Overview
It’s important to recognize the main signs of sudden onset type 2 diabetes that should not be ignored. These include:
- Increased thirst
- Frequent urination
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
- Tingling or numbness
- Skin changes
Many patients find that acknowledging these symptoms is the first step toward better health. Recognizing these signs is crucial for timely medical intervention, which can significantly improve health outcomes and reduce complications associated with the condition. Remember, taking action now can lead to a healthier future.
Introduction
Recognizing the signs of sudden onset type 2 diabetes is crucial for early intervention and effective management. Many individuals overlook key symptoms, and it’s alarming to think about the consequences. What if a simple change in thirst, urination patterns, or unexplained weight loss could signal a serious condition? Understanding these warning signs can empower you to take charge of your health.
In this article, we will explore nine critical indicators that should not be ignored. Each sign offers insights into how they relate to diabetes and underscores the importance of seeking timely medical advice.
Remember, you are not alone in this journey; awareness is the first step toward a healthier future.
Integrative Wellness Center: 30-Day Diabetes Reset Program for Lasting Health Transformation
At the Integrative Wellness Center, we understand the challenges that come with managing sudden onset diabetes type 2. That’s why we’ve created a transformative 30-Day Diabetes Reset Program, designed to empower you to take control of your well-being. This groundbreaking, clinically validated program combines personalized coaching, nutritional guidance, and educational resources to help you understand your condition and implement sustainable lifestyle changes.
It’s important to recognize that focusing on behavior change and comprehensive well-being can make a significant difference. Our program provides you with the essential resources for lasting success in controlling blood sugar levels, including stabilizing glucose levels without reliance on insulin and prescription medications. Many patients find that this approach not only helps them manage their condition, such as sudden onset diabetes type 2, but also enhances their overall quality of life.
As part of the program, you will also benefit from seminars and access to Dr. Shumard’s books, which offer additional insights into reversing the condition and attaining optimal wellness. Success narratives from former participants highlight notable advancements in managing their sudden onset diabetes type 2, demonstrating the program’s efficacy in promoting enduring wellness changes.
Join the thousands who have transformed their lives through this innovative approach. Are you ready to take the first step towards improved well-being? Reach out to us today to discover more about how you can begin your journey!
Increased Thirst: A Key Indicator of Sudden Onset Diabetes Type 2
One of the hallmark symptoms of sudden onset type 2 blood sugar disorder is increased thirst, medically known as polydipsia. This can be concerning, as it occurs when high blood sugar levels lead to dehydration, prompting your body to signal the need for more fluids. Have you ever found yourself feeling excessively thirsty, especially after drinking? If so, it may be time to consult a healthcare professional for further evaluation.
At Integrative Wellness Center, we prioritize a patient-centered approach, empowering you with personalized guidance to manage your health effectively. We understand that navigating these challenges can be overwhelming, and we’re here to support you. Don’t hesitate to reach out to Dr. Jason Shumard for a complimentary consultation. He is committed to transforming healthcare and assisting you in navigating your path towards reversing Type 2. Together, we can work towards a healthier future.
Frequent Urination: Recognizing a Warning Sign of Type 2 Diabetes
Frequent urination, or polyuria, can be a troubling sign of type 2 sugar intolerance. It’s important to recognize that as blood sugar levels rise, your kidneys work harder to filter and absorb the excess glucose, a condition that may result in sudden onset diabetes type 2 and increased urine production. Many patients find that they are urinating more frequently than usual, especially at night. If this sounds familiar, please don’t hesitate to seek medical advice to rule out any serious health issues or underlying conditions.
At Integrative Wellness Center, we truly understand the importance of personalized care, especially in light of concerning hospital safety issues, such as incorrect medications and infections. Dr. Jason Shumard’s holistic approach is designed to provide you with tailored guidance and support on your journey to better health. Remember, you are not alone in this; we are here to help you navigate these challenges.
Don’t wait to enhance your lifestyle changes and take charge of your health management. Reach out to us today, and together we can embark on this path toward a healthier you.
