Introduction
The Glucose Management Indicator (GMI) is emerging as a significant tool in the realm of diabetes management, offering a contemporary approach to tracking glucose levels. By utilizing continuous glucose monitoring (CGM) data, GMI provides a real-time perspective on an individual’s glycemic control, allowing healthcare providers to make timely and informed adjustments to treatment plans. This innovative metric not only enhances patient engagement and understanding of their condition but also addresses the complexities of diabetes management, including the challenges posed by traditional measures such as HbA1c.
As the landscape of diabetes care continues to evolve, the role of GMI becomes increasingly critical, promising to empower patients and improve health outcomes through a more nuanced understanding of their glucose patterns. This article delves into the intricacies of GMI, comparing it to established metrics, exploring its practical applications, and evaluating its reliability, while also highlighting the future advancements that may reshape diabetes management strategies.
What is the Glucose Management Indicator (GMI)?
The Glucose Management Indicator (GMI diabetes) is a calculated metric that reflects an individual’s average glucose levels over time, typically derived from continuous glucose monitoring (CGM) data. Unlike conventional methods of glycemic control, GMI provides a more prompt evaluation, enabling healthcare professionals to adjust care strategies with greater accuracy. This holistic method of diabetes care not only addresses the root causes but also aims to eliminate the anxiety associated with the potential complications of diabetes, empowering patients to take control of their health.
Current statistics reveal that in a study involving the Libre Pro system:
- 43% of participants exhibited an absolute difference of ≥0.5 percentage points
- 18% showed a difference greater than 1.0 percentage points
These differences are significant as they can indicate varying levels of glycemic control, directly impacting patient outcomes. Such data highlights the critical role of GMI diabetes in effectively monitoring sugar levels.
R.N. Aurora from the American Academy of Sleep Medicine emphasizes that GMI diabetes is pivotal for enhancing patient understanding of their glucose management, thereby fostering greater engagement and adherence to treatment protocols. Furthermore, understanding the relationship between glycosylated hemoglobin, time-in-range, and glycemic variability is essential, as GMI helps interpret these factors, ultimately contributing to improved health outcomes.
However, despite the benefits of GMI, challenges such as insurance coverage for CGM systems pose significant barriers to access. A recent study highlighted that most patients face complexities with claims processed as durable medical equipment, which can hinder the uptake of essential technology for managing blood sugar. As ongoing monitoring technology develops, the significance of GMI diabetes in blood sugar regulation, particularly within a holistic approach that includes a thorough regimen, is becoming more apparent.
GMI vs. HbA1c: Understanding the Differences and Applications
Both the Glucose Management Indicator (GMI diabetes) and glycated hemoglobin (HbA1c) serve as vital metrics in the management of diabetes, yet they differ significantly in methodology and clinical interpretation. HbA1c reflects an average of blood sugar levels over the preceding two to three months, thus providing a retrospective overview of glycemic control. In contrast, GMI diabetes offers a more immediate and dynamic assessment, derived primarily from continuous glucose monitoring (CGM) data, capturing daily glucose fluctuations.
The real-time nature of GMI diabetes allows healthcare professionals to detect the short-term impacts of dietary changes or adjustments in blood sugar medication. A prospective cohort study conducted from 2017 to 2019 with 144 adults ages 21 to 75 suffering from type 2 conditions and untreated obstructive sleep apnea found that GMI diabetes may be an unreliable measure of glycemic control, showing only moderate correlation with HbA1c and significant variability. Caution is advised in its clinical interpretation.
As noted by Dr. Ana M. Wägner from the Section of Endocrinology and Nutrition, “Understanding these distinctions is crucial for optimizing patient care and making informed treatment decisions.” Recent research highlights the clinical relevance of the differences between these two measures in relation to GMI diabetes, indicating that age and certain hematological parameters can influence their interpretation. The use of both metrics can improve health condition oversight, especially in customizing personal treatment strategies to better address the needs of patients.
