Overview
Managing diabetes can feel overwhelming at times, but there are effective strategies that can help you take control of your health. The article outlines eight key strategies for navigating your journey through an American diabetic diet plan. It emphasizes the importance of personalized nutritional guidance, carbohydrate counting, and regular monitoring of blood sugar levels.
Many patients find that using the Plate Method for portion control and incorporating fiber into their meals helps them stabilize blood sugar levels. Each strategy is backed by evidence showcasing its effectiveness in improving overall health outcomes. It’s important to recognize that these approaches empower you to take charge of your diabetes management, fostering a sense of autonomy and well-being.
As you explore these strategies, remember that you’re not alone in this journey. Each step you take towards understanding your dietary needs is a step towards better health. With the right support and knowledge, you can make informed choices that benefit your lifestyle. Let’s embrace this journey together, focusing on small, manageable changes that can lead to significant improvements in your health.
Introduction
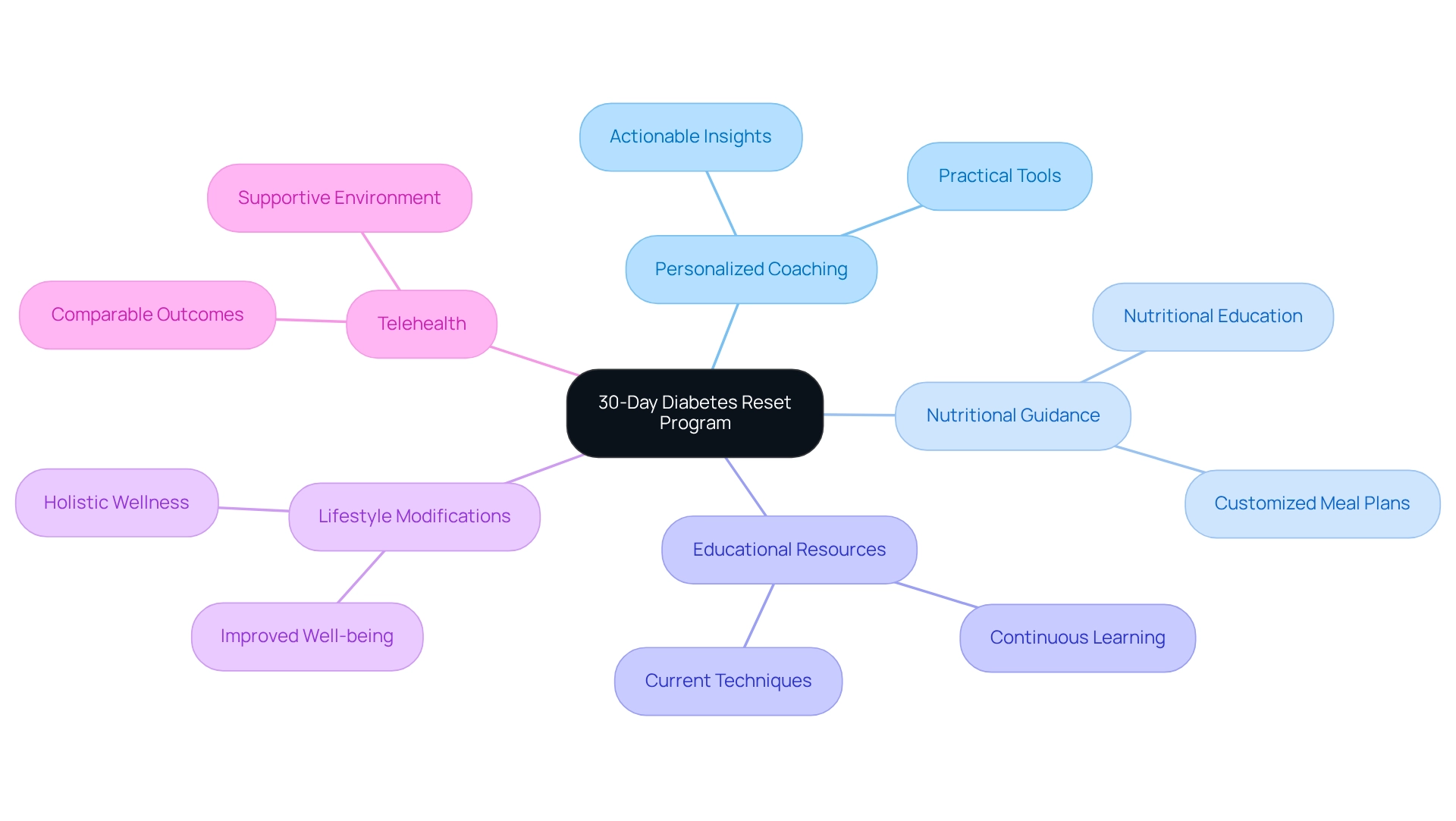
In a world where diabetes affects millions, it’s crucial to recognize the struggles faced by those living with this condition. The Integrative Wellness Center’s 30-Day Diabetes Reset Program stands as a beacon of hope for individuals seeking to regain control of their health. This innovative program goes beyond traditional methods, offering a comprehensive approach that combines personalized coaching, tailored nutrition, and ongoing education. Many patients find that this empowers them on their journey to better health.
By addressing the underlying causes of diabetes rather than merely managing symptoms, participants are equipped with the essential tools for sustainable lifestyle changes. Success stories abound, highlighting the program’s effectiveness in stabilizing blood sugar levels while fostering a supportive environment where holistic wellness can flourish. As individuals embark on this transformative path, they can envision a future free from the burdens of medication and complications, ultimately reclaiming their vitality and well-being. Isn’t it time to take that first step toward a healthier, more fulfilling life?
Integrative Wellness Center: 30-Day Diabetes Reset Program for Lasting Health Transformation
At the Integrative Wellness Center, we understand that managing diabetes can be a challenging journey. That’s why our 30-Day Diabetes Reset Program is designed to help you regain your well-being through a multifaceted approach. This innovative, clinically validated program offers personalized coaching and customized nutritional guidance, along with a wealth of educational resources. We equip you with essential tools for a sustainable wellness transformation.
It’s important to recognize that simply easing symptoms isn’t enough. Our program addresses the underlying factors of diabetes, encouraging substantial lifestyle modifications that can lead to improved well-being. Many patients find that those who engage in telehealth experience comparable positive health outcomes as those attending in-person appointments, showcasing the program’s effectiveness.
Imagine a supportive environment that fosters holistic wellness, enhancing your quality of life while reducing reliance on conventional medical treatments. Have you ever thought about how continuous learning can play a role in managing your health? Our program emphasizes this, ensuring that both you and your healthcare professionals are equipped with the most current information and techniques.
Picture stabilizing your glucose levels without depending on insulin or prescription drugs. You can avoid costly treatment regimens, experience renewed energy, and alleviate the anxiety surrounding potential complications of your condition. This transformation is within your reach, and we are here to support you every step of the way!
