Overview
The main focus of this article is to highlight essential medical abbreviations related to Type 2 diabetes that you should be familiar with. Understanding these terms can significantly enhance your ability to manage your condition effectively. It’s important to recognize that while the article provides an overview of various diabetes-related topics, it emphasizes the crucial role of education and awareness about these abbreviations. By familiarizing yourself with this information, you can empower yourself to make informed health decisions and improve your management strategies. Many patients find that this knowledge not only helps in their daily lives but also fosters a sense of control over their health journey.
Introduction
Understanding the medical abbreviations associated with Type 2 diabetes is crucial for both patients and healthcare providers navigating this complex condition. These abbreviations, such as A1C, BG, and DM, serve as shorthand for vital concepts in diabetes management, offering insights into blood sugar levels, treatment options, and potential complications.
It’s important to recognize that, with so much information available, many individuals may feel overwhelmed. How can you ensure that you are grasping the significance of these terms and applying them effectively in your health journey?
This article delves into ten key Type 2 diabetes medical abbreviations that everyone should know, empowering you with the knowledge to take control of your health.
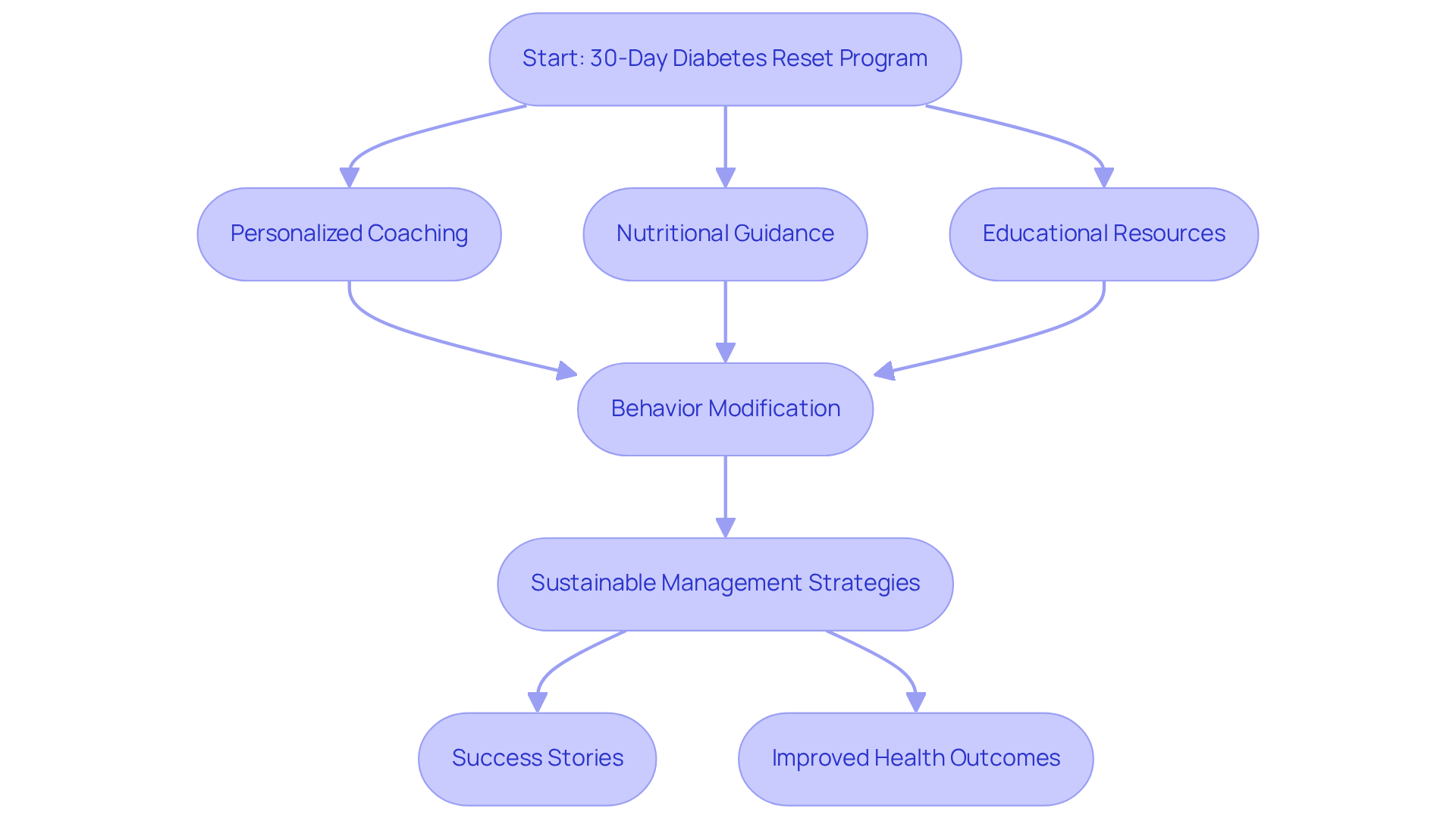
Integrative Wellness Center: 30-Day Diabetes Reset Program
The 30-Day Reset Program at the Integrative Wellness Center is a transformative initiative designed to empower individuals in managing their condition effectively. This program offers personalized coaching, nutritional guidance, and a wealth of educational resources, allowing participants to gain a deeper understanding of their condition and implement sustainable management strategies. By emphasizing behavior modification and lifestyle changes, the program equips individuals with essential tools for long-term success.
It’s important to recognize that recent research, including the Look AHEAD study and the Diabetes Prevention Program (DPP), suggests lifestyle changes, such as those provided in this program, can significantly lower the occurrence of the disease. For instance, individuals in comparable programs have shown a remarkable 58% decrease in the occurrence of diabetes compared to conventional therapies, as noted by Dr. Jason Shumard, who has nearly 20 years of experience in helping individuals reverse type II conditions. This underscores the effectiveness of comprehensive lifestyle modifications over medication alone.
Many success stories from participants highlight the program’s profound impact. Take Ed, for example, who struggled with Type 2 Diabetes for years. He shared, “I was on 2 different meds that weren’t working and was told that I needed insulin. After joining this program, I lost 55 lbs, and my A1C dropped from 9.1 to 5.7. I feel so much better and don’t need my meds anymore!” Numerous individuals report life-changing outcomes, including improved blood sugar levels and enhanced overall well-being. This comprehensive approach not only addresses the symptoms of the condition but also empowers individuals to regain control over their health.
As diabetes management continues to evolve, many patients find that personalized, behavior-driven programs like the 30-Day Diabetes Reset are becoming increasingly prominent in the context of type 2 diabetes medical abbreviation. This trend reflects a growing recognition of the importance of patient education and empowerment in achieving lasting health improvements. To learn more about the program and how it can support you, we invite you to visit our website or contact us today!
