Overview
The GMI to A1C chart is an effective tool for diabetes management as it allows individuals to monitor and adjust their blood sugar levels based on real-time data from continuous glucose monitoring systems. The article emphasizes that understanding the relationship between GMI and A1C can enhance treatment strategies by providing insights into daily glucose fluctuations and enabling personalized adjustments to diet, exercise, and medication.
Introduction
The Glucose Management Indicator (GMI) has emerged as a pivotal tool in the ongoing battle against diabetes, particularly for those managing type 2 diabetes. By providing a calculated estimate of average glucose levels over time through continuous glucose monitoring (CGM), GMI offers a more nuanced perspective on glucose fluctuations compared to traditional metrics.
This article delves into the significance of GMI in diabetes management, exploring its advantages, limitations, and practical applications. It highlights the differences between GMI and the well-established HbA1c metric, the role of Time in Range (TIR) in enhancing patient outcomes, and the importance of interpreting GMI readings in the context of individual health profiles.
Through a comprehensive examination of these elements, the article aims to equip readers with valuable insights for optimizing diabetes care and improving overall health outcomes.
Understanding the Glucose Management Indicator (GMI)
The Glucose Management Indicator (GMI) is crucial for understanding the gmi to a1c chart, as it signifies a computed value that approximates a person’s average sugar levels over time, utilizing data from continuous sugar monitoring (CGM) systems. This indicator is particularly beneficial for patients with type 2 sugar intolerance, as it offers a more dynamic view of sugar level fluctuations compared to traditional metrics, allowing for timely adjustments in management strategies. Understanding the GMI to A1C chart is essential for making informed decisions about diet, exercise, and medication.
Recent advancements in CGM technology have made it possible to obtain frequent interstitial readings without the need for calibration, thereby enhancing the reliability of GMI as a reflection of glycaemic control. Notably, a study highlighted that the gmi to a1c chart may better correlate with time in range (TIR), underscoring its relevance in both routine monitoring and clinical decision-making. Furthermore, in the context of awareness regarding blood sugar, it’s important to note that from 2017-2020, only 20.9% of Hispanic adults were aware of their prediabetes, emphasizing the need for improved education on glucose management.
Additionally, Viral N Shah et al. concluded that GMI may be a better reflection of glycaemic control in early pregnancy, indicating its broader applicability. As such, the GMI to A1C chart serves as an essential tool for enhancing the management of blood sugar levels and optimizing outcomes for individuals, despite the complexities involved in interpreting CGM data.
Incorporating insights from case studies, like those illustrating success stories at the Integrative Wellness Center, can further emphasize how personalized care strategies have reversed type 2 health issues. Furthermore, comprehending the risks of conventional therapies and the function of insulin resistance is crucial for individuals pursuing thorough management strategies. Understanding these factors is crucial for optimizing the use of CGM data and improving patient outcomes.
Comparing GMI and HbA1c: Key Differences and Similarities
GMI (Glucose Management Indicator) and HbA1c (Hemoglobin A1c) are both crucial metrics in evaluating sugar control for individuals managing diabetes, yet they differ significantly in their methodologies and implications. HbA1c reflects the average blood sugar levels over the preceding two to three months, providing a long-term view of glycemic control. In contrast, GMI provides a more immediate viewpoint derived from continuous monitoring, capturing real-time fluctuations of sugar levels.
This capability makes GMI particularly valuable for identifying daily variations in blood sugar, which may not be adequately represented by HbA1c alone. Research indicates that an MG (mean sugar) level of approximately 8.6 mmol/l (155 mg/dl) is equivalent to an HbA1c of less than 53 mmol/mol (less than 7.0%). Understanding the functional differences between these two indicators enables patients to leverage both GMI and the GMI to A1C chart for a comprehensive diabetes management strategy.
Recent studies have highlighted significant differences in control indicators among subgroups based on Δ GMI-HbA1c values, particularly in the coefficient of variation and time above range, underscoring the importance of utilizing both metrics to monitor and adjust treatment plans effectively. As noted by G.S., ‘All authors have read and agreed to the published version of the manuscript,’ which reflects the collaborative effort in the research process. Additionally, the case study titled ‘Explanations and Interpretations’ discusses potential clarifications for the observed deviations in the relationships between MG, TIR, and HbA1c, considering factors such as data completeness and erythrocyte lifespan, thereby providing valuable insights into the complexities of control metrics.