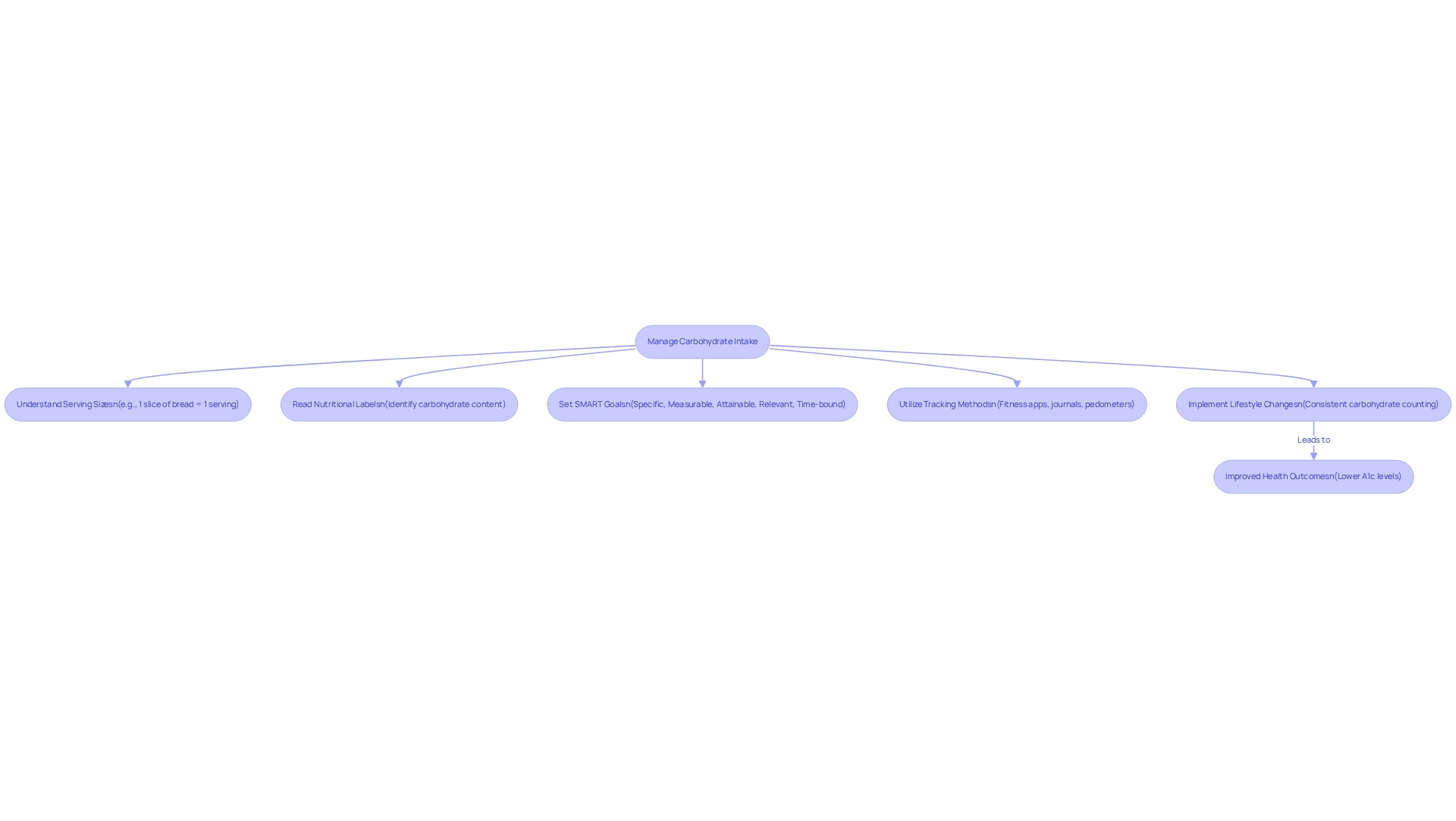
Count Carbohydrates: Understand Serving Sizes and Nutritional Labels
Counting carbohydrates is a fundamental practice in the American diabetic diet plan for effectively managing blood sugar levels. It’s important to recognize that understanding serving sizes and mastering the art of reading nutritional labels can empower you to make informed dietary choices. Maintaining a consistent carbohydrate intake at each meal is advisable as part of an American diabetic diet plan, as this approach helps stabilize blood sugar levels. Familiarity with common serving sizes—such as one slice of bread or half a cup of rice—can significantly enhance your ability to monitor carbohydrate consumption throughout the day.
Many patients find that visual references can be incredibly helpful. For instance, research indicates that half a cup is roughly equivalent to the size of your cupped hand. This practical tip aligns with Dr. Jason Shumard’s methodologies, which highlight actionable insights and practical tools for patients to regain their well-being through effective goal-setting and progress tracking. Implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost your focus and motivation in managing carbohydrate intake. For example, setting a goal to consistently track your carbohydrate consumption at each meal can lead to improved blood glucose control.
To aid in tracking, consider utilizing various methods such as fitness apps, journals, and pedometers. These tools can assist you in monitoring daily carbohydrate consumption and physical activity levels, offering a thorough method for addressing your condition. Additionally, expert advice underscores the importance of counting carbohydrates as part of an American diabetic diet plan, as it directly influences blood glucose levels. Dr. Josh Axe emphasizes that health encompasses the life gained, not merely the weight lost, reinforcing the notion that mindful eating as part of an American diabetic diet plan can lead to improved health outcomes.
Case studies reveal that lifestyle changes, including effective carbohydrate counting in the American diabetic diet plan, can lead to lower A1c levels, a crucial metric for diabetes management. For example, individuals who embraced consistent carbohydrate counting techniques reported substantial enhancements in their A1c levels, showcasing the efficacy of these lifestyle changes. By implementing these strategies, you can take proactive steps toward better health, ultimately reclaiming your well-being and reducing reliance on conventional medical interventions. Understanding nutritional labels is also essential, as it allows you to make informed choices that align with your dietary needs.
