Overview
The article titled “10 Key ADA Criteria for Diabetes Mellitus Management” highlights essential guidelines set forth by the American Diabetes Association (ADA) for effective diabetes management. It’s important to recognize that managing diabetes can be challenging, and these criteria aim to empower individuals on their journey.
The article outlines critical diagnostic standards, treatment recommendations, and lifestyle modifications that can significantly improve health outcomes. Supported by evidence from recent research and inspiring patient success stories, it illustrates how adherence to these criteria can lead to better management of diabetes and a healthier life.
Many patients find that making these changes not only helps in managing their condition but also enhances their overall well-being. This nurturing approach provides the necessary support for individuals to take actionable steps toward their health goals.
Introduction
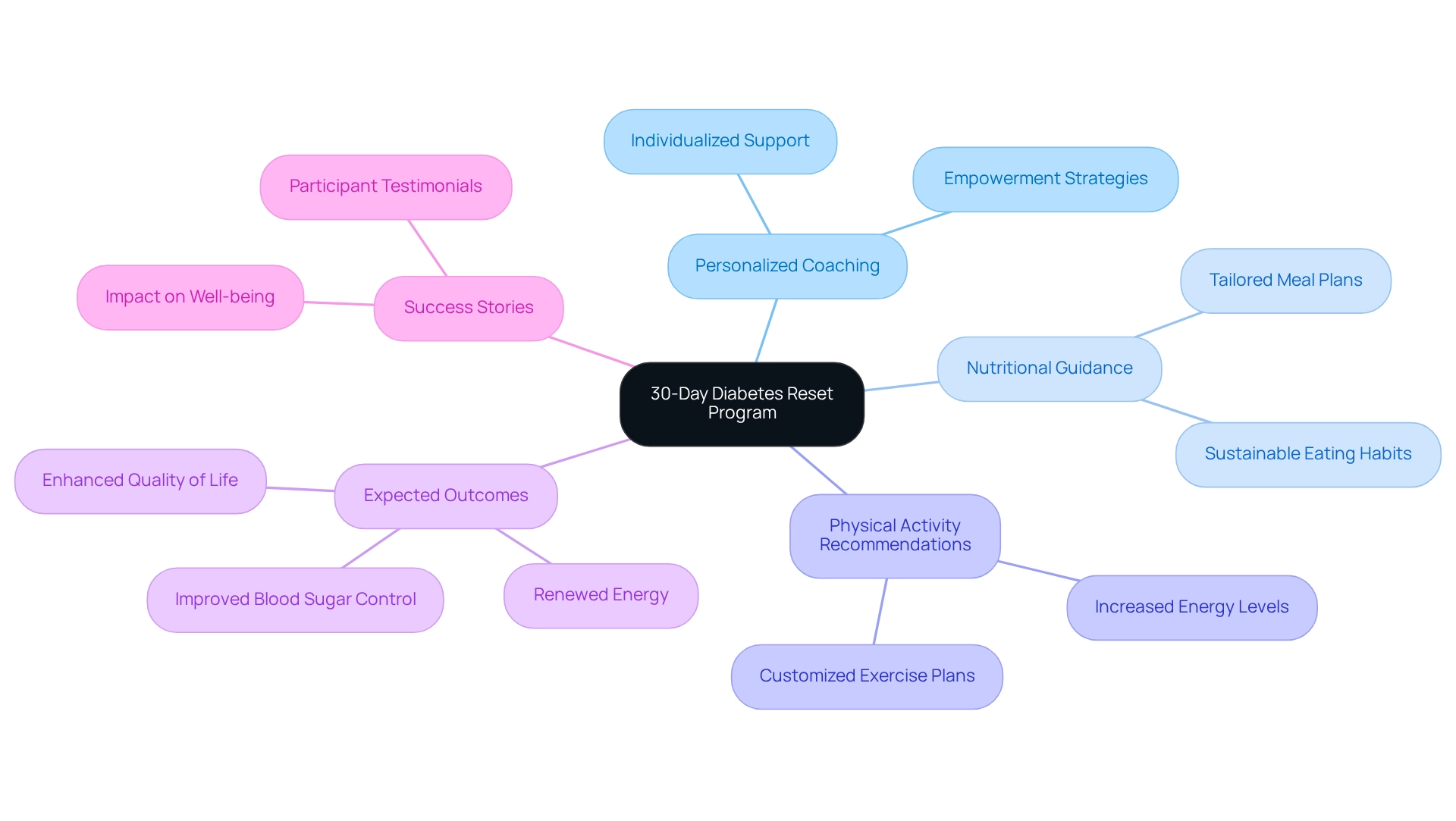
In a world where diabetes affects millions, effective management is more crucial than ever. It’s important to recognize that many individuals face daily challenges in managing their condition. The Integrative Wellness Center’s 30-Day Diabetes Reset Program stands out as a beacon of hope, offering a holistic approach tailored to individual needs. By combining personalized coaching, nutritional guidance, and physical activity recommendations, this program empowers participants to take control of their health and achieve sustainable lifestyle changes.
Many patients find that education and tailored strategies are key to their success. As research increasingly underscores this importance, success stories from program participants reveal transformative outcomes, showcasing the potential for renewed energy and improved blood sugar control. This article delves into the multifaceted strategies for diabetes management, emphasizing the significance of proactive approaches and community support in enhancing the quality of life for those living with this chronic condition. Together, we can navigate this journey towards better health.
Integrative Wellness Center: 30-Day Diabetes Reset Program for Effective Management
The Integrative Wellness Center’s 30-Day Diabetes Reset Program is designed to empower individuals in managing their diabetes effectively through a holistic approach. This groundbreaking, clinically validated program offers personalized coaching, nutritional guidance, and tailored physical activity recommendations, ensuring that each participant receives support that meets their unique needs. By focusing on sustainable lifestyle changes, participants can achieve improved blood sugar control and renewed energy, ultimately enhancing their overall health.
It’s important to recognize that education is a cornerstone of the program, equipping patients with essential knowledge and practical tools for long-term success. Research indicates that feedback strategies and programs of shorter duration (less than six months) are particularly effective for self-management, significantly enhancing health management outcomes. For many, this means taking small yet impactful steps towards a healthier future. An analysis of literature from 2013 to 2023 underscores the necessity for personalized strategies for older adults with diabetes, highlighting how the 30-Day Diabetes Reset Program corresponds with these conclusions by tackling intricate wellness needs through customized methods.
Many patients find that success stories from participants in the 30-Day Diabetes Reset Program further illustrate its impact. Numerous people describe significant improvements in their well-being, crediting their advancements to the program’s holistic method. One participant, C.H., shared, “I was depressed, no energy, and had insomnia. I hated how I felt and looked. After joining this program, I lost 55 lbs, and my A1C improved from 9.1 to 5.7. I feel empowered and in control of my well-being for the first time in years.” By cultivating a setting of empowerment and learning, the Integrative Wellness Center not only assists individuals in regaining their well-being but also diminishes their dependence on traditional medical treatments, ultimately resulting in an improved quality of life. As Dr. Jason Shumard states, “By offering individuals with actionable insights and practical tools, the center cultivates an atmosphere where people can regain their health and well-being, ultimately resulting in enhanced quality of life and decreased dependence on traditional medical interventions.