A1C: Understanding Your Average Blood Sugar Levels
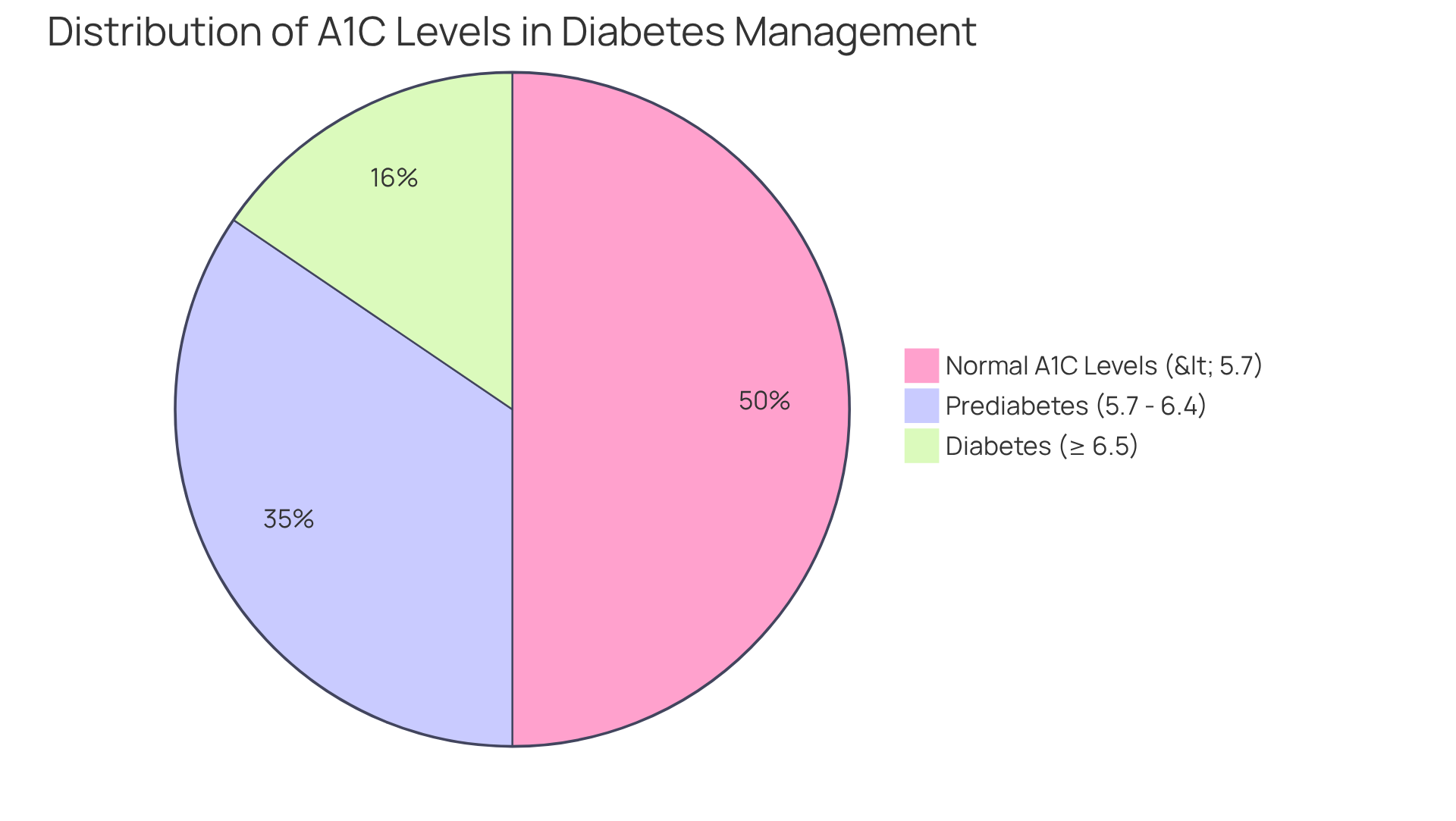
A1C, or glycated hemoglobin, is a vital test that reveals your average glucose concentrations over the past two to three months. This measurement is crucial for managing your blood sugar levels effectively, as it reflects how well your glucose is being controlled. It’s important to recognize that according to current guidelines, an A1C measurement below 5.7% is considered normal, while readings between 5.7% and 6.4% suggest prediabetes. A measurement of 6.5% or higher confirms a diabetes diagnosis. Consistently tracking your A1C values is essential, as it helps guide your treatment choices and lifestyle modifications.
Many patients find that incorporating holistic lifestyle strategies can significantly impact their A1C levels. Embracing a balanced diet rich in local produce, such as avocados and berries, alongside regular outdoor exercise in San Marcos, can enhance insulin sensitivity and blood sugar control. Participating in community wellness initiatives not only offers support but also fosters a sense of responsibility, which is crucial for effectively managing your condition. Consider joining local classes aimed at health education and stress management techniques, such as yoga or mindfulness practices, to further nurture your well-being.
Recent research emphasizes the importance of keeping A1C figures under 7% for most adults with high blood sugar to reduce the risk of complications. For example, individuals who actively engage in self-management education often report notable improvements in their A1C readings, with many achieving decreases of 1% or more within a few months of adopting lifestyle changes. This highlights the potential for effective management of your condition through informed decision-making and proactive health strategies.
Typically, individuals with the type 2 diabetes medical abbreviation have A1C readings near 7.5%. However, with dedicated efforts in nutrition, physical activity, and medication adherence, many can bring their A1C down to the recommended target range. Continuous glucose monitoring (CGM) technology is increasingly being used to provide real-time feedback, allowing you to make timely adjustments to your management plans, thereby enhancing your ability to maintain optimal A1C values. Additionally, setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can help you track your progress effectively.
Approximately 10.5% of the U.S. population is affected by this health issue, with 85% of the cases classified under the type 2 diabetes medical abbreviation. This underscores the importance of A1C monitoring in managing this widespread condition. It’s essential to note that reaching fasting plasma glucose (FPG) targets may not always align with ideal A1C readings, necessitating a broader strategy that includes tracking postprandial glucose (PPG) as well. For personalized guidance and support tailored to your unique needs, consider reaching out to Dr. Jason Shumard in San Marcos, CA.