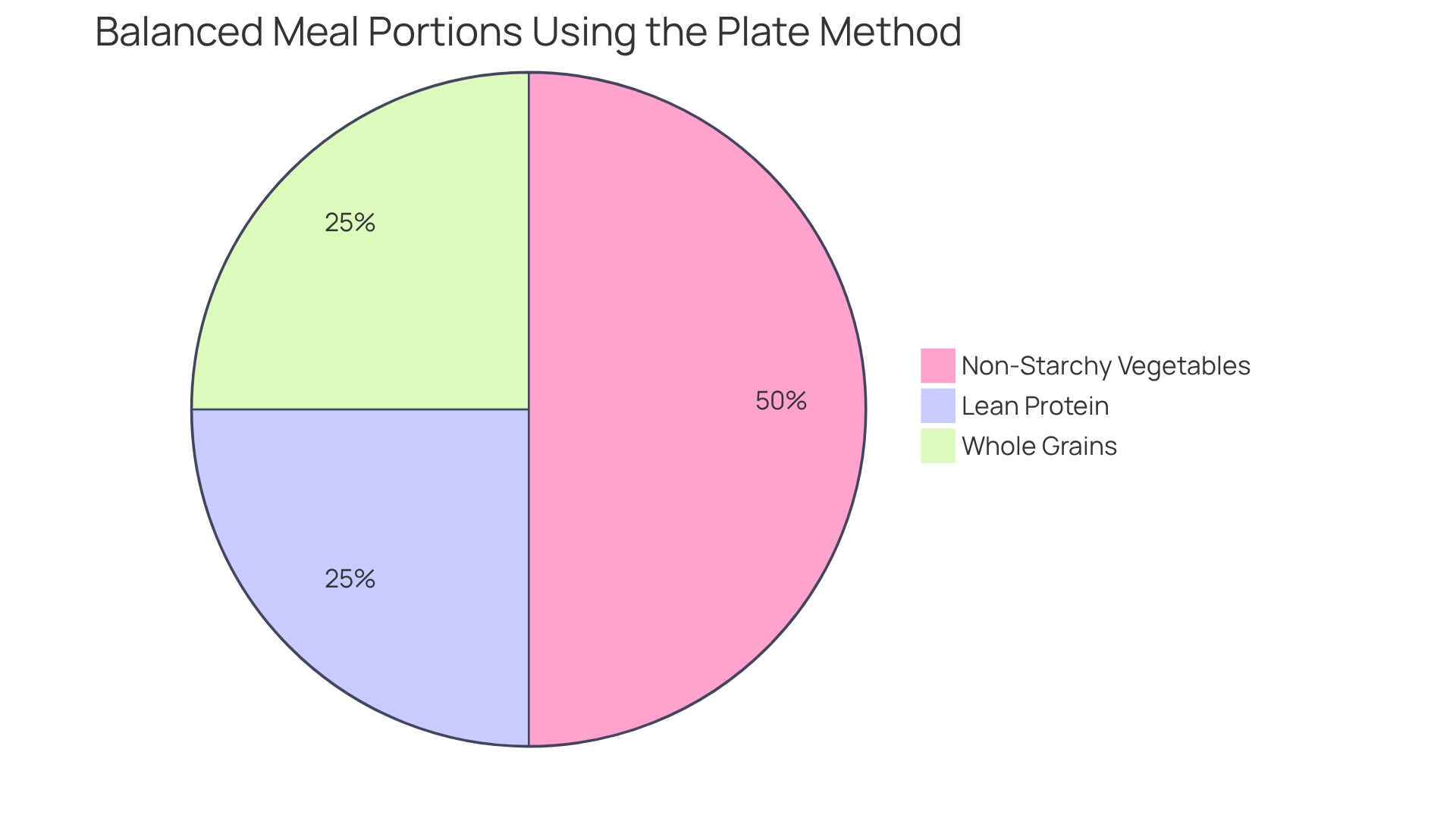
Use the Plate Method: Visualize Your Meal Portions for Balanced Nutrition
The Plate Method serves as a valuable tool for visualizing meal portions, which is essential for effectively managing blood sugar. By thoughtfully dividing your plate into three sections—half for non-starchy vegetables, a quarter for lean protein, and a quarter for whole grains—you can create balanced meals that not only support blood sugar control but also promote nutritional diversity. This approach encourages the inclusion of vital nutrients while simplifying portion control, making it easier for you to adhere to dietary guidelines.
It’s important to recognize that structured meal planning, like the Plate Method, significantly enhances your understanding of portion sizes. Many patients find that using this method allows them to grasp portion sizes quickly and apply them in their daily lives. Research indicates that participants using the Plate Method spent an average of 17.3 minutes on education, compared to 38.6 minutes for those relying on traditional counting methods. This efficiency underscores the Plate Method’s effectiveness in diabetes management.
To further support your progress, consider utilizing tools such as fitness apps, journals, and pedometers. By consistently tracking your meals and physical activity, you can gain clearer insight into your dietary habits and identify areas for improvement.
Dr. Jason Shumard emphasizes, “By offering individuals actionable insights and practical tools, the center cultivates a setting where people can regain their wellness and well-being.” This sentiment resonates in case studies from Dr. Shumard’s center, where individuals report enhanced health outcomes and a greater sense of empowerment through the use of the Plate Method and organized goal-setting strategies.
For instance, you might set a SMART goal to include at least one serving of non-starchy vegetables in every meal for a week, gradually increasing to two servings. Nutritionists highlight that visualizing meal portions can lead to better dietary choices, reinforcing the importance of this method in your daily meal planning. By adopting the Plate Method and establishing SMART goals, you can effectively manage your condition with the American diabetic diet plan while enjoying a variety of foods, ultimately leading to a healthier lifestyle.
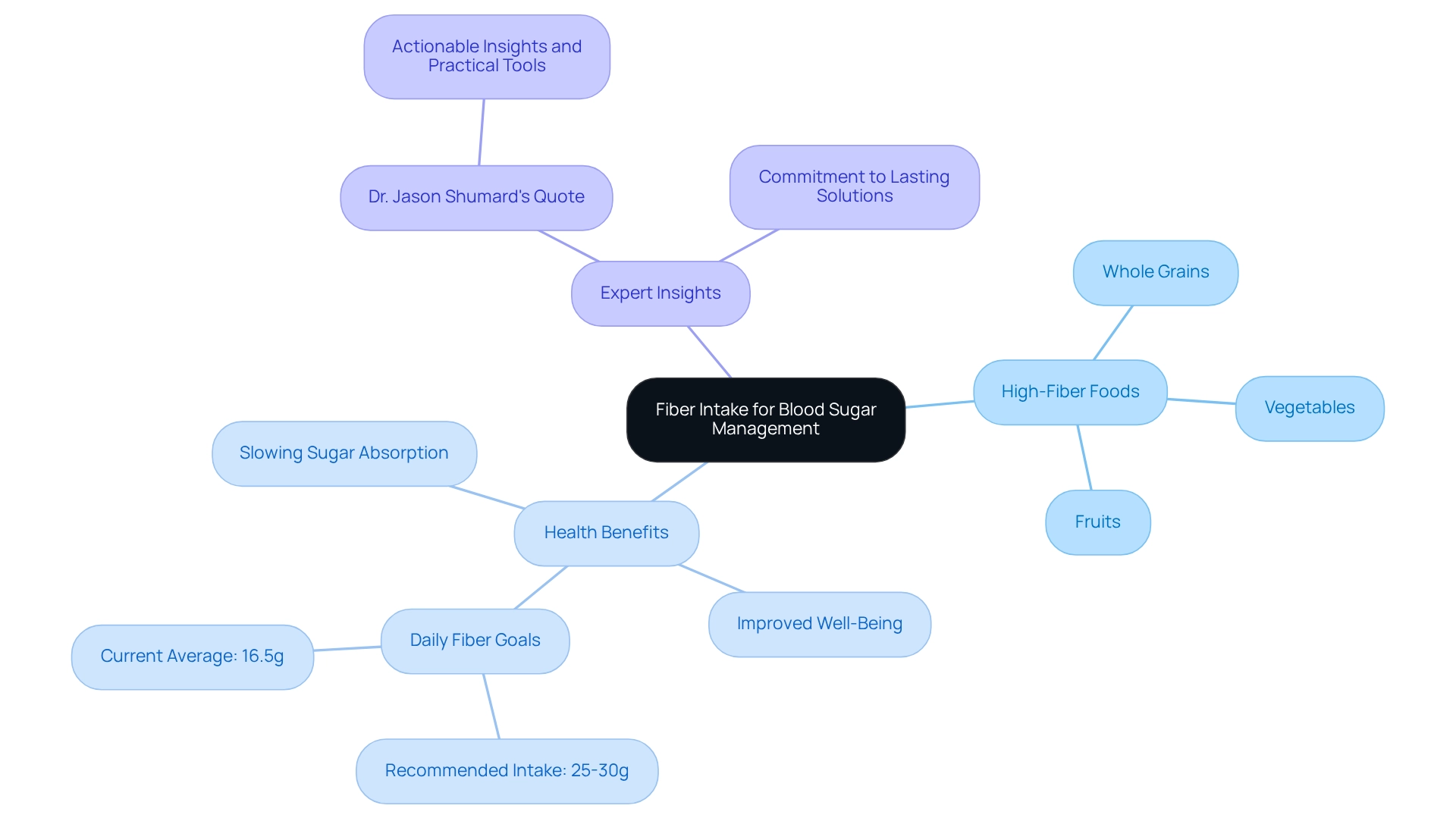
Incorporate Fiber: Choose Whole Grains, Fruits, and Vegetables
