Overview
The ADA Diabetic Diet is designed to help individuals manage blood sugar levels through balanced nutrition, portion control, and careful selection of foods, emphasizing the importance of carbohydrate management. The article outlines key components of the diet, including recommended food categories and meal planning strategies, while highlighting the need for personalized approaches to enhance adherence and improve health outcomes for those with diabetes.
Introduction
Managing diabetes requires a comprehensive understanding of dietary choices that can significantly impact blood sugar levels and overall health. The American Diabetes Association (ADA) Diabetic Diet serves as a foundational guideline, emphasizing balanced nutrition, portion control, and the importance of nutrient-dense foods.
By focusing on carbohydrate management and incorporating a variety of food groups, individuals can develop effective meal plans that not only support blood glucose control but also enhance adherence to dietary recommendations.
This article delves into the principles and practical applications of the ADA diet, exploring key food categories, meal planning strategies, and the significance of hydration in diabetes management. Through informed choices and tailored dietary approaches, individuals can take proactive steps towards better health outcomes.
Understanding the ADA Diabetic Diet: Principles and Guidelines
The ada diabetic diet is specifically crafted to support healthy eating patterns while effectively managing blood sugar levels. Its fundamental principles center on balanced nutrition, portion control, and the selection of nutrient-rich items, which are crucial for overall health. A significant consideration is the management of carbohydrate intake, as carbohydrates have the most pronounced effect on blood glucose levels.
Incorporating a diverse range of foods is encouraged, including:
- Whole grains
- Fruits
- Vegetables
- Lean proteins
- Healthy fats
while simultaneously minimizing the consumption of:
- Processed foods
- Added sugars
- Saturated fats
Notably, adherence to the ADA diabetic diet remains a challenge, with only 36.5% of patients with sugar-related conditions complying with the ADA guidelines. This statistic highlights the necessity for personalized approaches to nutrition, accommodating individual wellness needs and preferences.
Furthermore, it is vital to recognize the dangers of traditional treatments, which can lead to severe complications and increased anxiety for patients. Grasping the context-specific challenges encountered by diabetic patients, including the importance of tackling insulin resistance and the emotional burden of managing their condition, is crucial for formulating effective dietary strategies. Such tailored dietary plans not only enhance adherence but also promote better health outcomes, particularly in blood sugar control, which is vital for effective diabetes management, especially for those at risk of gestational diabetes.
Practical Meal Planning: Making Healthy Choices on the ADA Diet
Effective meal planning on the ADA diet requires careful selection of items that adhere to established dietary principles while accommodating individual preferences and lifestyles. A well-structured meal plan should maintain a balanced intake of carbohydrates, proteins, and fats, which is crucial for managing blood glucose levels. Organizing meals ahead of time is crucial in avoiding impulsive choices that could result in unhealthy eating habits.
Utilizing tools such as grocery lists not only aids in organizing food purchases but also ensures adherence to dietary guidelines. Hand measurements can be particularly helpful in estimating portion sizes:
- Use your palm for 3 ounces of meat
- Use your thumb for 1 ounce of cheese
- Use your fist for 1 cup of fruit
- Use your cupped hand for 1-2 ounces of nuts
- Use your thumb tip for 1 tablespoon
- Use your fingertip for [[1 teaspoon
Meal prep containers](https://cdc.gov/diabetes](https://drshumard.com/effective-nutrition-counseling-for-managing-type-2-diabetes)/healthy-eating/diabetes-meal-planning.html) and tracking apps can further streamline the process, making it more manageable and efficient.
Incorporating a variety of flavors and textures into meals not only enhances the dining experience but is also vital for long-term adherence to the diet. For instance, the Very Low Carbohydrate Meal Pattern focuses on significant dietary restrictions, promoting health improvements by limiting carbohydrate intake to 20–50g of non-fiber carbohydrates per day, with more than half of calories derived from fats. This pattern has shown effectiveness in reducing A1C levels and supporting weight management, as evidenced by the TRE intervention study conducted by Parr EB et al., which showed a decrease in HbA1c (p = 0.053).
