Overview
The article titled “10 Essential Facts on Type 2 Diabetes for Better Management” offers key insights designed to empower individuals in managing their condition effectively.
It’s important to recognize that understanding the risks, adopting lifestyle changes, and utilizing community resources can significantly improve health outcomes.
Many patients find that informed management strategies positively impact their blood sugar control and overall well-being, as demonstrated by various statistics and heartfelt testimonials.
This journey can be challenging, but with the right support and knowledge, you can take meaningful steps towards a healthier life.
Introduction
As we confront the growing diabetes epidemic, it’s crucial to recognize the challenges many face in managing their health. The journey toward effective diabetes management and lasting transformation can feel overwhelming, but there is hope. The Integrative Wellness Center’s 30-Day Diabetes Reset Program shines as a guiding light, offering a comprehensive approach that combines personalized coaching, nutritional guidance, and tailored exercise regimens.
It’s important to understand that by focusing on whole foods and sustainable lifestyle changes, this program not only aims to reset metabolic health but also empowers individuals to take control of their diabetes with confidence. Many patients find that making these adjustments can lead to significant improvements in their well-being. With alarming statistics highlighting the severe complications associated with poorly managed diabetes, this innovative program provides essential education and support, guiding participants toward a healthier, more vibrant life.
Imagine the possibilities of living without the constant worry of diabetes-related issues. With testimonials showcasing transformative experiences, the program exemplifies the profound impact of holistic health strategies in the fight against diabetes. Together, we can navigate this journey toward better health, one step at a time.
Integrative Wellness Center: 30-Day Diabetes Reset Program for Lasting Health Transformation
The 30-Day Diabetes Reset Program at the Integrative Wellness Center offers a compassionate, clinically approved approach designed to help individuals reclaim their health and well-being. This program features personalized coaching, dietary guidance, and tailored exercise recommendations, all aimed at restoring metabolic health. By focusing on whole foods, reducing processed sugars, and encouraging regular physical activity, participants can experience significant improvements in blood sugar levels and overall wellness. Additionally, educational resources play a crucial role by providing patients with essential information, such as facts on type 2 diabetes, for sustainable management of their condition.
For instance, healthcare services that include routine foot examinations and patient education can prevent up to 85% of amputations associated with this disease. Furthermore, in 2019, 11.8% of U.S. adults diagnosed with high blood sugar reported severe vision difficulties or blindness, underscoring the urgent need for effective management initiatives like the 30-Day Reset Program. Many participants share heartfelt testimonials about their experiences, with one stating, ‘This program has transformed my life; I feel empowered and in control of my health for the first time.’