Practical Applications of GMI in Diabetes Management
The GMI diabetes plays a crucial role in blood sugar control through various practical applications, particularly at the Integrative Wellness Center, which emphasizes holistic care and education. One important use of GMI is its capacity to inform healthcare providers about the effectiveness of existing treatment regimens, enabling timely adjustments based on observed sugar patterns. For instance, recent studies indicate that 18% of participants using the Libre Pro experienced a deviation exceeding 1.0 percentage points (>11 mmol/mol), highlighting the importance of precise monitoring in treatment optimization.
Moreover, contemporary continuous monitoring sensors offer regular interstitial readings without the necessity for calibration, which underscores the significance of GMI diabetes in current management practices for blood sugar conditions. By actively engaging with GMI diabetes, patients can evaluate how dietary modifications and physical activity affect their blood glucose levels, encouraging a proactive approach to their health and significantly alleviating anxiety about potential complications. This continuous engagement encourages a collaborative approach during regular check-ups, allowing patients and providers to discuss findings and adjust treatment plans accordingly.
Additionally, the Integrative Wellness Center employs specific strategies that utilize GMI diabetes to empower patients, helping them understand their condition better and alleviating fears associated with complications. Guidelines and suggestions for laboratory evaluation in blood sugar control emphasize the significance of incorporating GMI diabetes into clinical practice. As illustrated in the HYPNOS study, which evaluated the effects of positive airway pressure therapy on glycemic control, understanding the nuances of GMI diabetes can lead to more informed treatment adjustments.
As Matthew C. Riddle, a notable journal editor, observes, incorporating such data into clinical practice enriches the dialogue between patients and healthcare professionals, ultimately improving management outcomes.
Evaluating the Accuracy and Reliability of GMI
Research indicates that the Glucose Management Indicator (GMI diabetes) serves as a reliable measure of average sugar levels, often demonstrating a close correlation with traditional HbA1c values. However, its accuracy is affected by various personal factors, including:
- The type of condition
- Treatment regimen
- The performance of the continuous monitoring (CGM) device used
A significant study carried out from 2020 to 2023 involving 26 individuals with type 1 and type 2 conditions indicated that the recorded HbA1c was 0.34% greater than the GMI diabetes derived from CGM, highlighting the importance of comprehending differences between these metrics for effective control.
Additionally, a 2018 study found that 28% of participants experienced clinically significant discordance between GMI diabetes and laboratory HbA1c, defined as a difference of ≥0.5 percentage points. This highlights the variability in GMI accuracy that is not fully explained by known factors affecting HbA1c. Elizabeth Selvin from the Johns Hopkins Bloomberg School of Public Health highlights the importance of using mean CGM glucose alongside laboratory HbA testing to minimize confusion and enhance glycemic control.
As research continues to explore the accuracy and reliability of GMI diabetes, particularly in diverse populations and in those not on insulin therapy, it is crucial for healthcare providers to consider these factors when interpreting GMI diabetes results, especially given the sparse data linking CGM to long-term clinical outcomes.