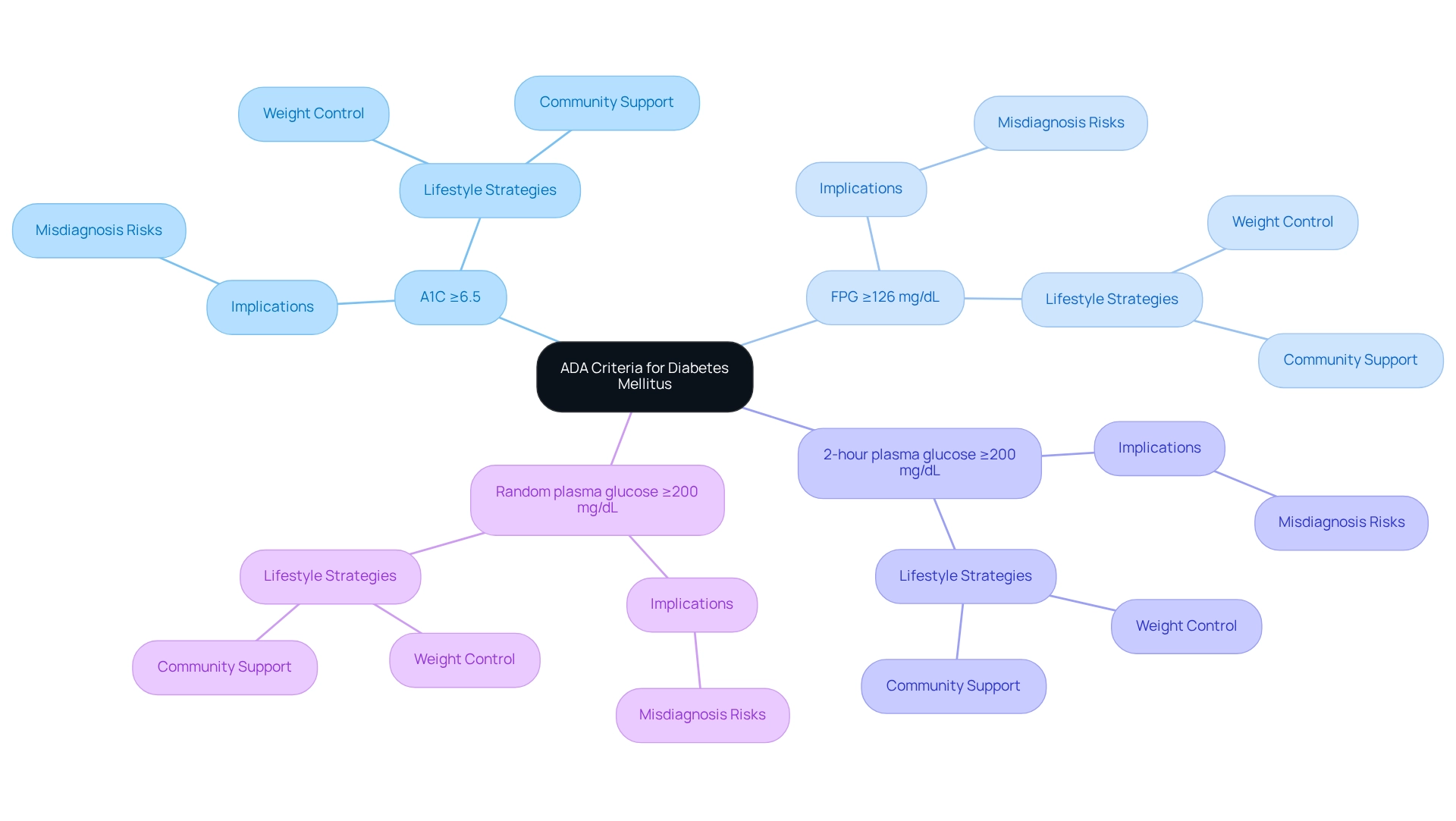
ADA Criteria: Diagnostic Standards for Diabetes Mellitus
The American Diabetes Association (ADA) establishes the ADA criteria for diabetes mellitus, which are pivotal for accurate diagnosis and effective management. These criteria include:
- A1C ≥6.5%
- Fasting plasma glucose (FPG) ≥126 mg/dL
- 2-hour plasma glucose ≥200 mg/dL during an oral glucose tolerance test (OGTT)
- Random plasma glucose ≥200 mg/dL in patients exhibiting classic symptoms of hyperglycemia
It’s important to recognize that accurate application of these standards is essential, as studies indicate that misdiagnosis can lead to inadequate treatment and worsening health outcomes.
Recent updates to the ADA criteria for diabetes mellitus in 2025 emphasize the importance of A1C testing. This not only aids in diagnosis but also provides insights into long-term glucose control. Many patients find that the A1C test is a dependable measure of average blood glucose levels over the previous two to three months, establishing it as a fundamental element in managing their condition.
Current statistics reveal that a significant portion of the population is diagnosed with this condition based on the ADA criteria for diabetes mellitus. This highlights the necessity for healthcare providers to remain vigilant in screening practices. For instance, individuals with a history of gestational diabetes mellitus (GDM) are advised to undergo screening for prediabetes or high blood sugar levels after childbirth. Early detection can greatly influence their well-being.
Furthermore, losing even 10 to 15 pounds can significantly affect the risk of diabetes-related conditions for individuals with prediabetes. This emphasizes the significance of weight control in the prevention and treatment of these issues. Dr. Jason Shumard stresses that in addition to these diagnostic criteria, embracing comprehensive lifestyle strategies—such as customized nutrition, consistent exercise, and community support—can empower individuals to take charge of their well-being.
Real-world examples illustrate the effectiveness of these diagnostic standards. In community engagement initiatives, such as seminars hosted by Dr. Jason Shumard’s Integrative Wellness Center, individuals receive educational resources that enhance their understanding of diabetes management. These occurrences not only boost involvement but also equip individuals with the knowledge required to manage their wellness challenges effectively. As Dr. Shumard states, “By offering individuals actionable insights and practical tools, the center cultivates a setting where people can regain their wellness and well-being, ultimately resulting in enhanced quality of life and decreased dependence on traditional medical treatments.”
In summary, the ADA criteria for diabetes mellitus are not just guidelines; they are essential tools that, when utilized properly, can lead to improved health outcomes and a better quality of life. This is particularly true when supplemented by holistic health solutions and customized functional medicine methods.
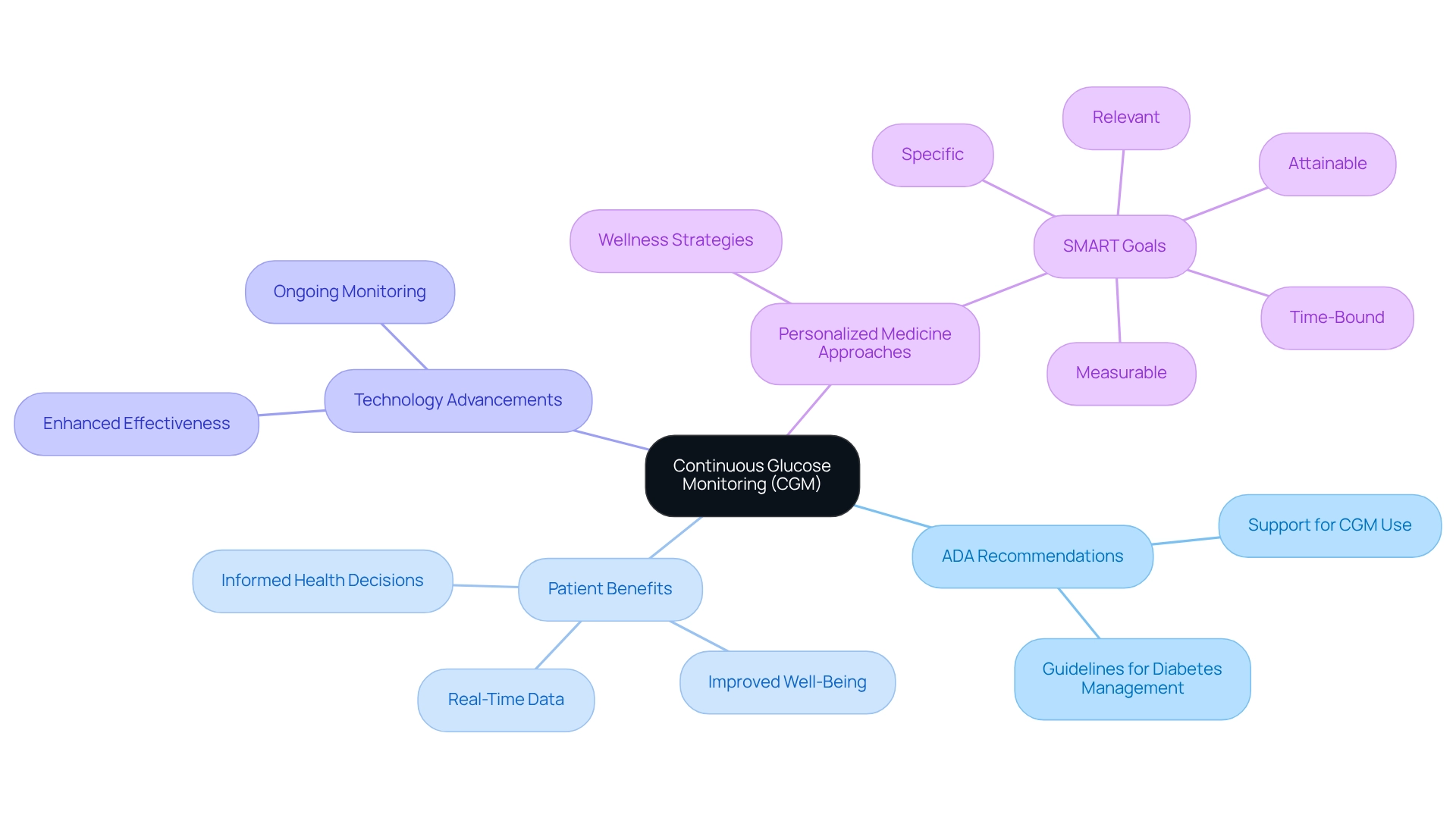
Continuous Glucose Monitoring: ADA Recommendations for Real-Time Management
The American Diabetes Association (ADA) understands the challenges faced by individuals with diabetes mellitus, particularly those on insulin therapy, as defined by the ADA criteria for diabetes mellitus. That’s why they strongly support the use of Continuous Glucose Monitoring (CGM). CGMs provide real-time glucose data, empowering patients to make timely adjustments to their diet, physical activity, and medication regimens. This proactive approach is vital for keeping blood glucose levels within target ranges, significantly reducing the risks associated with hypoglycemia and hyperglycemia.
