Introduction
Navigating the complexities of diabetes management requires a thorough understanding of key indicators such as the A1C test, which plays a pivotal role in assessing long-term glucose control. This article delves into the significance of A1C levels, exploring what different results mean for individual health and the necessary lifestyle changes to manage these levels effectively.
It also highlights the importance of medication when lifestyle adjustments alone are insufficient, as well as the critical role of regular monitoring in maintaining optimal health outcomes.
Furthermore, the establishment of a supportive care team is emphasized as a vital component in empowering individuals to take charge of their diabetes management. By addressing these facets, readers will gain valuable insights into creating a personalized approach that fosters better health and well-being.
Understanding the A1C Test: Importance and Functionality
The A1C test is a crucial measure of long-term glucose control, particularly when monitoring levels such as 6.6 a1c, which quantifies the percentage of glycated hemoglobin in the blood. This essential indicator offers insights into a person’s average blood sugar readings over the past two to three months. For individuals without the condition, a normal A1C level is below 5.7%, while an A1C of 6.6 a1c or higher indicates the disease.
Regular testing, typically every three to six months, is essential for evaluating the effectiveness of management strategies for the condition, particularly within a holistic framework that addresses root causes and alleviates the anxiety surrounding potential complications of the disease. By re-examining the origin of the condition, we can create a