Incorporating fiber into your diet is essential for effective blood sugar management. High-fiber foods, such as whole grains, fruits, and vegetables, play a vital role in slowing sugar absorption and enhancing blood sugar control. Research indicates that a habitual fiber intake of around 25-30 grams per day can significantly benefit individuals with type 2 diabetes. It’s important to recognize that a study from the UK Biobank discovered that an average fiber intake of around 16.5 grams daily is linked to better well-being outcomes, emphasizing the significance of striving for greater fiber intake.
Many patients find that to achieve this, opting for whole grain bread instead of white bread and ensuring meals are abundant in leafy greens and legumes can be incredibly helpful. These choices not only assist with blood sugar management but also enhance overall well-being, making fiber a fundamental element of an American diabetic diet plan. As Dr. Jason Shumard emphasizes, ‘By offering individuals with actionable insights and practical tools, the center cultivates an environment where they can reclaim their health and well-being, ultimately resulting in enhanced quality of life and decreased dependence on traditional medical interventions.’ This commitment to lasting solutions underscores the importance of fiber intake in managing diabetes effectively.
Dr. Shumard, who has nearly 20 years of experience and postgraduate education in functional endocrinology and clinical nutrition, leads the Integrative Wellness Center in San Diego, where personalized nutrition plans are designed to empower patients. His 30-Day Diabetes Reset program exemplifies how following an American diabetic diet plan can lead to transformative lifestyle changes, as demonstrated by success stories from individuals who have experienced significant wellness improvements. To discover more about how you can manage your well-being, consider calling Integrative Wellness Center at 858-564-7081 or signing up for our upcoming event to receive Dr. Shumard’s book for free.
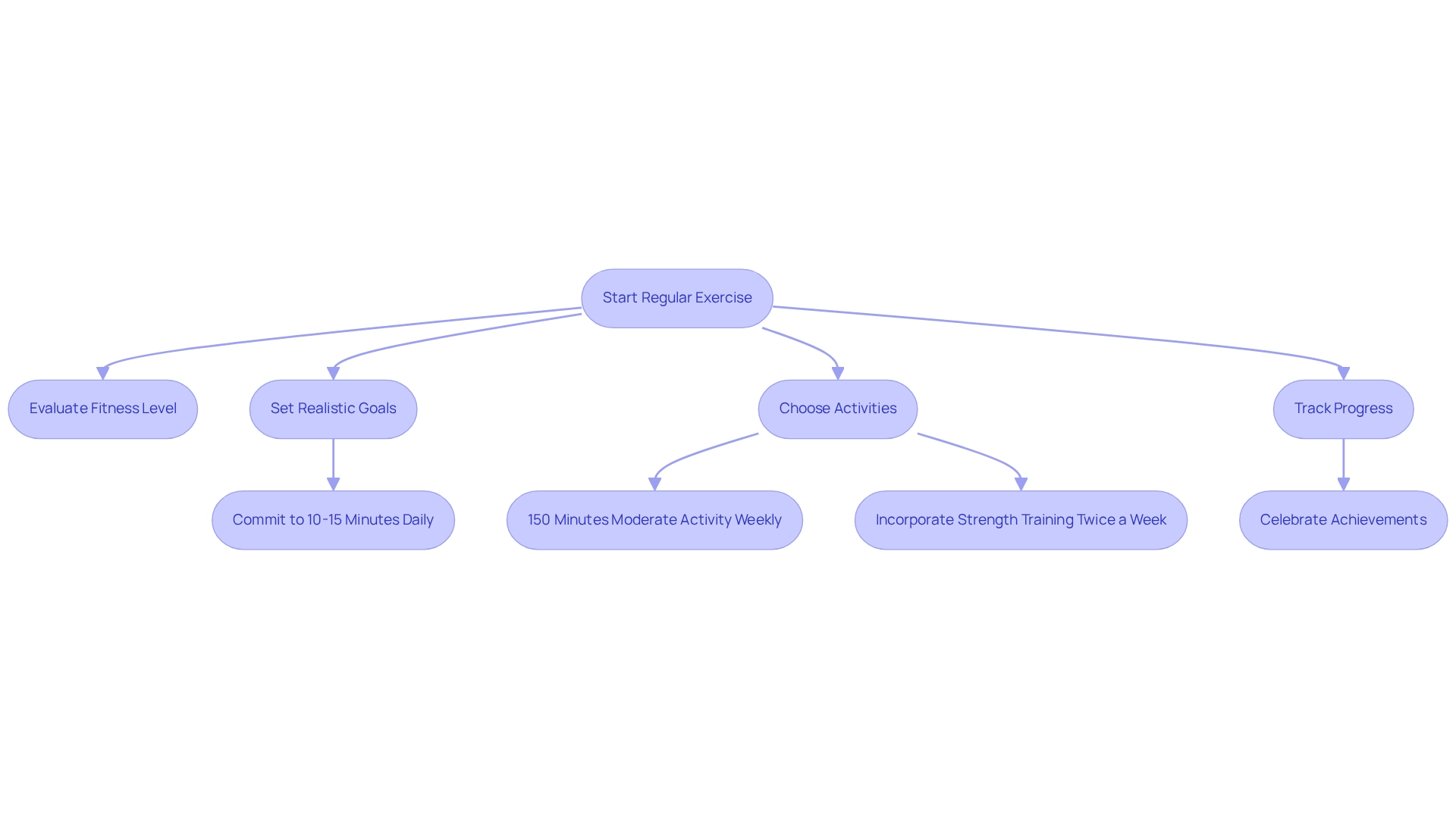
Engage in Regular Exercise: Boost Your Metabolism and Control Blood Sugar
Regular exercise plays a vital role in managing diabetes effectively. It not only boosts metabolism but also enhances insulin sensitivity and helps regulate blood sugar levels. If you’re looking to start a walking routine, consider referring to the structured walking program PDF. It’s essential to first evaluate your current fitness level and set realistic goals, such as committing to a daily walk of just 10-15 minutes. Aim for at least 150 minutes of moderate aerobic activity each week, like brisk walking or cycling, to truly reap these benefits. Additionally, incorporating strength training at least twice a week can further bolster your metabolic function and assist with weight management.