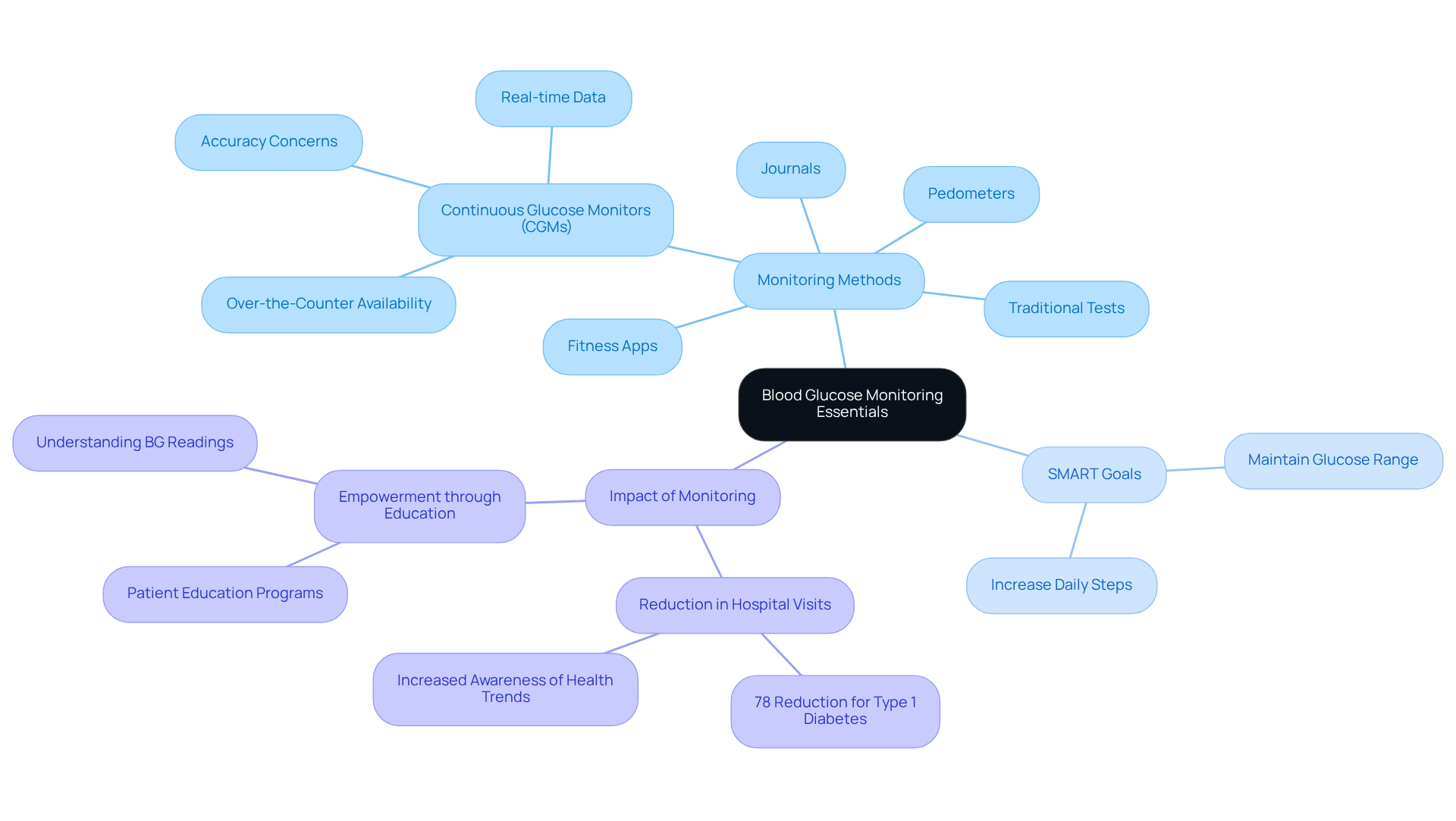
BG: Blood Glucose Monitoring Essentials
Monitoring blood glucose (BG) is essential for effectively managing diabetes. Regularly checking blood sugar levels helps maintain them within target ranges, which is crucial for preventing complications. Many patients face challenges in this area, but there are various methods available to assist them. Traditional fingerstick tests, advanced continuous glucose monitors (CGMs), fitness apps, journals, and pedometers can all play a role in this journey. CGMs, now easily accessible over the counter, provide real-time glucose data, empowering users to make informed health decisions. Many individuals find that using CGMs leads to significant improvements in managing their condition, including a notable reduction in hospital visits for heart-related issues.
To enhance diabetes management, consider implementing SMART goals—specific, measurable, attainable, relevant, and time-bound. For example, you might aim to:
- Keep your glucose readings within a certain range
- Increase your physical activity by walking a specific number of steps each day
By consistently observing your levels, you can identify trends that inform necessary adjustments in nutrition, activity, and medication. It’s important to recognize that individuals who have faced severe low blood sugar episodes are twice as likely to be hospitalized for heart-related complications, highlighting the critical nature of regular monitoring.
Diabetes educators stress that understanding BG readings is vital for effective management. This knowledge empowers patients to take control of their health. By regularly assessing your progress, you not only foster a sense of responsibility but also allow for the adjustment of goals as your fitness evolves. Dr. Peter notes, “It motivates people to see how food, exercise, and beverages can affect them in real time.” Integrating these practices into your daily routine can significantly improve your quality of life and lessen the need for conventional medical interventions. However, it’s crucial to be aware of potential inaccuracies in CGM readings, which can lead to unnecessary health concerns. Therefore, consulting healthcare professionals for guidance on effectively using CGMs is essential.
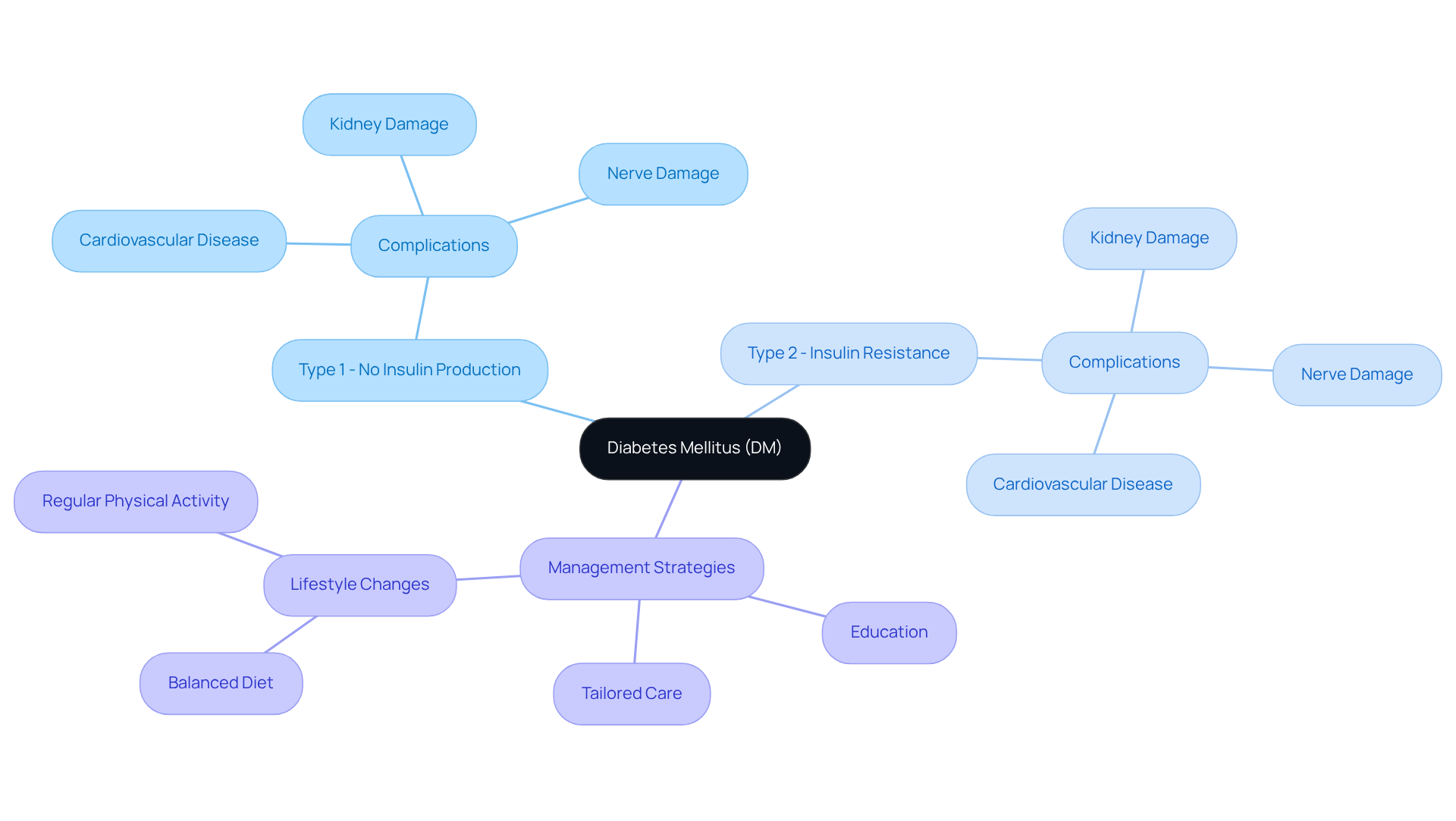
DM: Diabetes Mellitus and Its Implications
Diabetes mellitus (DM) is a chronic condition that many people grapple with, marked by high blood sugar levels due to the body’s challenges in producing or effectively using insulin. It’s essential to recognize that there are two primary categories:
- Type 1, where the body does not produce insulin
- Type 2, which involves [[insulin resistance
Understanding DM](https://drshumard.com/about](https://drshumard.com/about)) is crucial, as it can lead to serious health complications, including cardiovascular disease, kidney damage, and nerve damage if not managed properly.