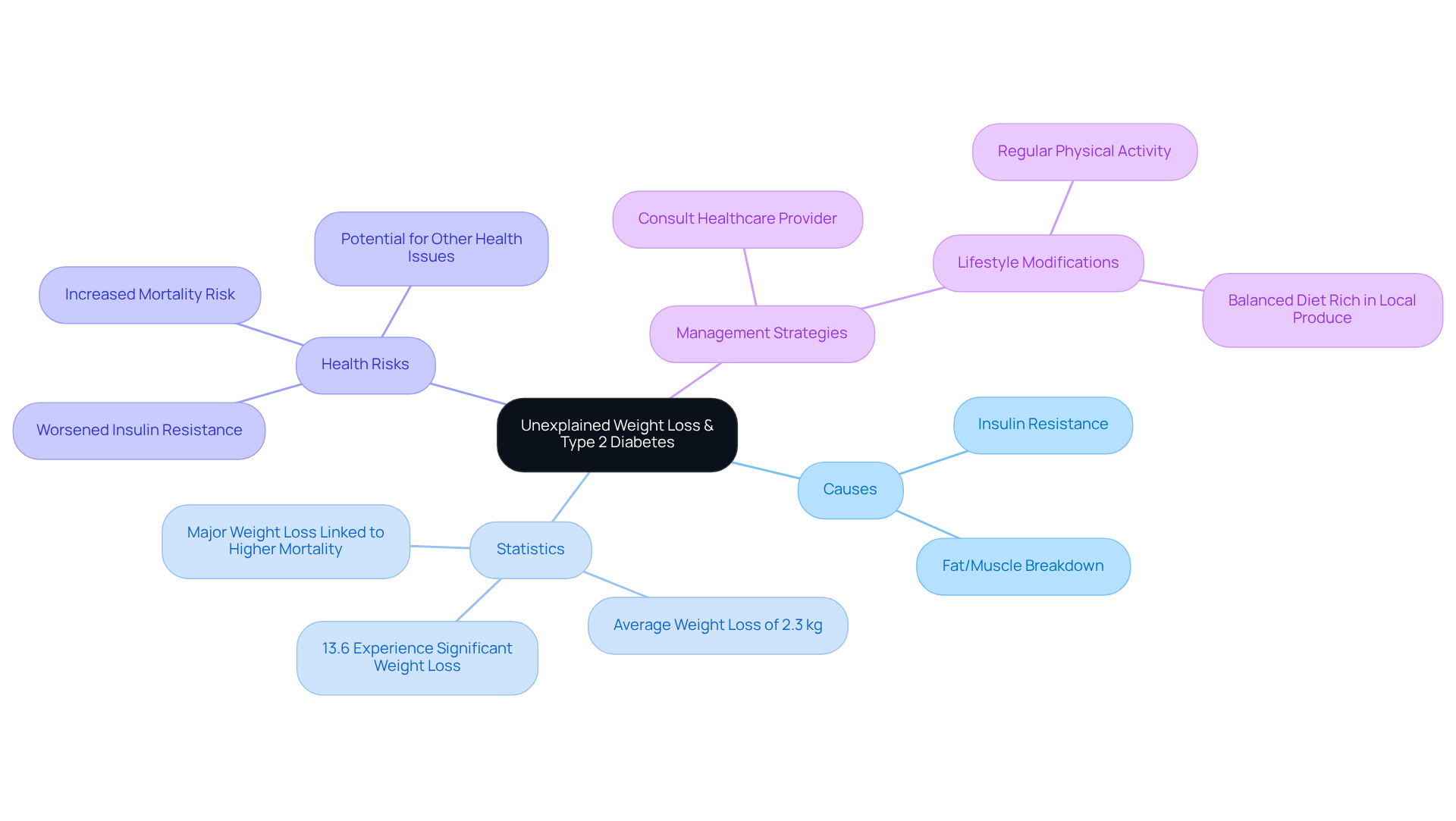
Unexplained Weight Loss: A Surprising Sign of Type 2 Diabetes
Unexplained weight loss can be a surprising sign of type 2 diabetes. When the body struggles to utilize glucose effectively due to insulin resistance, it compensates by breaking down fat and muscle for energy, leading to weight loss. Research shows that approximately 13.6% of individuals with type 2 diabetes experience significant weight reduction without any deliberate effort. This phenomenon often goes unnoticed until it becomes pronounced, prompting individuals to seek medical advice.
It’s important to recognize this symptom. Unexplained weight reduction of 10 pounds or more should not be overlooked, as it may indicate underlying health concerns, including other conditions. Nutritionists explain that when glucose fails to reach cells, the body perceives a state of starvation, leading to rapid fat and muscle breakdown. This process can worsen insulin resistance, creating a vicious cycle that complicates the management of the condition.
Recent studies have shed light on the relationship between weight loss and insulin resistance. For example, a meta-analysis uncovered that substantial weight reduction (≥ 10%) shortly after a diagnosis of diabetes-related conditions is associated with heightened mortality, especially among individuals with worsened lifestyles. On the other hand, purposeful weight reduction along with lifestyle enhancements can lead to improved wellbeing, lowering the chance of issues related to blood sugar conditions.
Many patients find that recognizing the impact of unexplained weight loss empowers them to seek help, leading to effective management strategies that address both weight and blood sugar levels. If you notice significant weight loss without trying, it is essential to consult a healthcare provider for a thorough evaluation, as this could indicate sudden onset diabetes type 2. Additionally, consider incorporating lifestyle modifications like regular outdoor activity in San Marcos, CA, and emphasizing a balanced diet rich in local produce to enhance your overall well-being and health management.