It’s important to recognize that increased physical activity can lead to significant improvements in insulin sensitivity. For example, a study titled “Role of Capillarisation in Insulin Sensitivity” found that aerobic exercise and weight loss can enhance capillary density, which is crucial for improving insulin sensitivity, especially in older adults with impaired glucose tolerance. This underscores the importance of regular exercise in achieving long-term metabolic well-being.
Many patients find that tracking progress is incredibly beneficial. Utilizing a journal or an app can help you stay motivated and celebrate your achievements along the way. Statistics reveal that even small changes in activity levels can lead to substantial effects; for instance, just one extra hour of inactivity over an eight-day period is linked to a 22% increase in the likelihood of developing type 2 metabolic disorder among adults aged 45-70. This statistic highlights the importance of reducing sedentary time and integrating more physical activity into your daily routine.
Success stories are everywhere, with numerous individuals experiencing remarkable improvements in their insulin sensitivity through structured exercise programs. For instance, individuals at the Integrative Wellness Center have reported significant wellness improvements, with an impressive 89.5% recognizing the benefits of structured walking programs. These programs not only enhance physical well-being but also empower participants to take charge of their diabetes management. As Dr. Jason Shumard emphasizes, “My dedication to patient education and empowerment, combined with innovative methodologies, offers a unique value proposition in the healthcare landscape.” Fitness professionals also stress that an American diabetic diet plan combined with tailored exercise routines can be particularly beneficial for diabetics, promoting both physical and mental well-being.
Incorporating these exercise recommendations into your lifestyle can lead to improved blood sugar control and overall health. Begin today by establishing attainable objectives for your physical activity, making exercise a fundamental aspect of effective health control.
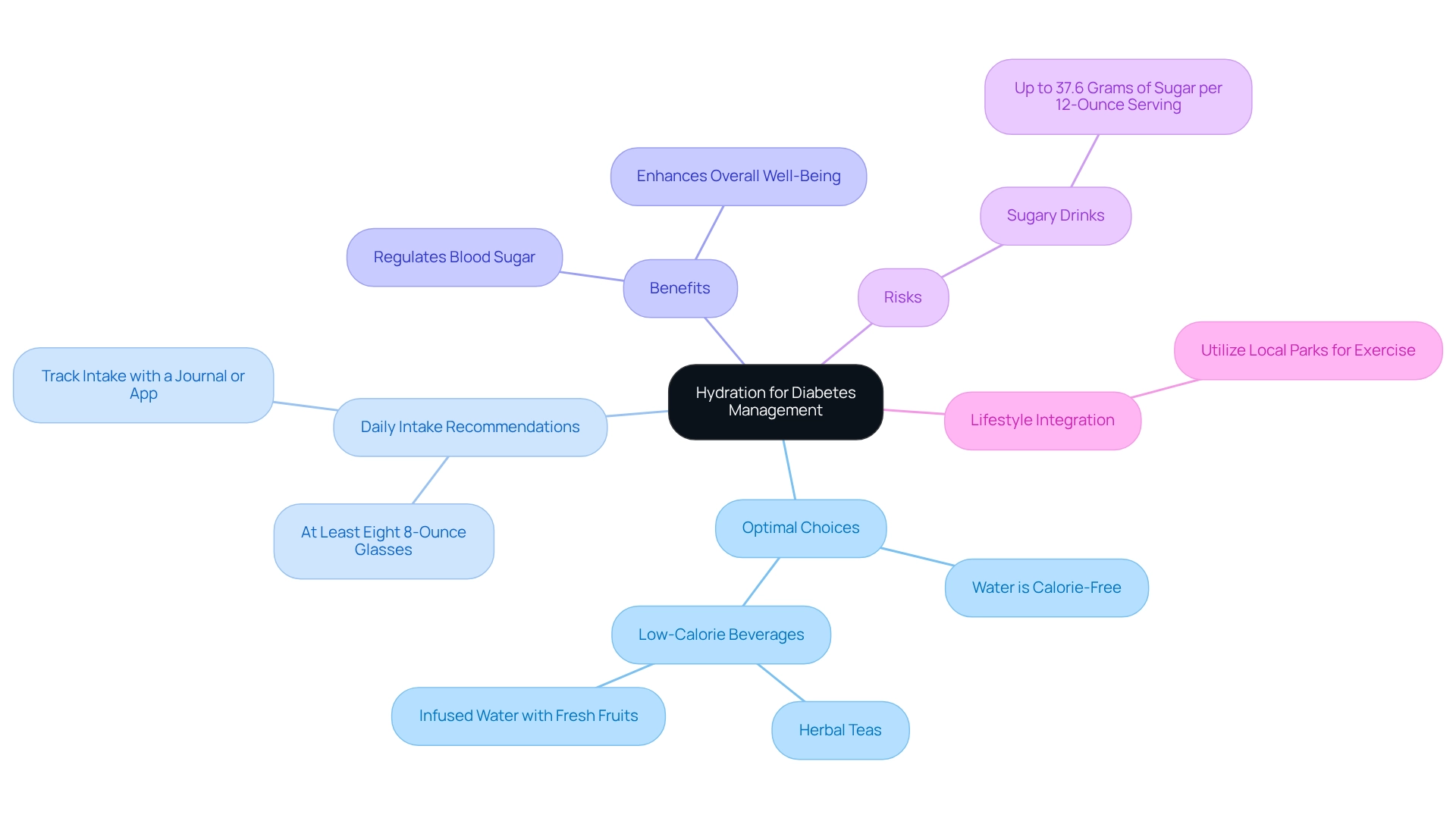
Stay Hydrated: Opt for Water and Low-Calorie Drinks
Staying hydrated is essential for effective diabetes management, especially in the vibrant environment of San Marcos, CA. Water is the optimal choice—calorie-free and sugar-free. It’s recommended to drink at least eight 8-ounce glasses of water each day to promote your well-being and help maintain balanced blood sugar levels. Have you considered tracking your hydration? Using a journal or a fitness app can be a helpful way to log your daily water intake. Alongside water, low-calorie beverages like herbal teas or infused water with fresh fruits can add variety without compromising your health goals.
