includes mental health and education, are now highlighted in these new standards. They provide a roadmap for empowering patients, acknowledging that each person’s experience with diabetes is unique.
As the prevalence of diabetes continues to rise, the need for proactive interventions and tailored treatment plans becomes increasingly critical. This article delves into the key updates from the ADA, exploring how these advancements can enhance the quality of life for individuals living with diabetes. Together, we can pave the way for better health outcomes and a brighter future.
Overview of the 2025 ADA Standards of Care in Diabetes
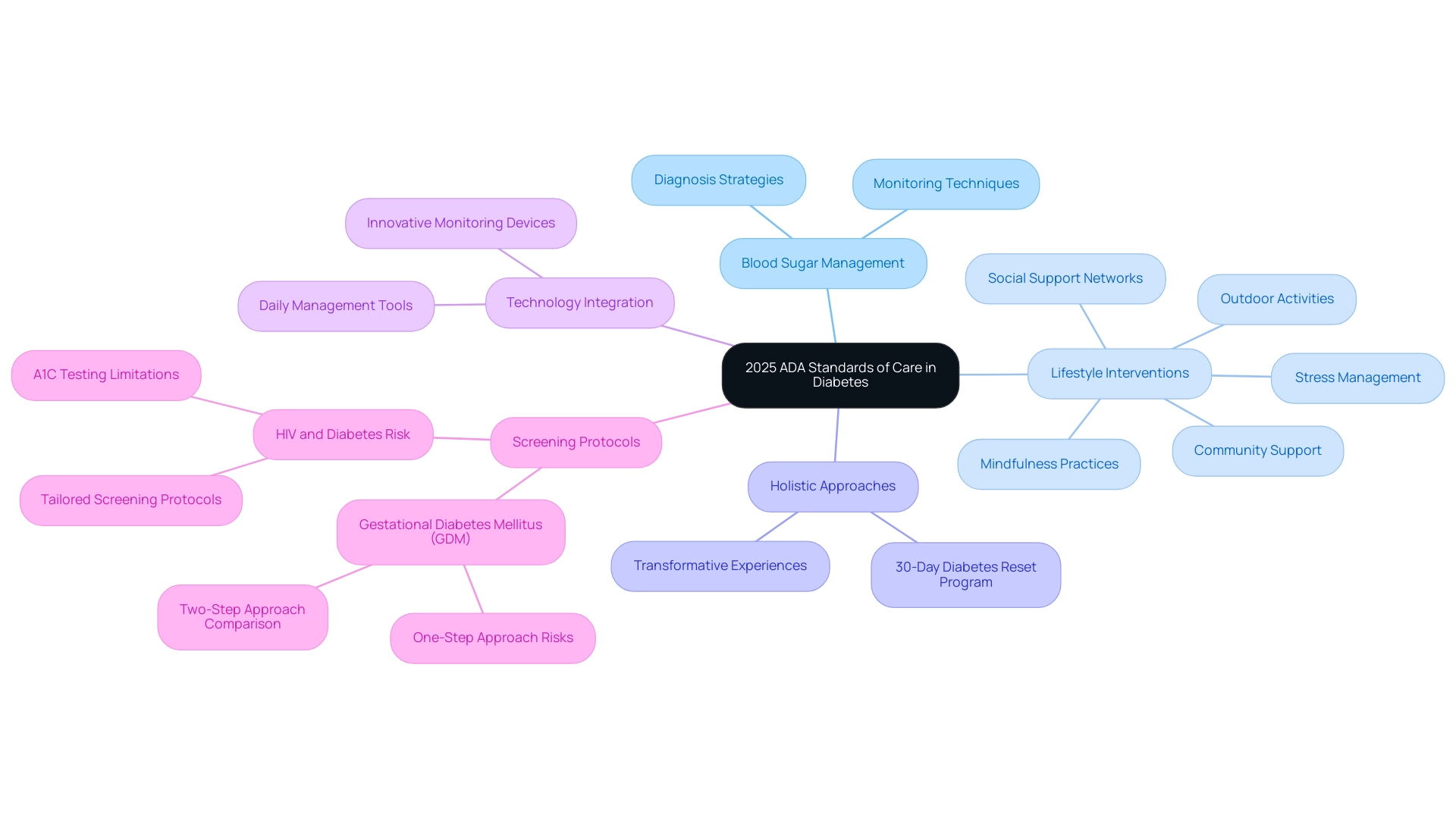
The American Diabetes Association Standards of Care 2025 for blood sugar regulation reflect a significant advancement in management, focusing on both clinical practice and patient-centered care. It’s important to acknowledge the challenges faced by individuals living with diabetes. Among the key updates are improved strategies for diagnosing the condition and innovative methods aimed at preventing or delaying the onset of type 2 diabetes. Notably, intensive lifestyle interventions, such as engaging in outdoor activities and fostering community support, are recognized as vital for preventing macrovascular disease in early adulthood, aligning with the ADA’s guidelines for comprehensive care.
Many patients find that holistic approaches can be transformative. Dr. Jason Shumard’s 30-Day Diabetes Reset Program empowers individuals to manage and even reverse type 2 diabetes through essential lifestyle changes that extend beyond nutrition and exercise. These changes also include:
- Stress management techniques
- The integration of mindfulness practices
- The importance of social support networks
These are part of the four lesser-known power-plays that can significantly enhance well-being. Furthermore, the incorporation of cutting-edge technology into daily management practices enhances the potential for better health outcomes.