This comprehensive approach not only addresses pressing wellness issues but also equips individuals with the tools they need for long-term success in managing diabetes. This is especially beneficial for those who may be struggling with obesity and could gain from focused nutritional guidance and coaching. With Dr. Jason Shumard’s supportive functional medicine approach, patients can stabilize their glucose levels without relying on insulin or prescription medications, fostering renewed energy and significantly reducing anxiety about their condition.
If you’re looking to transform your health, consider reaching out to the Integrative Wellness Center today to learn more about the 30-Day Diabetes Reset Program and how it can support you on your journey.
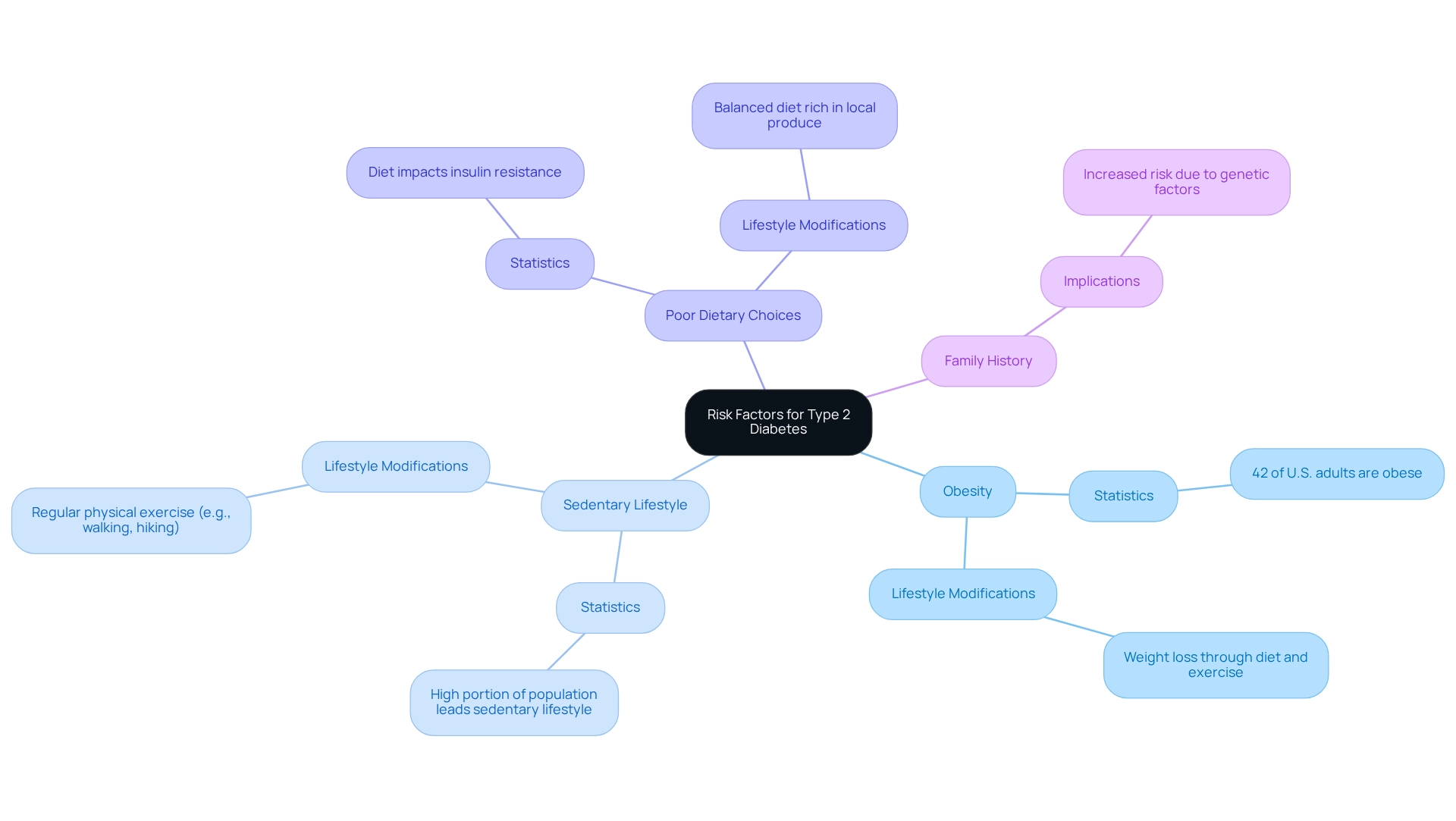
Understanding Risk Factors: Key Contributors to Type 2 Diabetes
Key risk factors for developing type 2 diabetes include:
- Obesity
- A sedentary lifestyle
- Poor dietary choices
- Family history
These factors highlight important facts on type 2 diabetes. It’s important to recognize that individuals who are overweight are considerably more susceptible to developing insulin resistance, which can lead to sugar-related disorders. In reality, obesity plays a significant role, with research showing that lifestyle changes—such as diet and exercise—are crucial for managing diabetes-related conditions and reducing obesity. Current statistics reveal that about 42% of U.S. adults are categorized as obese, and a considerable portion of the population leads a sedentary lifestyle, further increasing their risk for health issues. Additionally, factors like age, ethnicity, and medical conditions such as hypertension can amplify this risk. Significantly, 8.0% of U.S. adults with diagnosed blood sugar issues have a non-HDL level of 190 mg/dL or higher, underscoring the importance of monitoring lipid levels in managing this condition.
Understanding these factors allows individuals to take proactive steps. Many patients find that participating in regular physical exercise and maintaining a balanced diet can significantly reduce their risk of developing type 2 diabetes, as supported by various facts on type 2 diabetes. In San Marcos, CA, embracing an outdoor lifestyle can enhance these efforts. Regular exercise, such as walking or hiking in local parks, not only improves insulin sensitivity but also supports weight management. Moreover, focusing on a balanced diet rich in local produce, like avocados and berries, provides essential nutrients that aid in blood sugar regulation.
Community wellness initiatives in San Marcos offer invaluable assistance, providing resources and encouragement for individuals managing their health. As Dr. Jason Shumard states, “By offering individuals actionable insights and practical tools, the center cultivates an atmosphere where people can reclaim their health and well-being.” Additionally, a study titled ‘Effectiveness of Lifestyle Modifications in Managing Diabetes’ highlights important facts on type 2 diabetes, showing that weight loss through lifestyle changes is crucial for enhancing metabolic control and lowering the risk of this condition in overweight individuals.
Are you ready to take the first step towards a healthier life? Remember, small changes can lead to significant improvements in your health journey.
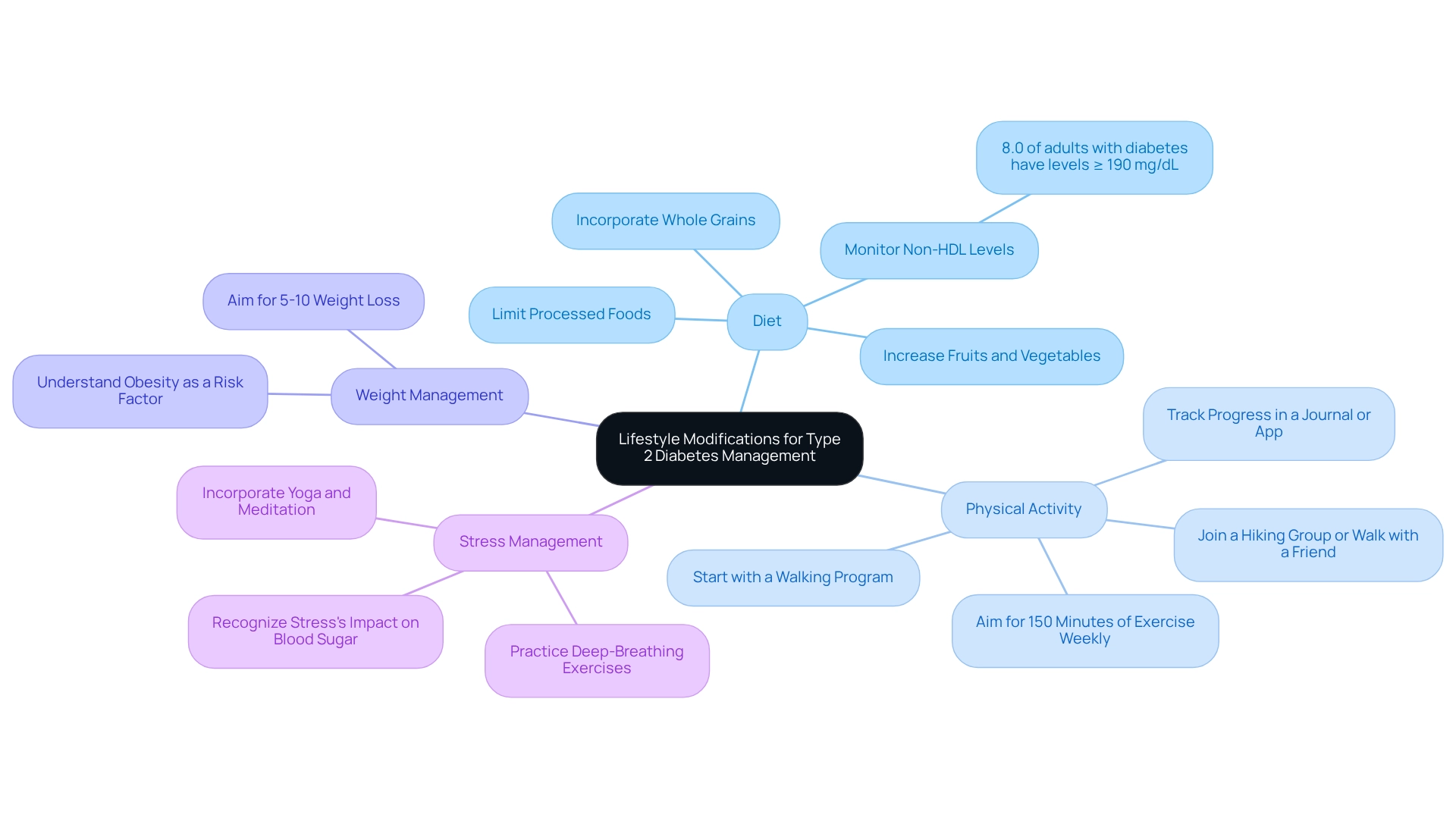
Lifestyle Modifications: Essential Changes for Managing Type 2 Diabetes
Managing type 2 diabetes can feel overwhelming, but the facts on type 2 diabetes show that making some essential lifestyle changes can truly make a difference. Let’s explore a few important modifications that can help you on this journey.