It’s important to recognize that recent advancements in CGM technology have further enhanced its effectiveness in managing diabetes. Many patients share inspiring stories about how CGM has transformed their approach to blood glucose management, leading to improved overall well-being. Experts point out that CGM is beneficial not only for those who rely on insulin but also for individuals not on insulin, as it offers valuable insights into their body’s glucose responses. Dr. Ovalle encourages those using insulin to consider ongoing glucose monitoring, while others may benefit from temporary use to better understand their body’s reactions.
Many patients find that integrating personalized functional medicine approaches, such as recognizing their wellness profiles and lifestyle factors, can enhance the effectiveness of CGM in controlling blood sugar. This involves thorough evaluations and diagnostic examinations to identify specific elements contributing to their condition, paving the way for a more tailored strategy. The guidelines provided by the ADA criteria for diabetes mellitus highlight the importance of incorporating CGM into wellness strategies to achieve the best possible outcomes. As Gregory J. Norman, PhD, observes, the use of CGM can significantly benefit the increasing number of individuals with diabetes, enhancing their understanding of glucose fluctuations and enabling more informed health decisions. Moreover, setting organized goals, like utilizing fitness applications and establishing SMART goals—specific, measurable, attainable, relevant, and time-bound—can empower individuals, promoting accountability and motivation in their health management journey. For instance, one might aim to lower their average glucose levels by a certain percentage over a set period. With the continuous advancements in CGM technology, individuals are better equipped than ever to navigate their condition effectively.
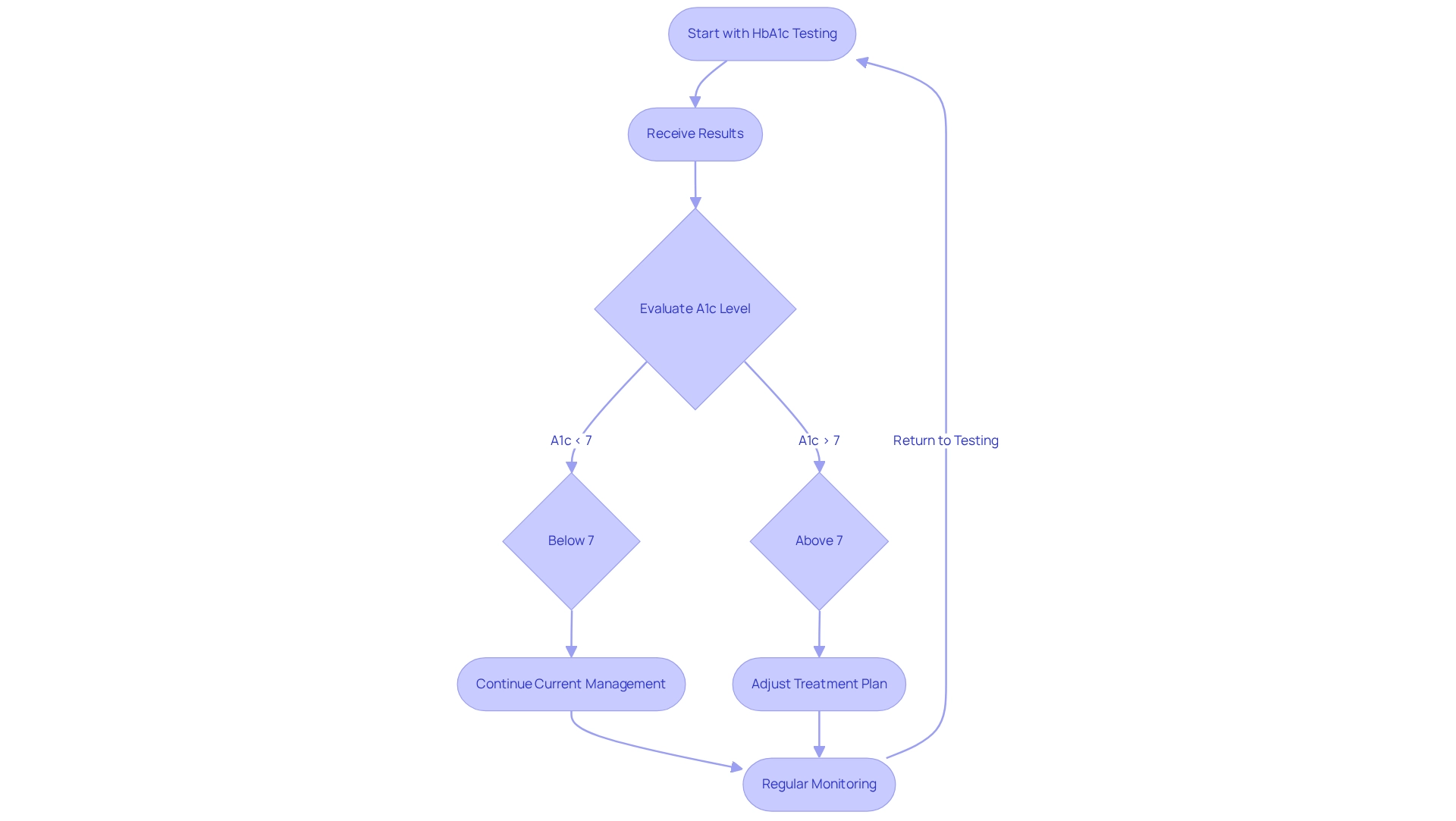
Hemoglobin A1c Testing: Essential for Diabetes Diagnosis and Monitoring
Hemoglobin A1c (HbA1c) testing plays a vital role in diagnosing and managing diabetes, offering a comprehensive view of average blood glucose levels over the past two to three months. This important metric helps healthcare providers understand how well individuals are managing their blood sugar. As we look at the average A1c levels among individuals with diabetes in 2025, it becomes clear that regular monitoring is essential, as many continue to face challenges in achieving optimal control.
It’s important to recognize that the recommendations from the ADA criteria for diabetes mellitus suggest most adults with diabetes aim for an A1c level below 7%. This goal significantly reduces the risk of complications. Routine A1c testing not only facilitates timely adjustments to treatment plans but also empowers individuals to take an active role in their health. Recent guidelines stress the necessity of frequent testing, especially for those experiencing fluctuations in blood glucose levels or those who are newly diagnosed.
Many patients find that HbA1c testing is crucial in managing their blood sugar conditions. Healthcare providers encourage its regular use, as it reflects the success of lifestyle changes and adherence to medications. For example, Ed’s journey at Dr. Jason Shumard’s center illustrates the positive impact of personalized care. He shared, “I lost 55 lbs. My A1C started at 9.1 after 8 months it is now 5.7. My regular MD has cut my blood pressure meds in half and will start reducing my other prescriptions in the near future.” This experience underscores the transformative power of understanding A1c levels and the importance of a holistic approach to health.