As Charles Henderson, the ADA’s chief executive officer, articulates,
Enhancing the lives of individuals impacted by this condition is a key part of the ADA’s mission.
This commitment highlights the necessity for comprehensive, individualized care that reflects the latest scientific evidence. It’s crucial to understand that recent findings show individuals diagnosed with gestational diabetes mellitus (GDM) through the one-step approach face a 3.4-fold higher risk of developing prediabetes and type 2 diabetes. This raises concerns about the increased incidence of GDM cases compared to the two-step approach.
The case study titled ‘People With HIV and Diabetes Risk‘ underscores the need for tailored screening protocols for prediabetes and glucose intolerance in populations at higher risk. Timely intervention and adherence to these updated guidelines are essential. Through patient-centered care and transformative experiences reported by individuals like Ed, who shared, ‘I lost 55 lbs and my A1C started at 9.1 and is now 5.7,’ the American Diabetes Association Standards of Care 2025 aim to empower individuals. We want to ensure you have the trusted support needed to manage your condition effectively and thrive.
The Role of Continuous Glucose Monitoring in Diabetes Management
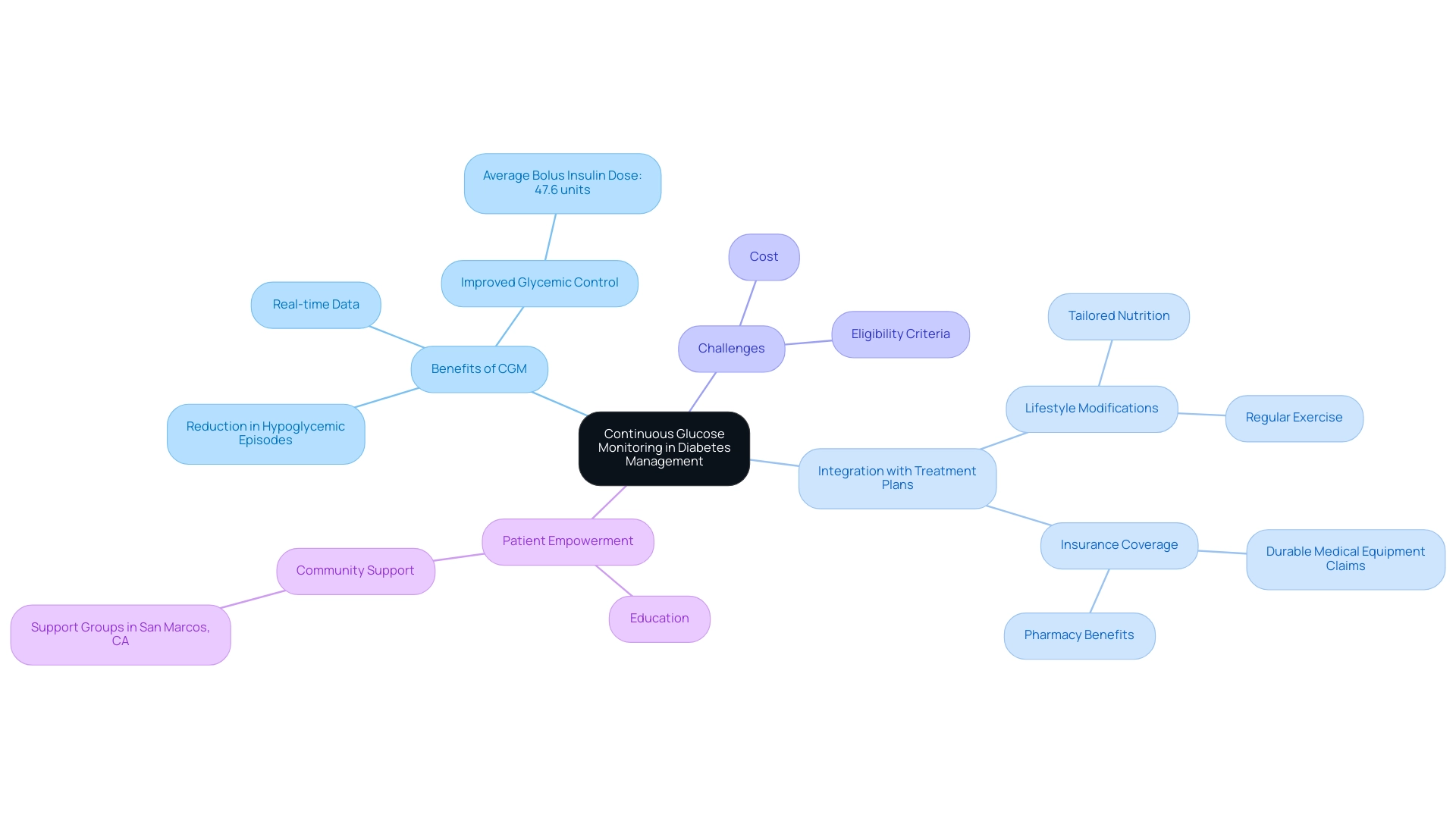
Continuous Glucose Monitoring (CGM) has emerged as a vital tool in managing blood sugar levels, particularly for individuals living with type 2 diabetes. The latest guidelines from the American Diabetes Association standards of care 2025 encourage the integration of CGMs, underscoring their ability to provide real-time blood glucose data. This functionality empowers patients to recognize their glucose patterns and make informed adjustments to their treatment strategies, aligning beautifully with the personalized approach offered by functional medicine.