-
Diet: Embracing a balanced diet is crucial. Think of incorporating whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables into your meals. It’s important to limit processed foods and added sugars, as these can worsen blood sugar levels. Many patients have noticed significant improvements in their well-being after making dietary changes. Did you know that 8.0% of adults with diagnosed blood sugar issues had a non-HDL level of 190 mg/dL or greater? This statistic highlights the health risks associated with poor dietary choices.
-
Physical Activity: Striving for at least 150 minutes of moderate-intensity exercise each week, such as brisk walking, cycling, or swimming, can greatly benefit you. Many find that starting with a structured walking program is effective. Begin by assessing your current fitness level and setting achievable goals, like a daily 10-15 minute walk. Choose a safe and comfortable environment for your walks, whether indoors or outdoors. As you progress, gradually increase the duration and frequency of your walks. Regular physical activity not only helps with weight control but also improves insulin sensitivity and regulates blood sugar levels. Keeping track of your progress in a journal or app can keep you motivated and allow you to celebrate your achievements. Have you considered joining a hiking group or walking with a friend for added support and enjoyment?
-
Weight Management: Even a modest weight loss of around 5-10% of your body weight can lead to significant improvements in insulin sensitivity and blood sugar control. This is particularly important since obesity is a major risk factor for type 2 diabetes.
-
Stress Management: Incorporating stress-reducing techniques like yoga, meditation, or deep-breathing exercises can greatly help in maintaining stable blood sugar levels. Persistent stress can lead to hormonal imbalances that negatively affect blood sugar control.
These lifestyle changes are not just theoretical; many case studies provide facts on type 2 diabetes, showing that patients who actively engage in dietary adjustments and regular exercise report better understanding and management of their condition. For instance, individuals who participated in educational programs focused on nutrition and physical activity often express gratitude for the knowledge gained, empowering them to take charge of their health. It’s also important to note that in 2019, 11.8% of U.S. adults with diagnosed health issues reported severe vision difficulties or blindness, underscoring the need for effective management of diabetes.
In conclusion, embracing these vital lifestyle changes, such as a regular walking routine, can enhance your quality of life and improve control over type 2 diabetes. This ultimately reduces reliance on traditional medical treatments. As nutritionists often say, “A well-balanced diet is essential for effectively managing blood sugar levels,” highlighting the crucial role of your dietary choices in this journey.
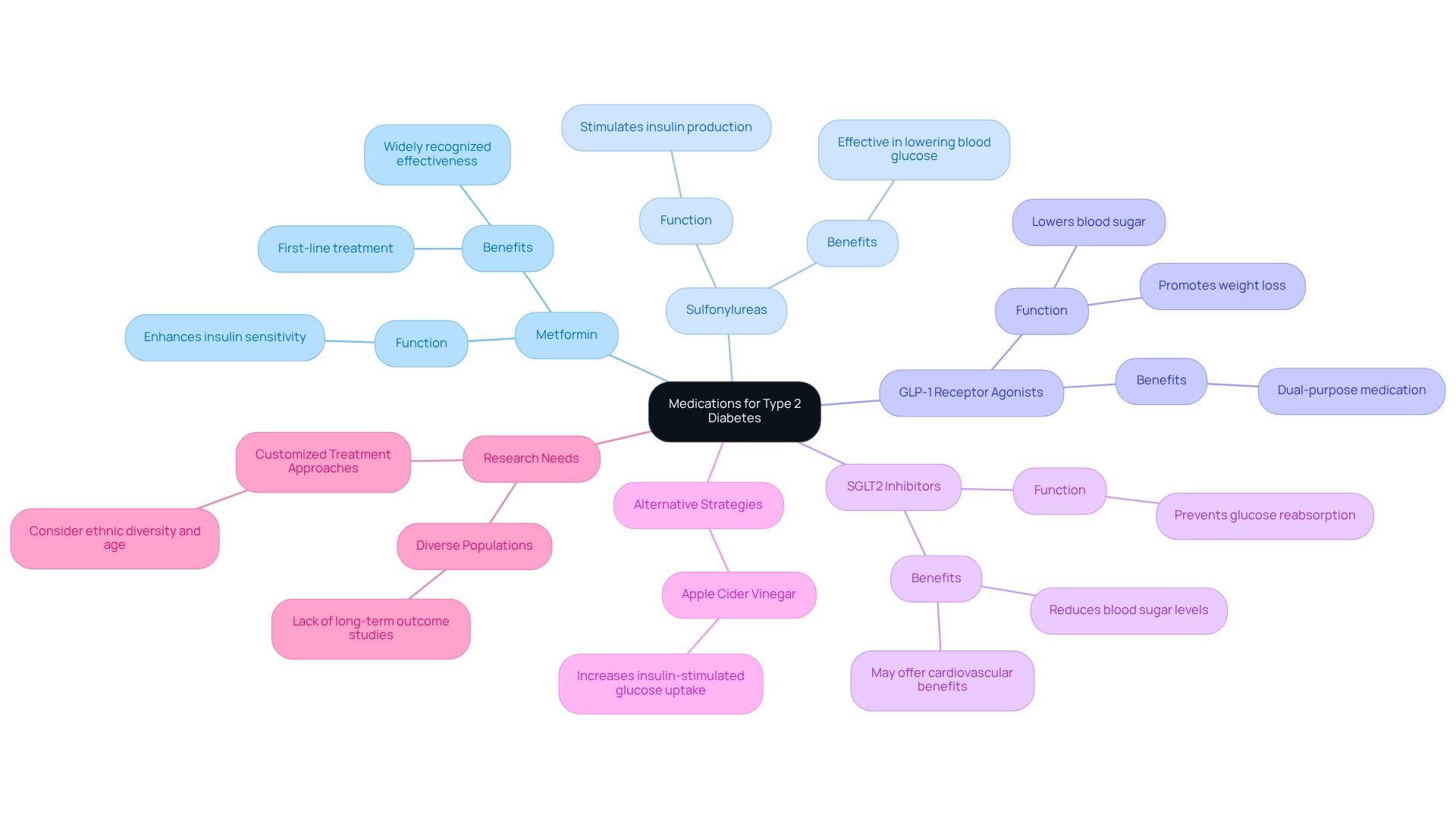
Medications for Type 2 Diabetes: Understanding Your Treatment Options
Managing sugar regulation can feel overwhelming, but understanding the facts on type 2 diabetes and the various medication classes available can empower you in your health journey. Here’s a look at some of the most common treatments:
- Metformin: Often the first-line treatment, Metformin is widely recognized for its ability to lower blood sugar levels by enhancing insulin sensitivity. Many patients find it effective and prefer it as their go-to option.
- Sulfonylureas: These medications stimulate the pancreas to produce additional insulin, effectively helping to lower blood glucose levels.
- GLP-1 Receptor Agonists: Not only do these drugs lower blood sugar, but they also promote weight loss, making them a dual-purpose choice for numerous patients.
- SGLT2 Inhibitors: By preventing the kidneys from reabsorbing glucose back into the bloodstream, these medications help reduce blood sugar levels and may also offer cardiovascular benefits.
