Overview
The article compares the A1C test and glucose test as methods for monitoring diabetes, highlighting their distinct roles in managing blood sugar levels. It explains that while the A1C test provides an average of blood glucose over two to three months, making it useful for long-term management, glucose tests measure immediate blood sugar levels, which is crucial for real-time monitoring and diagnosis, thus supporting a comprehensive approach to diabetes management.
Introduction
The A1C test stands as a pivotal tool in the management of type 2 diabetes, providing insights that extend beyond the limitations of daily glucose monitoring. By measuring average blood glucose levels over a span of two to three months, it offers a comprehensive perspective on blood sugar control, essential for both diagnosis and ongoing management.
As the prevalence of diabetes continues to rise, understanding the significance of A1C testing becomes increasingly critical. This article delves into the nuances of the A1C test, comparing it with traditional glucose tests, discussing optimal testing frequencies, and weighing the pros and cons of its use.
By exploring these facets, individuals can gain a clearer understanding of how to effectively navigate their diabetes management journey, ultimately leading to better health outcomes and reduced anxiety regarding potential complications.
Understanding the A1C Test: Definition and Importance
The A1C examination, also referred to as the hemoglobin A1C or glycated hemoglobin assessment, is a cornerstone for individuals managing type 2 diabetes. This assessment measures average blood glucose levels over the previous two to three months, offering a comprehensive overview of blood sugar control that highlights the differences between the A1C test vs glucose test and the sporadic nature of daily glucose monitoring. Results from the A1C examination are expressed as a percentage, with elevated levels indicating inadequate blood sugar management.
Beyond its diagnostic capabilities, the A1C assessment plays an essential role in ongoing management of the condition and evaluating the risk of complications, which can often lead to anxiety for patients. Regular A1C testing allows healthcare providers to customize treatment plans effectively, which is particularly crucial given the rising medical costs associated with diabetes—surging from $10,179 in 2012 to $12,022 in 2022. This financial burden underscores the test’s value in enhancing patient outcomes and mitigating long-term healthcare expenses.
Recent studies indicate that consistent A1C monitoring significantly improves management of the condition, leading to better health outcomes for patients. For instance, one patient, after following a holistic regimen at the Integrative Wellness Center, reported a significant drop in their A1C levels, which alleviated their anxiety about potential complications. Significantly, research supported by NIH grants has validated the effectiveness of the A1C test vs glucose test, while the ARIC study confirmed its predictive capability concerning future risk of the condition, particularly when the A1C test is combined with fasting glucose measurements.