Furthermore, testimonials from others reveal similar success stories, shedding light on the risks associated with traditional treatments that often lead to increased medication dependence without addressing the root causes. Consistent monitoring of HbA1c levels is linked to improved health outcomes, as individuals who engage in regular testing often experience fewer complications and a better quality of life. The VADT trial highlighted a three-fold increase in episodes of impaired consciousness among those in the intensive therapy group, emphasizing the need for careful management of blood sugar levels and the role of HbA1c testing in preventing complications. As we gain a clearer understanding of glycemic control and the potential for hyperglycemic organ damage, proactive monitoring through A1c testing according to the ADA criteria for diabetes mellitus becomes increasingly crucial. By prioritizing this essential aspect of blood sugar management, individuals can reclaim their health and lessen their reliance on conventional medical treatments.
Moreover, ongoing discussions in the medical community, as highlighted by Amir Qaseem, MD, PhD, regarding guidance statements on blood sugar control, reflect the evolving nature of treatment protocols and the significance of HbA1c testing. By embracing these insights, patients can navigate their health journeys with greater confidence and support.
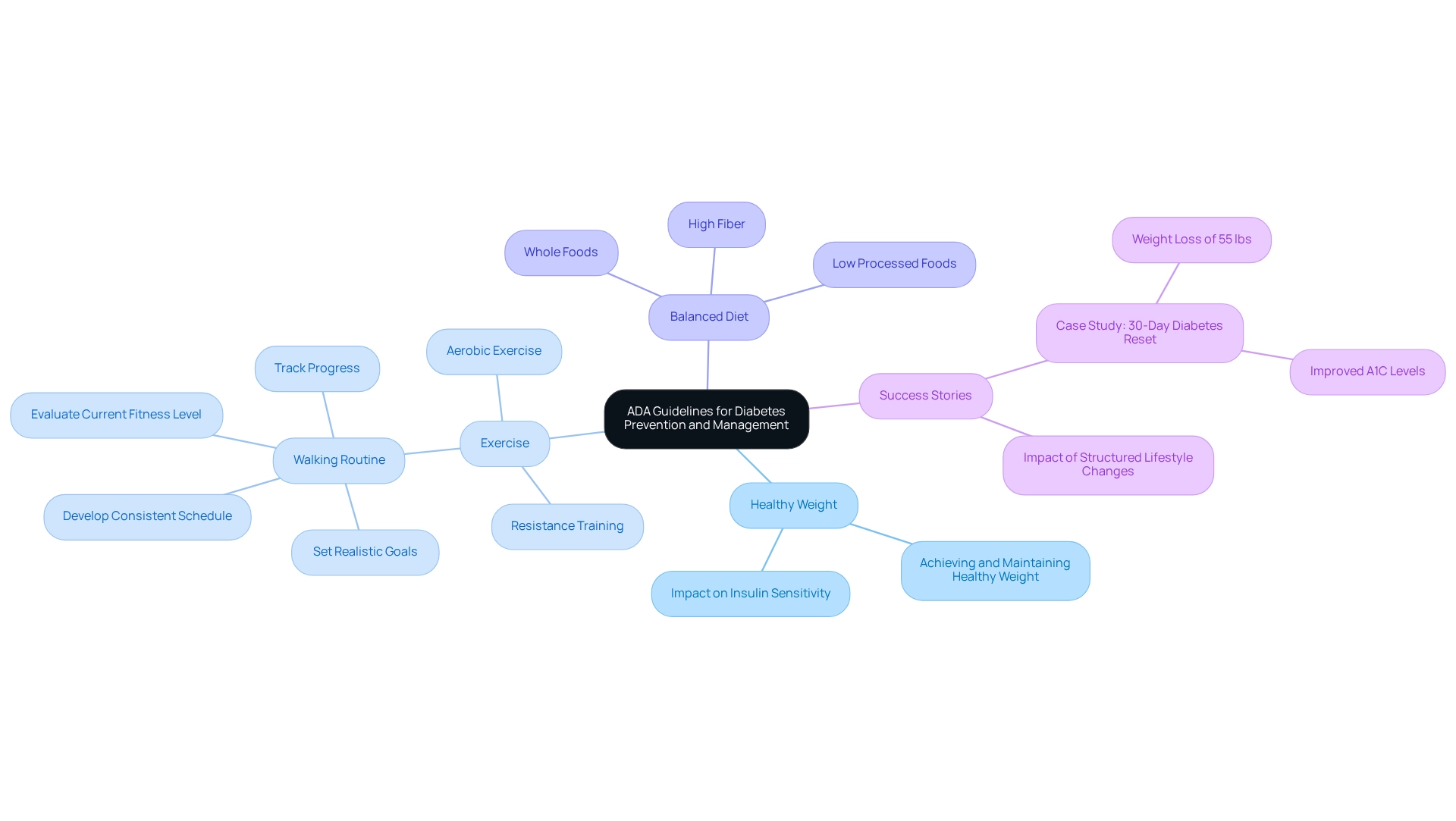
Lifestyle Modifications: ADA Guidelines for Diabetes Prevention and Management
The American Diabetes Association (ADA) emphasizes the vital role of lifestyle changes in both preventing and managing diabetes. It’s important to recognize that achieving and maintaining a healthy weight, engaging in at least 150 minutes of moderate-intensity exercise weekly, and adopting a balanced diet rich in whole grains, fruits, vegetables, and lean proteins can significantly enhance insulin sensitivity and improve blood glucose control. These lifestyle changes not only reduce the risk of diabetes-related complications but also empower individuals to take charge of their health.
Many patients find that starting a walking routine can be a transformative step. Referring to structured methods, such as those outlined in the walking program PDF, can provide a helpful framework. Begin by evaluating your current fitness level and setting realistic goals, like committing to a daily walk of 10-15 minutes. Selecting an appropriate environment is crucial; ensure it aligns with your safety and comfort preferences, whether indoors or outdoors. Developing a consistent schedule is imperative, gradually increasing both the duration and frequency of your walks over time. Tracking your progress is also highly beneficial; utilizing a journal or an app can help maintain motivation and allow you to celebrate your achievements along the way.
Real-world examples illustrate the effectiveness of these modifications. For instance, individuals who have successfully integrated regular physical activity into their routines report not only better management of their diabetes but also improved overall well-being. One inspiring case study highlights an individual who, after participating in Dr. Jason Shumard’s 30-Day Diabetes Reset program, lost 55 lbs and significantly improved their A1C levels. This showcases the profound impact of structured lifestyle changes.
The ADA criteria for diabetes mellitus in the current guidelines for 2025 stress the importance of physical activity, recommending that patients incorporate both aerobic and resistance training into their weekly regimen. This dual strategy not only assists in weight control but also improves cardiovascular well-being—essential for individuals with blood sugar issues. Additionally, research indicates that structured walking programs can lead to significant wellness improvements, with a success rate of 89.5% among specialists recognizing the benefits of such initiatives.
Expert advice from nutritionists highlights the significance of dietary changes. A diet low in processed foods and high in fiber can lead to substantial improvements in glycemic control. Statistics indicate that lifestyle changes can result in a 58% decrease in the likelihood of developing diabetes among high-risk individuals, underscoring the significant effect of these alterations.
As Dr. Jason Shumard wisely states, “By offering patients actionable insights and practical tools, the center cultivates an atmosphere where individuals can regain their wellness and well-being.” In summary, the ADA criteria for diabetes mellitus serve as an essential framework for preventing and controlling diabetes, empowering individuals to make informed choices and commit to sustained lifestyle changes.