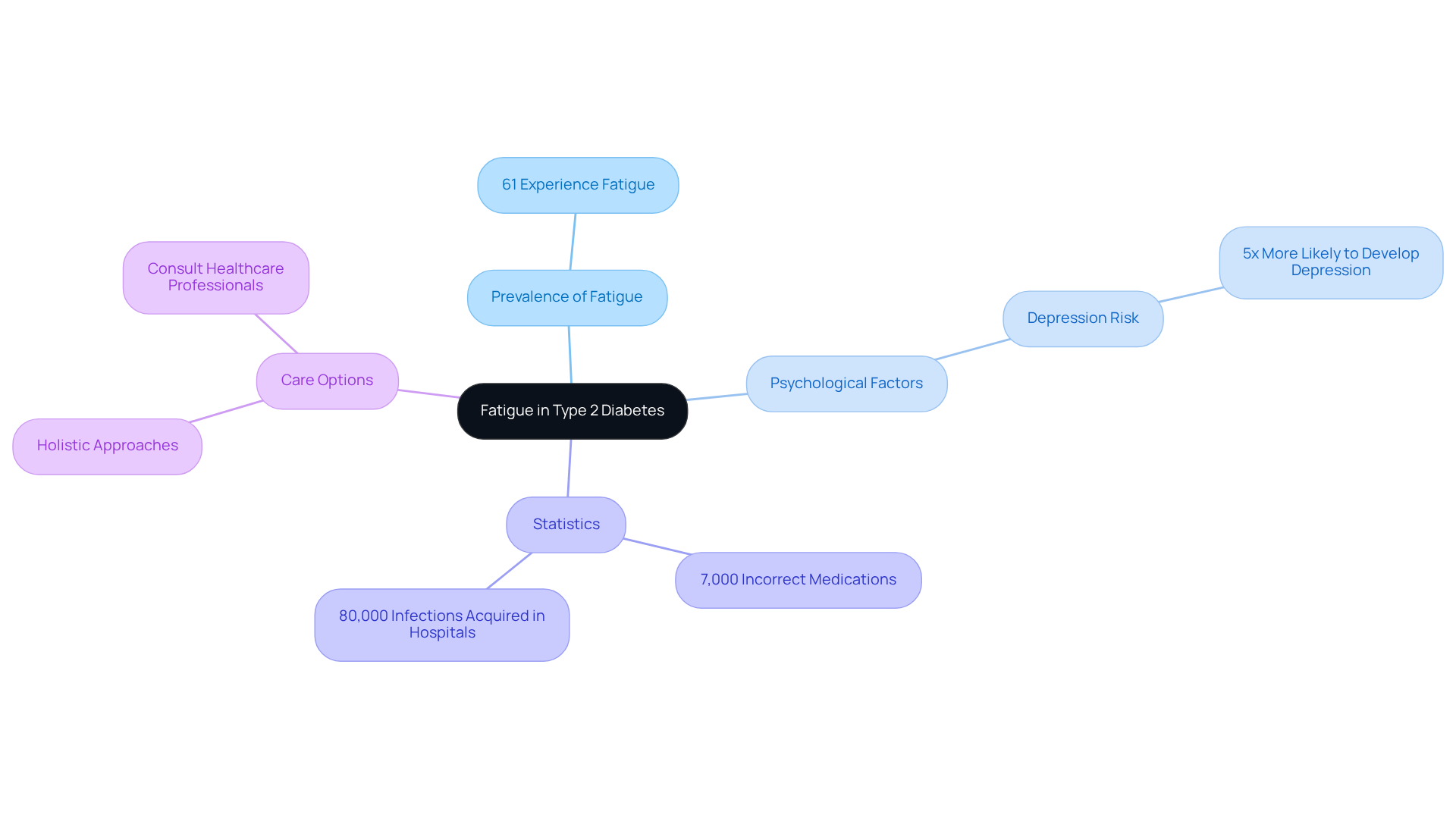
Fatigue: An Overlooked Symptom of Sudden Onset Diabetes Type 2
Fatigue is a frequent but often overlooked sign of sudden onset diabetes type 2, primarily stemming from the body’s reduced ability to utilize glucose effectively. Have you ever felt persistently tired or lethargic, even after a good night’s sleep? Elevated blood sugar levels can lead to these feelings, significantly affecting your daily activities. Research indicates that around 61% of individuals dealing with type 2 diabetes experience fatigue, with many describing it as a debilitating aspect of their condition. This fatigue can linger, suggesting that there may be deeper issues at play.
It’s important to recognize that fatigue in individuals with diabetes isn’t just a result of physical exertion. It’s also intricately linked to psychological factors such as depression and anxiety, which are common in this group. Did you know that individuals with diabetes are nearly five times more likely to experience depression compared to those without the condition? This connection can exacerbate feelings of fatigue, making it even more challenging to cope.
Given the concerning statistics of:
- 7,000 incorrect medications
- 80,000 infections acquired in hospitals
it’s crucial for patients to explore alternative care options. If you find yourself feeling unusually fatigued, especially after a full night’s rest, it may be wise to consult a healthcare professional who focuses on holistic and personalized approaches. Taking action against fatigue early can lead to better blood sugar control and enhance your overall quality of life. Remember, addressing both blood sugar management and fatigue symptoms together is essential for a comprehensive approach to your health.