Many patients find that education about DM is vital for effective self-management. At Integrative Wellness Center, Dr. Jason Shumard, D.C., who possesses advanced education in functional endocrinology and clinical nutrition, emphasizes the importance of assisting individuals in reversing their condition through thorough education and tailored care. This approach enables patients to take charge of their health, fostering a sense of empowerment.
It’s also important to acknowledge the financial strain of managing this condition, which can greatly affect patients’ lives. Simple lifestyle changes, such as maintaining a balanced diet and engaging in regular physical activity, can play a crucial role in effectively managing blood sugar levels. Remember, you are not alone in this journey; many have found success through small, consistent changes. What steps can you take today to start your path toward better health?
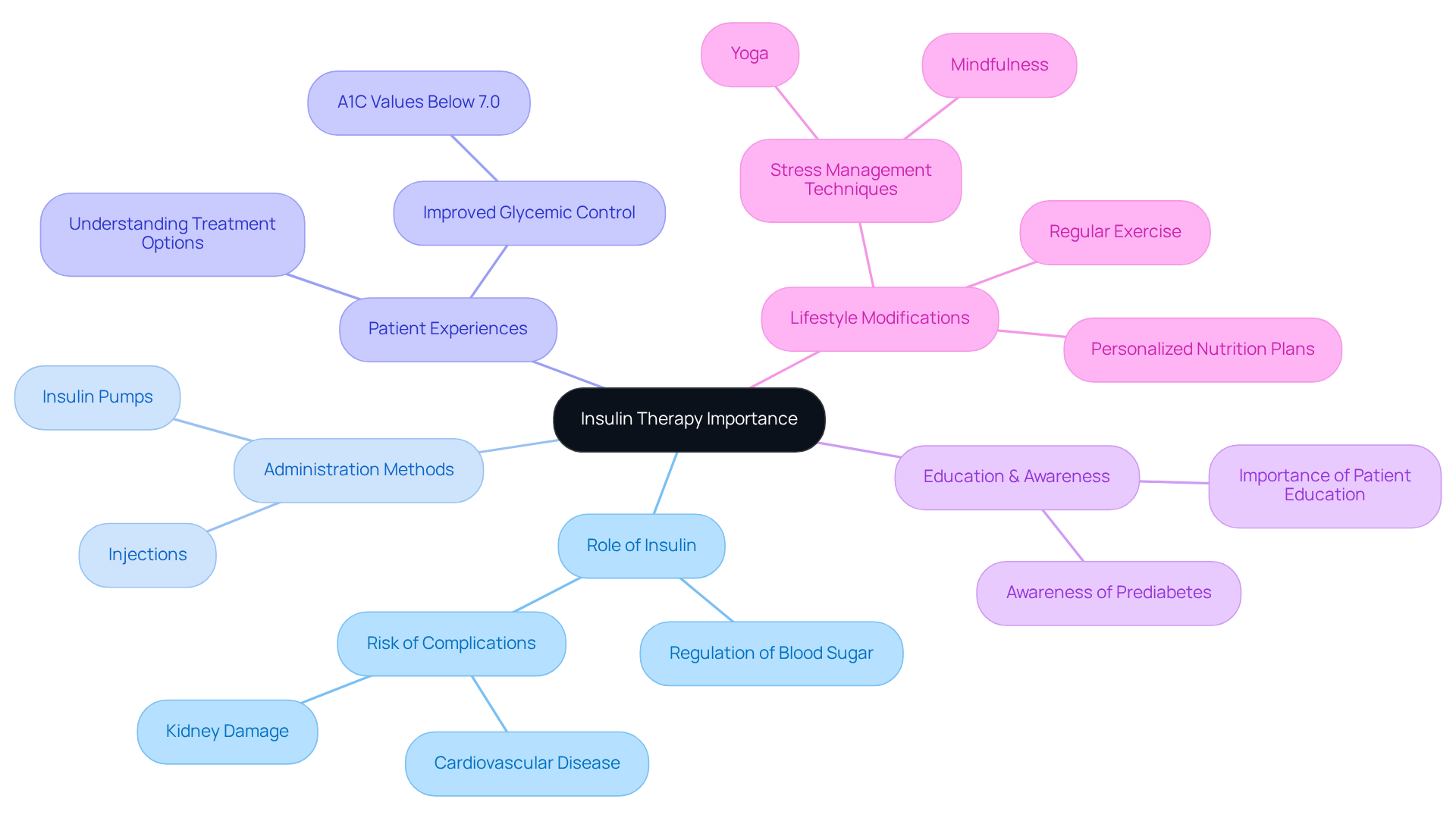
INS: Insulin and Its Importance in Treatment
Insulin is an essential hormone produced by the pancreas, playing a crucial role in regulating sugar levels in the body. For many individuals facing diabetes, particularly those with Type 1 and a significant number with the type 2 diabetes medical abbreviation, insulin therapy is vital for maintaining optimal blood glucose control. It’s important to recognize that current trends show a growing reliance on insulin therapy, with an increase in the number of insulin users for conditions represented by the type 2 diabetes medical abbreviation over the years. This reflects a broader understanding of its necessity in managing this illness.
Patients can administer insulin through various methods, including injections and insulin pumps, which allows for flexibility in treatment plans. The choice of administration method often depends on individual patient needs and preferences. Effective insulin management is crucial for preventing hyperglycemia, especially in individuals with type 2 diabetes medical abbreviation, as this condition can lead to severe complications like cardiovascular disease and kidney damage. Many patients find that understanding their treatment options significantly impacts their health journey. Research indicates that almost 39.2% of adults with diabetes also suffer from chronic kidney disease, underscoring the importance of strict sugar regulation.