It’s important to acknowledge the struggles many face in this journey. A recent analysis involving 182 patients—91 in the intervention group using CGMs and 91 matched controls—showed a significant impact on glycemic control, with the average bolus insulin dose recorded at 47.6 units among users. Furthermore, the use of CGM technology has been linked to a reduction in hypoglycemic episodes, enhancing the overall quality of life for many users. Tracy S. Tylee, a consultant in glucose control, emphasizes the importance of discussing CGM integration with healthcare providers, stating, “Addressing insurance coverage barriers is vital for ensuring equitable access to this essential technology.”
Understanding how CGMs fit into an individualized care plan is crucial. Many patients find that combining CGMs with lifestyle modifications, as emphasized by Dr. Jason Shumard—such as tailored nutrition and regular exercise—can lead to significant improvements. Functional medicine practitioners utilize comprehensive assessments and diagnostic tests, including metabolic panels and genetic testing, to identify individual wellness profiles and tailor treatment plans accordingly. However, the complexities of insurance coverage for CGM systems reveal that many claims are processed as durable medical equipment, with a growing percentage being covered under pharmacy benefits.
Yet, barriers such as cost and strict eligibility criteria can hinder access. As CGMs continue to evolve, they represent not just a technological advancement but a pivotal shift towards improved management strategies for diabetes. Empowering patients through education and community support in San Marcos, CA, further enhances their ability to manage their condition effectively and achieve long-term health improvements. Remember, you are not alone in this journey, and with the right support, positive change is possible.
Medication Management: New Guidelines for GLP-1 Receptor Agonists
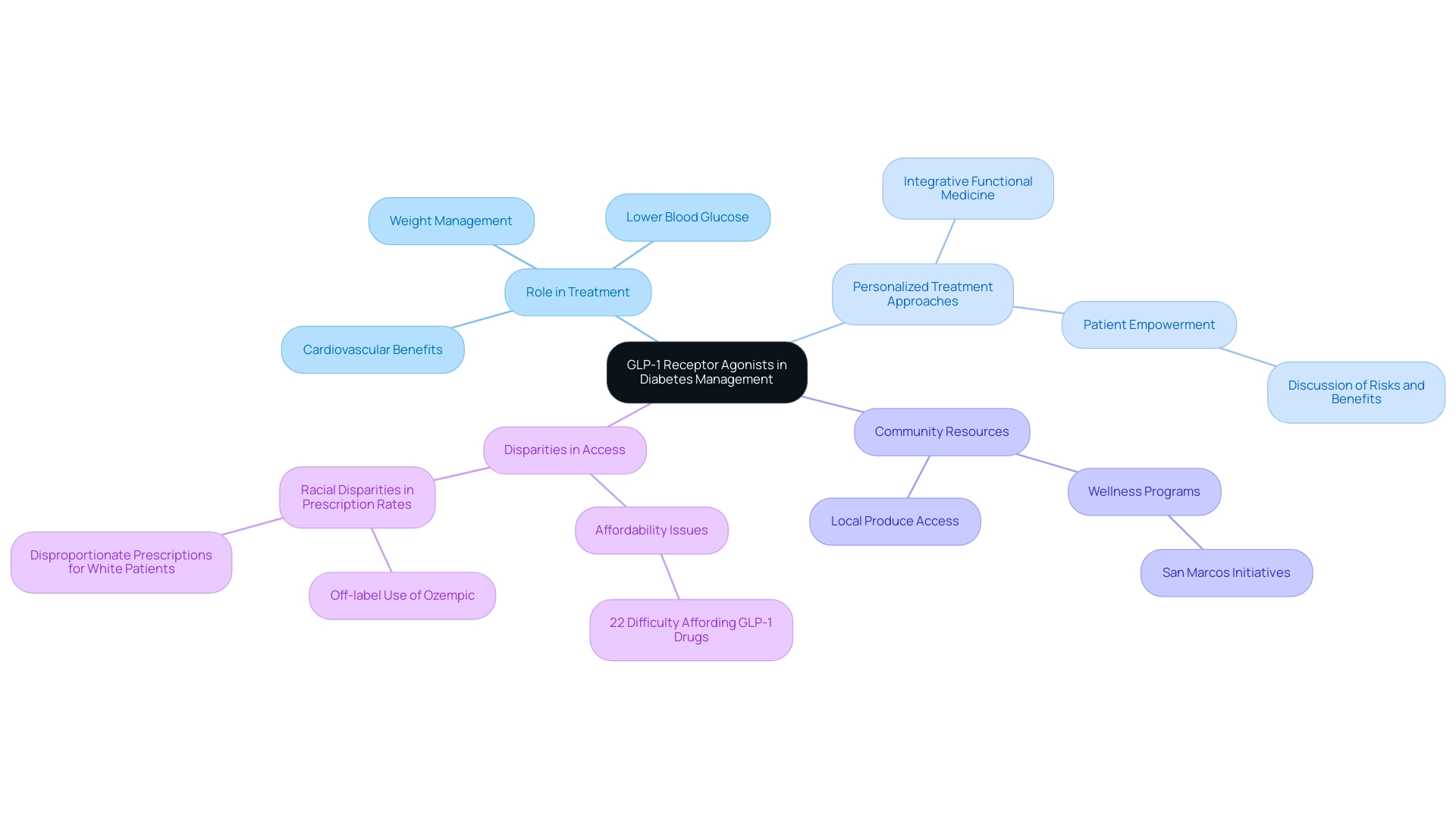
The latest updates to the American Diabetes Association (ADA) Standards highlight the essential role of GLP-1 receptor agonists in managing type 2 diabetes. These medications not only effectively lower blood glucose levels but also aid in weight management and offer significant cardiovascular benefits. It’s important to recognize that according to the American Diabetes Association standards of care 2025, healthcare providers are encouraged to consider GLP-1 receptor agonists early in the treatment process, especially for individuals who are obese or have cardiovascular risk factors.