Proper hydration not only aids in regulating blood sugar but also enhances your overall well-being. Many patients find that insufficient hydration can lead to increased blood glucose levels, making it crucial to prioritize fluid consumption. A case study titled ‘The Importance of Personalized Dietary Advice’ emphasized that customized hydration strategies can significantly improve management outcomes, reinforcing the need for individualized recommendations.
It’s important to recognize that hydration plays a vital role in metabolic functions. Maintaining proper fluid intake can help reduce the risks associated with blood sugar issues. However, be cautious—some energy and sports drinks can contain up to 37.6 grams of sugar per 12-ounce serving, which can drastically elevate blood glucose levels. By integrating these hydration habits into your daily routine, you can take charge of your well-being. Remember, this condition is not just a hardship; it’s also a lesson in resilience and self-care. Furthermore, embracing the local lifestyle by utilizing the area’s parks and trails for regular exercise can further enhance your hydration and overall health.
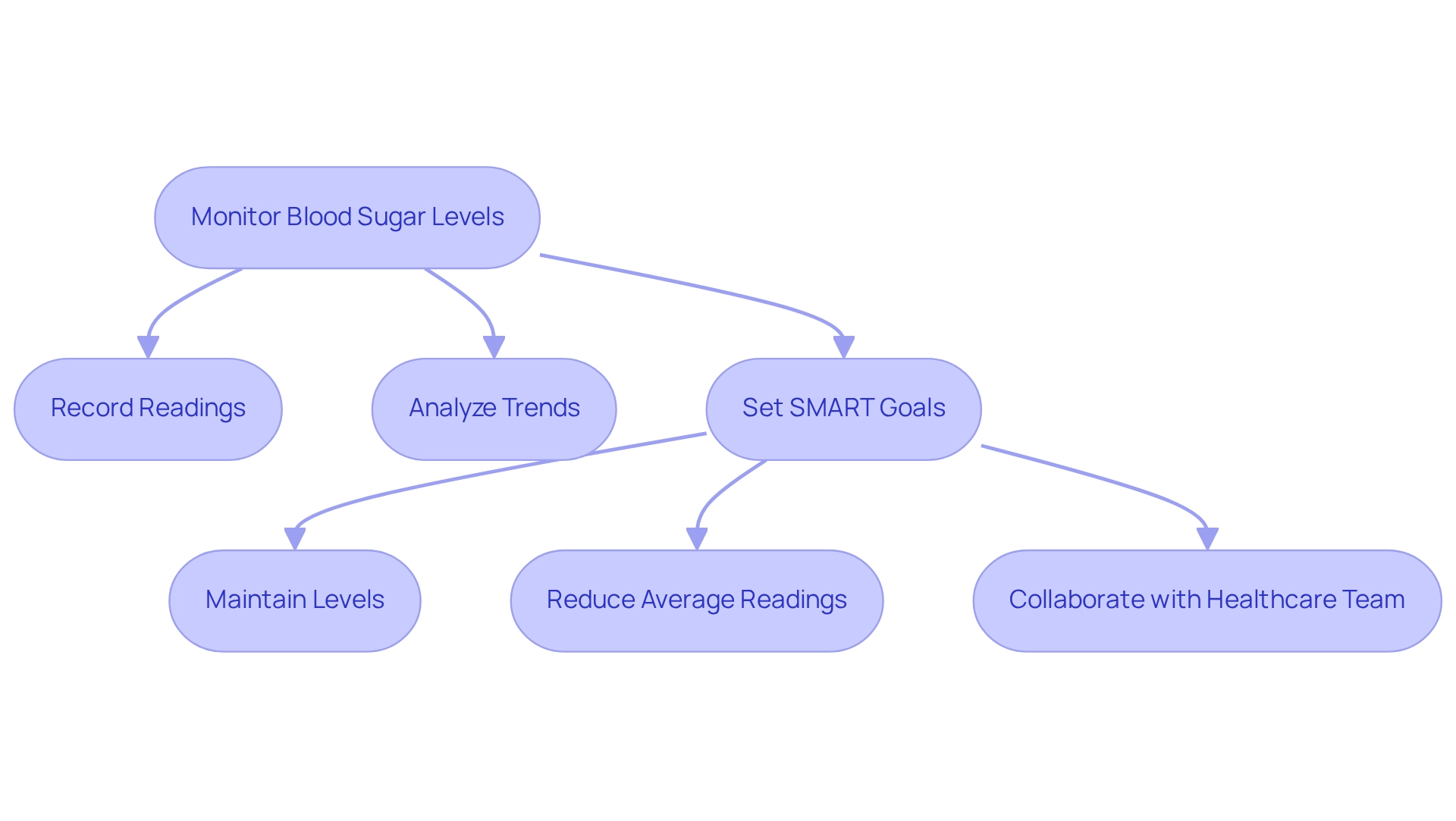
Monitor Blood Sugar: Track Your Levels to Adjust Your Diet Accordingly
Monitoring blood sugar levels is crucial for effective diabetes management. Regular glucose checks empower you to understand how various foods and activities influence your blood glucose levels. By using a glucose meter, you can monitor your readings before and after meals, keeping a thorough record to recognize trends over time. This practice not only informs your dietary choices but also facilitates necessary adjustments to stabilize your blood sugar levels.
It’s important to recognize that tracking your progress can be enhanced by implementing SMART goals—specific, measurable, attainable, relevant, and time-bound. For instance, you might aim to maintain your blood glucose levels within a specific range for a month or reduce your average glucose readings by a certain percentage over a set period. Many patients find that having at least 3–4 days of glucose data is essential to discern meaningful patterns in blood glucose fluctuations. Collaborating with your healthcare team to analyze this data can greatly improve your understanding and strategies. Adam Brown emphasizes that knowing your average glucose, standard deviation, coefficient of variation, and time-in-range are foundational metrics for effective diabetes management.
Effective blood glucose monitoring necessitates your active involvement alongside your healthcare team. Case studies show that the value of blood glucose monitoring is enhanced when you receive prompt feedback on your readings, along with advice on lifestyle changes. For example, the case study titled “Patient Engagement in BGM” emphasizes that effective use of blood glucose monitoring requires your active participation to interpret glucose data and make informed behavioral changes. This collaborative method promotes informed wellness behavior changes, ultimately leading to better management of diabetes.
Incorporating the latest tools for tracking blood glucose, such as FDA-cleared apps, can further streamline this process. These apps not only allow for easier logging of glucose readings but also provide insights and reminders that can help you stay on track with your monitoring. Clinicians are encouraged to enhance their access to these technologies and build confidence in their application within practice. By prioritizing blood sugar monitoring and setting personalized goals, you can take proactive steps toward achieving optimal health outcomes.