Blurred Vision: A Surprising Indicator of Type 2 Diabetes
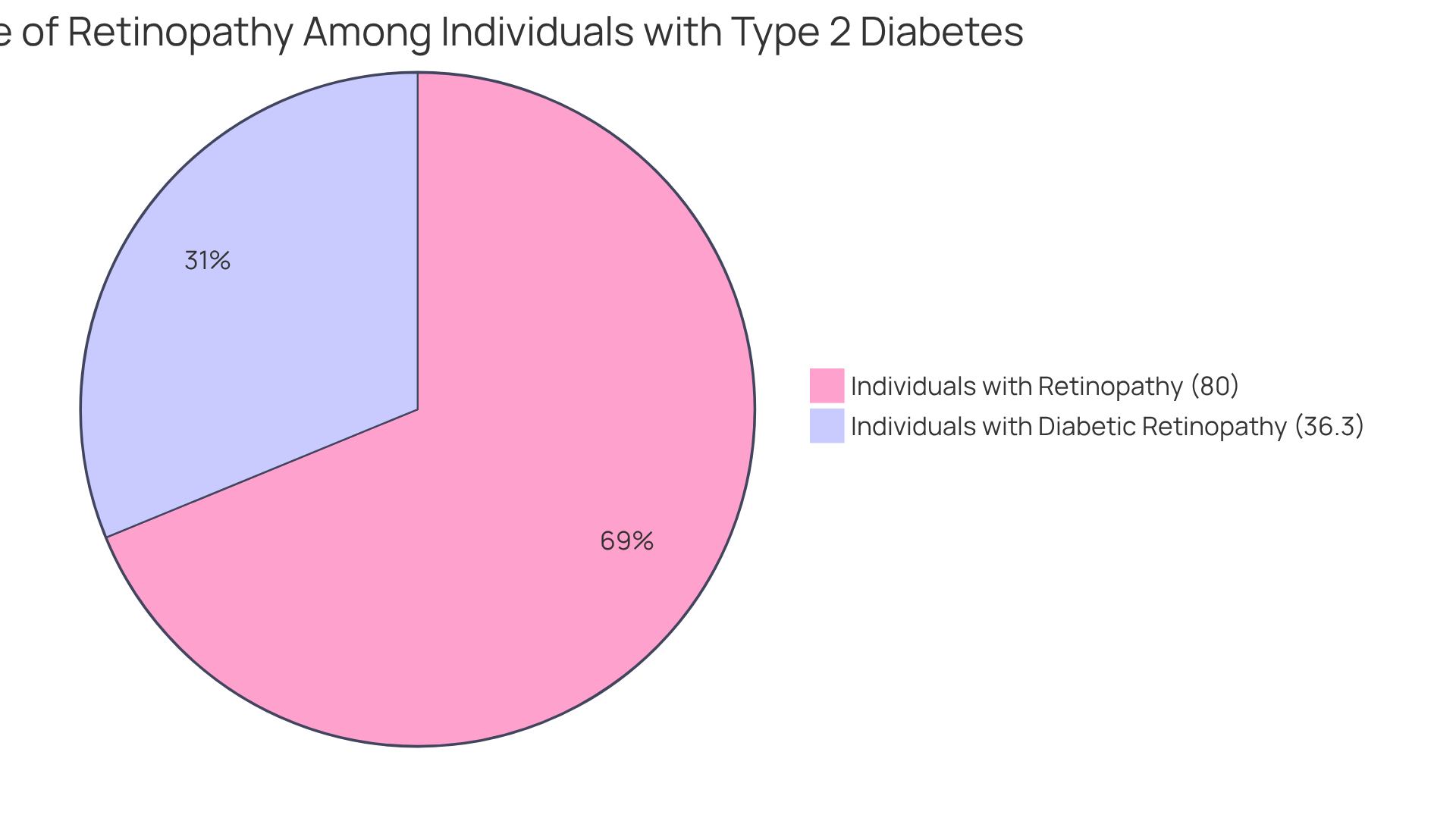
Blurred eyesight can be a significant yet often overlooked sign of diabetes. When blood sugar levels rise, the lens of the eye can swell, leading to temporary changes in vision. It’s concerning to note that about 80% of individuals with type 2 diabetes may experience some form of retinopathy, which can present as blurred vision. A study highlighted that 36.3% of those with diabetes encountered diabetic retinopathy, underscoring how common this issue is among those affected.
Many patients report sudden changes in their eyesight, which may indicate sudden onset diabetes type 2, prompting them to seek medical evaluation. It’s important to recognize that ophthalmologists stress the need to manage high blood sugar levels, as uncontrolled diabetes, such as sudden onset diabetes type 2, can lead to serious complications, including vision loss. For instance, an estimated 9.6 million people in the U.S. are affected by diabetic retinopathy, with 1.84 million facing vision-threatening forms of the condition.
Understanding the link between high blood sugar and eyesight is crucial. If you notice any sudden changes in your vision, please consult a healthcare professional to uncover the underlying causes and receive the care you need. This proactive approach can significantly reduce the risks associated with diabetes-related eye diseases. Dr. Jason Shumard’s center is committed to empowering patients through education and personalized care, ensuring you have the tools to manage your health effectively amid the challenges posed by hospital safety concerns. For more information or support, please reach out to the Integrative Wellness Center.
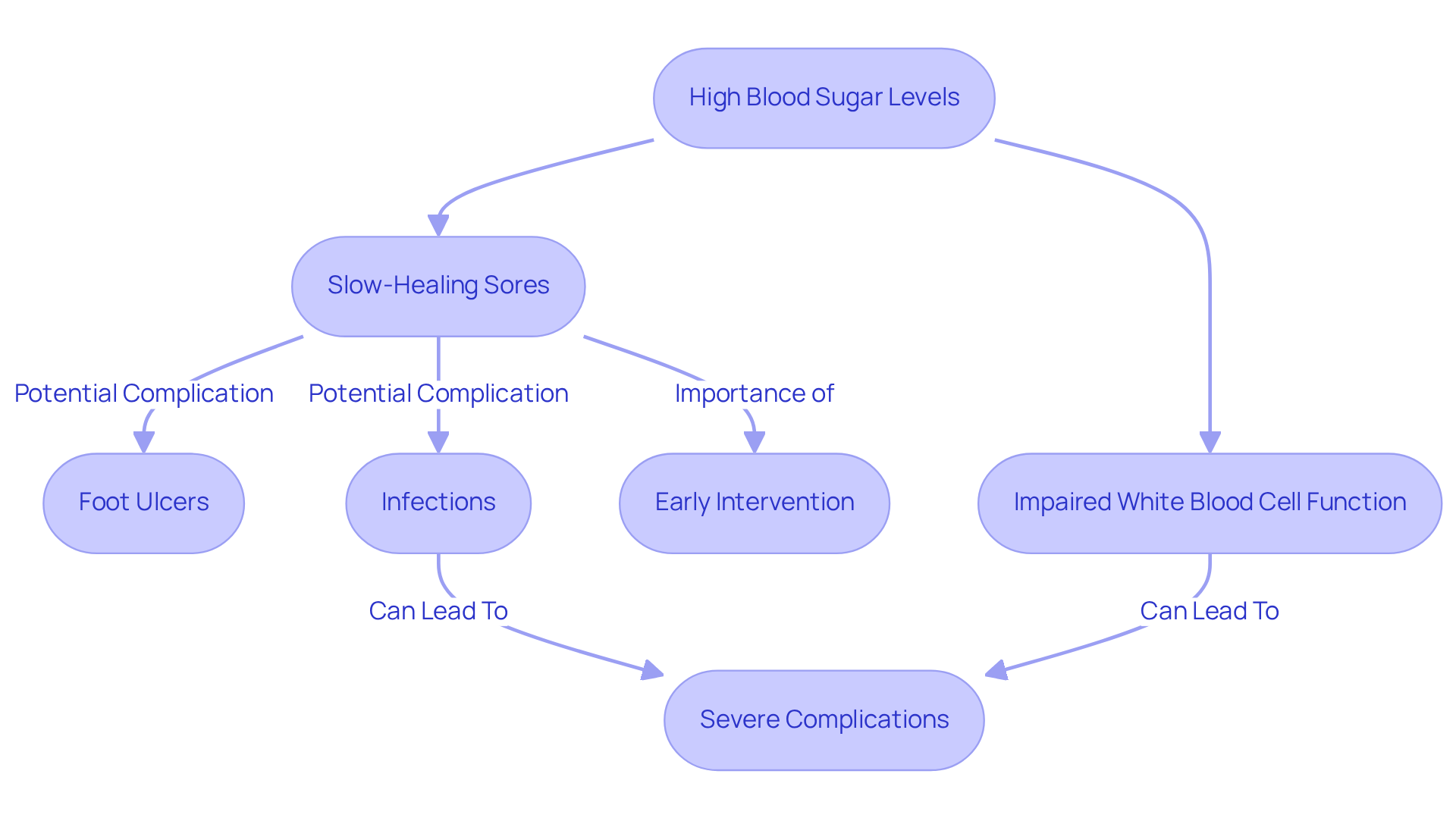
Slow-Healing Sores: A Critical Sign of Type 2 Diabetes