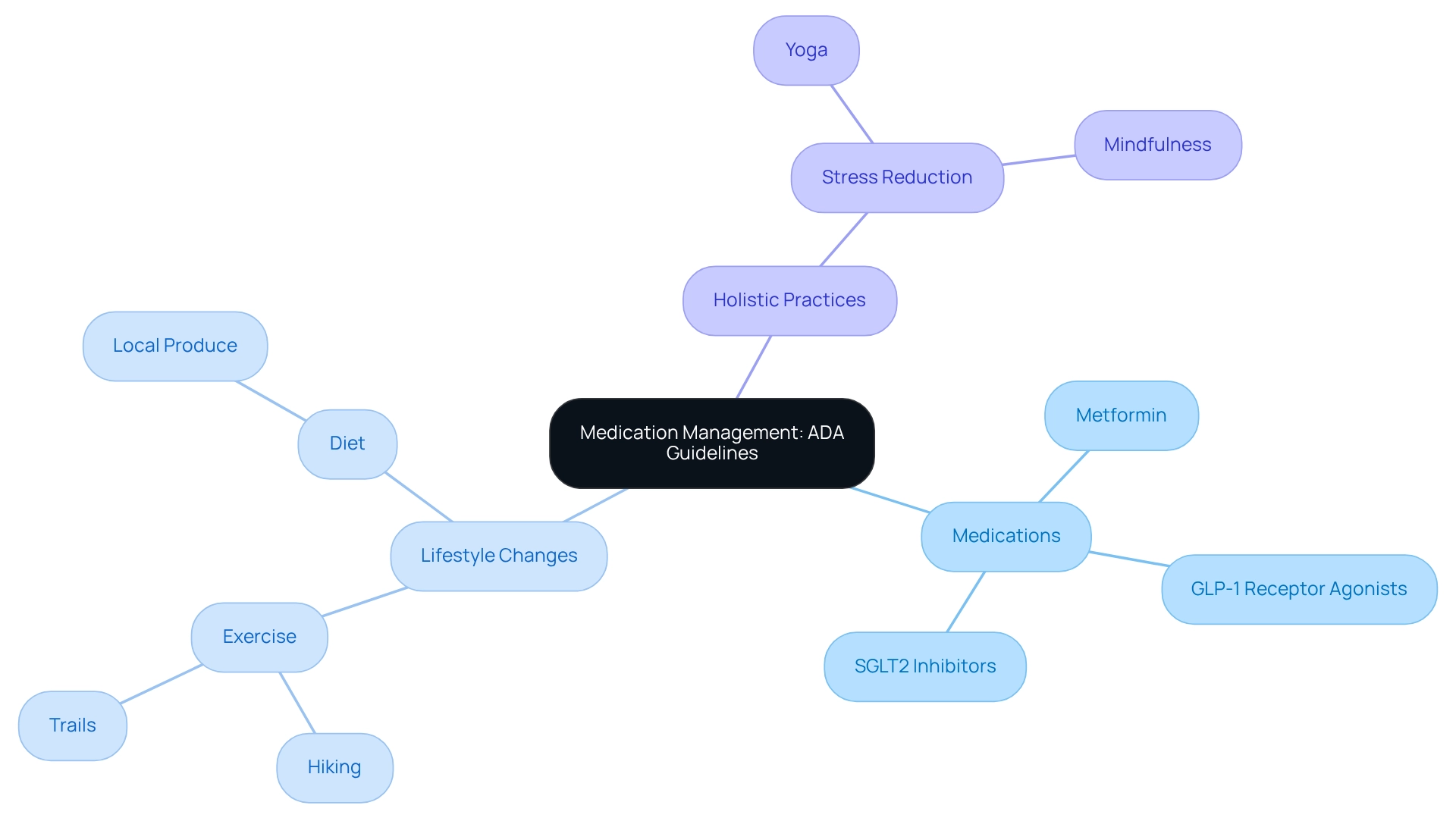
Medication Management: ADA Guidelines for Effective Diabetes Treatment
The American Diabetes Association (ADA) offers essential guidelines, including the ADA criteria for diabetes mellitus, for effective medication management in treating this challenging condition. Metformin remains the cornerstone of first-line treatment, recognized for its ability to lower blood glucose levels and its favorable tolerability among patients. It’s important to acknowledge that a significant majority of individuals with blood sugar issues rely on Metformin, underscoring its vital role in managing this condition.
In addition to Metformin, the ADA criteria for diabetes mellitus suggest considering other medications like GLP-1 receptor agonists and SGLT2 inhibitors, especially for patients with unique needs. These medications not only enhance glycemic control but also assist in reducing cardiovascular risks. This is particularly relevant given that 8.0% of U.S. adults with diagnosed conditions have non-HDL cholesterol levels of 190 mg/dL or higher.
However, managing diabetes effectively extends beyond medication. Embracing a holistic lifestyle is crucial, particularly in San Marcos, CA, where outdoor activities can greatly enhance physical health. Many patients find that regular exercise, such as hiking at Lake San Marcos or strolling along the trails at Discovery Lake, can improve insulin sensitivity and help regulate blood sugar levels. Coupled with a balanced diet rich in local produce like avocados and seasonal berries from vibrant farmers’ markets, individuals can take meaningful steps toward managing their blood sugar while enjoying the community atmosphere.
Integrating stress reduction methods, such as yoga or mindfulness practices, is also vital for a holistic approach to blood sugar care. Regularly assessing medication effectiveness and monitoring for side effects are essential components of optimizing treatment plans. A notable case study reveals that 31.9% of adults with diagnosed conditions engage in less than 10 minutes of moderate or vigorous physical activity weekly, highlighting a significant barrier to effective management. This emphasizes the need for a comprehensive approach that includes lifestyle modifications alongside pharmacotherapy.
Expert insights from endocrinologists highlight the importance of Metformin in managing blood sugar, with many supporting its continued use as a foundational therapy. As new treatments for blood sugar regulation are approved in 2025, including innovative options that enhance individual outcomes, the ADA criteria for diabetes mellitus will evolve, ensuring that individuals receive the most effective and personalized care possible. The financial burden of diabetes management is substantial, with excess medical costs per person rising from $10,179 to $12,022 between 2012 and 2022, which underscores the necessity of effective medication management.
Dr. Jason Shumard emphasizes, “By offering individuals actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being.” By following these guidelines and integrating holistic lifestyle strategies, healthcare providers can significantly enhance patient outcomes and overall quality of life.
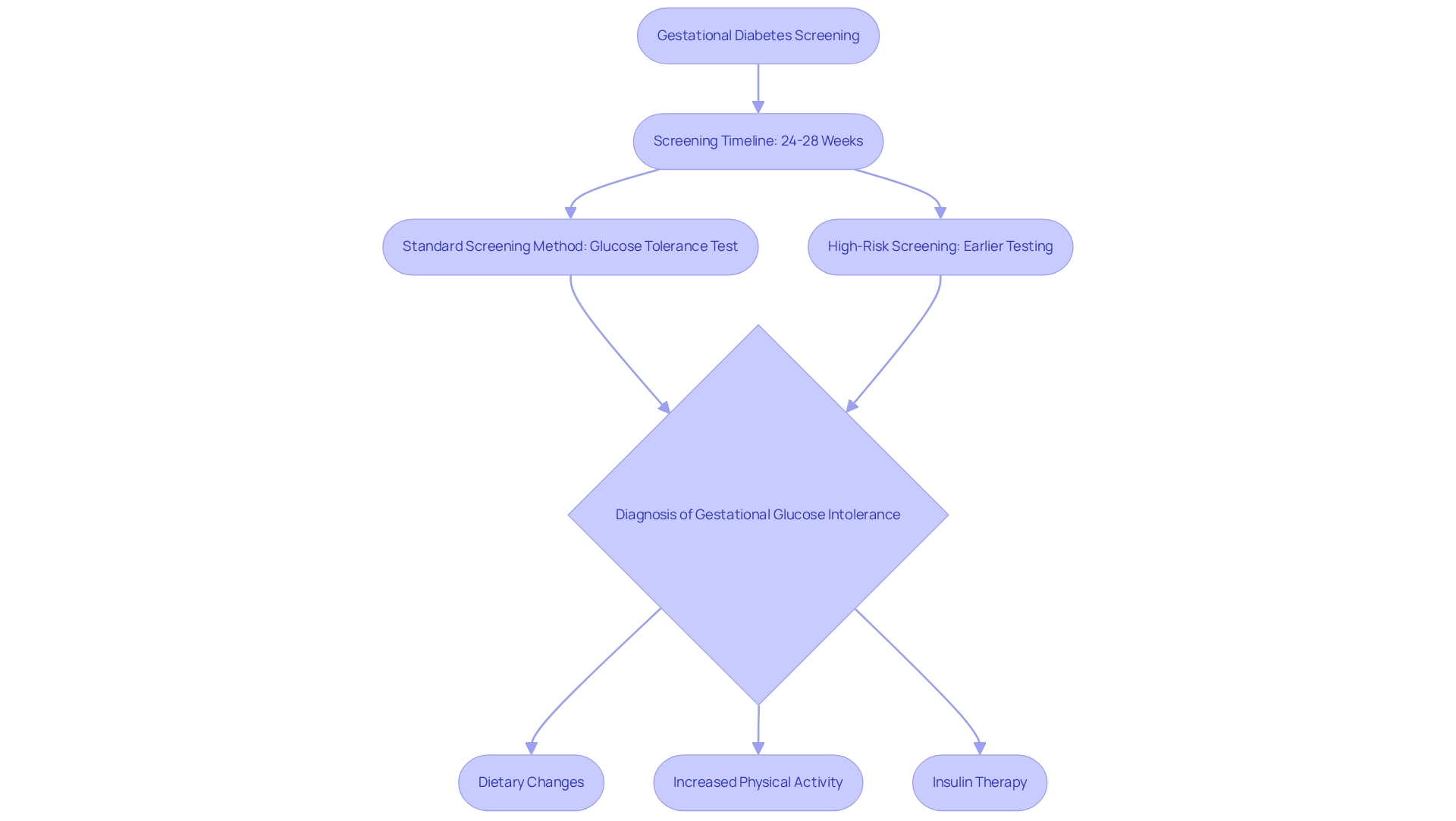
Gestational Diabetes Screening: ADA Criteria for Expecting Mothers
The American Diabetes Association (ADA) emphasizes the importance of testing for gestational conditions between 24 and 28 weeks of pregnancy. It’s crucial for expectant mothers to be aware of this timeline, as early detection can significantly impact their health and that of their baby. For those identified as high-risk, earlier screening may be necessary to ensure timely intervention. The standard screening method, a glucose tolerance test, assesses how well the body processes sugar. If gestational glucose intolerance is diagnosed, management strategies typically include dietary changes, increased physical activity, and sometimes, insulin therapy.