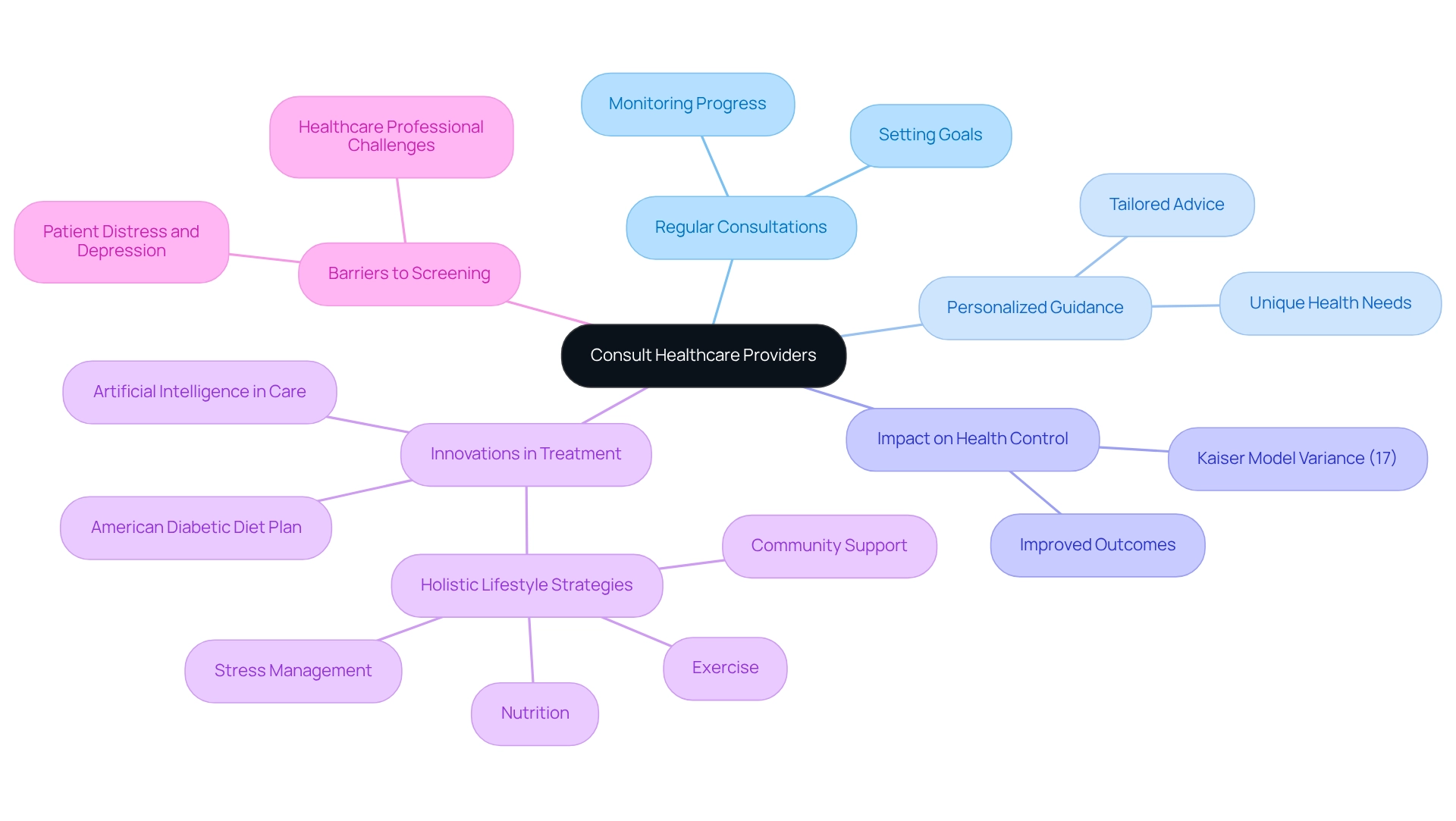
Consult Healthcare Providers: Get Personalized Guidance and Support
Interacting with healthcare professionals is vital for effectively managing blood sugar conditions. Have you had regular consultations with your doctor, dietitian, or diabetes educator? These interactions can provide valuable insights and necessary adjustments to your treatment plan. These professionals are essential in helping you set realistic goals, monitor your progress, and offer tailored advice that fits your unique health needs. It’s important to recognize that statistics show a significant proportion of patients who consult healthcare providers experience improved outcomes, highlighting the importance of professional guidance.
For instance, the Kaiser model accounted for the largest share of variance (17%) in HbA1c levels, underscoring the impact of professional support on health control. Many patients find that recent studies reveal various barriers and enablers healthcare professionals encounter when screening for diabetes-related distress and depression. This emphasizes the need for open communication and support. As Randy Jackson insightfully noted, “With this condition, there are numerous aspects that you discover which you never expected to be interested in, but now that you have this illness, you must deal with it.” By actively seeking help, you empower yourself to navigate your journey more effectively, ultimately enhancing your quality of life.
Additionally, innovations in diabetes treatment, including the American diabetic diet plan along with holistic lifestyle strategies that emphasize nutrition, exercise, community support, and stress management, are transforming personalized care. By fostering a confident patient base, you can support your recovery and contribute to improved outcomes. Remember, you are not alone in this journey, and together with your healthcare team, you can achieve a healthier, more fulfilling life.