It’s important to recognize that alongside conventional medications, alternative strategies like apple cider vinegar consumption have shown promise in increasing insulin-stimulated glucose uptake for those with type 2 conditions. This offers additional avenues for managing your health. Comprehending these treatment choices is essential for patients seeking to make informed decisions about their health management, particularly regarding the facts on type 2 diabetes. While Metformin remains a cornerstone of therapy for blood sugar management, ongoing research is vital to evaluate the long-term effectiveness of various medications across diverse populations. Many patients find that customized treatment approaches, which consider ethnic diversity and age-related factors, are particularly beneficial.
Amid increasing concerns regarding hospital safety—such as the alarming figures of 7,000 erroneous medications and 80,000 infections contracted by patients—there is a growing dedication to minimizing reliance on traditional medical treatments. This highlights the significance of exploring all possible alternatives for effective blood sugar management. Remember, you are not alone in this journey, and there are options available to help you take control of your health.
Complications of Type 2 Diabetes: Risks of Poor Management
Poorly managed type 2 conditions can lead to a multitude of serious complications, significantly impacting quality of life and overall health. It’s important to recognize that understanding these risks is crucial for anyone navigating this journey. Key complications include:
- Cardiovascular Disease: Individuals with diabetes face a heightened risk of heart attack and stroke. Significantly, studies show that 8.0% of U.S. adults with diagnosed blood sugar conditions have non-HDL cholesterol levels of 190 mg/dL or higher, which is a critical risk factor for cardiovascular issues. Managing cholesterol levels through diet and regular check-ups can significantly reduce this risk.
- Neuropathy: This condition involves nerve damage that can result in pain, tingling, or loss of sensation, particularly in the extremities. If left untreated, neuropathy can lead to severe complications, including infections and amputations.
- Kidney Damage: Diabetes is a leading cause of chronic kidney disease, which can progress to kidney failure, necessitating dialysis or transplantation. Regular monitoring of kidney function is essential for early intervention.
- Vision Problems: Diabetic retinopathy is a major concern, increasing the risk of severe eye diseases that can ultimately lead to blindness. Approximately 28.5% of adults with the condition have some form of diabetic retinopathy, highlighting the importance of regular eye exams.
- Foot Damage: Poor circulation and nerve damage can result in serious foot infections, with some cases requiring amputations. Daily foot care and regular check-ups can help prevent these complications.
Comprehending these risks highlights the essential requirement for regular monitoring and efficient oversight strategies. Many patients find that being proactive about their health makes a significant difference. In 2021, approximately 38.4 million Americans received a diagnosis of diabetes-related conditions, emphasizing the urgency of adopting effective management strategies to mitigate these risks. By adopting a healthy lifestyle—such as maintaining a balanced diet, engaging in regular physical activity, and utilizing resources available through Dr. Shumard’s center—most individuals with diabetes can postpone or even avoid these severe outcomes.
Transformative experiences of individuals highlight the effectiveness of Dr. Jason Shumard’s 30-Day Diabetes Reset program. Participants have reported significant improvements in their health. For instance, one individual shared, ‘I lost 55 lbs. My A1C started at 9.1 after 8 months it is now 5.7.’ Another noted, ‘I feel so much better… I lost a lot of weight, have more energy and feel great.’ These testimonials emphasize the importance of a holistic approach to reversing type 2 diabetes and enhancing overall well-being.
Furthermore, efficient approaches for progress monitoring and goal establishment can enable patients in their wellness journey. Employing tools like fitness applications and establishing SMART objectives can greatly enhance motivation and accountability, resulting in improved wellness outcomes. This emphasizes the significance of education and proactive health oversight.