Real-world experiences highlight how insulin therapy can improve blood sugar control. Patients utilizing insulin often report significant improvements in their glycemic levels, with many achieving A1C values below the critical threshold of 7.0%. This is especially significant considering that 47.4% of U.S. adults with diagnosed high blood sugar levels have A1C values of 7.0% or greater. It’s crucial to recognize the pressing need for effective insulin management strategies.
Moreover, integrating lifestyle modifications such as personalized nutrition plans, regular exercise, and stress management techniques—like mindfulness and yoga—can further enhance the effectiveness of insulin therapy. The importance of education in insulin therapy cannot be overstated. Patients must understand how and when to use insulin to maximize its benefits and minimize risks. Continuous education and support systems are essential for empowering patients to manage their condition effectively and enhance their overall health outcomes. Notably, only 19.0% of adults with prediabetes reported being informed by a health professional about their condition, highlighting the need for improved education and awareness. Furthermore, 31.9% of U.S. adults with diagnosed conditions related to blood sugar were physically inactive, emphasizing the significance of lifestyle factors in managing this health issue.
To take charge of your condition management, consider reaching out to healthcare professionals for personalized guidance and support tailored to your unique needs. Remember, you are not alone on this journey, and there are resources available to help you thrive.
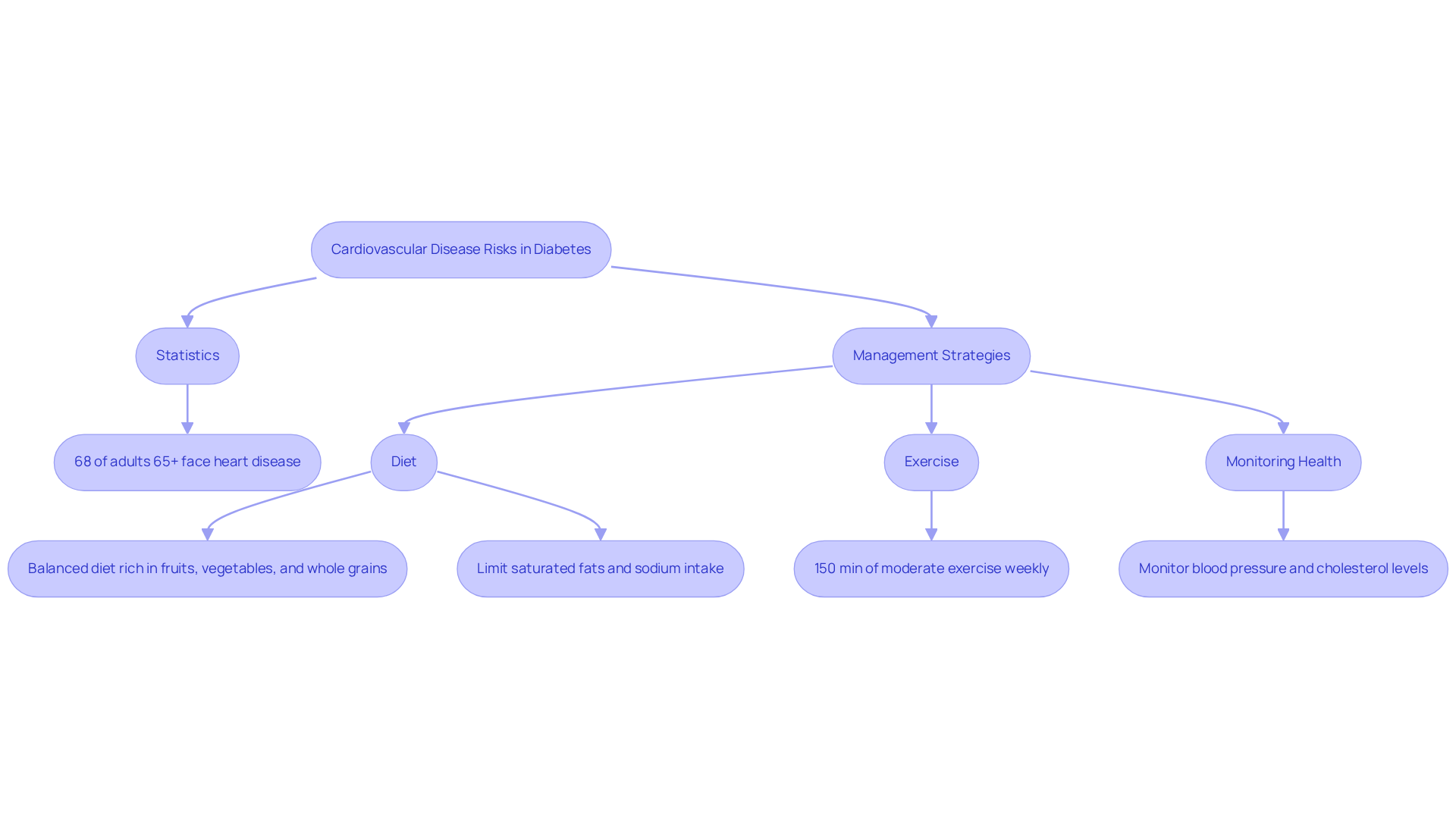
CVD: Cardiovascular Disease Risks in Diabetes
Individuals facing this condition often experience a significantly heightened risk of developing cardiovascular disease (CVD), which includes serious issues like heart disease and stroke. It’s important to recognize that increased glucose concentrations can damage the vascular structures and nerves that control heart function, leading to serious complications. Current statistics reveal that nearly 68% of adults aged 65 and older with diabetes succumb to some form of heart disease, underscoring the urgent need for effective management strategies.
To reduce this risk, patients must actively manage their sugar levels through a balanced diet rich in fruits, vegetables, and whole grains, while also limiting saturated fats and sodium intake. In San Marcos, CA, many individuals find joy in embracing local produce from vibrant farmers’ markets, incorporating seasonal fruits like avocados and berries into their meals. Many patients find that engaging in consistent physical activity—aiming for at least 150 minutes of moderate exercise each week—can significantly lower blood pressure and enhance overall cardiovascular health. Moreover, monitoring additional risk factors such as blood pressure and cholesterol levels is crucial, as reducing dietary sodium to under 1500 mg daily can decrease blood pressure by 5-6 mm Hg.
Adopting these lifestyle changes not only helps control blood sugar levels but also plays a vital role in lowering the risk of cardiovascular disease. Community wellness programs in San Marcos provide valuable resources and support for individuals eager to improve their health. These programs often feature classes on nutrition, exercise, and stress management techniques, such as yoga or mindfulness practices, which can further bolster overall well-being and blood sugar control.
As healthcare experts emphasize, a proactive approach to health management, featuring personalized advice from specialists like Dr. Jason Shumard, can lead to improved outcomes and a better quality of life for those managing this condition. Remember, you are not alone on this journey—support is available, and taking small steps can lead to significant changes.