As Imai S. noted, ‘Subjects who consumed dinner in one sitting exhibited significantly higher values in the incremental AUC,’ underscoring the importance of meal timing and composition in managing blood sugar levels. By incorporating these components into meal planning within an ADA diabetic diet, individuals can better manage their condition and support their overall health.
Key Food Categories in the ADA Diabetic Diet
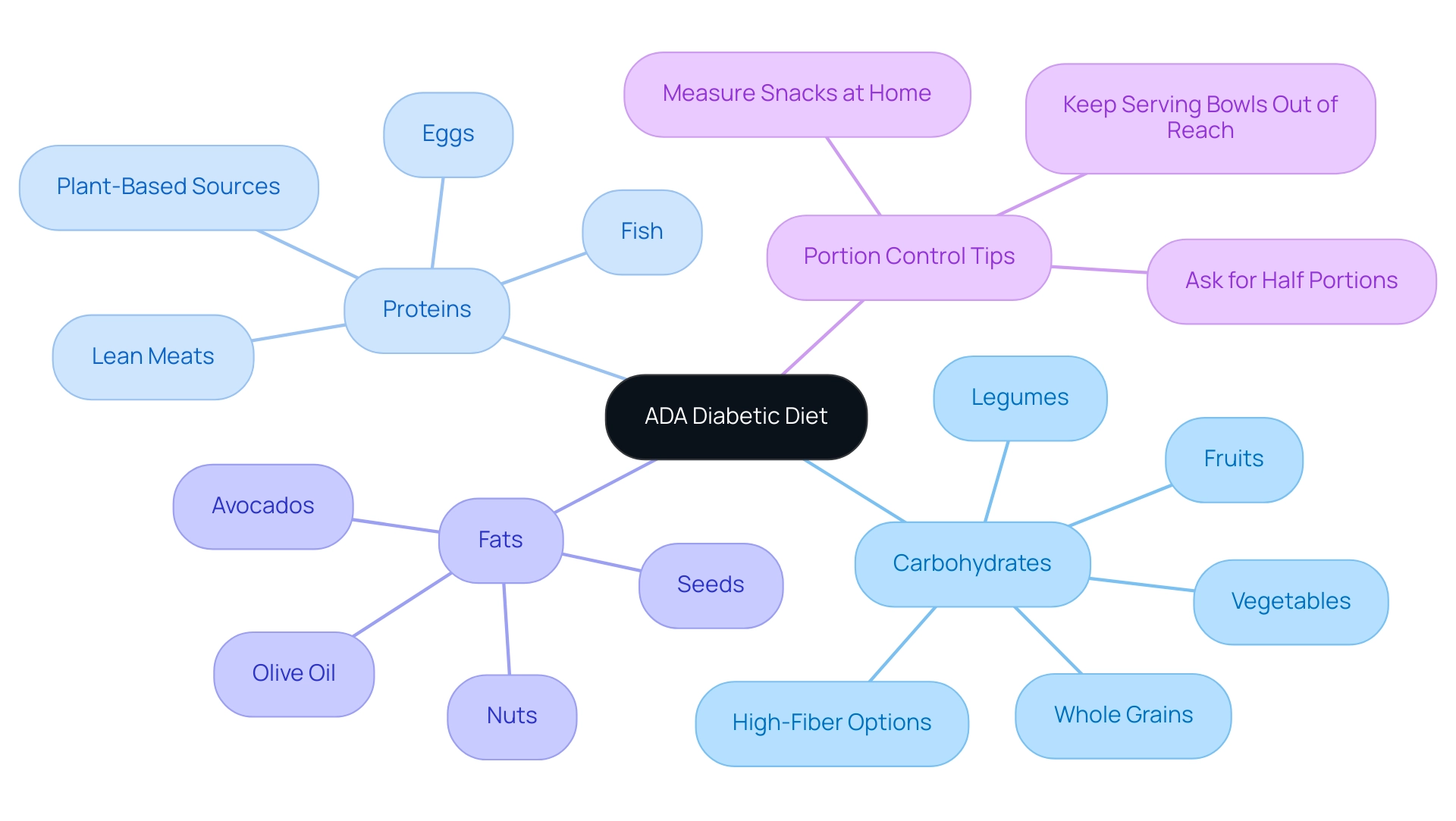
The American Diabetes Association (ADA) classifies items into essential categories, specifically carbohydrates, proteins, and fats, all of which play a crucial role in the ADA diabetic diet for managing blood sugar levels. Carbohydrates, which encompass fruits, vegetables, whole grains, and legumes, must be selected with care. Focusing on high-fiber options is particularly beneficial, as fiber aids in regulating blood sugar levels and promoting satiety.