Recognizing the need for early detection and effective management of gestational glucose intolerance is vital for minimizing potential complications. Did you know that the rate of gestational diabetes is notably higher among older mothers? In 2021, it reached 15.3% for those aged 40 and above. This statistic underscores the need for proactive screening and intervention, especially in under-resourced communities where awareness may be lacking and targeted actions are crucial.
Empowering individuals through education is essential in managing blood sugar levels effectively during pregnancy. Many patients find that educational initiatives can make a significant difference. For instance, Dr. Shumard’s method, which offers resources and workshops, has proven effective in helping individuals better understand their medical conditions. Testimonials reveal that patients feel more prepared to oversee their well-being, leading to better outcomes. As Joyce A. Martin noted, increases in gestational diabetes have been observed across all maternal age groups, highlighting the importance of early detection.
The significance of early detection cannot be overstated; it greatly influences both maternal and infant well-being, paving the way for healthier pregnancies and reducing the risk of long-term complications. Patients are encouraged to seek educational materials and engage in screening programs. Taking these proactive steps can empower you in managing your well-being and potentially reduce insulin dependency.
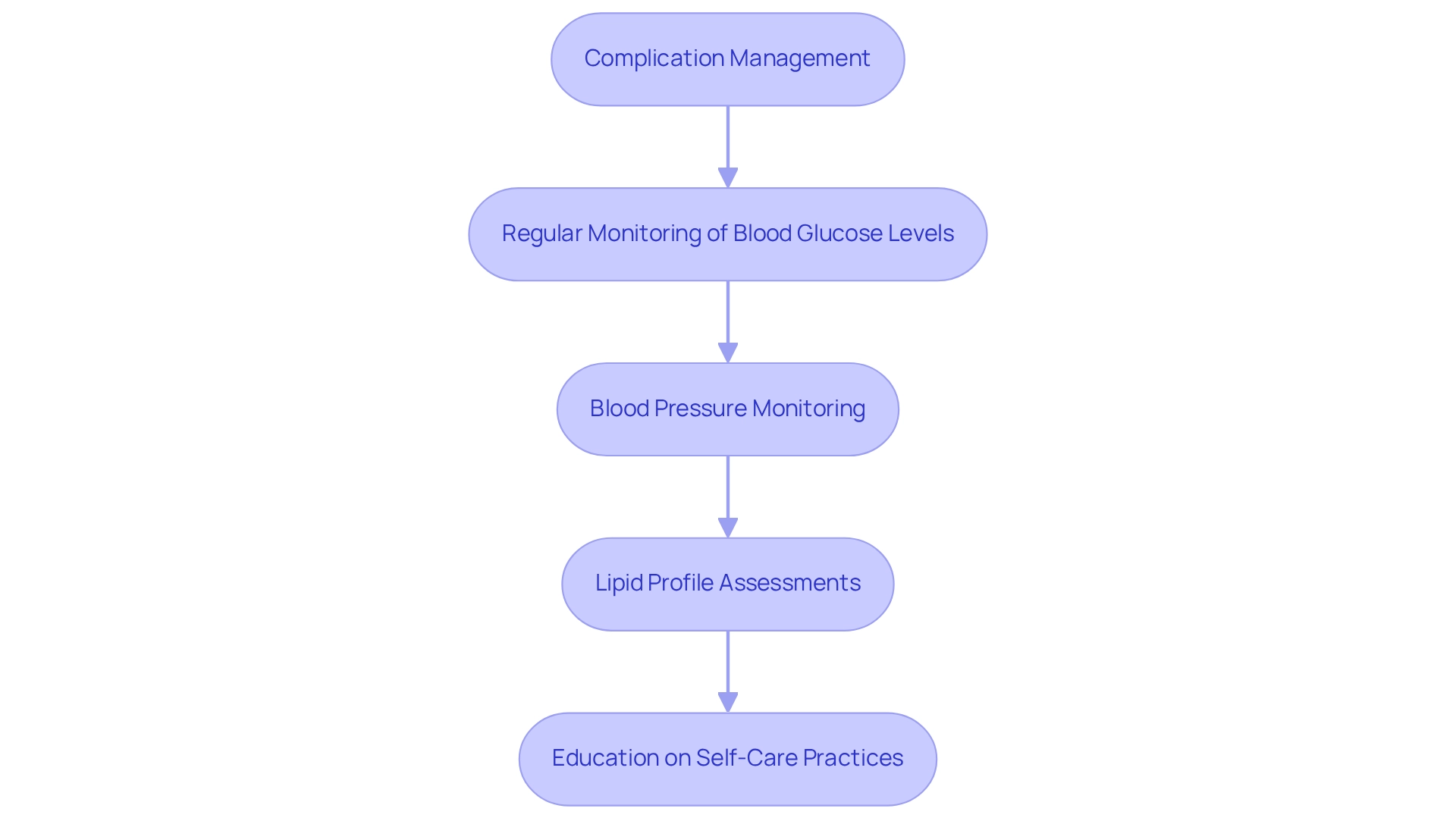
Complication Management: ADA Guidelines for Diabetes-Related Health Issues
The American Diabetes Association (ADA) emphasizes essential guidelines for managing diabetes-related complications, including cardiovascular disease, neuropathy, nephropathy, and retinopathy. It’s important to recognize that regular screenings play a vital role, as early detection can significantly enhance the effectiveness of interventions. Did you know that macrovascular disease accounts for up to 85% of the expenses linked to diabetes complications? This statistic underscores the considerable financial strain these conditions impose on individuals and the healthcare system.
Many patients find that maintaining optimal blood glucose levels, managing blood pressure and cholesterol, and engaging in regular physical activity can help mitigate the risk of complications. In San Marcos, CA, embracing an outdoor lifestyle can significantly contribute to these goals. Residents have the opportunity to take advantage of the area’s parks and trails for regular exercise, which is crucial for improving insulin sensitivity and controlling weight. Activities like hiking at Lake San Marcos or strolling the paths at Discovery Lake not only boost physical fitness but also elevate mood and overall well-being.
The latest research highlights that non-HDL cholesterol is a more reliable predictor of cardiovascular disease risk than LDL. This reinforces the need for comprehensive lipid management strategies that can directly impact patient care. Incorporating a balanced diet rich in local produce, such as avocados and berries, can further support blood sugar regulation and overall health. Participating in community wellness initiatives can offer essential assistance, providing resources tailored for effectively managing blood sugar levels.
Real-world examples demonstrate the effectiveness of structured screening and prevention programs. A recent study highlighted the high frequency of chronic complications among individuals with type 2 conditions, advocating for improved screening initiatives to tackle these issues proactively. As observed by Somayeh Heydari, “This study indicated that the occurrence of complications related to the condition was significant and was greater in individuals facing more self-care obstacles,” emphasizing the importance of individual involvement in managing their well-being.