Slow-healing sores can be a significant concern for those living with sudden onset diabetes type 2. Elevated blood sugar levels, which can result from sudden onset diabetes type 2, often hinder circulation and nerve function, leading to delayed wound healing. Did you know that approximately 34% of individuals with high blood sugar will develop a foot ulcer in their lifetime? Alarmingly, 50% of those may face some form of infection. This reality underscores the importance of keeping a close eye on any cuts or sores that take longer than expected to heal.
It’s important to recognize that high blood glucose levels related to sudden onset diabetes type 2 can impair white blood cell function, diminishing the body’s ability to fight infections effectively. Untreated infections can escalate into severe complications, such as gangrene or sepsis, which can be life-threatening. A recent study revealed that the median recovery time for diabetic foot ulcers is around 75.5 days, illustrating the challenges faced by individuals.
Many patients find that slow-healing wounds can lead to serious complications, particularly in those with sudden onset diabetes type 2. For instance, during the COVID-19 pandemic, limited access to healthcare meant that minor injuries sometimes resulted in significant issues. This delay has contributed to increased amputation rates, with 85% to 90% of amputations originating from infected wounds.
Experts emphasize the importance of early intervention and proper wound care. Regular foot inspections and timely consultations with healthcare providers can help prevent severe complications. As one wound care specialist wisely noted, “Prompt treatment of wounds is essential to prevent severe complications.” By being vigilant about slow-healing sores, individuals can take proactive steps to manage their condition and improve their overall health outcomes.
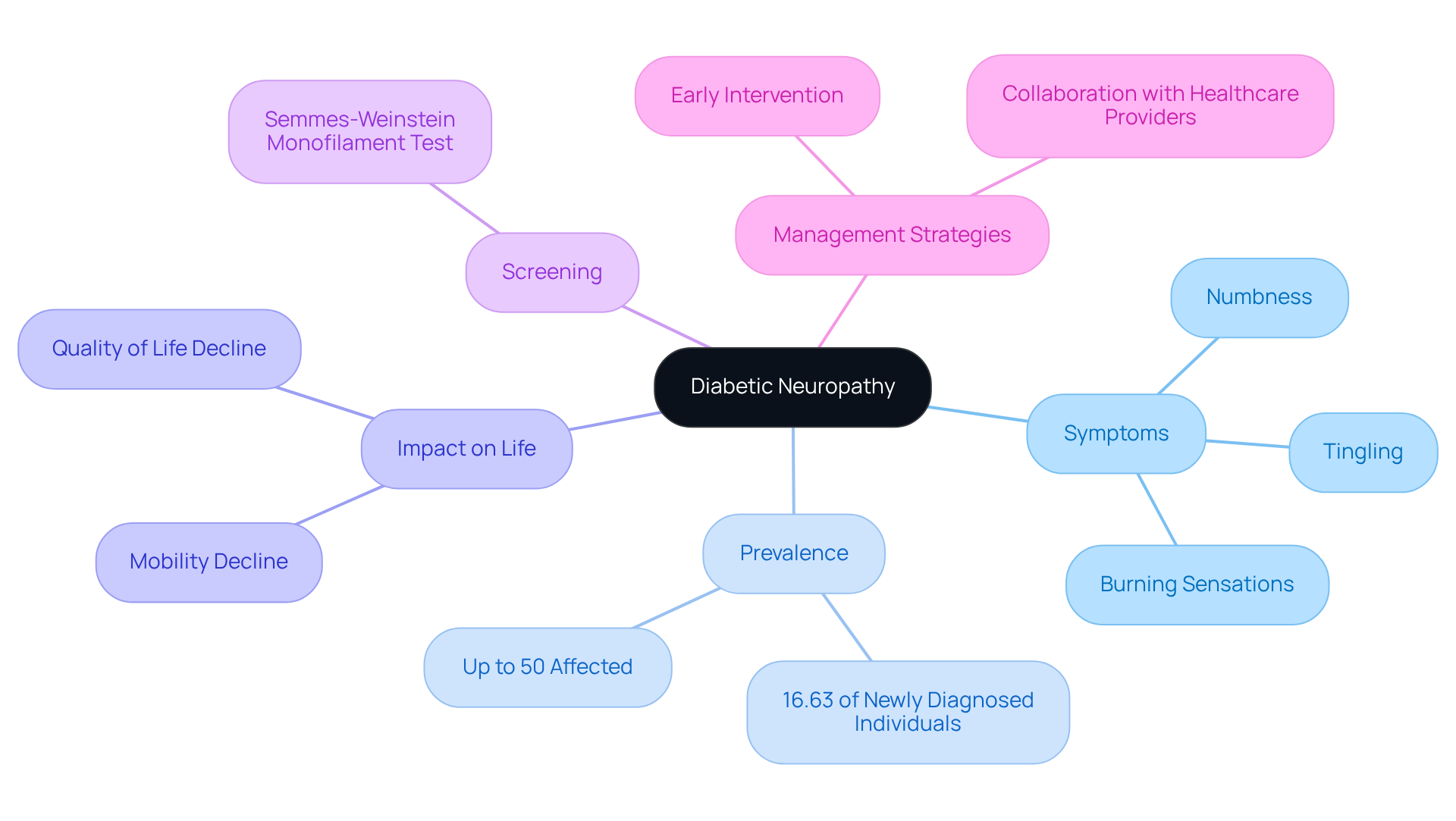
Tingling or Numbness: A Symptom of Sudden Onset Diabetes Type 2
