Overview
It’s important to recognize the significant geographic disparities in the prevalence of Type 2 diabetes. Many individuals in rural areas face higher rates of this condition, reaching up to 14.3%, compared to approximately 10.8% in urban settings. This reality can be disheartening, but understanding the reasons behind these differences can empower us to seek solutions. Factors such as socioeconomic status, access to healthcare resources, and lifestyle choices all play a crucial role in this landscape.
As we reflect on these challenges, it becomes clear that targeted public health strategies are essential. By addressing these disparities, we can help manage diabetes more effectively in diverse environments. Together, we can work towards healthier living and support one another in the journey to better health. Remember, you are not alone in this; there are resources and programs available, such as the 30-Day Diabetes Reset, that can guide you toward a healthier lifestyle.
Introduction
The rising prevalence of type 2 diabetes is a significant public health challenge that affects many individuals, especially when we consider the stark contrasts between urban and rural populations. With nearly 12% of the U.S. population grappling with this chronic condition, it’s important to recognize the factors contributing to these geographic disparities. Understanding these elements is vital for crafting effective management strategies that truly resonate with those impacted.
This article delves into the complexities of diabetes prevalence, shedding light on how socioeconomic status, access to healthcare, and lifestyle choices can vary significantly between different settings. Many patients find that their circumstances can greatly influence their health journey. By exploring innovative solutions and community-driven initiatives, we can see that tailored approaches are essential to empower individuals in their pursuit of better health.
Through compelling case studies and expert insights, readers will discover the potential for transformative change in diabetes management across diverse environments. Together, we can navigate these challenges and foster a supportive community that encourages healthier living.
Understanding Type 2 Diabetes Prevalence
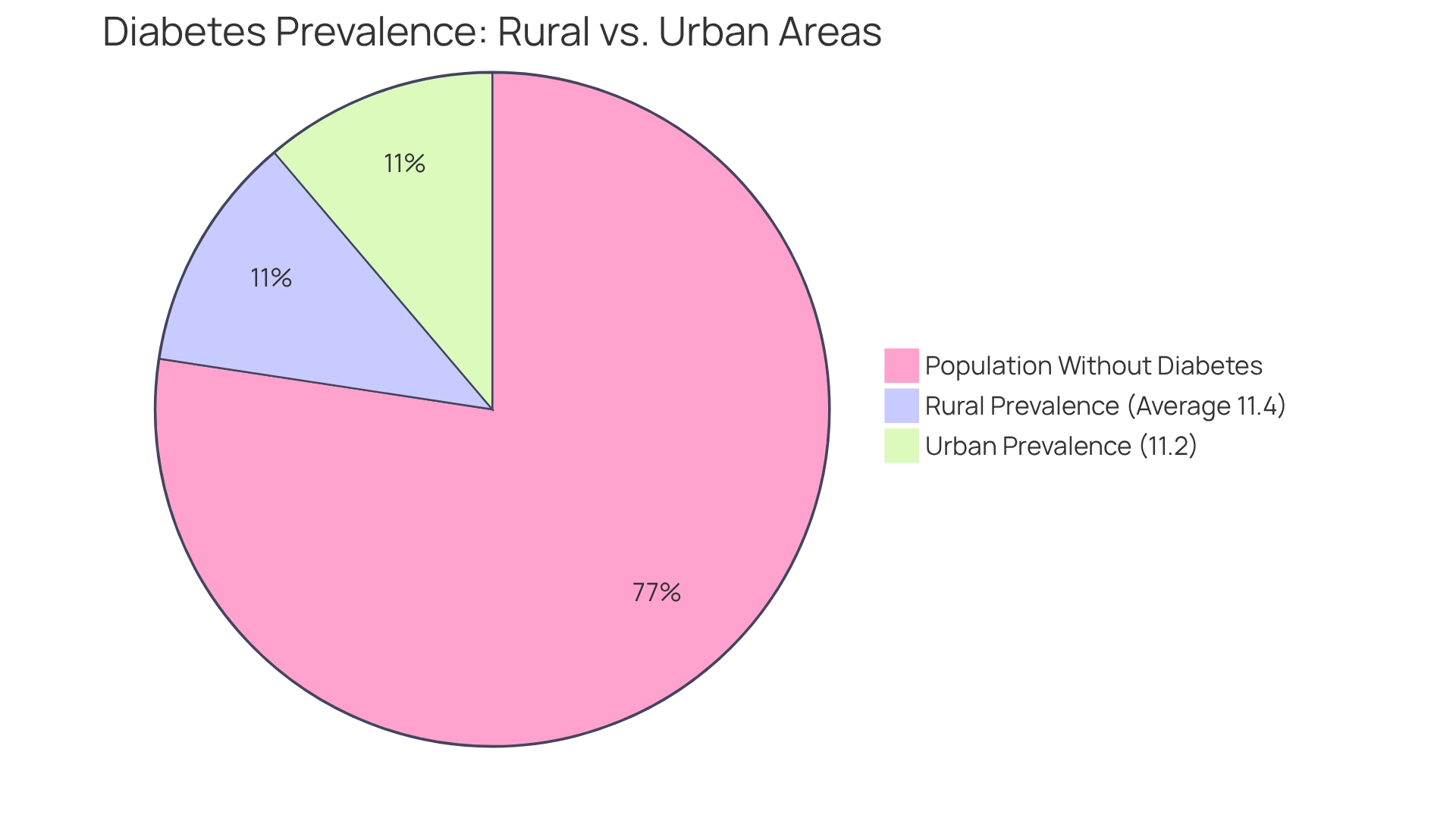
Type 2 diabetes mellitus is a persistent condition characterized by insulin resistance and increased blood sugar levels, accounting for roughly 90-95% of all occurrences of this illness. It’s concerning to note that recent estimates indicate about 11.6% of the U.S. population is affected by diabetes type 2 prevalence, highlighting notable geographic disparities. In urban settings, the diabetes type 2 prevalence is approximately 10.8%, while in rural areas, it reports rates as high as 14.3%. This disparity underscores the urgent need for targeted public wellness strategies and tailored management approaches to combat diabetes type 2 prevalence.
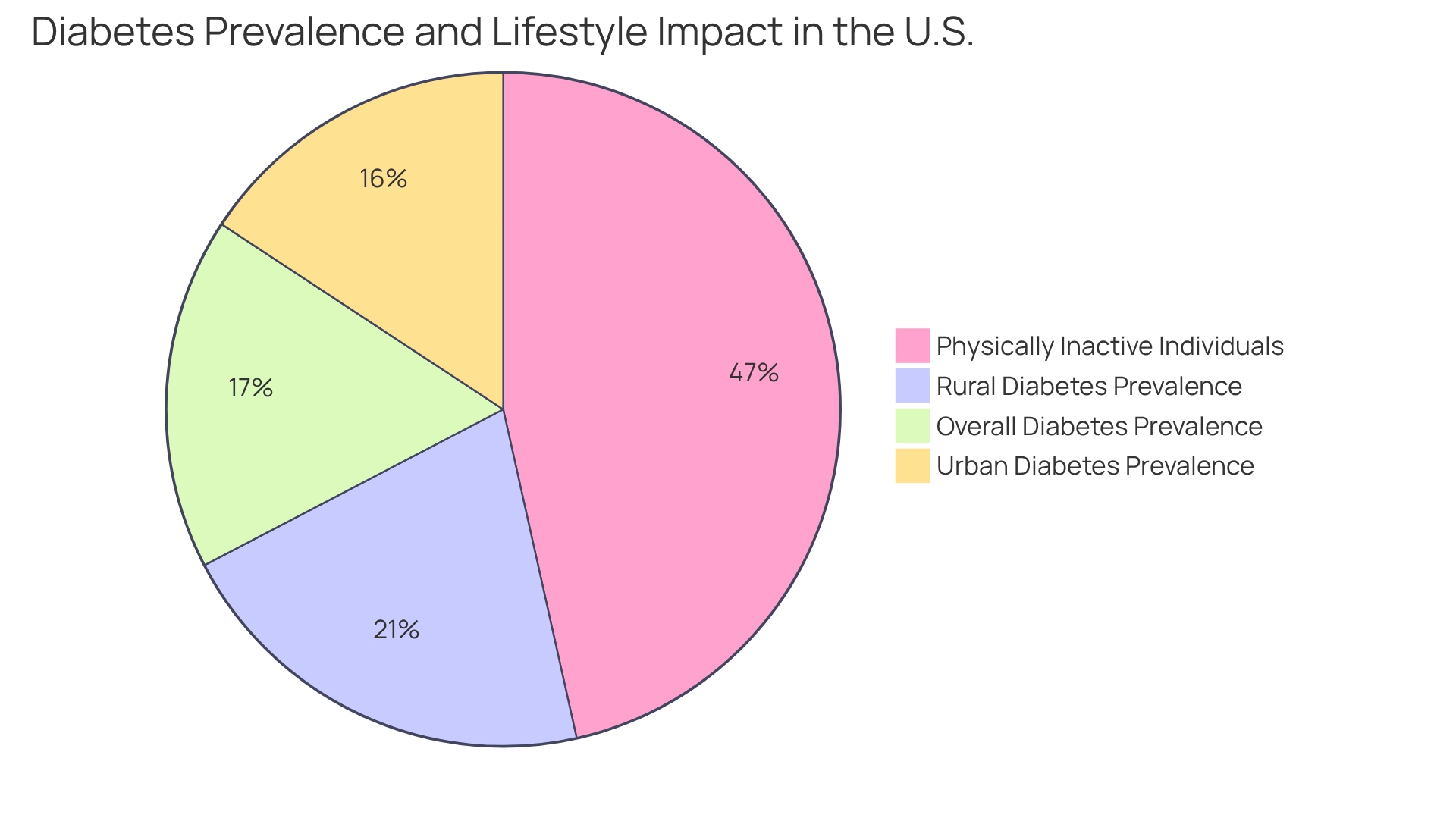