This approach allows for a more personalized treatment plan that aligns with the principles of integrative functional medicine. Many patients find that engaging in discussions about potential risks and benefits tailored to their unique health profiles is empowering. Furthermore, with the recent approval of GLP-1 drugs for heart disease, eligibility for coverage has expanded, addressing some access issues faced by individuals with diabetes. However, it’s crucial to acknowledge that disparities still exist, particularly among racial groups, underscoring the need for equitable treatment practices.
For instance, the off-label prescription of Ozempic for weight loss has increased, leading to supply shortages for individuals with diabetes who genuinely require the drug. Racial disparities in prescription rates are evident, raising concerns. As Ryan Costello emphasizes, maintaining clear communication about treatment options is vital. This ensures that individuals receive the best possible care without the burden of financial barriers, as 22% of adults report significant difficulties affording GLP-1 medications. This interprofessional team approach is essential for managing T2DM and obesity effectively, ensuring all aspects of a patient’s well-being are considered.
Additionally, empowering lifestyle modifications through personalized guidance—such as embracing a balanced diet rich in local produce and engaging in community wellness programs—can significantly enhance the management of blood sugar levels. Community wellness initiatives in San Marcos, CA, offer valuable resources, education, and support for individuals managing their condition, assisting them in connecting with others who share similar wellness objectives. Incorporating local resources such as farmers’ markets and outdoor activities can further support holistic wellness strategies.
For a comprehensive understanding of GLP-1 receptor agonists and their application in managing blood sugar levels, the American Diabetes Association standards of care 2025 provide extensive insights. The functional medicine approach emphasizes comprehensive assessments and diagnostic tests to identify individual health factors, ensuring that treatment plans are as effective as possible.
Early Detection: Autoantibody Screening and Type 1 Diabetes
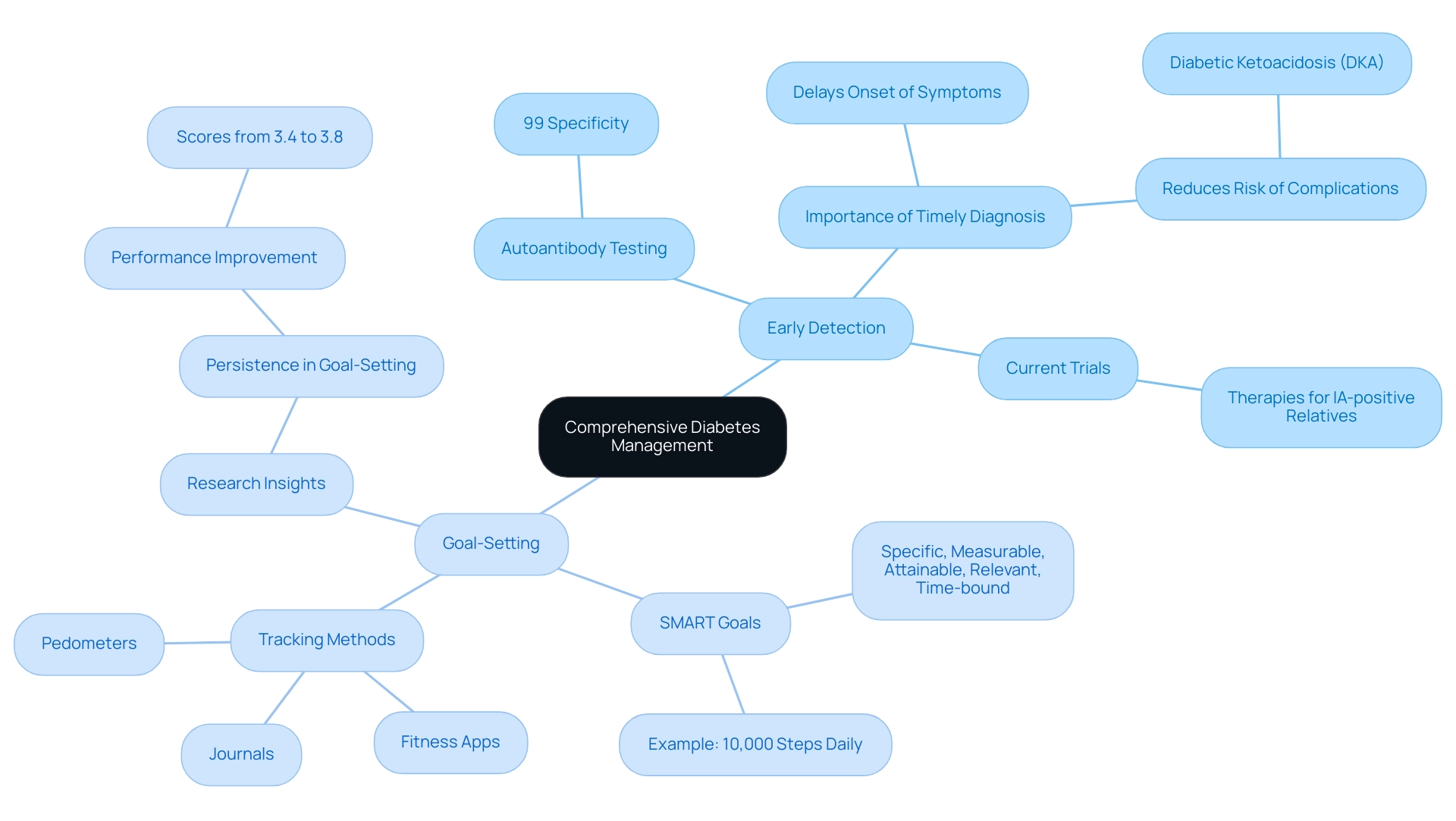
The American Diabetes Association Standards of Care 2025 highlight the vital importance of autoantibody testing for early screening of individuals at risk for type 1 diabetes. Recognizing the presence of autoantibodies can lead to timely diagnoses and prompt interventions. This proactive approach not only has the potential to delay the onset of clinical symptoms but also reduces the risk of severe complications, such as diabetic ketoacidosis (DKA). If you have a family history of type 1 conditions or genetic predispositions, it’s important to engage in discussions with your healthcare provider about the benefits of screening.