personalized regimen that empowers patient health. Recent statistics indicate that the baseline mean A1C for individuals with newly diagnosed condition stands at 6.8%, highlighting the significance of achieving a target of 6.6 a1c in monitoring the illness and guiding integrative treatment plans.
Additionally, the mean baseline fasting plasma glucose (FPG) level for individuals with this condition was recorded at 5.4 mmol/l, providing further context for management. The stability in blood sugar condition prevalence, unchanged from 2017 to 2023, underscores the ongoing need for effective 6.6 a1c monitoring as a critical component of comprehensive care. As healthcare professionals observe, the combination of A1C and OGTT tests improves the prediction of progression to the condition among those with glucose intolerance, reaffirming the A1C test’s critical role in guiding personalized treatment strategies and empowering patient health.
What Does a 6.6 A1C Mean for Your Health?
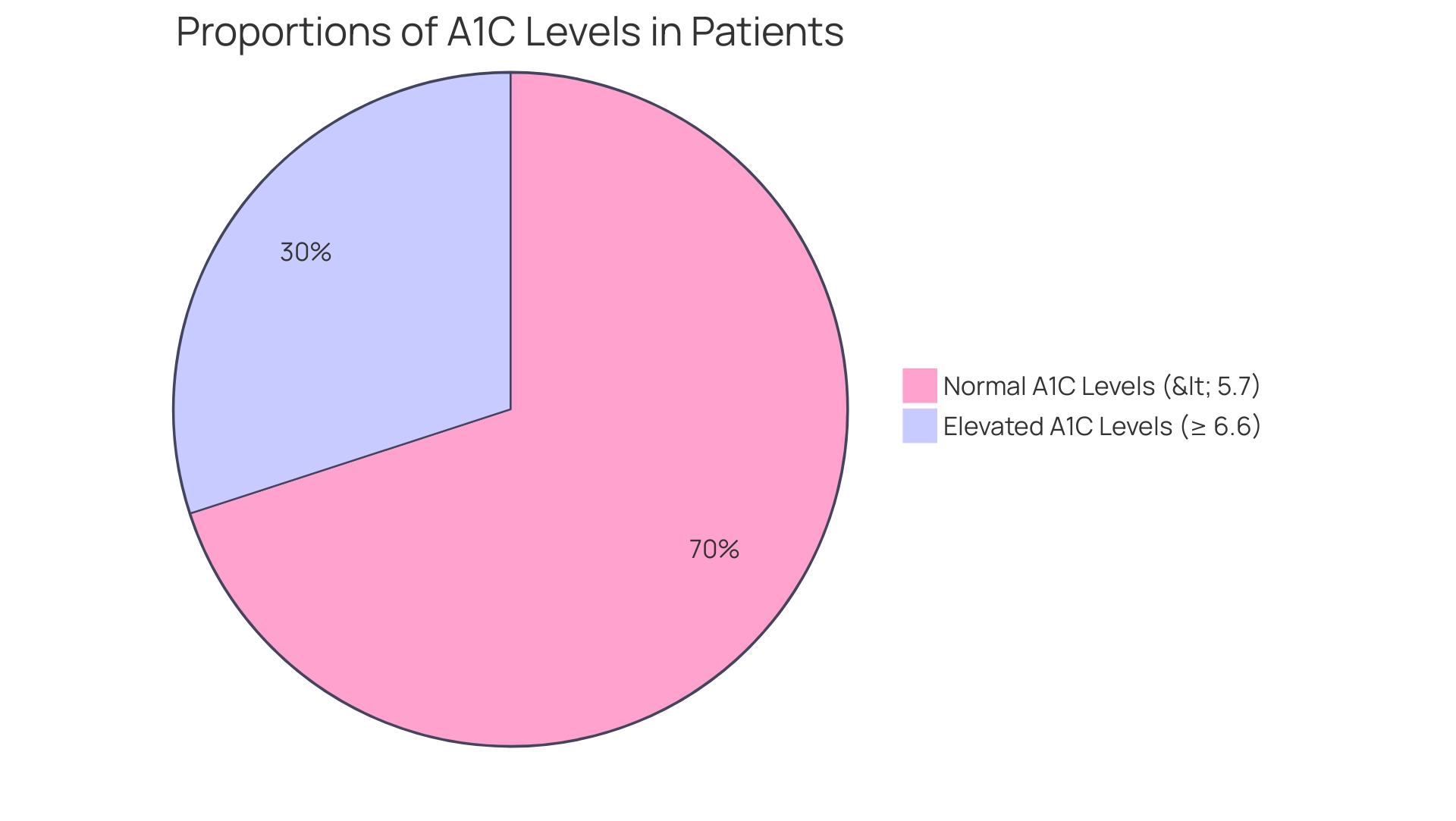
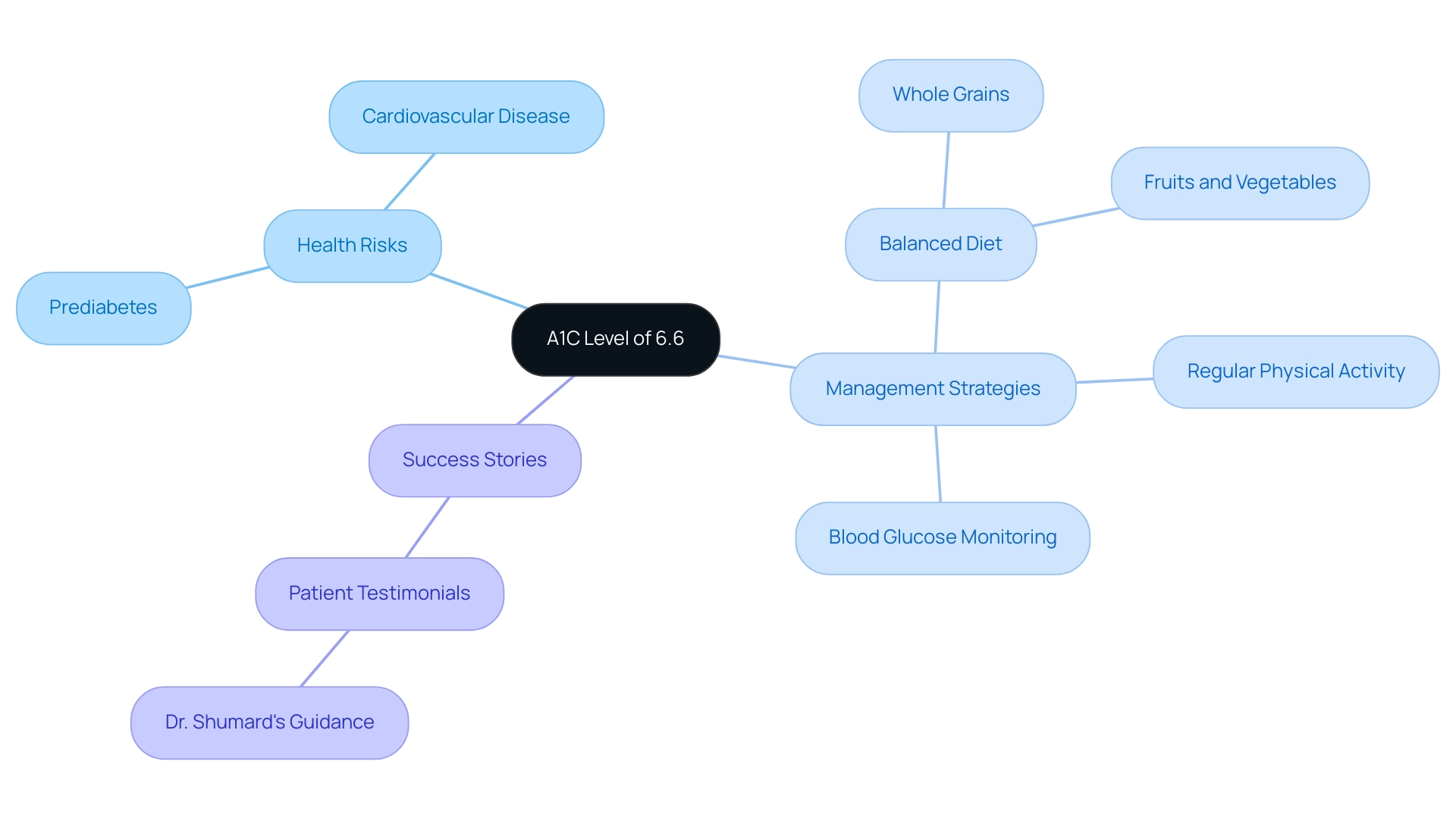
An A1C measurement of 6.6 a1c indicates that your average blood glucose values have exceeded the normal range, categorizing you as prediabetic. This stage is linked to a heightened risk of advancing to type 2 blood sugar disorder and associated complications, including cardiovascular disease. Recent studies emphasize the implications of maintaining an A1C level in this range, particularly noting that individuals with A1C levels between 6.5% and 7.0% face significant risks to their well-being.