Blood Sugar Monitoring: A Critical Component of Diabetes Management
Monitoring blood sugar levels is essential for individuals living with diabetes, as it provides valuable insights into the facts on type 2 diabetes and how their bodies respond to food, activity, and medication. It’s important to recognize that, according to the facts on type 2 diabetes, effective blood sugar management can significantly improve quality of life. Here are some key considerations to help you navigate this journey:
-
Frequency: Depending on your treatment plan, you may need to check your blood sugar multiple times a day. Studies show that consistent monitoring can greatly enhance your ability to manage your condition, especially when you understand the facts on type 2 diabetes. The facts on type 2 diabetes show that unfortunately, around 50% of individuals with diabetes do not check their blood sugar as often as recommended, highlighting the need for increased awareness and education about this vital practice.
-
Methods: While using a glucometer for fingerstick tests is common, many patients find that continuous glucose monitors (CGMs) offer real-time tracking that allows for immediate adjustments based on fluctuating levels. The SHARE intervention has demonstrated that CGMs can improve user satisfaction and involvement in care, with many individuals reporting greater confidence in managing their diabetes, which aligns with the facts on type 2 diabetes. Additionally, incorporating various tracking methods, such as fitness apps, journals, and pedometers, can further support effective monitoring.
-
Record Keeping: Keeping a log of your blood sugar readings is crucial for identifying patterns and informing treatment adjustments. This practice not only helps you recognize trends but also encourages you to take an active role in your wellness by understanding the facts on type 2 diabetes. You might find that incorporating goal-setting techniques, such as SMART goals, enhances this process. For instance, setting a target to check your blood sugar at specific times each day can foster consistency and accountability. Collaborating with your healthcare provider to establish personalized target blood sugar levels is vital for understanding the facts on type 2 diabetes. Adjusting your management strategies according to these targets can lead to improved health outcomes. Regularly reviewing your progress towards these goals not only fosters accountability but also allows for necessary adaptations as your health changes, particularly in light of the facts on type 2 diabetes.
-
Expert Recommendations: Experts recommend that diabetes educators stress the importance of monitoring techniques to understand the facts on type 2 diabetes. They suggest being proactive in sharing your data with care partners to enhance communication and support. Specific recommendations include checking your blood sugar before meals and adjusting insulin doses accordingly. Participating in community wellness initiatives can also provide additional resources, including facts on type 2 diabetes, tailored to effectively managing your blood sugar levels.
-
Real-World Success: Case studies highlight the effectiveness of CGMs in improving blood sugar control, with many users expressing increased confidence in their ability to manage their condition. The SHARE intervention, for example, reported high satisfaction among participants and improvements in diabetes-related quality of life. Individuals who set organized health objectives often find greater motivation and focus.
-
Latest Technology: Advances in blood sugar monitoring technology are continually emerging, including smartphone-integrated CGMs and wearable devices that alert users to high or low blood sugar levels. These innovations offer individuals more options for effective management. Statistics indicate that many individuals with diabetes do not monitor their blood sugar as frequently as recommended, emphasizing the need for increased awareness and education on the facts on type 2 diabetes and the importance of regular monitoring. Studies have shown that those who monitor their blood sugar levels consistently can achieve better glycemic control and reduce the risk of complications, which aligns with the facts on type 2 diabetes.
The importance of regular blood sugar monitoring relates to the facts on type 2 diabetes, as it is not just about managing a health condition but also a crucial aspect of overall well-being. It empowers you to make informed choices about your lifestyle and treatment. As Peter M. House wisely stated, “Diabetes is not a burden, but a lesson in perseverance and self-care.” By incorporating effective tracking techniques and setting attainable goals, you can enhance your health journey.
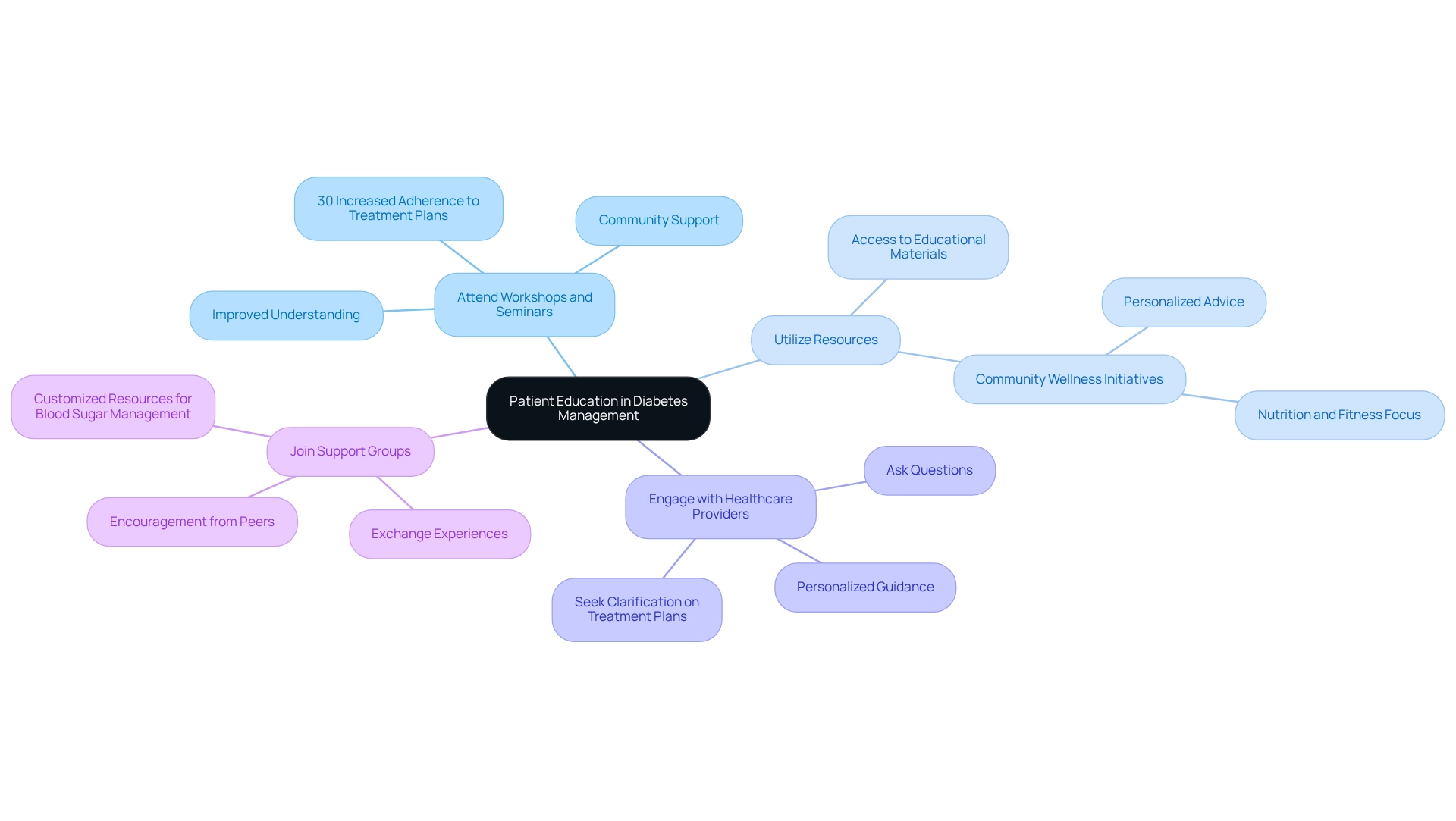
Patient Education: Empowering Yourself in Diabetes Management
Empowering yourself through education about the facts on type 2 diabetes is essential for taking effective control of your condition. It’s important to recognize that the facts on type 2 diabetes can be a powerful tool in your journey. Here are several ways to enhance your understanding:
-