Applying GMI in Diabetes Management: Practical Insights
To effectively utilize Glucose Management Indicator (GMI) in diabetes care, individuals should consistently track their sugar levels with a continuous monitoring (CGM) device. Examining the GMI to A1C chart enables individuals to identify patterns in their blood sugar responses to various foods, physical activities, and medications. This critical insight can inform necessary adjustments in diet, exercise regimens, and medication dosing.
For example, a randomized clinical trial titled Effect of Continuous Glucose Monitoring on Glycemic Control in Adolescents and Young Adults With Type 1 Diabetes demonstrated that CGM led to a statistically significant reduction in hemoglobin A1c levels by 0.37% when compared to standard blood glucose monitoring methods, underscoring the effectiveness of CGM in enhancing glycemic control in younger individuals. However, as individuals approach their A1C target, achieving further improvements can become increasingly challenging, highlighting the importance of ongoing monitoring and adjustments. Furthermore, establishing specific goals based on GMI readings not only serves to motivate individuals but also promotes adherence to management plans, ultimately improving overall health outcomes.
Recent advancements in CGM technology, as noted by Kovatchev BP, indicate that in silico preclinical trials are paving the way for better control mechanisms in diabetes management. These advancements are anticipated to empower individuals further, with increasing accuracy expected to enhance clinical applications and facilitate more personalized management strategies. The growing emphasis on utilizing CGM data suggests a trend towards greater clinical adoption, reinforcing the importance of monitoring trends using the GMI to A1C chart.
The Role of Time in Range (TIR) in Managing Diabetes with GMI
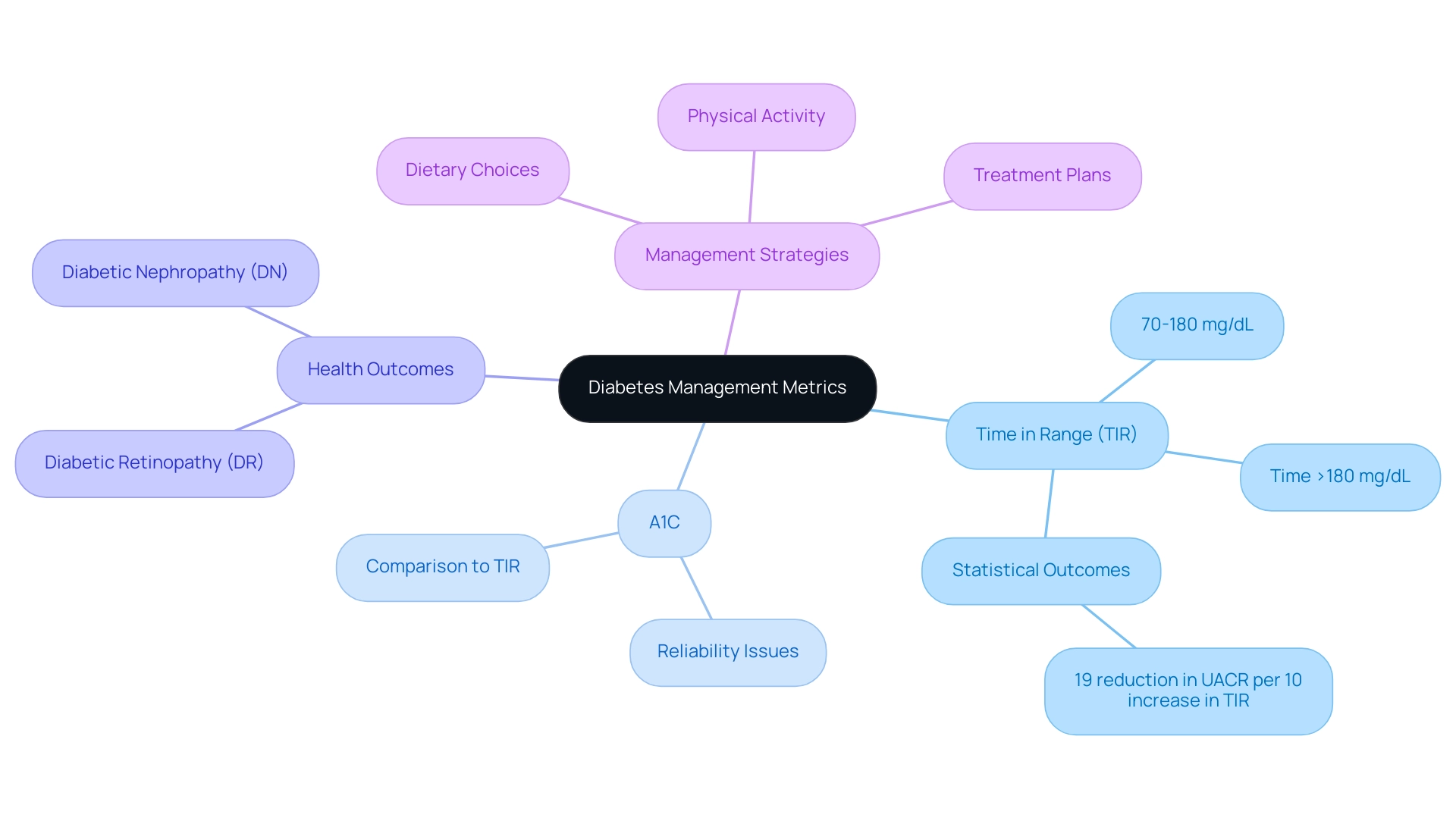
Time in Range (TIR) is an essential metric that defines the percentage of time a patient’s sugar levels remain within the target range, typically set between 70 and 180 mg/dL. This measurement, when evaluated alongside the gmi to a1c chart, provides profound insights into daily glucose control. A higher TIR percentage suggests improved management of the condition, correlating with a reduced risk of complications such as diabetic nephropathy (DN) and retinopathy (DR).
For instance, one patient, M.L., who struggled with blood sugar issues for 10 years, experienced a remarkable transformation after engaging with the Integrative Wellness Center. M.L. shared, ‘When I started this program, the Doctor gave great personal attention and care in helping fix my condition.’