Educate Yourself: Understand Diabetes and Its Dietary Implications
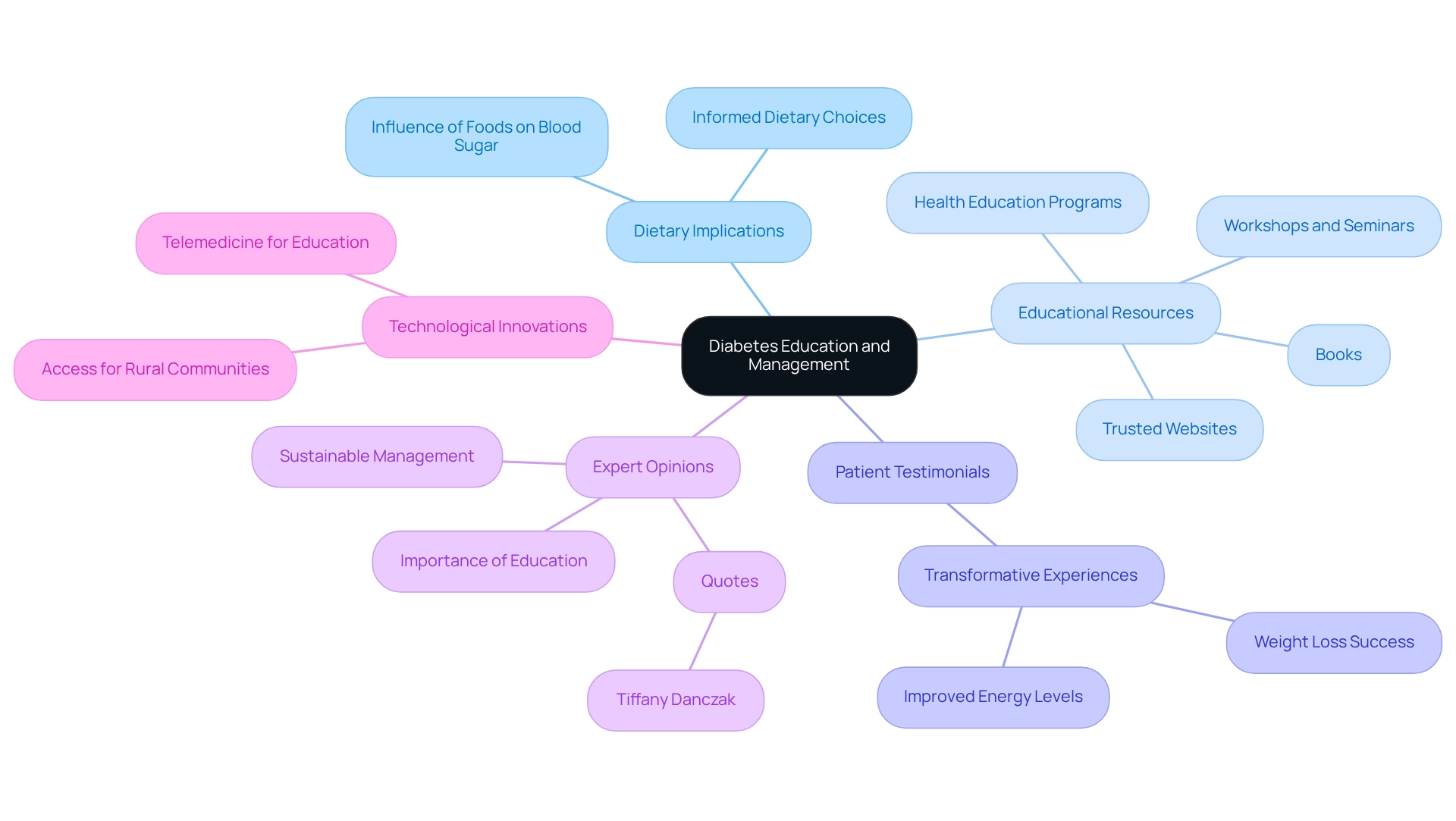
Achieving a comprehensive understanding of this condition and its dietary implications is essential for effective management. It’s important to recognize that knowledge about how various foods influence blood sugar levels empowers you to make informed dietary choices. Engaging with educational materials like books, trusted websites, and health education programs can greatly enhance your understanding. Many patients find that participating in seminars and workshops not only keeps them updated on the latest research but also presents effective strategies for managing blood sugar levels.
Research indicates that individuals who participate in diabetes education are more likely to engage in self-care and preventive health practices, leading to improved health outcomes. For instance, individuals who have completed Dr. Jason Shumard’s 30-Day Diabetes Reset program have shared transformative experiences. One patient shared, “I lost 55 lbs. My A1C started at 9.1 after 8 months; it is now 5.7.” Another noted, “I feel so much better… I lost a lot of weight, have more energy, and feel great.” These testimonials highlight the significant impact of education and a comprehensive approach to managing this condition.
Moreover, specialist views consistently emphasize the essential role of education in managing health conditions, promoting accessible resources that can aid this learning. As Tiffany Danczak wisely stated, “Don’t let yourself fall, you gotta pick yourself right up and strive to do better and be better!” This mindset is crucial, especially considering that this condition is not curable; it’s sustainable. By actively pursuing these educational opportunities, you can make substantial progress toward improved well-being and a more empowered method of managing your condition.
Furthermore, case studies have indicated that individuals who received diabetes education were more inclined to participate in self-care practices, emphasizing the significance of continuous education in attaining improved wellness results. To learn more about how you can transform your health, consider reaching out to the Integrative Wellness Center today.
Conclusion
The Integrative Wellness Center’s 30-Day Diabetes Reset Program offers a transformative opportunity for those seeking to take charge of their health. Recognizing the challenges faced by individuals with diabetes, this program provides personalized coaching, tailored nutrition, and ongoing education. By addressing the root causes of diabetes, participants are empowered to make sustainable lifestyle changes. It’s not just about managing symptoms; it’s about focusing on holistic wellness, stabilizing blood sugar levels, and reducing reliance on medication, ultimately enhancing quality of life.
Key strategies play a vital role in effective diabetes management. Many individuals find that:
- Counting carbohydrates
- Utilizing the Plate Method for balanced nutrition
- Incorporating fiber-rich foods
can make a significant difference. Regular exercise and proper hydration further contribute to improved metabolic health. Additionally, blood sugar monitoring and consultations with healthcare providers ensure that each person receives the personalized support they need. Education stands as a cornerstone of successful diabetes management, enabling informed dietary choices and fostering a proactive approach to health.
In summary, the journey to better health for those living with diabetes is about reclaiming vitality and fostering a lifestyle that promotes well-being. By engaging with the resources available through the Integrative Wellness Center and committing to a comprehensive approach, individuals can envision a future where they thrive without the constraints of diabetes. Taking that first step toward a healthier life is not only possible but also empowering. Remember, you are not alone on this journey; support is available, and a brighter, healthier future awaits.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at the Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a clinically validated program designed to help individuals manage diabetes through personalized coaching, customized nutritional guidance, and educational resources to support sustainable wellness transformation.
How does the program address diabetes management?
The program focuses on addressing the underlying factors of diabetes, encouraging substantial lifestyle modifications rather than just easing symptoms, which can lead to improved well-being.
Can I participate in the program through telehealth?
Yes, many patients find that engaging in telehealth provides comparable positive health outcomes to in-person appointments, showcasing the program’s effectiveness.
What role does continuous learning play in the program?
The program emphasizes continuous learning, ensuring that both participants and healthcare professionals are equipped with current information and techniques for effective diabetes management.
How does the program help stabilize glucose levels?
The program aims to help individuals stabilize their glucose levels without relying on insulin or prescription drugs, potentially reducing treatment costs and alleviating anxiety about complications.
What is the importance of counting carbohydrates in managing diabetes?
Counting carbohydrates is a fundamental practice in the American diabetic diet plan that helps stabilize blood sugar levels by maintaining a consistent carbohydrate intake at each meal.
What tools can assist in tracking carbohydrate consumption?
Tools such as fitness apps, journals, and pedometers can help individuals monitor daily carbohydrate consumption and physical activity levels.
What is the Plate Method and how does it help with portion control?
The Plate Method is a visual tool for meal planning that divides a plate into three sections: half for non-starchy vegetables, a quarter for lean protein, and a quarter for whole grains, helping to create balanced meals and simplify portion control.
How does the Plate Method compare to traditional counting methods?
Research shows that participants using the Plate Method spend less time on education (17.3 minutes) compared to those relying on traditional counting methods (38.6 minutes), indicating its efficiency in diabetes management.
How can setting SMART goals enhance diabetes management?
Setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost focus and motivation in managing carbohydrate intake and overall health outcomes.