Attend Workshops and Seminars: Engaging in educational events can significantly improve your understanding of diabetes management strategies. Many patients find that participating in health workshops makes them 30% more likely to adhere to their treatment plans, leading to better management outcomes. These gatherings not only provide valuable insights but also share facts on type 2 diabetes, fostering a sense of community among participants and helping you feel less alone in your journey.
-
Utilize Resources: Access a variety of educational materials, including books, online courses, and reputable websites focused on health education. Think about joining community wellness initiatives in San Marcos that emphasize health education, nutrition, and fitness. These programs often offer personalized advice and resources to help you manage your condition effectively, giving you the tools you need to thrive.
-
Engage with Healthcare Providers: Make the most of your appointments by asking questions and seeking clarification on your treatment plans. Open communication with healthcare professionals, such as Dr. Jason Shumard, is crucial for understanding your condition and making informed decisions about your health. Personalized guidance can empower you to implement effective lifestyle changes tailored to your unique needs.
-
Join Support Groups: Connecting with others facing similar challenges can provide valuable insights and encouragement. Support groups create a space for exchanging experiences and tactics, enhancing your ability to manage the condition effectively. Many find that participating in community wellness initiatives also offers assistance and resources customized for managing blood sugar levels, all while appreciating the lovely San Marcos environment.
The significant influence of patient education on blood sugar regulation is highlighted by the facts on type 2 diabetes. Studies indicate that individuals who understand the facts on type 2 diabetes are more likely to follow treatment plans and achieve better health results. As health educator Randy Jackson states, “With this condition, there are so many things that you learn that you didn’t think you wanted to know, but now you have this illness, you’ve gotta do it.” This emphasizes the importance of self-empowerment through knowledge as a foundation for effectively managing your condition. Furthermore, promoting education on blood sugar management in primary care settings is essential to enhance care quality and patient outcomes.
Community Support: Leveraging Resources for Diabetes Management
Community resources play a vital role in managing type 2 conditions by providing essential support, information, and facts on type 2 diabetes to those affected.
-
Local Support Groups: Many communities organize support groups where individuals can share personal experiences and effective strategies for managing their condition. These groups nurture a sense of belonging and offer emotional support, which is essential for long-term well-being management. Engaging with local wellness programs in San Marcos can also provide invaluable support by offering personalized advice and resources based on the facts on type 2 diabetes to manage it effectively.
-
Wellness Fairs and Screenings: Participating in local wellness fairs is a great method to obtain complimentary screenings and informational resources. For example, a recent wellness fair saw involvement from 186 adult Latina women, emphasizing the community’s dedication to enhancing well-being results. These events often address specific barriers to healthcare access, such as food insecurity, which can exacerbate chronic conditions. A study titled “Food Insecurity and Health Outcomes” revealed that participants reported challenges related to limited access to fresh produce, underscoring the need for educational initiatives and resource referrals at future health fairs to mitigate these impacts. Additionally, local farmers’ markets in San Marcos provide fresh, nutritious options like avocados and berries that support a diabetes-friendly diet.
-
Online Communities: Virtual support groups and forums offer a platform for individuals to connect, share tips, and find encouragement from others facing similar challenges. Many patients find that these online networks can be particularly beneficial for those who may have difficulty attending in-person meetings.
-
Healthcare Partnerships: Collaborating with local healthcare providers can improve management of the condition. Numerous providers offer workshops and resources designed for managing blood sugar conditions, including facts on type 2 diabetes, ensuring that patients receive comprehensive support. Collaborations between public and private sectors are crucial in tackling inequalities and enhancing access to quality medical care, as emphasized by recent conversations about the necessity for joint efforts in the community. For personalized guidance and support tailored to your unique needs, consider reaching out to Dr. Jason Shumard in San Marcos, CA.
-
Success Stories: Local support groups for those with blood sugar issues frequently share success stories that inspire and motivate members. These stories not only emphasize successful oversight tactics but also illustrate the beneficial influence of community support on personal wellness journeys. As Austin Freeman stated, “I just took the chance. [Diabetes] wasn’t going to stop me from playing. There was no fear. I was never convinced that anything would keep me from getting back to playing.” This resilience exemplifies the strength found within community support.