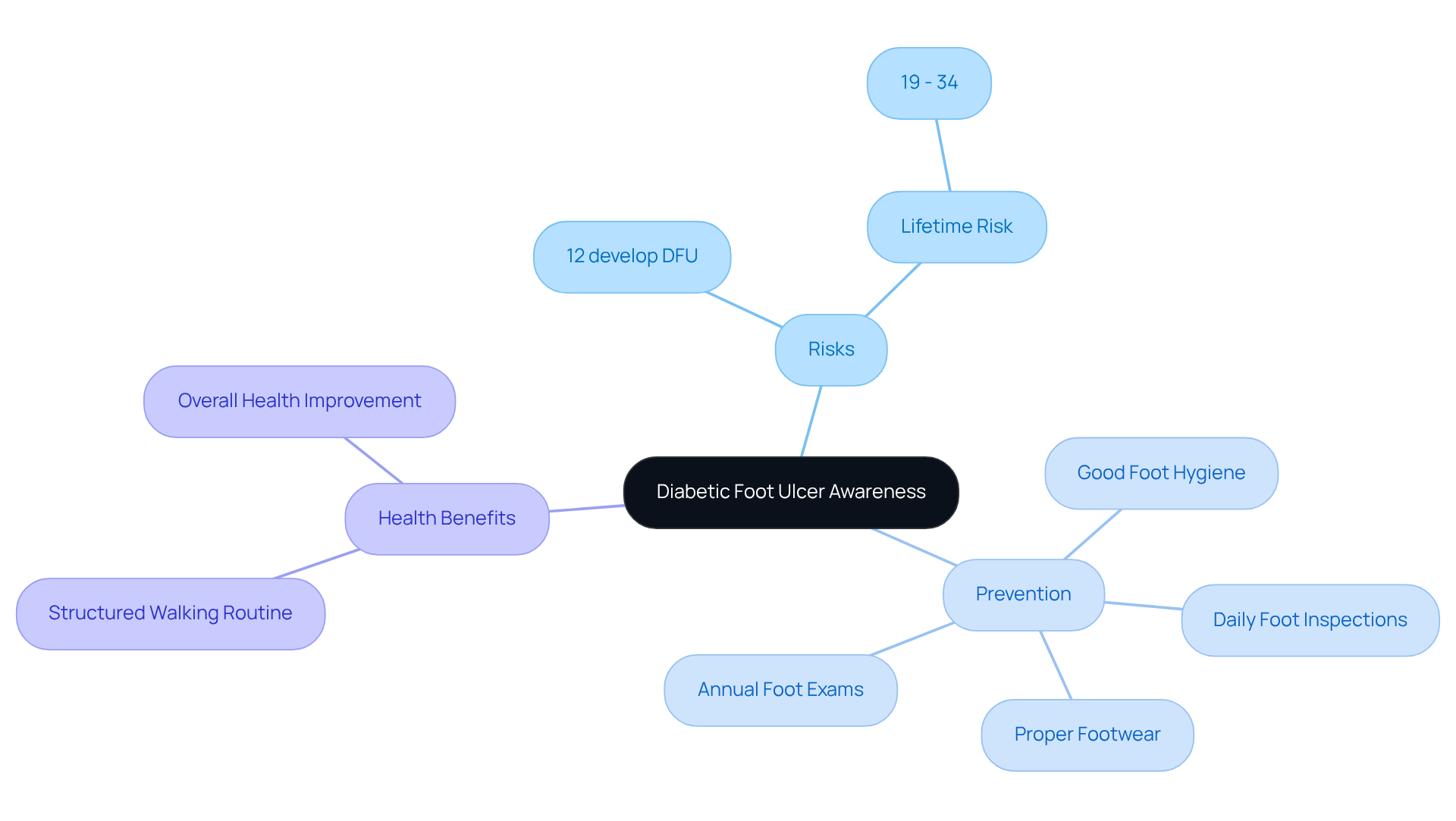
DFU: Diabetic Foot Ulcer Awareness
Diabetic foot ulcers (DFUs) can be a significant source of concern for many individuals living with diabetes. If not addressed promptly, these ulcers can lead to severe infections and even amputations. It’s important to recognize that elevated blood sugar levels can cause nerve damage and impaired circulation, increasing the risk of foot injuries and ulcers. Did you know that about 12% of individuals with diabetes will develop a diabetic foot ulcer during their lifetime? The lifetime risk can range from 19% to 34%.
Routine foot examinations are crucial for prevention. Individuals should inspect their feet daily for cuts, blisters, or sores. Maintaining good foot hygiene, such as washing feet with lukewarm water and mild soap, is essential. Many patients find that wearing suitable footwear can make a significant difference in preventing injuries. It’s best to avoid flip-flop sandals and stockings with seams, as these can create pressure points that lead to complications. Early detection and treatment of foot issues are vital in preventing DFUs, as complications can escalate quickly.
Following current guidelines, it’s recommended that patients have annual foot exams and consult healthcare providers at the first sign of any foot problems. As Dr. Jason Shumard emphasizes, “Complications can be avoided or delayed with yearly comprehensive foot exams and treatment.” Furthermore, initiating a structured walking routine can greatly improve overall health and energy, which is essential for managing blood sugar levels. Individuals should start by evaluating their current fitness levels and setting realistic walking goals, such as committing to a daily walk of 10-15 minutes.
By focusing on foot care and participating in regular physical activity, individuals with high blood sugar can enhance their overall health results. Remember, you are not alone in this journey, and with the right care and support, you can take proactive steps towards better health.