The authors of this study affirmed, ‘These findings support A1C as a suitably efficient tool to identify people at risk and should help to advance efforts to identify individuals at risk for type 2 for referral to appropriate preventive interventions.’ Collectively, this evidence not only highlights the critical role of A1C testing in managing blood sugar levels but also aligns with the holistic approach employed by the Integrative Wellness Center, addressing root causes and empowering patient health for those overcoming metabolic disorders and chronic health issues.
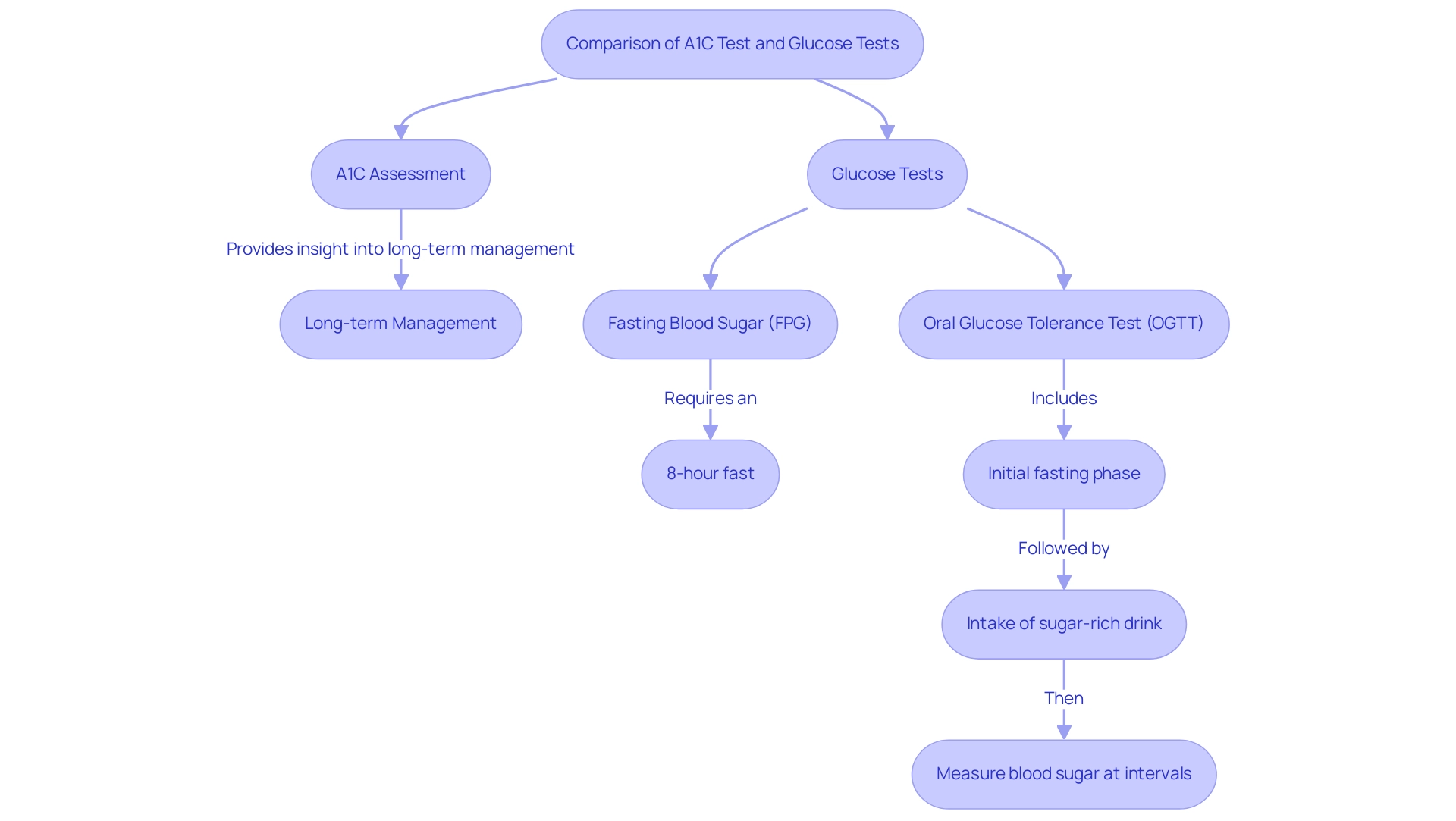
A1C Test vs. Glucose Tests: Key Differences Explained
The A1C assessment and sugar evaluations, including fasting blood sugar (FPG) assessments and oral sugar tolerance evaluations (OGTT), serve distinct roles in managing blood sugar levels. The A1C assessment shows average blood sugar levels over the prior two to three months, providing insight into long-term sugar management, which is essential for pregnant women to avoid gestational diabetes. In contrast, sugar measurements evaluate blood sugar levels at a specific moment.
For example:
- Fasting blood sugar assessments require an eight-hour fast before evaluation.
- The oral tolerance assessment includes:
- An initial fasting phase
- The intake of a sugar-rich drink
- Blood sugar levels later measured at intervals to assess the body’s reaction to sugar consumption.
Each testing method has its unique advantages:
- The A1C test is particularly beneficial for ongoing management of blood sugar levels, providing a broader view of glycemic control.
- Sugar tests are crucial for immediate assessments and diagnosing the condition.
Recent findings indicate that the optimal HbA1c threshold for diagnosing the condition based on OGTT criteria is 6.2%. Additionally, the Thai CV risk score demonstrates a notable difference in median scores, with a score of 10 for the OGTT-defined condition group compared to 3 for individuals with normal sugar tolerance (NGT).
Despite procedural challenges related to HbA assessment—highlighted in the case study titled ‘Procedural Challenges of HbA Assessment’ which emphasized the necessity for trained personnel—evidence indicates that a single A1C evaluation can reliably identify individuals at lower risk for type 2 metabolic disorder. As highlighted by specialists in metabolic disorders, the comparison of the A1C test vs glucose test serves a crucial function in the thorough evaluation of dysglycemic status, assisting both patients and healthcare providers in making informed choices about monitoring strategies. Notably, it is advocated that OGTT should continue to be used as a screening tool for identifying dysglycemic status in particular populations.