At the same time, individuals with Type 2 diabetes are encouraged to embrace effective strategies for tracking progress and setting goals on their wellness journey. Utilizing SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly enhance focus and motivation in managing health. For example, consider setting a goal to walk 10,000 steps each day to increase daily physical activity.
To effectively monitor progress, individuals can use various tracking methods, such as fitness apps, journals, and pedometers. Research shows that persistence in goal-setting can positively influence performance; for instance, scores improved from 3.4 (SD = 2.0) to 3.8 (SD = 1.9) under specific conditions, illustrating the power of structured goal-setting. The Barbara Davis Center Autoantibody Laboratory proudly boasts a remarkable 99% specificity for its assays, ensuring the accuracy of these tests, which supports informed decision-making.
Moreover, recent trials involving IA-positive first-degree relatives are exploring therapeutic approaches aimed at preventing type 1 conditions, showcasing ongoing advancements in early detection methods. Insights shared by researchers, including statements from experts like L.Y., who emphasized, ‘Effective communication regarding screening results is crucial for managing the psychological impact on individuals and their families,’ highlight the importance of addressing these concerns. By prioritizing both early detection and organized goal-setting, along with effective tracking methods, individuals can cultivate a sense of achievement and maintain engagement in their wellness management. This ultimately leads to improved health outcomes.
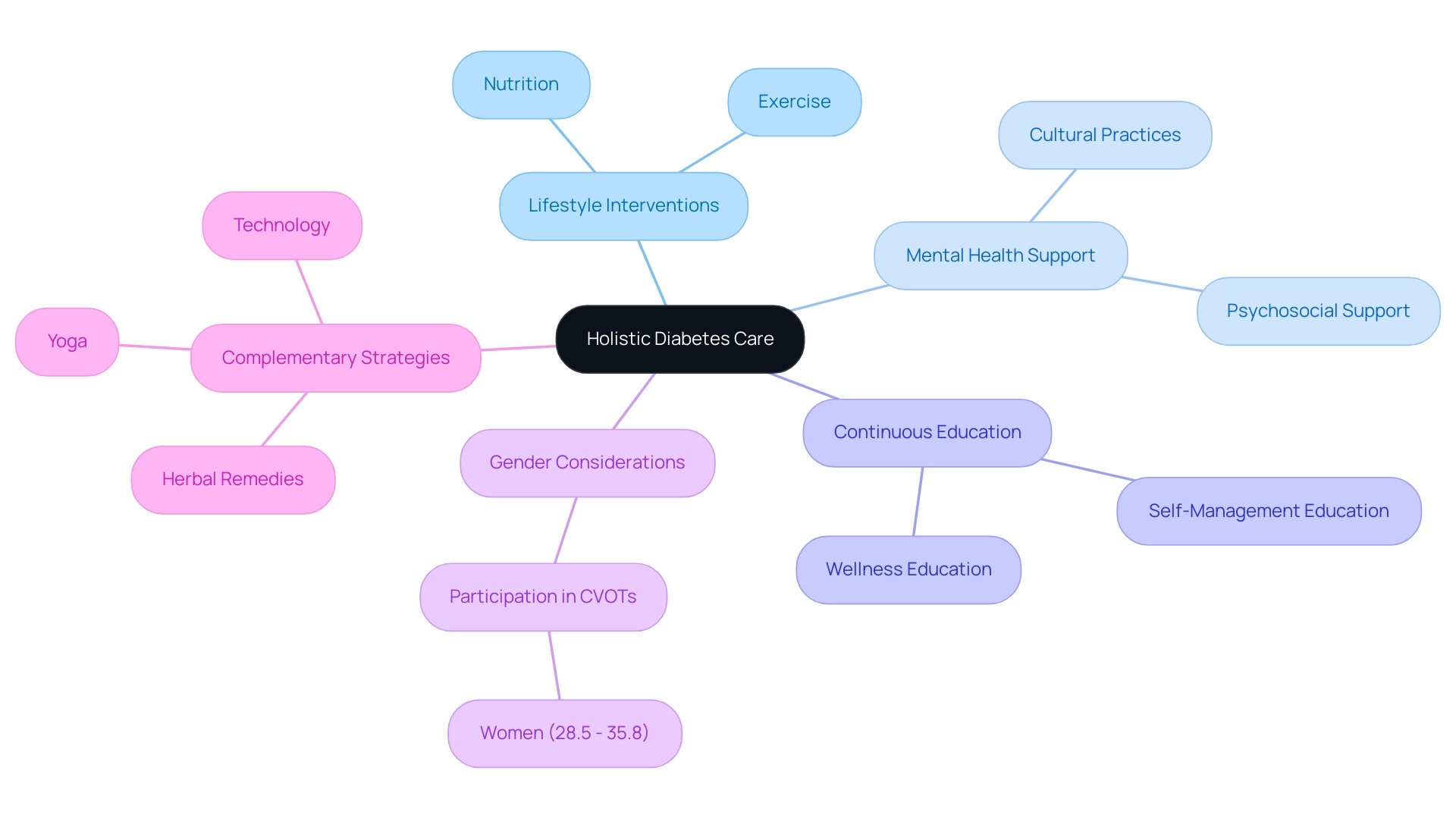
Holistic Diabetes Care: Integrating Lifestyle, Mental Health, and Education
The American Diabetes Association Standards of Care 2025 emphasize the necessity for a holistic approach to managing diabetes, integrating lifestyle interventions—such as nutrition and exercise—with mental health support and continuous education. We offer services that include detailed testing beyond typical lab work, allowing us to create a customized plan specifically tailored to your unique needs. Many patients find that self-management education significantly enhances their skills and glycemic control, leading to a greater number of individuals reaching their target HbA1c levels.