By utilizing these community resources, individuals can improve their health condition handling, gain valuable insights, and build connections that empower them on their journey to better health. Consider visiting a local farmers’ market this week to explore fresh produce options that can support your diabetes-friendly diet.
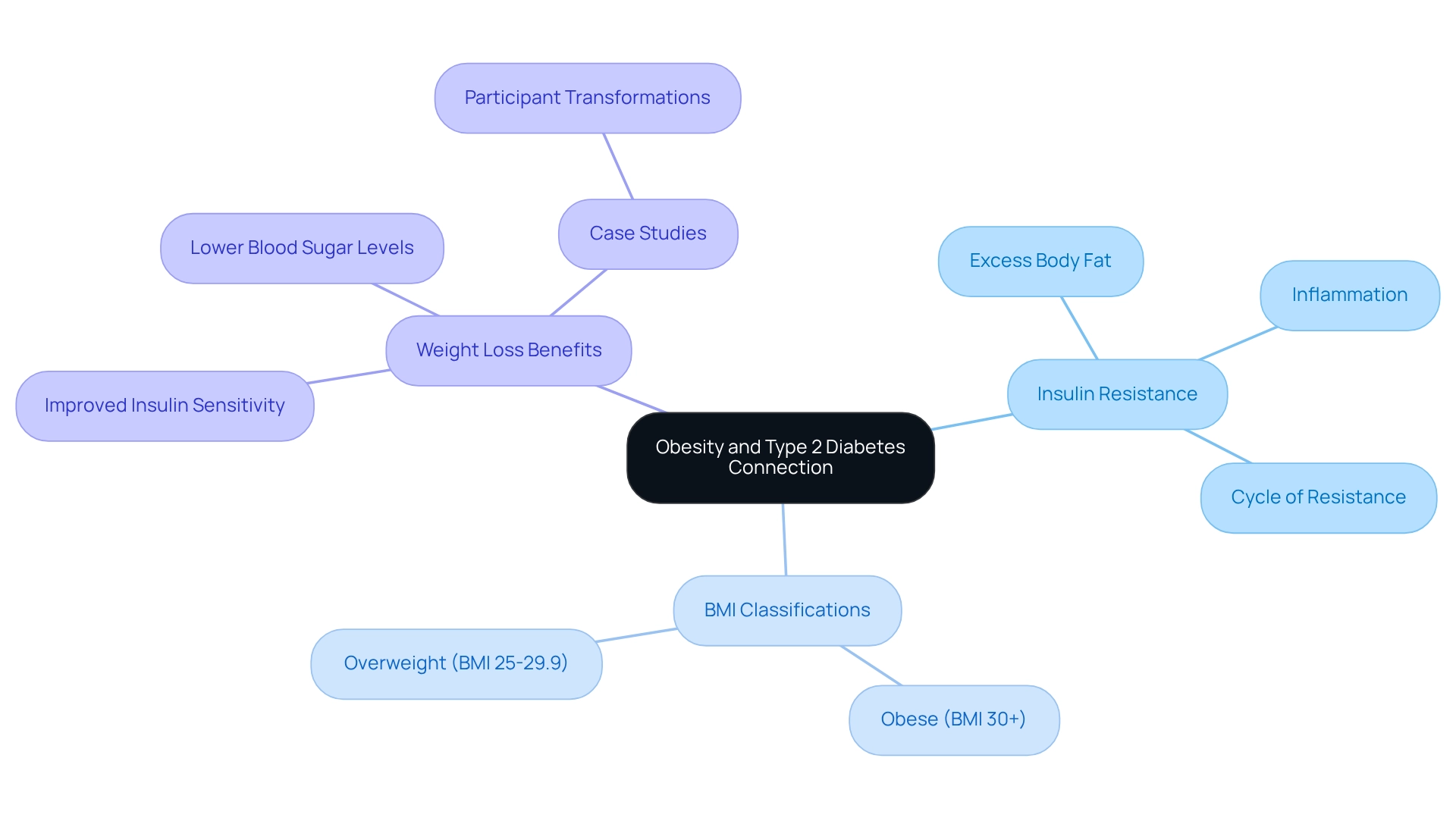
Obesity and Type 2 Diabetes: Understanding the Connection
Obesity is a significant risk factor for developing type 2 diabetes, and understanding the facts on type 2 diabetes is crucial for effective management. Let’s explore how these elements are interconnected:
- Insulin Resistance: It’s important to recognize that excess body fat, especially around the abdomen, contributes to insulin resistance. The facts on type 2 diabetes indicate that this condition makes it difficult for the body to use insulin effectively and is common among individuals with obesity, which increases their vulnerability to diabetes-related complications. This inflammation exacerbates insulin resistance, creating a harmful cycle that complicates the management of diabetes, which is why understanding the facts on type 2 diabetes, including the weight loss benefits that show even modest weight loss can significantly improve insulin sensitivity and lower blood sugar levels, is crucial. For instance, losing just 5-10% of body weight can lead to substantial improvements in metabolic health. Participants in Dr. Jason Shumard’s 30-Day Diabetes Reset program have shared remarkable transformations, including one individual who lost 55 lbs and lowered their A1C from 9.1 to 5.7. This illustrates the program’s effectiveness in promoting weight loss and enhancing overall health.
- BMI Classifications: Understanding BMI classifications is essential. A BMI of 30 or above is considered obese, while 25 to 29.9 is classified as overweight. Recognizing these categories can help individuals identify their risk levels and take proactive steps toward improving their health by understanding the facts on type 2 diabetes, which emphasize the importance of a holistic approach that includes dietary changes—like increasing whole foods and reducing processed sugars—regular exercise such as walking or strength training, and behavioral modifications to effectively address obesity. Programs like the 30-Day Diabetes Reset empower individuals with the knowledge and resources needed for sustainable lifestyle changes. As one participant expressed, ‘I feel so much better… I lost a lot of weight, have more energy, and feel great,’ highlighting the positive impact of Dr. Shumard’s holistic approach. By providing actionable insights and practical tools, the center fosters an environment where individuals can reclaim their well-being, leading to an improved quality of life and reduced reliance on traditional medical interventions.