Additionally, it is important to consider the dangers of traditional treatments for insulin resistance, as these can lead to severe complications if not monitored effectively, underscoring the necessity of regular testing and personalized management strategies.
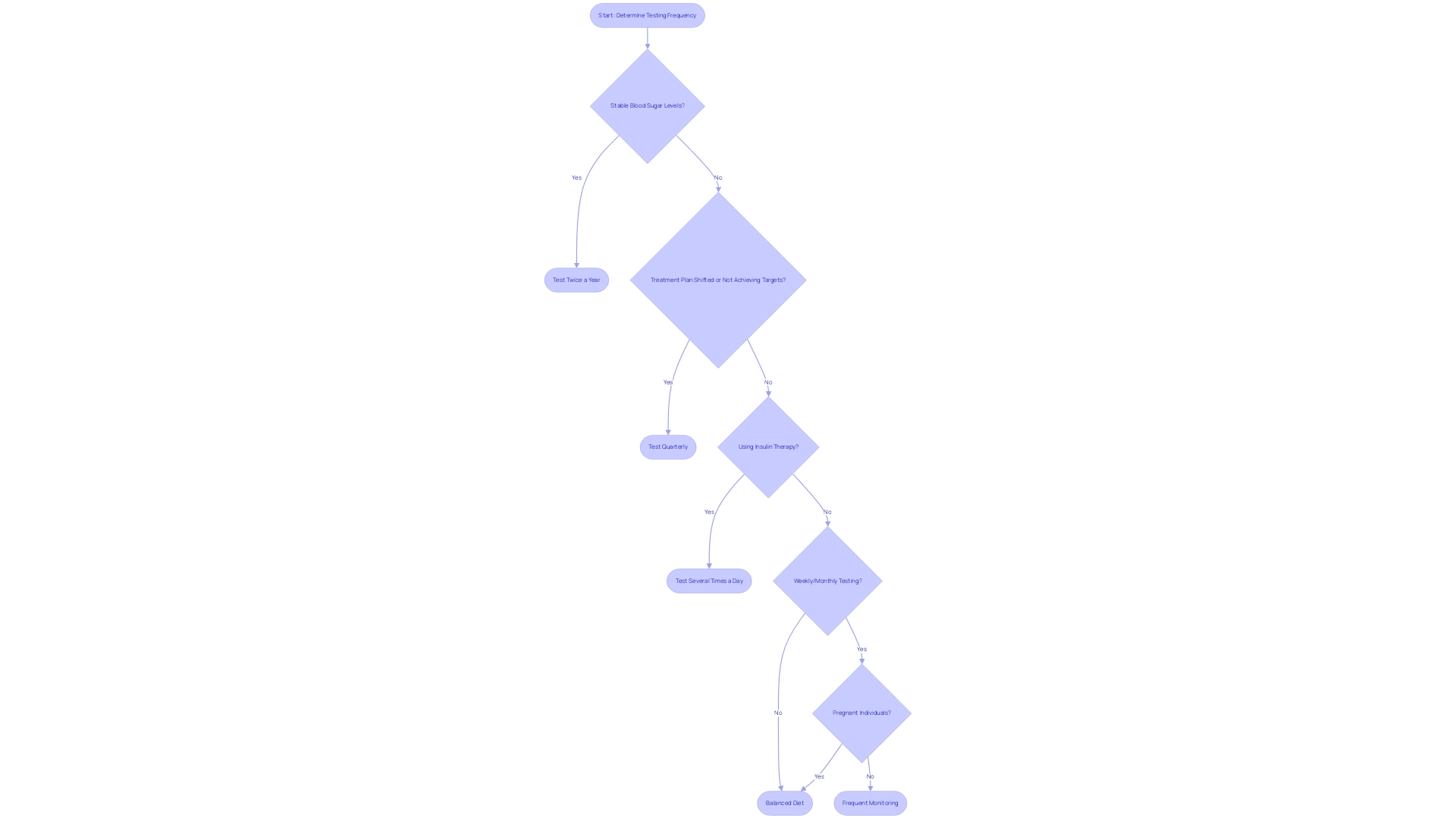
How Often Should You Get Tested? A1C and Glucose Testing Frequency
The frequency of A1C testing, when considering the A1C test vs glucose test, is largely dependent on an individual’s health management and overall control. According to the American Diabetes Association Professional Practice Committee, as stated in their 2024 Standards of Care in Diabetes, individuals with stable blood sugar levels should undergo A1C testing at least twice a year. However, for those whose treatment plans have shifted or who are not achieving their glycemic targets, quarterly testing is recommended.