Looking ahead to 2025, the importance of regular screenings is emphasized by the ADA criteria for diabetes mellitus, recommending that healthcare providers implement current guidelines to identify and manage complications early. Key recommendations from the 2025 guidelines, which align with the ADA criteria for diabetes mellitus, include:
- Regular monitoring of blood glucose levels
- Blood pressure monitoring
- Lipid profile assessments
- Education on self-care practices
This proactive strategy not only enhances personal health but also alleviates the overall healthcare burden related to this condition. By empowering individuals with knowledge and resources, including tailored advice from Dr. Jason Shumard, the ADA aims to cultivate a culture of self-care that can lead to improved management of diabetes-related complications. Additionally, for those seeking to enhance their wellness through physical activity, a structured walking program can be an effective way to start, with resources available to help track progress and set achievable goals.
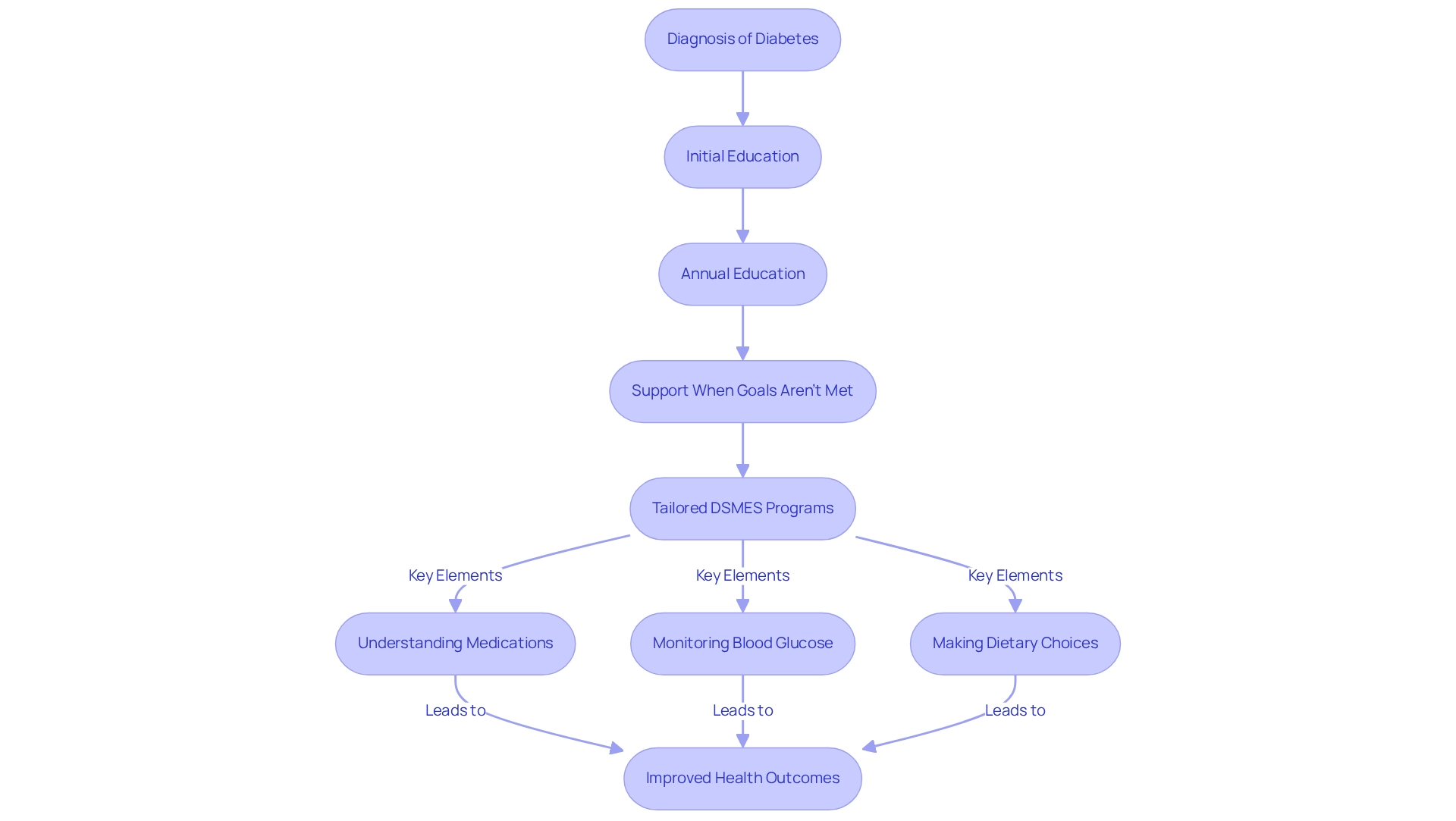
Patient Education: ADA Criteria for Empowering Diabetes Self-Management
The American Diabetes Association (ADA) emphasizes the crucial role of diabetes self-management education and support (DSMES) as a cornerstone of diabetes care. It’s essential for patients to receive education at the time of diagnosis, annually, and whenever treatment goals are not met. Effective DSMES programs empower patients with the knowledge and skills necessary to manage their condition effectively. This includes understanding medications, monitoring blood glucose levels, and making informed dietary choices—elements that are vital for building confidence and enhancing health outcomes.
It’s important to recognize that traditional treatments for blood sugar management can carry risks, particularly concerning elevated insulin levels. Many patients, like C.H., have encountered the adverse effects of insulin injections and medications that do not address the underlying causes of their condition. C.H. shared, “I was on 2 different meds that weren’t working and was told that I needed insulin. When I started this program, the Doctor gave great personal attention and care in helping fix my condition. I have lost 55 lbs. My A1C started at 9.1 after 8 months; it is now 5.7.”
Real-world examples illuminate the effectiveness of tailored DSMES programs. For instance, a study conducted on older women in Shiraz, Iran, with a sample size of 41 individuals per group and accounting for a 20% dropout rate, demonstrated that focused self-management education significantly improved participants’ quality of life. Such findings underscore the importance of customizing education to meet the unique needs of various demographics.
Statistics further reinforce the efficacy of these programs; participants in lifestyle-focused interventions reported quality-adjusted life years of 6.89 over a decade, indicating substantial long-term benefits. Expert opinions align with this perspective, as educators in the field advocate for comprehensive education as a standard of care. As outlined by the ADA criteria for diabetes mellitus, ‘Diabetes education is presently advised as a standard of care by numerous guidelines like the ADA,’ highlighting the necessity for ongoing support and education to empower individuals to take charge of their health and make informed decisions.
As health education continues to evolve, current trends emphasize integrating technology and personalized approaches to enhance patient engagement. By prioritizing education and support, healthcare providers can significantly improve management outcomes for patients with diabetes-related conditions, ultimately contributing to a healthier population. Patients are encouraged to actively seek out health education resources and engage in programs that align with their individual needs, fostering a proactive approach to their wellbeing. The experiences of individuals like C.H. serve as a powerful reminder of the potential for transformative change through holistic care.