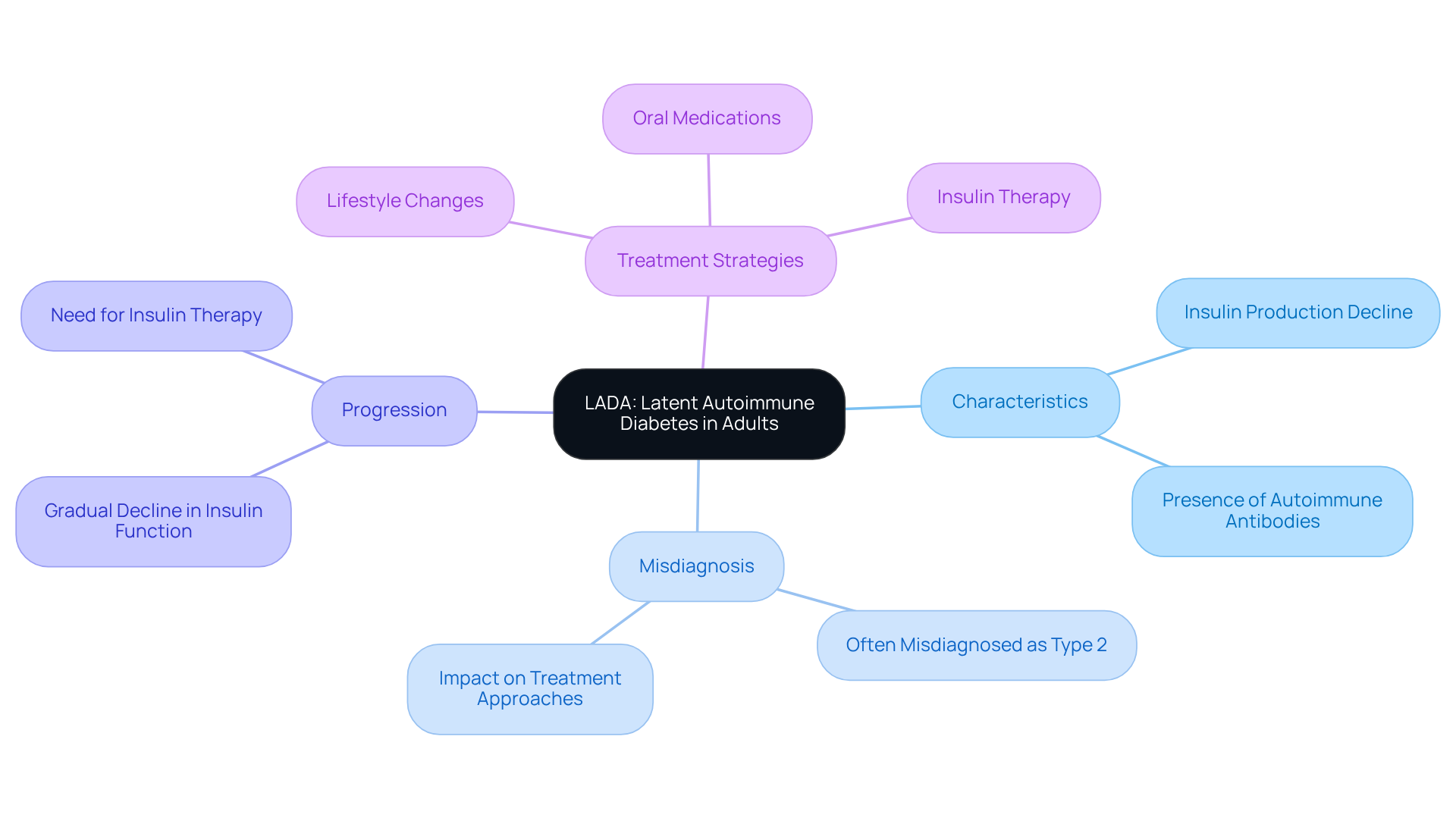
LADA: Latent Autoimmune Diabetes in Adults
Latent Autoimmune Diabetes in Adults (LADA) is a unique condition that blends characteristics of both Type 1 and Type 2 diabetes, typically emerging in adults. Unfortunately, it is often misdiagnosed as Type 2. LADA is marked by a gradual decline in insulin production, alongside the presence of autoimmune antibodies. Unlike conventional Type 2 diabetes, where insulin resistance is the primary issue, individuals with LADA experience an autoimmune attack on their insulin-producing cells, leading to a slow decrease in insulin function.
Initially, many individuals with LADA may find that they can manage their condition through lifestyle changes and oral medications. However, as the disease progresses, insulin therapy often becomes necessary to maintain glycemic control. It’s important to recognize LADA for effective management, as misdiagnosis can result in unsuitable treatment approaches. Research indicates that LADA accounts for about 9% of those diagnosed with the type 2 diabetes medical abbreviation, underscoring the need for greater awareness among healthcare professionals.
At Integrative Wellness Center, we emphasize the importance of personalized treatment strategies tailored to the unique needs of individuals with LADA. By conducting advanced testing, we can identify the specific dietary requirements of each patient, allowing us to develop comprehensive plans aimed at reversing the condition and achieving glucose stabilization without relying solely on insulin.
If you suspect that you may have LADA or are struggling to manage your condition, we invite you to schedule a consultation with our functional medicine practitioners. Together, we can craft a personalized approach to enhance your health and well-being.
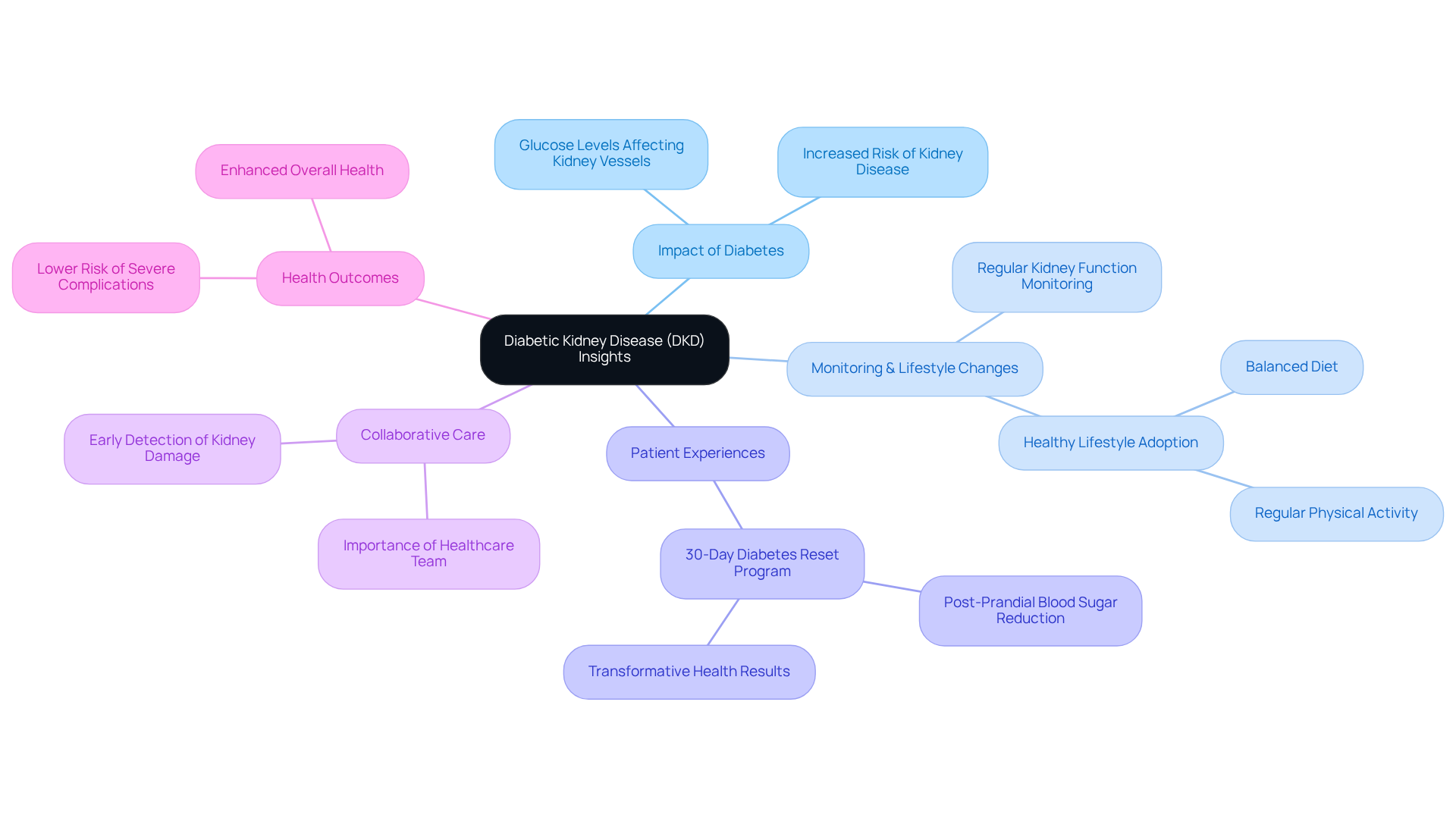
DKD: Diabetic Kidney Disease Insights
Diabetic kidney disease (DKD) is a prevalent complication of diabetes, significantly increasing the risk of chronic kidney disease and eventual kidney failure. It’s important to recognize that increased glucose levels can harm the kidney’s vessels, hindering their waste filtration abilities. To prevent or slow the progression of DKD, regular monitoring of kidney function is essential, alongside maintaining blood sugar and blood pressure within recommended ranges. Adopting a healthy lifestyle, which includes a balanced diet and regular physical activity, plays a vital role in managing these conditions.