It’s important to recognize that women constituted between 28.5% and 35.8% of participants in recent cardiovascular outcome trials (CVOTs) related to managing blood sugar conditions. This highlights the importance of considering gender demographics in care. As Yupin Aungsuroch, an Associate Professor at Chulalongkorn University, emphasizes, a comprehensive care strategy for managing blood sugar conditions includes:
- Psychosocial support
- Lifestyle changes
- Wellness education
- Herbal remedies
- Cultural practices
- Yoga
- Technology
This holistic perspective empowers individuals to develop sustainable habits that enhance their physical health and improve emotional well-being.
Additionally, educational materials and support networks play a vital role in cultivating community. They offer essential insights for individuals navigating the complexities of care. Enhancing data connectivity and accessibility across different environments is essential for increasing the reliability and usefulness of real-world evidence (RWE) in diabetes care. Moreover, care for individuals with blood sugar issues must be tailored. As shown in the case study named ‘Individualization of Diabetes Care,’ collaborative decision-making is crucial to align treatment plans with individuals’ values and preferences.
By adopting these comprehensive strategies, including the removal of reliance on insulin and other medication therapies, we align with the American Diabetes Association standards of care 2025. This ensures that blood sugar level control is tailored to meet the unique needs and preferences of each individual. Testimonials from our patients highlight their success in managing and overcoming their condition through our services, ultimately empowering them to make informed choices.
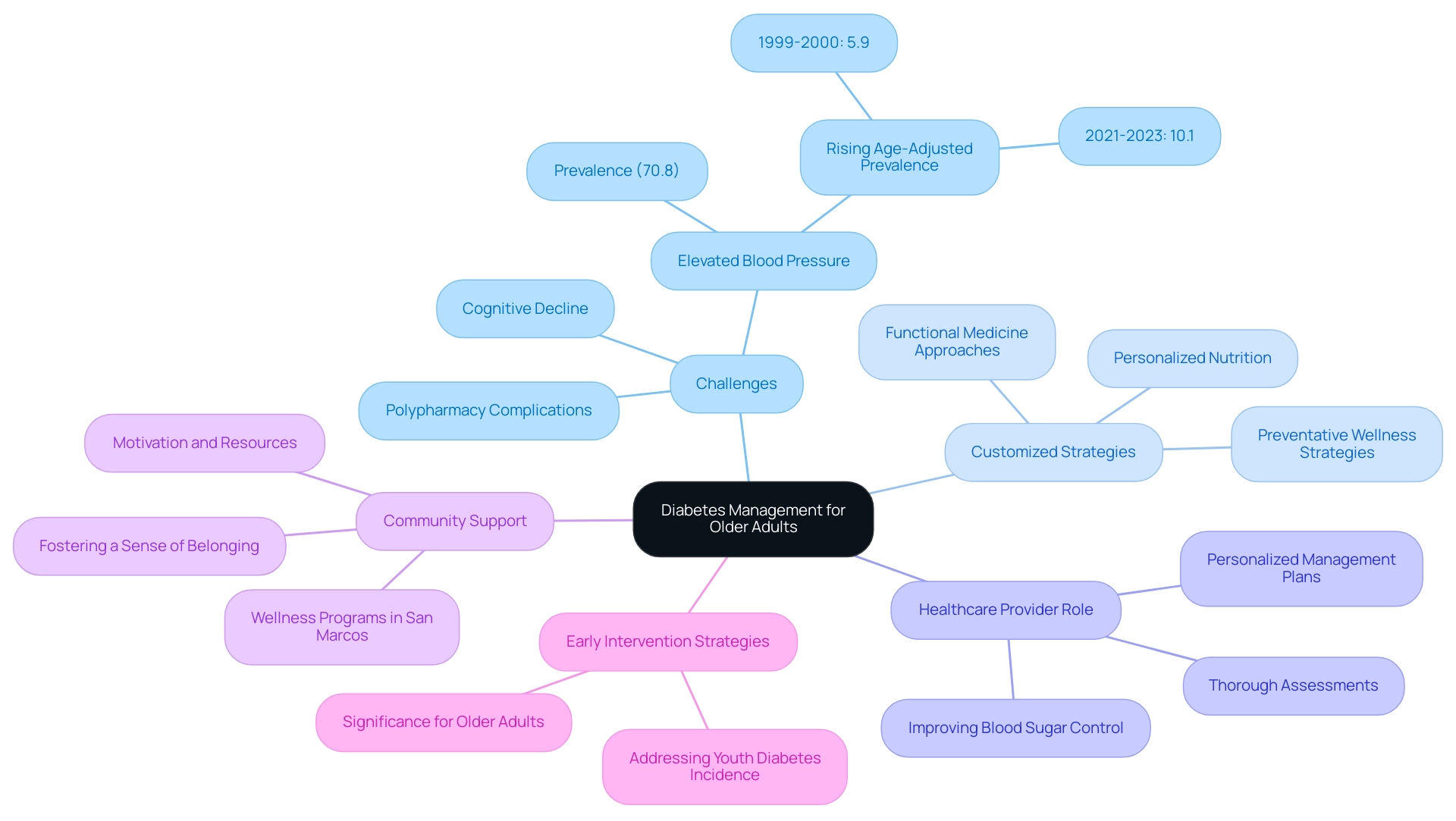
Tailored Approaches for Older Adults in Diabetes Management
The American Diabetes Association Standards of Care 2025 highlight the importance of customized health strategies for older adults, recognizing the unique challenges this group faces, such as cognitive decline. Did you know that over 70.8% of U.S. adults with diagnosed conditions experience elevated blood pressure? This prevalence of comorbidities complicates management for older adults. Alarmingly, the age-adjusted prevalence of this condition has risen from 5.9% in 1999–2000 to 10.1% as of August 2023. This underscores an urgent need for effective interventions.