Starting with an A1C of 9.1, M.L. achieved an A1C of 5.7 after just eight months, alongside significant weight loss and improved fasting glucose levels. Recent studies have shown that a 10% increase in TIR is associated with significant improvements in health outcomes, including a 19% reduction in urinary albumin-to-creatinine ratio (UACR) per 10% increase in TIR.
Notably, the gmi to a1c chart reveals that CGM-derived TIR has been found to be comparable to A1C in predicting DN and DR, underscoring its significance in diabetes management. Additionally, several organizations have published consensus statements on specific CGM metrics for assessing hyperglycemia, hypoglycemia, and glycemic variability, highlighting the importance of metrics like:
- time >180 mg/dL
- time in range of 70-180 mg/dL
To enhance their TIR, individuals are encouraged to adopt informed dietary choices, maintain regular physical activity, and meticulously follow their prescribed treatment plans.
As David Rodbard noted, ‘Numerous studies have shown that there are a wide range of possible mean glucose levels for a given A1C level, meaning that for some individuals, A1C may not be a reliable indicator of glucose control.’ By consistently monitoring both GMI and TIR, patients can utilize the gmi to a1c chart to take proactive measures to optimize their management of the condition, thus improving their overall health and well-being. This holistic approach not only aids in managing diabetes but also alleviates the worry associated with potential complications.
Evaluating the Accuracy of GMI in Estimating A1C Levels
The GMI to A1C chart serves as a useful tool for monitoring sugar levels; however, it is crucial to acknowledge its limitations in estimating A1C levels. Recent research has shown that while GMI can often provide a reliable estimate of A1C, individual factors such as hemoglobin disorders may significantly impact its accuracy. A notable study revealed that 28% of participants exhibited clinically significant discordance between their GMI readings and laboratory HbA1c results.
This discrepancy suggests that variability and inaccuracy in continuous glucose monitoring (CGM) readings could further contribute to the differences observed. Additionally, it is expected that averaging estimated A1C (eAG A1c) and CGM (eAG CGM) data can reduce error when CGM data is available for fewer than 26 days, highlighting the importance of context in interpreting GMI readings. Furthermore, the original equations for ADAG and DCCT do not fully align with GMI, which underscores foundational differences in how these measures are derived.