According to public health research, the increase of this condition as a public health issue necessitates efficient identification of risk, illustrating the need for awareness and proactive management. Additionally, Shimazaki notes that ‘the combination of A1C and OGTT enables more precise prediction of progression to diabetes in those with glucose intolerance,’ emphasizing the importance of accurate testing. It is also important to understand that red blood cells regenerate roughly every three months, which means that A1C readings reflect your average blood glucose over that period.
To effectively manage a 6.6 a1c level, it is crucial to adopt healthy lifestyle changes, which include:
- Following a balanced diet rich in whole grains, fruits, and vegetables
- Engaging in regular physical activity
- Consistently monitoring blood glucose levels
Transformative patient success stories from the Integrative Wellness Center highlight how Dr. Shumard’s personalized care has empowered individuals to reverse type 2 conditions through tailored treatment plans. For instance, one patient shared, ‘Thanks to Dr. Shumard’s guidance, I’ve not only lowered my A1C but also regained my energy and confidence.’
Moreover, referencing the case study titled ‘Public Health Implications of A1C Thresholds’ underscores the necessity of identifying diabetes risk and selecting specific A1C thresholds based on likely interventions. Collaborating closely with healthcare professionals to formulate a personalized management plan is advisable. This plan may include medications if necessary, as timely interventions can mitigate risks associated with prediabetes.
Grasping the significance of a 6.6 a1c reading enables individuals to take proactive measures towards better wellness results. We encourage you to explore more success stories and testimonials on our website to see how others have improved their well-being.