Tingling or numbness, often referred to as neuropathy, can be a concerning indication linked to sudden onset diabetes type 2. Elevated blood sugar levels can lead to nerve damage, resulting in sensations such as tingling, burning, or numbness, particularly in the extremities. It’s important to recognize that studies show over half of diabetic neuropathy cases appear within six years of a diagnosis, emphasizing the need to identify these symptoms promptly. Many patients find that around 16.63% of newly diagnosed individuals with the second type of diabetes experience diabetic neuropathy during follow-up, highlighting how common this condition can be.
Neuropathy can significantly impact daily life, with chronic symptoms affecting mobility and overall quality of life. Neurologists emphasize the importance of early intervention, as untreated neuropathy can lead to complications such as foot ulcers and infections. For instance, a case study revealed that individuals experiencing tingling or numbness often reported a significant decline in their ability to perform daily activities. This reinforces the need for proactive management to maintain a fulfilling life.
Statistics indicate that diabetic neuropathy impacts up to 50% of individuals with type 2 diabetes, making it one of the most prevalent complications of the condition. The Semmes-Weinstein monofilament test is a straightforward yet effective screening tool for recognizing individuals at risk for diabetic foot complications, enabling timely intervention.
In real-life situations, many individuals describe their experiences with tingling and numbness as alarming, prompting them to seek medical advice. Testimonials from those who have undergone screening and management for neuropathy highlight the transformative impact of early detection and treatment. Neurologists suggest that individuals collaborate closely with healthcare providers to track symptoms and sustain optimal blood glucose levels, which are vital for preventing further nerve damage. By understanding the implications of tingling or numbness, patients can take proactive steps toward managing their condition effectively.