By focusing on these interconnected factors, individuals can take proactive steps toward reclaiming their health and enhancing their quality of life, ultimately decreasing their dependence on conventional medical treatments.
Regular Check-Ups: The Importance of Ongoing Medical Support
Regular check-ups with healthcare providers are vital for effective diabetes management, offering numerous benefits that can significantly enhance patient outcomes:
- Monitoring Progress: Consistent visits enable healthcare professionals to track key health indicators such as blood sugar levels, weight, and overall well-being, ensuring that patients remain on the right path. Many patients find it helpful to utilize various tracking methods, including fitness apps, journals, and pedometers, to enhance this process. Implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost focus and motivation. For instance, setting a target to reach 10,000 steps daily within a month can be a practical objective for individuals.
- Preventing Complications: It’s important to recognize that early detection of potential complications is crucial. Regular evaluations can uncover problems before they intensify, enabling prompt actions that can avert serious medical concerns. Statistics indicate that approximately 73,000 lower-limb amputations occur annually among diabetics aged 20 and older, underscoring the importance of proactive care.
- Adjusting Treatment Plans: Continuous assessments enable healthcare professionals to customize medications and lifestyle suggestions according to the individual’s present condition, enhancing treatment efficacy. Regularly reviewing one’s progress not only fosters accountability but also allows for the adaptation of goals in response to changing fitness levels.
- Patient Engagement: Frequent interactions with healthcare professionals promote a cooperative method to managing blood sugar levels. This engagement empowers individuals, as they become active participants in their health journey, leading to better adherence to treatment plans. Research indicates that goal-setting persistence can positively influence performance, emphasizing the advantages of structured goals in managing health.
Expert insights highlight that regular check-ups are not just about monitoring; they are essential for education and support. John Landry, a licensed respiratory therapist, emphasizes the significance of evidence-based research in healthcare, stressing that well-informed individuals are better prepared to handle their conditions. He observes that regular check-ups can greatly lower the typical medical costs among individuals with the condition, which are 2.6 times greater than expenses without the illness.
Moreover, real-life instances from community efforts demonstrate that educational seminars and resources can greatly improve patient comprehension and involvement, fostering a supportive atmosphere for individuals managing their condition. As Ally Brooks states, “I may have a health condition, but I am not limited by it,” and Peter M. House adds, “This condition is not a burden, but a lesson in perseverance and self-care.”
Incorporating these practices into daily life can lead to improved health outcomes and a greater quality of life for individuals, especially when they understand the facts on type 2 diabetes.
Conclusion
The journey toward effective diabetes management is not only achievable but can also be transformative with the right support and resources. The Integrative Wellness Center’s 30-Day Diabetes Reset Program shines as a beacon of hope, combining personalized coaching, nutritional guidance, and tailored exercise regimens to empower individuals in reclaiming their health. By focusing on whole foods and sustainable lifestyle changes, participants can reset their metabolic health and gain the confidence needed to manage their diabetes successfully.
It’s important to recognize that understanding the interplay between obesity, insulin resistance, and diabetes is crucial for effective management. Many patients find that adopting essential lifestyle modifications, such as a balanced diet and regular physical activity, plays a significant role in improving health outcomes. Moreover, the importance of ongoing medical support through regular check-ups cannot be overstated; these consultations enable healthcare providers to monitor progress, prevent complications, and tailor treatment plans to individual needs.
Community support and education are also vital components of diabetes management. Engaging with local resources, attending workshops, and connecting with others facing similar challenges can provide invaluable insights and encouragement. As individuals embrace these holistic health strategies, they can experience significant improvements in their well-being and quality of life.
Ultimately, the path to managing diabetes effectively involves a collaborative effort, integrating knowledge, lifestyle changes, and community support. With determination and the right resources, individuals can navigate their diabetes journey and achieve lasting health transformation.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program?
The 30-Day Diabetes Reset Program is a compassionate, clinically approved approach designed to help individuals reclaim their health and well-being through personalized coaching, dietary guidance, and tailored exercise recommendations aimed at restoring metabolic health.
How does the program help participants manage their diabetes?
The program helps participants manage their diabetes by focusing on whole foods, reducing processed sugars, encouraging regular physical activity, and providing educational resources about type 2 diabetes for sustainable management of their condition.
What are some key risk factors for developing type 2 diabetes?
Key risk factors for developing type 2 diabetes include obesity, a sedentary lifestyle, poor dietary choices, and family history.
What is the significance of lifestyle changes in managing diabetes?
Lifestyle changes, such as diet and exercise, are crucial for managing diabetes-related conditions, reducing obesity, and enhancing metabolic control, as they can significantly lower the risk of developing type 2 diabetes.
What role does community wellness play in diabetes management?
Community wellness initiatives provide invaluable resources and encouragement for individuals managing their health, helping them take proactive steps towards improving their well-being.
What dietary modifications are recommended for managing type 2 diabetes?
Recommended dietary modifications include incorporating whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables while limiting processed foods and added sugars.
How much physical activity is suggested for individuals managing diabetes?
It is suggested that individuals strive for at least 150 minutes of moderate-intensity exercise each week, such as brisk walking, cycling, or swimming, to improve insulin sensitivity and regulate blood sugar levels.
What impact can weight management have on diabetes?
Even a modest weight loss of around 5-10% of body weight can lead to significant improvements in insulin sensitivity and blood sugar control, which is particularly important for those who are obese.
How can stress management techniques benefit individuals with diabetes?
Incorporating stress-reducing techniques like yoga, meditation, or deep-breathing exercises can help maintain stable blood sugar levels, as persistent stress can negatively affect blood sugar control.
What is the overall goal of the 30-Day Diabetes Reset Program?
The overall goal of the 30-Day Diabetes Reset Program is to equip individuals with the tools and knowledge necessary for long-term success in managing diabetes, ultimately improving their quality of life and reducing reliance on traditional medical treatments.