As older adults often deal with complications from polypharmacy and cognitive decline, a nuanced approach to diabetes care is critical. Dr. Jason Shumard’s comprehensive guide emphasizes empowering individuals through preventative wellness strategies, including personalized nutrition and functional medicine approaches. It’s essential to modify medication plans while concentrating on each individual’s functional abilities and overall well-being.
Healthcare providers are encouraged to conduct thorough assessments of older adults’ unique needs to formulate personalized management plans that improve blood sugar control. This comprehensive perspective on care not only tackles health issues but also addresses the intricacies of managing other conditions, ultimately enhancing patient outcomes. Additionally, community wellness programs in San Marcos provide invaluable resources and support for individuals managing their condition, fostering a sense of belonging and motivation.
The increasing prevalence of the condition in youth highlights the significance of early intervention strategies that can also be advantageous for older adults. By fostering a community of support and well-being, we can create a nurturing environment that benefits everyone.
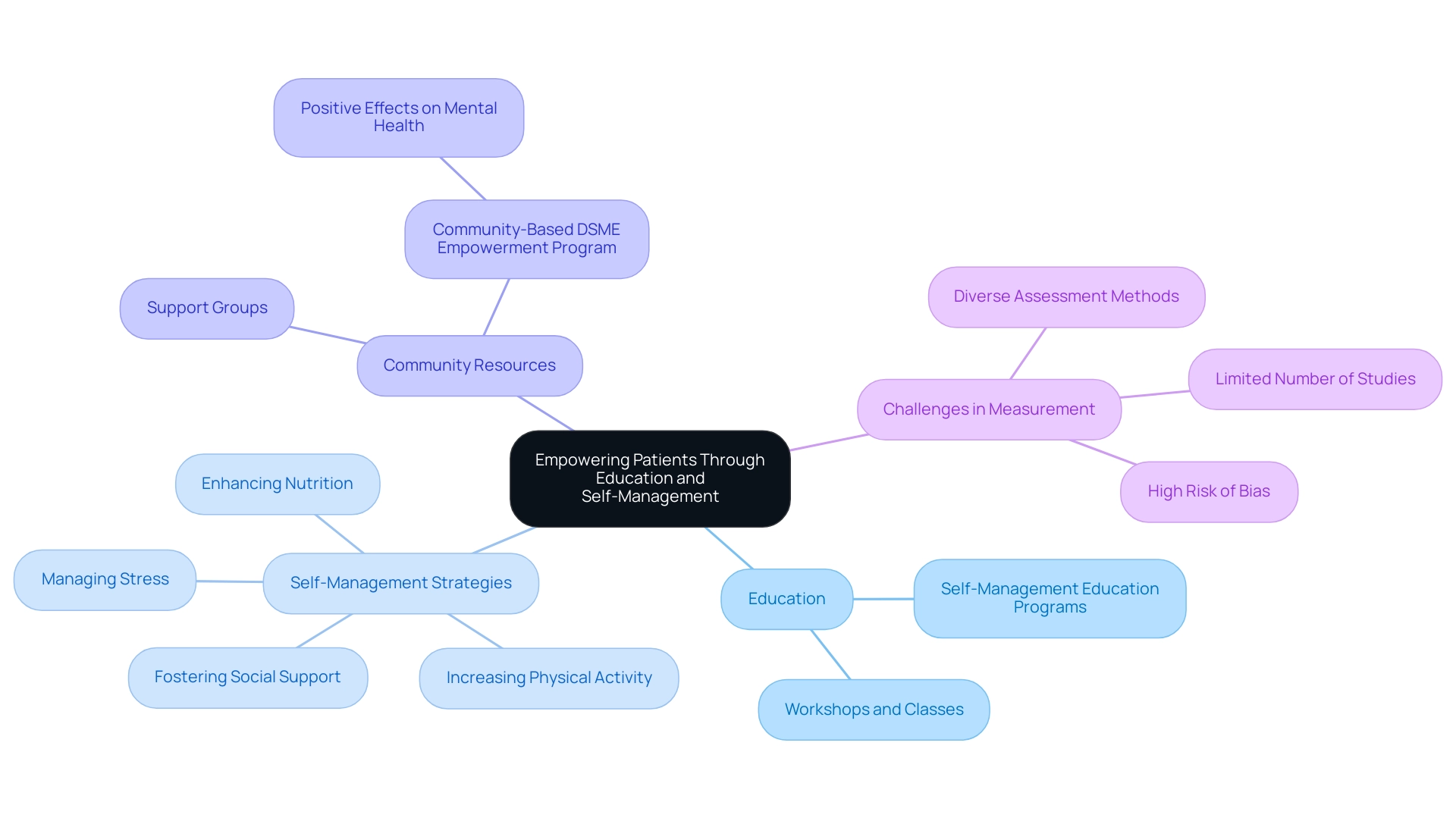
Empowering Patients: The Importance of Education and Self-Management
Empowering individuals through education is a fundamental principle outlined in the American Diabetes Association Standards of Care 2025. It’s essential to recognize that taking an active role in managing one’s condition can be transformative. By gaining a comprehensive understanding of diabetes, establishing realistic wellness goals, and making informed choices regarding treatment options, individuals can truly empower themselves. This empowerment is crucial as many navigate the journey toward functional medicine solutions aimed at reversing Type 2 metabolic disorders and related conditions like hypothyroidism.