Lifestyle Changes to Lower Your A1C
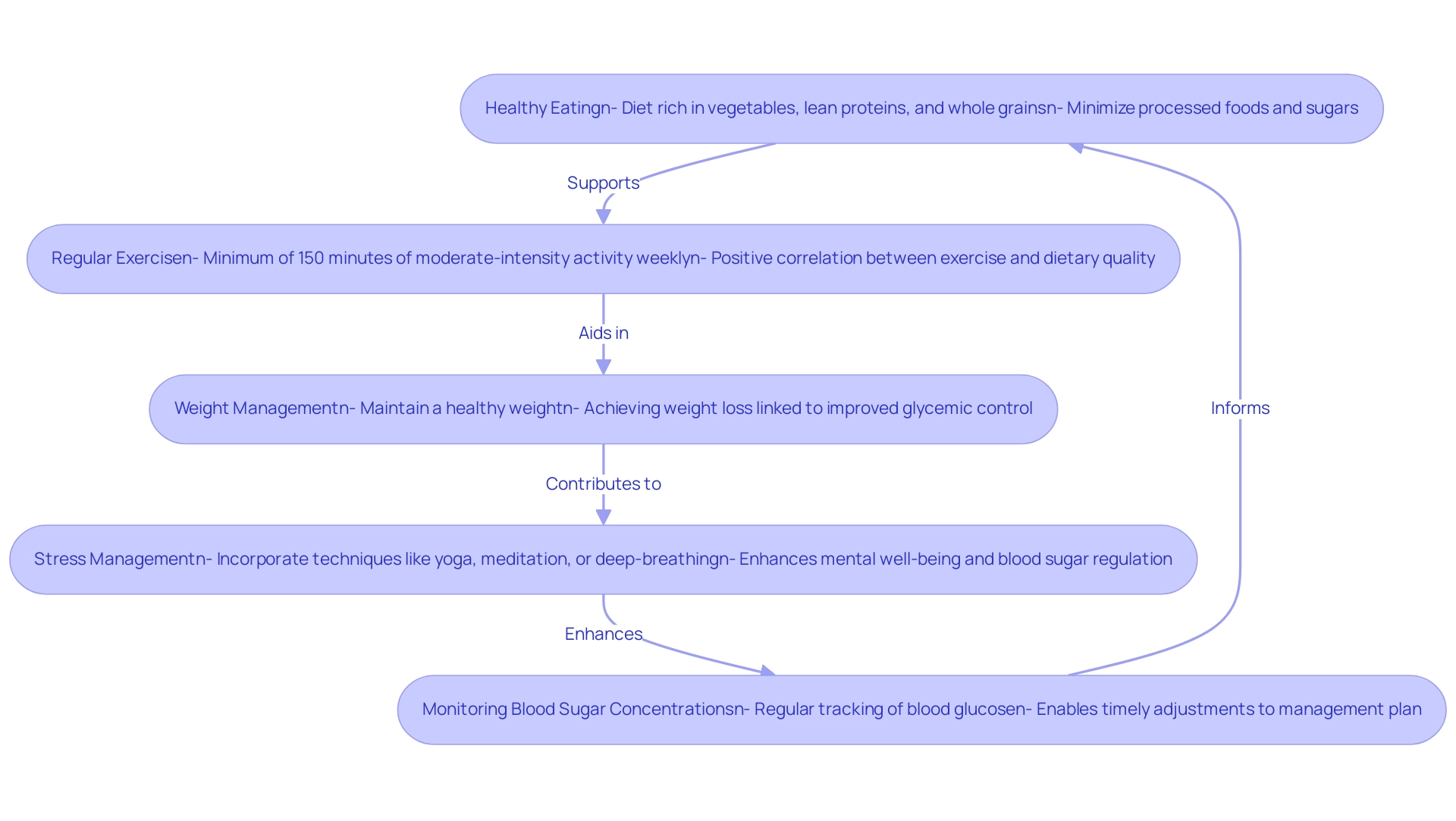
To effectively lower your A1C levels to 6.6 a1c and promote overall well-being, it is essential to adopt a comprehensive approach that combines dietary adjustments with lifestyle changes. By addressing the root causes of your condition, you can also alleviate the anxiety that often accompanies concerns about potential complications. Consider the following recommendations, grounded in the principles of integrative wellness:
-
Healthy Eating: Prioritize a diet rich in vegetables, lean proteins, and whole grains while minimizing processed foods and sugars. This dietary approach not only helps regulate blood sugar but may also improve overall health outcomes. As Dr. Kirsten S. Dorans notes,
This dietary approach may be an option for people with or at high risk of T2D to improve glycemic and other markers…
Notably, the mean healthy diet score is 3.52, underscoring the importance of healthier food choices in reversing diabetes.
-
Regular Exercise: Strive for a minimum of 150 minutes of moderate-intensity aerobic activity each week, such as brisk walking or swimming. Research indicates that participants who engage in regular physical activity are more likely to achieve a healthy food score above the median, particularly among women, highlighting a positive correlation between exercise and dietary quality.
This integration of physical activity into your routine is vital for managing diabetes effectively.
-
Weight Management: Maintaining a healthy weight can significantly influence levels, including a target of 6.6 a1c. Achieving weight loss, when necessary, is linked to improved glycemic control and overall well-being, contributing to the holistic management of diabetes.