Notably, recent studies have highlighted that one entree at a restaurant can often equal three or four servings, underscoring the need for portion control and mindful eating practices. Additionally, research by Djousse et al. analyzed the intake of eggs and its related risk factors for type 2 diabetes mellitus among African Americans, suggesting that particular dietary selections can greatly influence management of the condition.
Proteins, including lean meats, fish, eggs, and plant-based sources, are vital for muscle maintenance and help individuals feel full, effectively managing hunger. Healthy fats, sourced from nuts, seeds, avocados, and olive oil, contribute to heart health and overall wellness. A systematic review and meta-analysis of prospective studies titled ‘Nutrient categories and risk of developing type 2 diabetes mellitus‘ provides further insights into the relationship between various nutrient categories and the risk of developing type 2 conditions, reinforcing the importance of dietary choices.
By understanding the nutritional breakdown of these key categories, individuals can create balanced meals tailored to their dietary needs, such as following an ADA diabetic diet. Moreover, it is advisable to measure snacks at home and keep serving bowls out of reach during meals to further control portion sizes. This knowledge enables patients to make informed dietary selections that promote their health and effectively manage their condition with an ADA diabetic diet.
Utilizing the Diabetes Plate Method for Balanced Meals
The Plate Method serves as an effective visual tool for individuals managing type 2 conditions, aiding in the understanding and implementation of portion control within a balanced diet. This method divides a standard plate into specific sections:
- Half is designated for non-starchy vegetables
- One-quarter for lean protein
- One-quarter for carbohydrates
Such an approach not only simplifies portion control but also encourages the intake of nutrient-dense foods, supporting a comprehensive regimen aimed at addressing the underlying causes of the condition.
Recent studies, including the Diabetes Nutrition Education Study (DINES), have demonstrated that both carbohydrate counting and the modified plate method significantly enhance glycemic control in patients with an initial HbA1c between 7–10%. Specifically, the carbohydrate counting group showed a reduction in HbA1c of −0.86%, while the modified plate method group experienced a reduction of −0.76%, and the combined CDE group demonstrated an HbA1c reduction of −0.80%. This method is easily adaptable to various cuisines and personal preferences, making it a practical and versatile tool for daily meal planning.
As Joan Schilling from Michigan State University Extension highlights, ‘Ultimately, it is crucial to recognize that the plate approach does not substitute for your medical practitioner,’ underscoring the necessity to incorporate this method within the wider framework of blood sugar control. By adopting this approach, patients can alleviate some of the anxiety surrounding the potential complications of the disease, empowering them to take control of their well-being through informed dietary choices.
Hydration and Beverage Choices in the ADA Diabetic Diet
Hydration is essential not only for general well-being but also for efficient management of blood sugar levels. Individuals identified with the condition are encouraged to maintain adequate fluid intake, aiming for approximately:
- 1.7 liters (6.5 cups) for women
- 2.0 liters (8.5 cups) for men daily
Distributing this intake throughout the day can aid in sustaining hydration levels and supporting essential metabolic processes.
It is crucial to recognize that combining dehydration and blood sugar issues can lead to serious health complications, making proper hydration a priority. Minimizing the consumption of sugary beverages, such as sodas and sweetened juices, is essential, as they can cause significant spikes in blood sugar levels. Instead, individuals should prioritize water, herbal teas, or beverages devoid of added sugars, which can enhance hydration without adversely affecting glucose regulation.