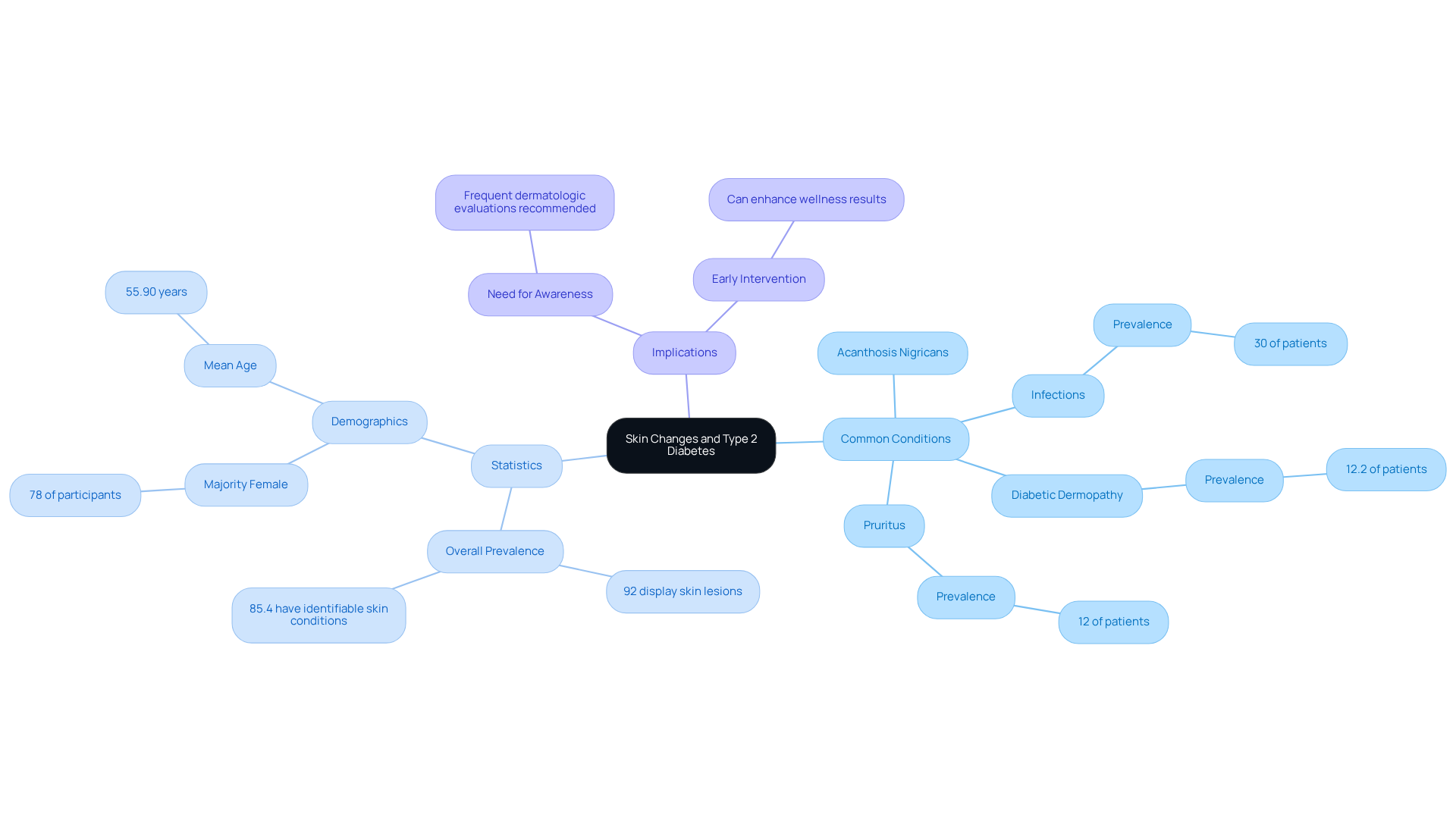
Skin Changes: Surprising Signs of Type 2 Diabetes You Shouldn’t Ignore
Skin alterations, such as dark spots or infections, can be unexpected signs of type 2 diabetes. It’s important to recognize that high blood sugar levels may lead to various skin conditions, notably acanthosis nigricans, which is characterized by velvety dark patches in body folds. This condition often links to insulin resistance and can serve as an early warning sign of diabetes. Many patients find that understanding these signs is crucial for their health.
Research indicates that skin disorders are common among individuals with diabetes, with studies showing that up to 92% display identifiable skin lesions. Common manifestations include:
- Infections
- Diabetic dermopathy
- Pruritus
Infections occur in at least 30% of diagnosed cases. Dermatologists emphasize the importance of recognizing these skin changes, as they can reflect underlying metabolic issues. For instance, a study found that 61% of diabetic patients had idiopathic guttate hypomelanosis, a skin condition that can signal poor glycemic control.
If you observe unusual skin changes, it is essential to seek a medical professional for assessment and management. Remember, early intervention can greatly enhance your wellness results. Taking action now can lead to a healthier future.
Seek Medical Advice: Essential Action for Recognizing Signs of Type 2 Diabetes
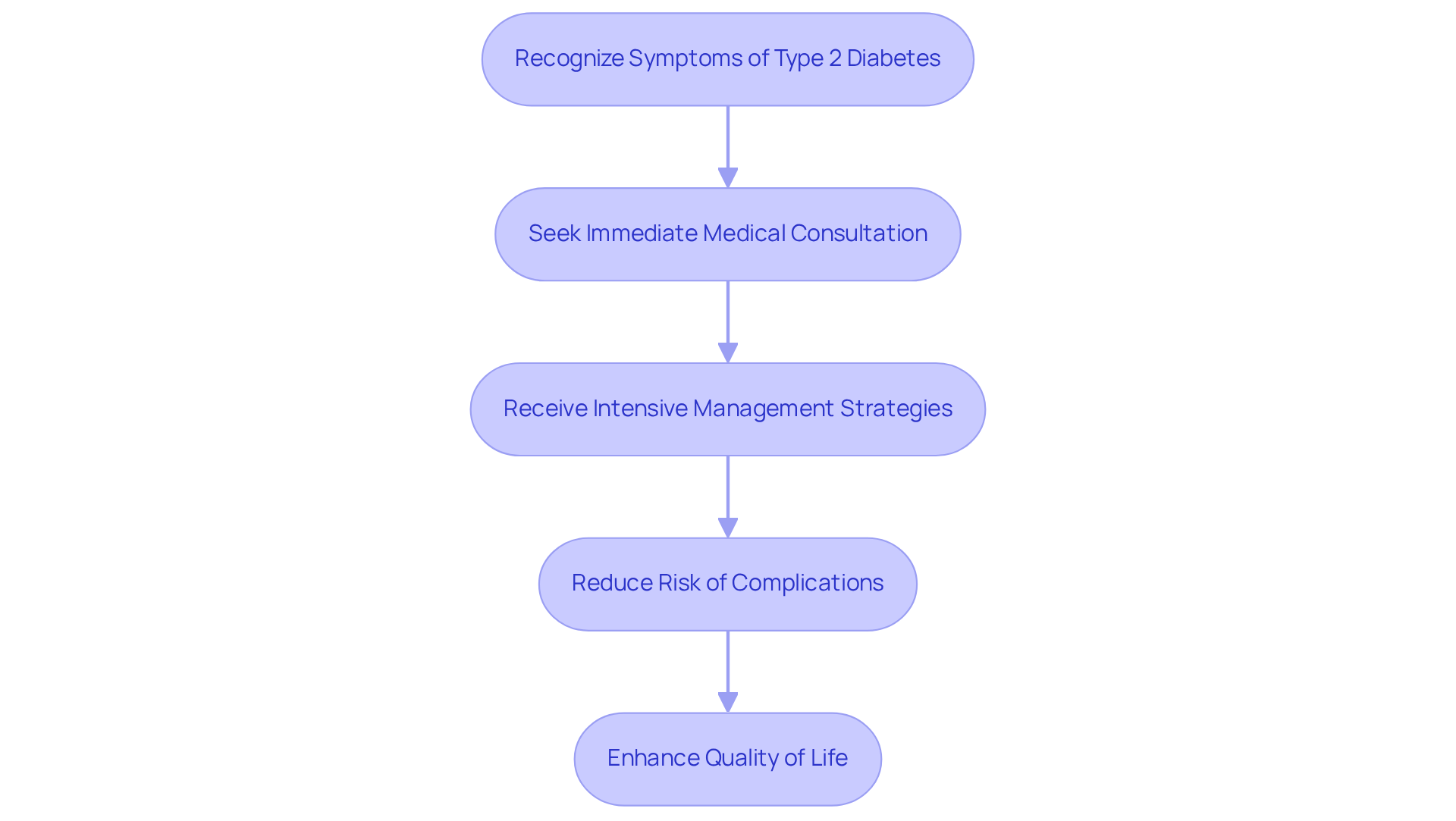
Identifying the symptoms of sudden onset diabetes type 2 can be overwhelming, and seeking immediate medical consultation is crucial. It’s important to recognize that timely identification and action can significantly improve health outcomes and reduce complications associated with sudden onset diabetes type 2. Did you know that statistics show timely medical advice can lower the risk of severe complications? Studies highlight that intensive management strategies not only reduce mortality rates but also enhance quality of life. For instance, individuals who engage in proactive management of their condition often report fewer microvascular and macrovascular complications.
Many patients find that they only seek medical advice after noticing symptoms, which underscores the need for increased awareness and education. Regular check-ups and open communication with healthcare providers are essential for effective diabetes management. This approach empowers patients to take control of their health and make informed decisions about their care. Remember, you are not alone on this journey; support is available to help you navigate your path to better health.
Conclusion
Recognizing the signs of sudden onset diabetes type 2 is crucial for timely intervention and effective management. Increased thirst, frequent urination, unexplained weight loss, fatigue, blurred vision, slow-healing sores, tingling or numbness, and skin changes are all key symptoms that should not be ignored. Each of these indicators serves as a warning signal, and addressing them promptly can help prevent serious complications.