-
Stress Management: Incorporate stress-reduction techniques into your routine, such as yoga, meditation, or deep-breathing exercises. These practices enhance mental well-being and contribute to better blood sugar regulation, empowering you to take control of your health. By managing stress, you can also reduce anxiety related to your condition, which is essential for a holistic approach.
-
Monitoring Blood Sugar Concentrations: Regular tracking of blood glucose concentrations is crucial for understanding how dietary and lifestyle changes impact your levels, particularly your 6.6 a1c. This ongoing assessment enables timely adjustments to your management plan. It is important to note that while studies often depend on self-reported measures, which can be flawed, the findings suggest that objective assessments are essential for accurately tracking lifestyle changes and their impacts on A1C values, particularly when considering the target of 6.6 a1c.
For instance, recent studies highlight small yet significant differences in healthy food scores, correlating with decreases in HbA1c among women. Therefore, adopting these modifications not only aids in lowering A1C but also promotes enhanced overall well-being through a holistic approach to managing the condition, starting with re-examining the source of your health issue.
Medications and Their Role in Managing A1C
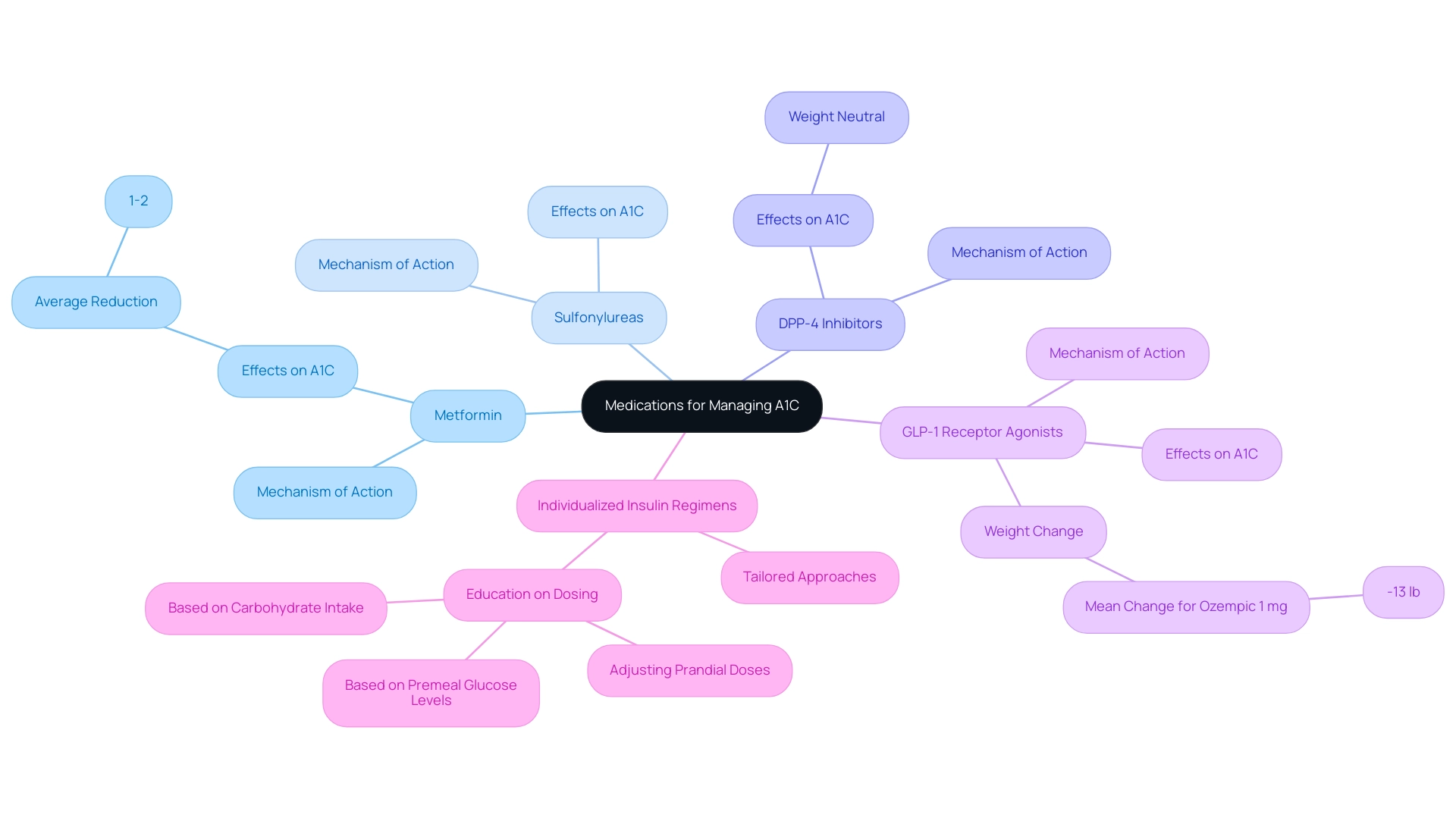
While lifestyle changes are crucial for managing Type 2 condition, they may not always be enough to achieve an optimal 6.6 a1c. In such scenarios, medications become crucial in reaching target levels of 6.6 a1c. The common classes of diabetes medications include:
- Metformin: Acknowledged as the primary option for treatment, Metformin effectively reduces blood sugar amounts and improves insulin sensitivity. Recent studies indicate that it can lead to significant reductions in A1C values, particularly in patients with a 6.6 a1c, where average decreases of about 1-2% are observed.