In contrast, the frequency of the A1C test vs glucose test can vary significantly among patients. For instance, individuals on insulin therapy may need to monitor their blood sugar levels several times a day, while others may find that weekly or monthly testing suffices. Recognizing the appropriate testing frequency, particularly the A1C test vs glucose test, is vital for maintaining optimal blood sugar control and mitigating the risk of complications.
Furthermore, recent guidelines underscore the importance of personalized monitoring strategies to enhance management of the condition, particularly in the context of the A1C test vs glucose test, emphasizing the need for tailored approaches based on individual health conditions and treatment responses. Significantly, for pregnant individuals, it is essential to implement strategies such as:
- Maintaining a balanced diet
- Regular physical activity
- Frequent monitoring of blood sugar levels to prevent gestational complications
Additionally, traditional treatments for managing blood sugar levels can pose significant risks, including the potential for increased insulin resistance and adverse health effects if not carefully monitored.
In a recent study, 165 participants who did not qualify for gestational glucose management were treated for isolated elevated fasting plasma glucose levels exceeding 95 mg/dL, highlighting the importance of monitoring in diverse patient populations. Additionally, updates to chronic kidney disease management strategies illustrate the real-world implications of A1C testing frequency, particularly for diabetic patients with chronic conditions, showcasing how integrated management can lead to improved outcomes.
Pros and Cons of A1C Testing for Diabetes Management
The A1C assessment provides considerable benefits in managing the condition, especially its capacity to indicate long-term blood sugar regulation, which is essential for assessing the efficacy of treatment approaches. This test is notably convenient, requiring only a blood sample without the need for fasting, making it accessible for routine monitoring. A1C is acknowledged as a reasonable method for diagnosing the condition; however, it is important to consider the limitations associated with A1C testing.
For instance, a study from the Finnish Diabetes Prevention Study revealed that the sensitivity of an A1C level of ≥6.5% for diagnosing the condition is only 39%, indicating potential underdiagnosis in certain populations. Moreover, A1C may not accurately represent blood sugar levels in individuals with conditions such as anemia or other hemoglobinopathies that can distort results. Another critical drawback is that the A1C test does not provide immediate feedback on current blood sugar levels, which can be particularly disadvantageous for patients needing real-time data for insulin adjustments.
This emphasizes the significance of a comprehensive strategy for managing blood sugar levels, which should incorporate both the A1C test vs glucose test and real-time sugar monitoring, while also addressing the underlying causes of the condition, including insulin resistance. Importantly, addressing the anxiety and worry surrounding potential complications of this condition can significantly enhance patient well-being and management outcomes. Comprehending postprandial sugar excursions is essential, as these are vital signs of complications, highlighting the significance of sugar variability.
For further insights, readers may refer to the book ‘Hemoglobin A1C’ by Eyth and Naik, which provides a comprehensive overview of the topic. Through a holistic regimen, patients can re-examine the source of their condition and adopt strategies that empower them to manage their health more effectively.
Interpreting A1C and Glucose Test Results for Better Diabetes Control
Interpreting results from the A1C test vs glucose test is crucial for effective management of the condition, especially for type 2 patients seeking to eliminate anxiety over potential complications. At the Integrative Wellness Center, we provide transformative health solutions customized to your needs, ensuring that when considering the A1C test vs glucose test, A1C results, presented as a percentage, are typically aimed below 7% for most adults with this condition, as higher percentages relate to a heightened risk of complications. Recent studies indicate that among various demographics, non-Hispanic Black children and adolescents exhibit the highest incidence of type 2 conditions, emphasizing the need for tailored management strategies.