As such, it is advisable for patients to regard the GMI to A1C chart as a complementary measure to A1C rather than a complete substitute. Regular consultations with healthcare providers are essential for accurately interpreting both GMI and A1C levels, which can lead to more effective management of the condition. As stated by V.T., the guarantor of a recent study, they had full access to all data and take responsibility for the integrity of the data and its analysis, underscoring the importance of accurate readings in managing diabetes.
The complexity of predicting GMI accuracy for individuals versus populations is further illustrated by the case study titled ‘Accuracy of GMI in Individual Patients,’ which emphasizes the need for caution when relying solely on GMI.
Conclusion
The Glucose Management Indicator (GMI) represents a significant advancement in the management of diabetes, particularly for individuals with type 2 diabetes. By providing real-time insights into glucose levels through continuous glucose monitoring (CGM), GMI enhances the ability to make informed decisions regarding diet, exercise, and medication. It stands in contrast to traditional metrics like HbA1c, offering a more dynamic view of glucose fluctuations that can lead to timely adjustments in management strategies.
Understanding the nuances of GMI, including its strengths and limitations, is essential for optimizing diabetes care. The correlation between GMI and Time in Range (TIR) underscores its importance in achieving better health outcomes. Higher TIR percentages indicate improved glucose control, which is crucial in minimizing the risk of complications associated with diabetes. Personal success stories highlight the transformative potential of integrating GMI into diabetes management, demonstrating that tailored approaches can lead to significant improvements in patient health.
While GMI is a valuable tool, it is important to acknowledge its limitations in estimating A1C levels. Variability in CGM readings and individual health factors can affect accuracy, reinforcing the necessity of using GMI as a complementary measure rather than a standalone solution. Regular consultations with healthcare providers will ensure that both GMI and A1C readings are interpreted effectively, fostering a comprehensive approach to diabetes management.
In summary, the integration of GMI into diabetes care represents a promising avenue for enhancing patient outcomes. By embracing continuous glucose monitoring and understanding the interplay between GMI and TIR, individuals can take proactive steps towards better health, ultimately improving their quality of life in the face of diabetes.
Frequently Asked Questions
What is the Glucose Management Indicator (GMI)?
The GMI is a computed value that approximates a person’s average sugar levels over time, utilizing data from continuous glucose monitoring (CGM) systems.
Why is GMI important for patients with type 2 sugar intolerance?
GMI offers a more dynamic view of sugar level fluctuations compared to traditional metrics, allowing for timely adjustments in management strategies.
How does the GMI to A1C chart assist in diabetes management?
Understanding the GMI to A1C chart is essential for making informed decisions about diet, exercise, and medication.
What advancements have been made in CGM technology?
Recent advancements in CGM technology allow for frequent interstitial readings without the need for calibration, enhancing the reliability of GMI as a reflection of glycaemic control.
How does GMI correlate with time in range (TIR)?
Studies suggest that the GMI to A1C chart may better correlate with time in range (TIR), highlighting its relevance in routine monitoring and clinical decision-making.
What awareness issues exist regarding prediabetes among Hispanic adults?
From 2017-2020, only 20.9% of Hispanic adults were aware of their prediabetes, indicating a need for improved education on glucose management.
In what context is GMI particularly useful?
GMI may be a better reflection of glycaemic control in early pregnancy, indicating its broader applicability.
How can personalized care strategies impact type 2 health issues?
Insights from case studies, such as those at the Integrative Wellness Center, illustrate how personalized care strategies have successfully reversed type 2 health issues.
Why is it important to understand the risks of conventional therapies and insulin resistance?
Understanding these factors is crucial for individuals pursuing thorough management strategies for diabetes.
What are the key differences between GMI and HbA1c?
HbA1c reflects average blood sugar levels over the preceding two to three months, while GMI provides a more immediate viewpoint from continuous monitoring, capturing real-time fluctuations in sugar levels.
How can both GMI and HbA1c be utilized in diabetes management?
Leveraging both GMI and the GMI to A1C chart allows for a comprehensive diabetes management strategy by providing insights into both immediate and long-term glycemic control.