- Sulfonylureas: These medications work by stimulating the pancreas to produce additional insulin, thus aiding in blood sugar regulation.
- DPP-4 inhibitors: Recognized for their capacity to lower blood sugar amounts without resulting in weight gain, these agents are advantageous for numerous patients.
- GLP-1 receptor agonists: These medications not only help lower blood sugar but also promote weight loss by slowing digestion, with a mean change in weight for Ozempic 1 mg reported at -13 lb.
Individualized insulin regimens, particularly for patients with Type 1 diabetes, demonstrate how tailored approaches can enhance glycemic control, emphasizing the need for personalized treatment plans.
As indicated in recent guidelines, effective management strategies involve education on modifying prandial doses according to carbohydrate consumption and premeal glucose readings. It is essential for patients to consult with their healthcare providers to explore medication options that align with their specific wellness profiles and management goals. For more information about Lilly’s privacy practices, please view the Privacy Statement.
The Importance of Regular Monitoring
Consistent monitoring of blood glucose readings and maintaining a 6.6 A1C is crucial for effective management of diabetes, particularly given that the diagnosed diabetes prevalence stands at 7.8%. This practice allows individuals to assess their progress, identify the effect of lifestyle changes on their well-being, and make informed adjustments to their management strategies. The American Diabetes Association Professional Practice Committee recommends that A1C readings, particularly aiming for a 6.6 A1C, should be monitored every three to six months, adjusted to personal health situations.
Beyond periodic A1C tests, daily blood glucose monitoring offers immediate insights into how specific foods, physical activities, and medications affect blood sugar. For pregnant individuals, it’s essential to adopt specific strategies such as:
- Meal planning
- Regular physical activity
- Close monitoring of blood sugar levels to prevent gestational complications
Incorporating a holistic approach to managing the condition, as highlighted at the Integrative Wellness Center, can further empower patients by addressing the underlying causes and fostering a comprehensive lifestyle strategy.
This includes understanding the dangers of traditional treatments, which may not address root causes and can sometimes lead to adverse effects. Maintaining a comprehensive log of these readings not only aids in self-awareness but also fosters constructive discussions with healthcare providers, ultimately enhancing overall diabetes management outcomes. Recent statistical analyses emphasize the importance of this practice, revealing a strong correlation between time in range (TIR) and 6.6 A1C values, with a target of 70% TIR closely aligning with a 6.6 A1C.
Case studies from landmark trials such as ACCORD, ADVANCE, and VADT highlight the importance of regular monitoring, demonstrating that lower A1C levels, such as 6.6 A1C, are associated with reduced complications, although caution is warranted due to potential risks noted in certain studies. By reassessing the origin of your condition, individuals can embrace a more effective and comprehensive approach for managing their well-being.
Building a Supportive Care Team
Forming a supportive care team is crucial for individuals managing their condition, as it facilitates a comprehensive approach to well-being aimed at empowering patients to remove anxiety over potential complications and discover new peace in life. This team typically includes:
- Primary Care Physician: Responsible for overseeing overall well-being and coordinating care among specialists, ensuring that all aspects of wellness are addressed.
- Endocrinologist: A specialist in blood sugar disorders who provides advanced insights and treatment options tailored to individual needs, helping patients feel more secure in their management plan.