Moreover, 8.0% of U.S. adults with diagnosed conditions related to blood sugar had a non-HDL level of 190 mg/dL or higher, highlighting a specific health concern that warrants attention. Many patients find that their daily routines can significantly impact their health. Recent research highlights that 31.9% of U.S. adults with this condition are physically inactive, engaging in less than 10 minutes of moderate or vigorous activity weekly. This inactivity is a crucial area for intervention; maintaining a healthy weight and participating in regular physical activity—150 to 300 minutes weekly—can significantly postpone the onset of prediabetes or type 2 conditions.
It’s important to recognize that understanding the distinctions in diabetes type 2 prevalence between urban and rural populations is essential for developing effective treatment strategies. The CDC’s findings on these geographic disparities emphasize the importance of addressing the unique challenges faced by different communities, particularly concerning diabetes type 2 prevalence. By focusing on reversing chronic conditions, as exemplified by Dr. Jason Shumard’s 30-Day Diabetes Reset program, patients have reported transformative experiences. For instance, one patient shared, “I have lost 55 lbs. My A1C started at 9.1 after 8 months it is now 5.7,” while another stated, “I feel so much better… I lost a lot of weight, have more energy and feel great.”
These testimonials highlight the potential for comprehensive wellness solutions. By providing patients with actionable insights and practical tools, the Integrative Wellness Center fosters an environment where individuals can reclaim their health and well-being. We believe in empowering you to improve your quality of life.
Reach out to us today to discover how our programs can assist you in effectively managing your condition.