Furthermore, managing caffeine intake is crucial, as excessive caffeine may lead to dehydration and could interfere with blood sugar control. As noted by Angela Ginn Meadow, RN, RDN, CDCES, Program Director at the Baltimore Metropolitan Diabetes Regional Partnership, proper hydration is a cornerstone of the ADA diabetic diet for effective diabetes care. Effective methods for quick blood sugar control include:
- Drinking water
- Engaging in physical activity
- Consuming high-protein snacks
- Administering fast-acting insulin as prescribed
Adopting these hydration strategies, along with awareness of the latest recommendations, can significantly contribute to better blood glucose management as part of an ADA diabetic diet and overall health.
Conclusion
Understanding and implementing the ADA Diabetic Diet can significantly impact blood sugar management and overall health for individuals with diabetes. The diet emphasizes balanced nutrition, portion control, and the selection of nutrient-dense foods, with a particular focus on managing carbohydrate intake. By incorporating a variety of food groups and minimizing processed options, individuals can tailor their meal plans to better meet their health needs.
Practical meal planning is essential for adhering to the ADA guidelines. Utilizing tools such as grocery lists and portion size aids can help streamline the process, making healthy choices more accessible. The Diabetes Plate Method further simplifies meal assembly, promoting a balanced intake of vegetables, proteins, and carbohydrates, which is crucial for effective diabetes management.
Hydration also plays a pivotal role in maintaining health while managing diabetes. Adequate fluid intake, primarily through water and unsweetened beverages, supports metabolic processes and helps prevent complications associated with dehydration. By prioritizing hydration and making informed food choices, individuals can take proactive steps toward better health outcomes.
In conclusion, the ADA Diabetic Diet provides a comprehensive framework for managing diabetes through mindful eating and hydration strategies. By embracing these principles, individuals can not only enhance their blood glucose control but also improve their overall well-being, empowering them to lead healthier lives.
Frequently Asked Questions
What is the ADA diabetic diet designed to achieve?
The ADA diabetic diet is crafted to support healthy eating patterns while effectively managing blood sugar levels through balanced nutrition, portion control, and the selection of nutrient-rich foods.
What are the fundamental principles of the ADA diabetic diet?
The fundamental principles include balanced nutrition, portion control, and managing carbohydrate intake, as carbohydrates significantly affect blood glucose levels.
What types of foods should be included in the ADA diabetic diet?
The diet encourages a diverse range of foods, including whole grains, fruits, vegetables, lean proteins, and healthy fats.
What foods should be minimized or avoided on the ADA diabetic diet?
Processed foods, added sugars, and saturated fats should be minimized in the ADA diabetic diet.
What is the compliance rate of patients with sugar-related conditions following the ADA guidelines?
Only 36.5% of patients with sugar-related conditions comply with the ADA guidelines, indicating a need for personalized nutrition approaches.
Why is it important to tailor dietary plans for diabetic patients?
Tailored dietary plans enhance adherence to the diet and promote better health outcomes, particularly in blood sugar control, which is vital for effective diabetes management.
What is essential for effective meal planning on the ADA diet?
Effective meal planning requires careful selection of items that adhere to dietary principles while accommodating individual preferences and lifestyles.
How can individuals estimate portion sizes while meal planning?
Hand measurements can be used: palm for 3 ounces of meat, thumb for 1 ounce of cheese, fist for 1 cup of fruit, cupped hand for 1-2 ounces of nuts, thumb tip for 1 tablespoon, and fingertip for 1 teaspoon.
What tools can assist with meal planning on the ADA diet?
Tools such as grocery lists, meal prep containers, and tracking apps can help organize food purchases and streamline the meal planning process.
What is the Very Low Carbohydrate Meal Pattern, and how does it relate to diabetes management?
The Very Low Carbohydrate Meal Pattern limits carbohydrate intake to 20–50g of non-fiber carbohydrates per day, promoting health improvements and has shown effectiveness in reducing A1C levels and supporting weight management.
How does meal timing and composition impact blood sugar management?
Meal timing and composition are crucial for managing blood sugar levels, as evidenced by studies indicating that the way meals are consumed can affect incremental blood glucose responses.