- Dietitian/Nutritionist: Responsible for developing customized meal plans that support wellness objectives and nutritional needs, directly enhancing confidence in dietary choices.
- Diabetes Educator: Offers essential education and resources that empower individuals with effective self-management strategies, reducing anxiety about their condition.
- Mental Health Professional: Addresses the emotional and psychological challenges associated with managing this condition, enhancing overall well-being and fostering a sense of peace.
Research indicates that interprofessional collaborative practice (ICP), which involves multiple health professions working together, is associated with significant improvements in clinical outcomes for patients with diabetes-related conditions.
A systematic review and meta-analysis demonstrated that such collaborative efforts led to an average reduction in HbA1c levels of -1.73% after 12 months, especially for patients with baseline levels of 9 or higher, aligning with the target of 6.6 a1c. As Mohammed Ali stated, ‘Collaborative care is crucial in managing this condition effectively, as it brings together diverse expertise to address the multifaceted needs of patients.’ This collaborative approach ensures comprehensive management of all health aspects, ultimately leading to improved health outcomes, enhanced quality of life, and peace of mind for individuals living with diabetes.
Conclusion
Understanding and managing A1C levels is vital for anyone navigating the complexities of diabetes. The A1C test serves as a key indicator of long-term glucose control, making it essential for evaluating individual health. An A1C level of 6.6% signals a prediabetic state, highlighting the urgency for proactive lifestyle changes and potential medical interventions. Adopting a healthy diet, engaging in regular exercise, managing weight, and incorporating stress-reduction techniques are all crucial steps to effectively lower A1C levels.
While lifestyle modifications play a significant role, they may not always be sufficient. Medications can provide necessary support in achieving target A1C goals, underscoring the importance of a personalized treatment plan developed in collaboration with healthcare providers. Regular monitoring of blood glucose and A1C levels is equally important, enabling individuals to track their progress and make informed decisions about their health.
Building a supportive care team enhances this journey, as it fosters a holistic approach to diabetes management. By involving various healthcare professionals, individuals can receive comprehensive care tailored to their unique needs. This collaborative effort not only improves clinical outcomes but also empowers patients to take control of their health, reducing anxiety and enhancing their quality of life.
In conclusion, a thorough understanding of A1C levels, combined with proactive lifestyle changes, medication when necessary, and a robust support network, can significantly improve health outcomes for individuals with diabetes. Taking these steps leads to a more empowered and healthier life, emphasizing the importance of a personalized and comprehensive approach to diabetes management.
Frequently Asked Questions
What is the A1C test and why is it important?
The A1C test measures long-term glucose control by quantifying the percentage of glycated hemoglobin in the blood, providing insights into a person’s average blood sugar readings over the past two to three months. It is crucial for monitoring conditions such as prediabetes and diabetes.
What does an A1C level of 6.6 indicate?
An A1C level of 6.6 indicates that average blood glucose values have exceeded the normal range, categorizing the individual as prediabetic, which is associated with an increased risk of developing type 2 diabetes and related complications.
What are the normal A1C levels?
For individuals without diabetes, a normal A1C level is below 5.7%. An A1C of 6.6 or higher indicates the presence of diabetes.
How often should A1C testing be done?
Regular A1C testing should be conducted every three to six months to evaluate the effectiveness of management strategies for diabetes or prediabetes.
What lifestyle changes can help manage a 6.6 A1C level?
To manage a 6.6 A1C level, individuals should adopt healthy lifestyle changes, including following a balanced diet rich in whole grains, fruits, and vegetables, engaging in regular physical activity, and consistently monitoring blood glucose levels.
What is the significance of the combination of A1C and OGTT tests?
The combination of A1C and Oral Glucose Tolerance Test (OGTT) improves the prediction of progression to diabetes among individuals with glucose intolerance, highlighting the importance of accurate testing in managing health.
What is the average baseline A1C level for newly diagnosed individuals?
The baseline mean A1C for individuals newly diagnosed with diabetes is 6.8%, making it significant to achieve a target of 6.6 for effective monitoring and treatment planning.
How can individuals take proactive measures regarding their A1C levels?
Individuals can take proactive measures by understanding the significance of their A1C readings, adopting healthy lifestyle changes, collaborating with healthcare professionals for personalized management plans, and considering timely interventions if necessary.