Many patients find that real-world examples illustrate the effectiveness of proactive diabetes management. For instance, individuals who have participated in Dr. Jason Shumard’s 30-Day Diabetes Reset program have reported transformative results. One individual shared, “I experienced a drop in post-prandial blood sugar levels from 554 mg/dL to 201 mg/dL within just a few days of implementing dietary changes.” This showcases the potential for structured lifestyle interventions to enhance kidney function and overall health.
Current guidelines highlight the significance of collaborative care. It’s crucial for individuals to work closely with their healthcare teams to monitor kidney health effectively. This partnership is key in identifying early signs of kidney damage and implementing timely interventions. Significantly, one in five individuals with blood sugar issues will require care for kidney disease at some point in their lives, underscoring the importance of observing kidney health. Dr. Aisling McMahon emphasizes that preventing severe kidney issues in individuals with blood sugar conditions is a priority, highlighting the significance of cooperative care.
By prioritizing kidney health and adopting holistic lifestyle strategies, individuals with blood sugar issues can significantly enhance their overall health outcomes and lower the risk of severe complications linked to DKD. Remember, taking these steps not only supports your kidneys but also fosters a healthier, more vibrant life.
DR: Diabetic Retinopathy and Its Impact
Diabetic retinopathy (DR) is a serious eye condition that can lead to vision loss and blindness in individuals with diabetes. It occurs when elevated sugar levels harm the vessels in the retina. It’s important to recognize that there are two primary stages of diabetic retinopathy:
- Non-Proliferative Diabetic Retinopathy (NPDR), the early stage marked by leaking vessels
- Proliferative Diabetic Retinopathy (PDR), where new, delicate vessels develop on the retina
Many patients find that the initial phases of DR may not show any symptoms, but they might notice warning signs like seeing floaters or blurred vision. This makes regular eye examinations essential for early detection.
To effectively manage DR and overall health, patients should:
- Monitor their blood sugar levels
- Maintain a healthy lifestyle that includes regular exercise and a balanced diet rich in fiber and nutrients
- Utilize tracking methods such as fitness apps and journals to help individuals stay accountable and motivated
- Establish SMART objectives—specific, measurable, attainable, relevant, and time-bound—to greatly improve focus and motivation in managing health. For instance, individuals might aim to walk 10,000 steps daily or incorporate more fresh produce into their meals
- Participate in community wellness initiatives that can offer assistance and resources customized for managing blood sugar levels
Regular eye check-ups are essential for preventing or managing DR effectively. Treatment options may include laser therapy and anti-VEGF injections, which can significantly reduce the risk of vision loss. However, it is important to note that while these treatments can prevent further deterioration, they cannot reverse existing damage. Additionally, managing other risk factors such as high blood pressure and high cholesterol is essential for maintaining eye health in diabetes patients. Remember, you are not alone in this journey, and there are resources and support available to help you thrive.
Conclusion
Understanding the key medical abbreviations associated with type 2 diabetes is essential for effective disease management. It’s important to recognize that terms like A1C, BG, DM, INS, CVD, DFU, LADA, DKD, and DR represent critical aspects of diabetes care. By familiarizing yourself with these abbreviations, you can better navigate your health journey and make informed decisions regarding your treatment and lifestyle choices.
Many patients find that acknowledging the challenges of diabetes is the first step toward improvement. The discussion covered various facets of diabetes, including the importance of lifestyle modifications, the role of insulin therapy, and the need for regular monitoring of blood glucose levels. Programs like the 30-Day Diabetes Reset can lead to transformative results, as evidenced by inspiring participant success stories. Additionally, it’s crucial to be aware of potential complications arising from diabetes, such as cardiovascular disease and diabetic retinopathy, while exploring proactive strategies for prevention and management.
In conclusion, the journey to managing type 2 diabetes is multifaceted, requiring a comprehensive understanding of medical terms and a commitment to lifestyle changes. Empowerment through education and support is key. Engaging with healthcare professionals, participating in community wellness initiatives, and adopting informed strategies can significantly enhance health outcomes. Taking these steps not only fosters better management of diabetes but also promotes a healthier, more fulfilling life. Remember, you are not alone on this journey; support is available, and every small step counts.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at the Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a transformative initiative designed to help individuals manage their diabetes through personalized coaching, nutritional guidance, and educational resources. It focuses on behavior modification and lifestyle changes for long-term success.
How effective is the 30-Day Diabetes Reset Program?
Research, including the Look AHEAD study and the Diabetes Prevention Program (DPP), indicates that lifestyle changes offered in this program can lead to a significant 58% decrease in the occurrence of diabetes compared to conventional therapies.
Can you provide an example of a success story from the program?
One participant, Ed, who struggled with Type 2 Diabetes, lost 55 lbs and reduced his A1C from 9.1 to 5.7 after joining the program, eliminating the need for medications.
What is A1C and why is it important?
A1C, or glycated hemoglobin, is a test that measures average glucose levels over the past two to three months. It is crucial for managing blood sugar levels and determining treatment choices, with readings below 5.7% considered normal.
What A1C levels indicate prediabetes or diabetes?
A1C readings between 5.7% and 6.4% suggest prediabetes, while a measurement of 6.5% or higher confirms a diabetes diagnosis.
How can lifestyle changes impact A1C levels?
Incorporating holistic strategies like a balanced diet and regular exercise can significantly improve A1C levels, with many individuals achieving reductions of 1% or more after adopting these changes.
What role does blood glucose monitoring play in diabetes management?
Regular blood glucose monitoring is essential for maintaining target sugar levels and preventing complications. It helps individuals make informed decisions regarding their nutrition, activity, and medication.
What methods are available for monitoring blood glucose?
Methods for monitoring blood glucose include traditional fingerstick tests, continuous glucose monitors (CGMs), fitness apps, journals, and pedometers.
What are SMART goals in the context of diabetes management?
SMART goals are specific, measurable, attainable, relevant, and time-bound objectives that help individuals track their progress, such as maintaining glucose readings within a certain range or increasing daily physical activity.
What should individuals be aware of when using continuous glucose monitors (CGMs)?
While CGMs provide real-time glucose data and can improve diabetes management, users should be cautious of potential inaccuracies in readings and consult healthcare professionals for proper guidance.