It’s important to acknowledge the struggles that many individuals face when dealing with these symptoms. Proactive health management is essential, and seeking medical advice upon noticing these signs can significantly improve health outcomes. Programs like the 30-Day Diabetes Reset Program at the Integrative Wellness Center offer valuable resources and support for those looking to take control of their diabetes management. With a focus on personalized care, nutritional guidance, and lifestyle changes, these programs emphasize the importance of a supportive community.
Ultimately, awareness and early action are key to navigating the challenges of sudden onset diabetes type 2. Many patients find that consulting healthcare professionals for a comprehensive evaluation opens up a path to better health. It’s a journey that can lead to a healthier, more fulfilling life, and individuals are encouraged to explore available resources that can aid in transforming their health. Taking that first step towards understanding and managing diabetes is a powerful move toward a brighter future.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at the Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a transformative program designed to help individuals manage sudden onset type 2 diabetes through personalized coaching, nutritional guidance, and educational resources. It focuses on empowering participants to make sustainable lifestyle changes and control their well-being.
How does the program help in managing blood sugar levels?
The program provides essential resources to stabilize glucose levels without relying on insulin or prescription medications. It emphasizes behavior change and comprehensive well-being, which can significantly improve the management of blood sugar levels.
What additional resources are included in the program?
Participants have access to seminars and Dr. Shumard’s books, which offer insights into reversing type 2 diabetes and achieving optimal wellness.
What are the common symptoms of sudden onset type 2 diabetes?
Common symptoms include increased thirst (polydipsia) and frequent urination (polyuria). Increased thirst occurs due to dehydration from high blood sugar levels, while frequent urination results from the kidneys filtering excess glucose.
What should I do if I experience increased thirst or frequent urination?
If you experience excessive thirst or frequent urination, it is advisable to consult a healthcare professional for further evaluation to rule out any serious health issues or underlying conditions.
How can Dr. Jason Shumard assist in managing diabetes?
Dr. Jason Shumard offers personalized guidance and support to help patients navigate the challenges of managing diabetes. He is committed to transforming healthcare and assisting individuals in their journey towards reversing type 2 diabetes.
How can I get started with the 30-Day Diabetes Reset Program?
You can reach out to the Integrative Wellness Center to discover more about the program and take the first step towards improved well-being.