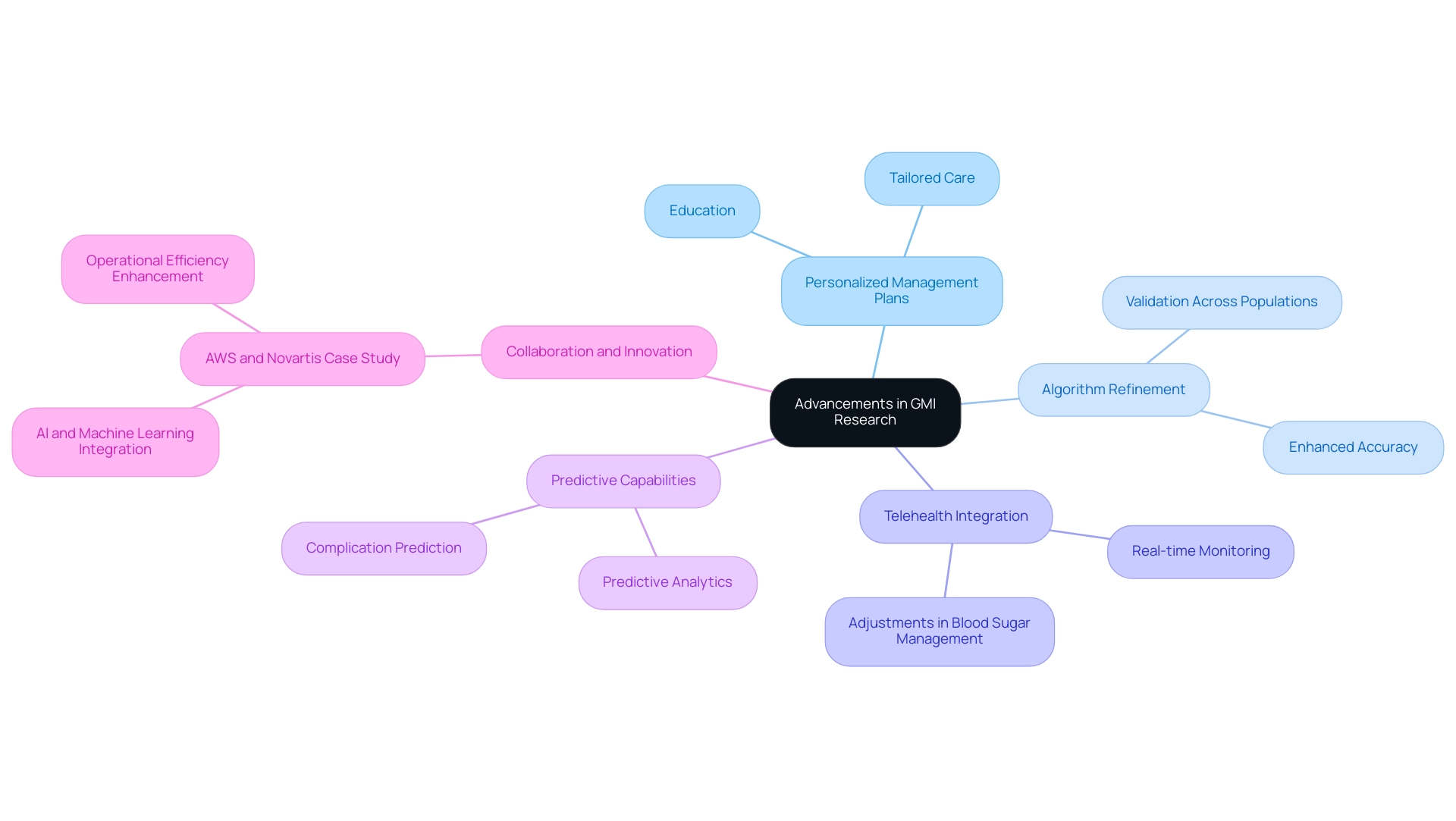
The Future of Diabetes Management: Advancements in GMI Research
Continuous progress in gmi diabetes research is crucial for the development of personalized management plans, especially for type 2 patients. With 1 out of every 3 individuals likely to develop this condition in their lifetime, it is crucial to address this issue with transformative health solutions that empower individuals through education and tailored care. GMI Research, known for delivering around 10 full-fledged business plans every year, is at the forefront of these developments, consistently praised for exceeding expectations in quality and meeting tight project timelines.
Current studies focus on refining algorithms that enhance the accuracy of GMI calculations, ensuring validation across diverse populations. A promising area of exploration is the integration of GMI within telehealth frameworks, offering the potential for real-time monitoring and adjustments in managing blood sugar. Moreover, researchers are actively investigating GMI’s capability to predict diabetes-related complications, which could fundamentally transform management strategies and alleviate the anxiety associated with these complications.