The economic impact of this condition is significant, with the total estimated costs of diagnosed cases in the United States reaching $413 billion in 2022, highlighting the importance of effective management. When evaluating fasting levels below 100 mg/dL for individuals without this condition, it is important to consider the A1C test vs glucose test, with glucose results measured in mg/dL. Understanding these metrics, such as the A1C test vs glucose test, enables patients to make informed adjustments to their treatment plans, dietary choices, and physical activity levels.
Furthermore, as highlighted by Wagenknecht LE, it is essential for patients to collaborate with healthcare providers when interpreting these results. This partnership can lead to more personalized and effective management strategies at the Integrative Wellness Center, ultimately enhancing health outcomes and improving quality of life. The integration of continuous glucose monitoring techniques, as noted in the International Comparison of Glycemic Control study, highlights the potential for improved glycemic control across various populations, offering valuable insights for managing results.
Additionally, with 447 case subjects having prior severe hypoglycemia compared to 520 control subjects, the importance of monitoring and accurately interpreting test results becomes even more evident, supporting the holistic approach to reversing the condition by addressing root causes and empowering patient health. Register now to take the first step towards a healthier future and eliminate the worry about diabetes complications.
Conclusion
The A1C test is a vital tool for managing type 2 diabetes, providing insights into average blood glucose levels over two to three months. This comprehensive assessment aids in treatment adjustments and helps evaluate the risk of complications, making it increasingly important as diabetes-related healthcare costs rise.
Differentiating between the A1C test and traditional glucose tests is essential. While the A1C test focuses on long-term control, glucose tests deliver immediate results. Using both testing methods effectively informs management strategies tailored to individual patient needs.
Regular testing frequency is critical in diabetes care. Guidelines recommend personalized monitoring, with A1C testing intervals adjusted based on blood sugar stability and treatment changes. This approach is essential for maintaining optimal control.
However, the A1C test has limitations, including potential inaccuracies in certain populations and the lack of real-time feedback. Acknowledging these drawbacks highlights the need for a comprehensive management strategy that combines A1C testing with real-time glucose monitoring.
In summary, the A1C test is indispensable in type 2 diabetes management. Committing to regular testing, understanding results, and working closely with healthcare providers empower individuals to enhance their diabetes care, leading to improved health outcomes and reduced anxiety about complications.
Frequently Asked Questions
What is the A1C examination?
The A1C examination, also known as the hemoglobin A1C or glycated hemoglobin assessment, measures average blood glucose levels over the previous two to three months, providing a comprehensive overview of blood sugar control.
How are the results of the A1C test expressed?
Results from the A1C examination are expressed as a percentage, with elevated levels indicating inadequate blood sugar management.
Why is the A1C assessment important for individuals with type 2 diabetes?
The A1C assessment is crucial for ongoing management of diabetes, evaluating the risk of complications, customizing treatment plans, and improving overall patient outcomes, which can help mitigate long-term healthcare expenses.
How does the A1C test compare to other blood sugar evaluations?
The A1C test shows average blood sugar levels over two to three months, while other tests like fasting blood sugar (FPG) and oral glucose tolerance tests (OGTT) measure blood sugar levels at a specific moment.
What are the specific procedures for fasting blood sugar and oral glucose tolerance tests?
Fasting blood sugar assessments require an eight-hour fast, while the OGTT involves an initial fasting phase, consumption of a sugar-rich drink, and subsequent blood sugar measurements at intervals.
What is the optimal HbA1c threshold for diagnosing diabetes based on OGTT criteria?
The optimal HbA1c threshold for diagnosing diabetes based on OGTT criteria is 6.2%.
What role does regular A1C monitoring play in diabetes management?
Regular A1C monitoring significantly improves diabetes management, leading to better health outcomes and reducing patient anxiety about potential complications.
What challenges are associated with A1C assessments?
Procedural challenges related to A1C assessments require trained personnel, but a single evaluation can reliably identify individuals at lower risk for type 2 metabolic disorders.
Why is it important to continue using OGTT as a screening tool?
OGTT should continue to be used as a screening tool for identifying dysglycemic status in specific populations, as it provides immediate assessments crucial for diagnosing the condition.
What are the dangers of traditional treatments for insulin resistance?
Traditional treatments for insulin resistance can lead to severe complications if not monitored effectively, highlighting the necessity for regular testing and personalized management strategies.