Self-management education programs play a vital role in this process. They enhance individuals’ knowledge, skills, and confidence, leading to improved health outcomes. For instance, many have found success through the Community-Based DSME Empowerment Program, which has shown positive effects on mental health-related quality of life through a causal mediation analysis. This highlights the beneficial impact of educational initiatives. Many patients find that effective techniques for progress monitoring and goal formulation, such as applying SMART objectives within walking initiatives, greatly assist in their wellness journeys related to thyroid conditions.
These strategies include:
- Enhancing nutrition
- Increasing physical activity
- Managing stress
- Fostering social support
Resources such as education classes, workshops, and support groups are invaluable for enhancing individual empowerment. However, it’s important to note that quantifying the exact effects of self-management education (DSME) on patient-reported outcomes can be challenging. With only 137 articles obtained for review and diverse assessment methods, the landscape is complex.
The high risk of bias, particularly from studies conducted in Iran, presents challenges in drawing definitive conclusions. As trends in patient empowerment evolve, these educational programs continue to play a crucial role in fostering effective management strategies for diabetes, aligning with the American Diabetes Association Standards of Care 2025. To take the first step toward reversing diabetes and enhancing your health, why not schedule a session today or register for our upcoming workshops? You deserve support on this journey.
Conclusion
The 2025 Standards of Care in Diabetes established by the American Diabetes Association mark a significant evolution in diabetes management. These guidelines focus on personalized care that integrates innovative strategies and lifestyle modifications, acknowledging the unique struggles that individuals with diabetes face. By emphasizing continuous glucose monitoring, medication management with GLP-1 receptor agonists, and early detection through autoantibody screening, they provide a comprehensive framework aimed at improving patient outcomes.
It’s important to recognize that a holistic approach, which incorporates mental health support and education, is vital for empowering individuals with diabetes. Many patients find that the integration of community resources and tailored interventions—especially for older adults and those at higher risk—ensures that care is not only effective but also adaptable to the unique challenges they encounter. The emphasis on self-management education and structured goal-setting further underscores the importance of patient agency in navigating their health journeys.
Ultimately, the 2025 ADA Standards advocate for a transformative shift towards individualized, compassionate care that recognizes the complexities of diabetes. By prioritizing patient education and support, healthcare providers can foster environments where individuals feel equipped to manage their conditions effectively. This collective effort can lead to enhanced quality of life and better health outcomes for those living with diabetes, paving the way for a brighter, healthier future. Together, we can embrace this journey towards wellness, ensuring that every step taken is one of hope and empowerment.
Frequently Asked Questions
What are the main advancements in the American Diabetes Association Standards of Care 2025 for blood sugar regulation?
The main advancements include improved strategies for diagnosing diabetes, innovative methods to prevent or delay type 2 diabetes, and a focus on intensive lifestyle interventions such as outdoor activities and community support to prevent macrovascular disease.
What holistic approaches are recommended for managing type 2 diabetes?
Holistic approaches include stress management techniques, mindfulness practices, and the importance of social support networks, as highlighted in Dr. Jason Shumard’s 30-Day Diabetes Reset Program.
How does technology play a role in diabetes management according to the 2025 guidelines?
The integration of Continuous Glucose Monitoring (CGM) technology is encouraged, as it provides real-time blood glucose data, helping patients understand their glucose patterns and make informed treatment adjustments.
What are the benefits of using Continuous Glucose Monitoring (CGM) for individuals with type 2 diabetes?
CGMs have been linked to improved glycemic control, a reduction in hypoglycemic episodes, and an overall enhancement in the quality of life for users.
What challenges do patients face regarding CGM technology?
Patients may encounter barriers such as cost, strict eligibility criteria, and issues with insurance coverage, as many CGM claims are processed as durable medical equipment.
What is the significance of gestational diabetes mellitus (GDM) in the context of diabetes risk?
Individuals diagnosed with GDM through the one-step approach have a 3.4-fold higher risk of developing prediabetes and type 2 diabetes compared to those diagnosed through the two-step approach, highlighting the need for tailored screening protocols.
How can patients empower themselves in managing diabetes?
Patients can empower themselves by combining CGM use with lifestyle modifications, receiving education, and engaging with community support to improve their management strategies and health outcomes.