As highlighted by industry experts, the growth potential of GMI research parallels that of the Precision Aquaculture segment, expected to grow at a higher CAGR. Additionally, the collaboration between AWS and Novartis to enhance operational efficiency through advanced AI solutions serves as a compelling case study, illustrating how advanced technologies can integrate into healthcare. As GMI continues to evolve, it is increasingly important for patients and healthcare providers to stay informed about these advancements, fostering a community wellness approach that supports education, nutrition, and comprehensive care in managing type 2 diabetes, including holistic regimens that address health at the root level.
Conclusion
The Glucose Management Indicator (GMI) represents a significant advancement in diabetes management, providing a dynamic and real-time assessment of an individual’s glucose levels through continuous glucose monitoring (CGM) data. Unlike traditional metrics such as HbA1c, GMI allows for timely adjustments in treatment plans, facilitating a more personalized approach to diabetes care. Its ability to empower patients by enhancing their understanding of glucose patterns and promoting engagement is crucial in addressing the complexities of managing diabetes effectively.
The comparative analysis between GMI and HbA1c highlights the strengths and limitations of both metrics. While GMI offers immediate insights into daily glucose fluctuations, it is essential for healthcare providers to exercise caution in its interpretation, given its variability across different populations and treatment regimens. The practical applications of GMI further demonstrate its utility in optimizing treatment strategies, fostering proactive patient involvement, and ultimately improving health outcomes.
As research into GMI continues to advance, the potential for integrating this tool within telehealth frameworks and its role in predicting diabetes-related complications could reshape the landscape of diabetes management. Staying informed about these developments is vital for both patients and healthcare professionals, ensuring that the most effective and personalized care strategies are employed. The journey towards improved diabetes management is ongoing, and GMI stands at the forefront, promising to enhance the quality of life for those affected by this chronic condition.
Frequently Asked Questions
What is the Glucose Management Indicator (GMI) and how is it calculated?
The Glucose Management Indicator (GMI) is a calculated metric that reflects an individual’s average glucose levels over time, typically derived from continuous glucose monitoring (CGM) data.
How does GMI differ from traditional methods of glycemic control?
Unlike conventional methods, GMI provides a more prompt evaluation of glucose levels, allowing healthcare professionals to adjust care strategies with greater accuracy and address the root causes of diabetes more effectively.
What are the benefits of using GMI in diabetes care?
GMI helps eliminate anxiety associated with potential complications of diabetes and empowers patients to take control of their health by providing a better understanding of their glucose management.
What were the findings of the study involving the Libre Pro system regarding GMI?
In a study involving the Libre Pro system, 43% of participants exhibited an absolute difference of ≥0.5 percentage points, and 18% showed a difference greater than 1.0 percentage points, indicating varying levels of glycemic control.
Why is GMI considered important for patient engagement in diabetes management?
GMI enhances patient understanding of glucose management, fostering greater engagement and adherence to treatment protocols, as emphasized by R.N. Aurora from the American Academy of Sleep Medicine.
What challenges exist regarding the accessibility of GMI and CGM systems?
Challenges include insurance coverage complexities for CGM systems, which are often processed as durable medical equipment, hindering patients’ access to essential technology for managing blood sugar.
How does GMI compare to glycated hemoglobin (HbA1c) in diabetes management?
GMI offers a more immediate and dynamic assessment of glucose levels, capturing daily fluctuations, while HbA1c reflects an average of blood sugar levels over the preceding two to three months, providing a retrospective overview.
What are the limitations of using GMI as a measure of glycemic control?
A study found that GMI may be an unreliable measure, showing only moderate correlation with HbA1c and significant variability, suggesting caution in its clinical interpretation.
What factors can influence the interpretation of GMI and HbA1c?
Recent research indicates that age and certain hematological parameters can influence the interpretation of GMI and HbA1c, highlighting the importance of using both metrics for optimal patient care.