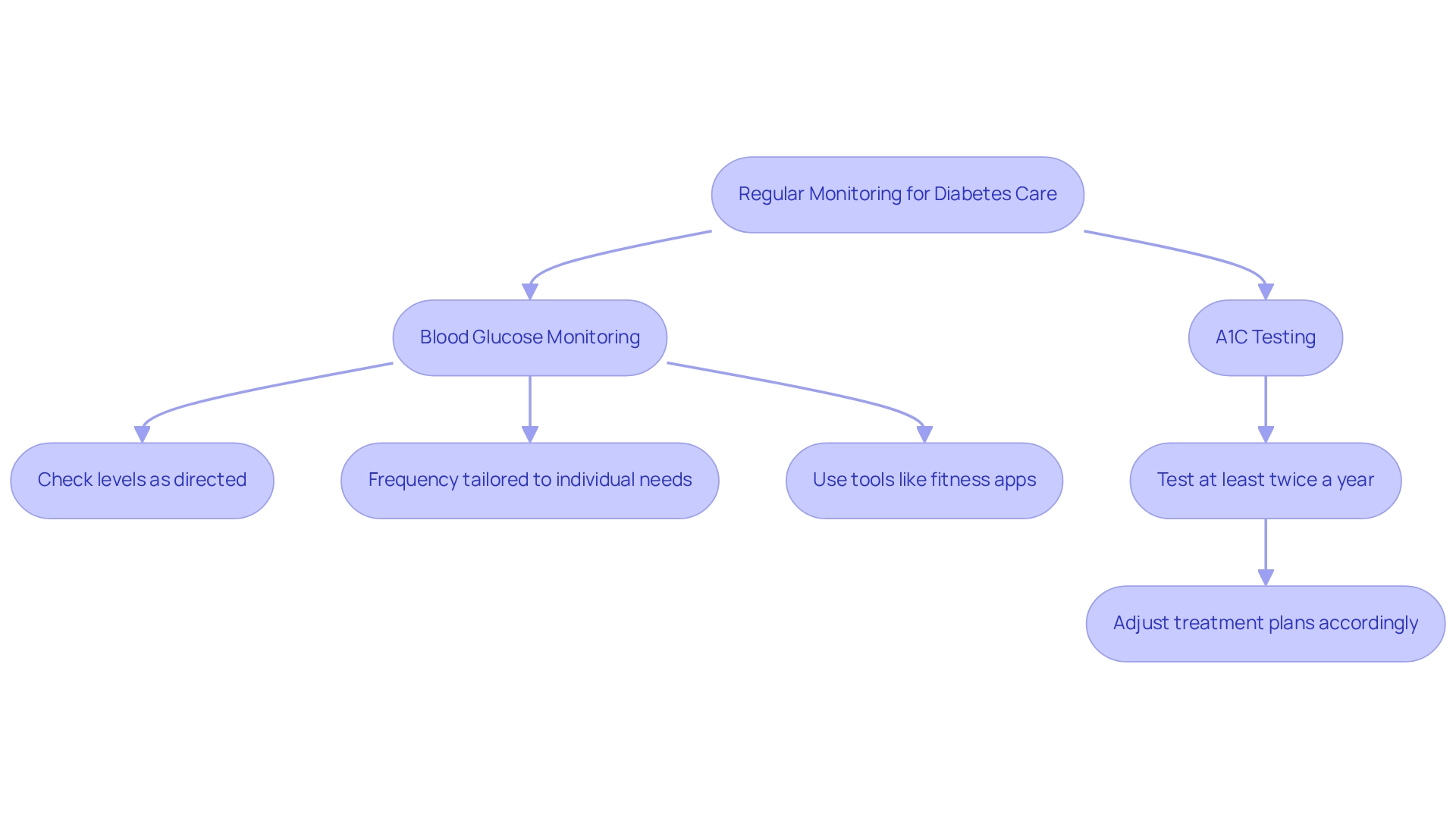
Regular Monitoring: ADA Recommendations for Ongoing Diabetes Care
The American Diabetes Association (ADA) stresses that adhering to the ADA criteria for diabetes mellitus includes the crucial importance of regular blood glucose monitoring in effectively managing the condition. It’s essential for patients to check their blood glucose levels as directed by their healthcare providers, with the frequency tailored to their unique treatment plans. This personalized approach ensures that monitoring aligns with each individual’s specific health needs.
Equally vital is regular A1C testing, which offers insights into long-term glycemic control. According to the ADA criteria for diabetes mellitus, individuals with elevated blood sugar levels should undergo A1C testing at least twice a year. This allows for timely adjustments to treatment plans, empowering both individuals and healthcare providers to make informed decisions that optimize diabetes management and improve overall health outcomes.
To effectively track and enhance progress, individuals are encouraged to explore various monitoring methods, such as fitness apps, journals, and pedometers. Setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly enhance focus and motivation. For example, you might set a goal to achieve 10,000 steps daily within a month or gradually increase your exercise duration by five minutes each week. Research shows that persistence in goal-setting can positively influence performance; for instance, scores improved from 3.4 (SD = 2.0) to 3.8 (SD = 1.9) under specific conditions, underscoring the effectiveness of structured goal-setting. However, it’s important to recognize that the study also found systematic negative relationships between goal achievement and goal difficulty for many individuals, highlighting the need for appropriately challenging goals. Regularly reviewing your progress fosters accountability and allows for adjustments in response to evolving fitness levels.
Real-world examples showcase the benefits of consistent monitoring. Consider the case study titled “Education in Diabetes Management,” which revealed that individuals who received comprehensive education about their condition—particularly concerning diet, exercise, and medication adherence—were more likely to engage in self-care practices. These empowered individuals often reported improved health outcomes and a better quality of life, emphasizing the importance of ongoing care and monitoring.
According to the ADA criteria for diabetes mellitus, regular blood glucose monitoring is advocated as a foundational element in managing blood sugar levels. Healthcare professionals stress that collaboration among providers is key to developing effective monitoring strategies. Dr. Jason Shumard notes, “By providing individuals with actionable insights and practical tools, the center fosters an environment where people can reclaim their well-being, ultimately leading to improved quality of life and reduced reliance on traditional medical interventions.” By nurturing an atmosphere of education and support, patients can take charge of their health and lessen their dependence on conventional medical interventions, paving the way for more effective diabetes management.
Conclusion
Managing diabetes can feel overwhelming, and it’s essential to recognize the complexities involved. The journey requires a multifaceted approach that includes education, lifestyle changes, and personalized care. The Integrative Wellness Center’s 30-Day Diabetes Reset Program exemplifies this holistic strategy, empowering participants to take control of their health through tailored coaching, nutritional guidance, and physical activity recommendations. Many participants have shared success stories that highlight the transformative potential of personalized support in improving blood sugar control and overall well-being.
It’s important to understand that regular monitoring plays a crucial role in effective diabetes management. The American Diabetes Association (ADA) emphasizes the significance of A1C testing and continuous glucose monitoring as essential tools. These practices provide critical insights into glucose levels and enable proactive adjustments to treatment plans, fostering a sense of empowerment among patients. By integrating these monitoring strategies with lifestyle changes—such as maintaining a balanced diet and engaging in regular exercise—individuals can significantly reduce their risk of diabetes-related complications.
Ultimately, the key to successful diabetes management lies in proactive education and community support. As patients become more informed about their condition and the impact of their lifestyle choices, they are better equipped to make decisions that enhance their quality of life. By fostering an environment of empowerment and continuous learning, both healthcare providers and patients can work together to navigate the challenges of diabetes, paving the way for healthier futures. Remember, you are not alone on this journey—support is always available, and together, we can achieve better health.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program?
The 30-Day Diabetes Reset Program is a clinically validated program designed by the Integrative Wellness Center to help individuals manage their diabetes through a holistic approach, including personalized coaching, nutritional guidance, and tailored physical activity recommendations.
How does the program support participants?
The program supports participants by providing personalized coaching, nutritional guidance, and exercise recommendations tailored to individual needs, focusing on sustainable lifestyle changes to improve blood sugar control and overall health.
What role does education play in the program?
Education is a cornerstone of the program, equipping participants with essential knowledge and practical tools for long-term success in managing their diabetes effectively.
What evidence supports the effectiveness of the program?
Research indicates that shorter duration programs (less than six months) are effective for self-management, and the 30-Day Diabetes Reset Program aligns with findings emphasizing personalized strategies for older adults with diabetes.
Can you share a success story from the program?
One participant, C.H., reported losing 55 lbs and improving their A1C from 9.1 to 5.7 after joining the program, expressing feelings of empowerment and control over their well-being for the first time in years.
What are the ADA criteria for diabetes mellitus?
The ADA criteria for diabetes mellitus include: – A1C ≥6.5% – Fasting plasma glucose (FPG) ≥126 mg/dL – 2-hour plasma glucose ≥200 mg/dL during an oral glucose tolerance test (OGTT) – Random plasma glucose ≥200 mg/dL in patients with classic symptoms of hyperglycemia.
Why is accurate application of ADA criteria important?
Accurate application of ADA criteria is essential because misdiagnosis can lead to inadequate treatment and worsening health outcomes.
What recent updates have been made to the ADA criteria?
Recent updates in 2025 emphasize the importance of A1C testing for both diagnosis and insights into long-term glucose control.
How can weight loss impact diabetes management?
Losing even 10 to 15 pounds can significantly affect the risk of diabetes-related conditions for individuals with prediabetes, highlighting the importance of weight control in prevention and treatment.
What is Continuous Glucose Monitoring (CGM) and its benefits?
Continuous Glucose Monitoring (CGM) provides real-time glucose data, empowering patients to make timely adjustments to diet, physical activity, and medication regimens, significantly reducing risks associated with hypoglycemia and hyperglycemia.
How can personalized functional medicine approaches enhance diabetes management?
Personalized functional medicine approaches enhance diabetes management by recognizing individual wellness profiles and lifestyle factors, leading to tailored strategies for better blood sugar control.
What strategies can help individuals manage their health effectively?
Setting organized goals, utilizing fitness applications, and establishing SMART goals (specific, measurable, attainable, relevant, and time-bound) can promote accountability and motivation in health management.