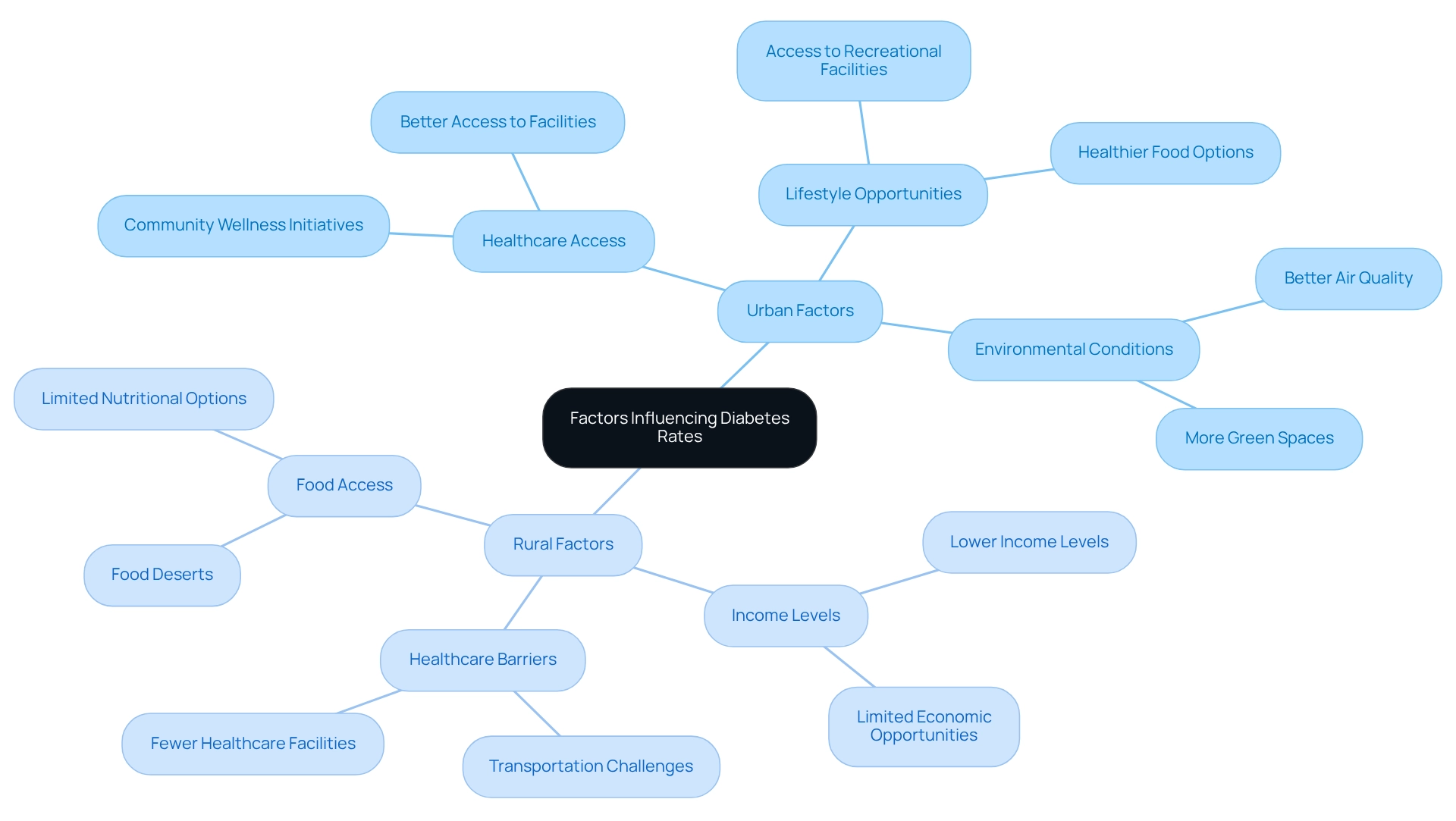
Factors Influencing Urban vs. Rural Diabetes Rates
The occurrence of type 2 conditions can vary significantly between city and countryside populations, influenced by several factors. It’s important to recognize that in San Marcos, CA, holistic lifestyle strategies can be vital in effectively managing blood sugar levels. Socioeconomic status plays a crucial role; remote communities often face lower income levels and limited access to healthcare resources, which can hinder effective diabetes management. In contrast, city areas typically provide better access to recreational facilities and healthier food options, fostering improved lifestyle choices.
Lifestyle factors are pivotal in this context. Many patients find that urban residents generally enjoy more opportunities for physical activity and access to nutritious foods, while rural populations may encounter food deserts that restrict their dietary options. In San Marcos, embracing an outdoor lifestyle by utilizing local parks and trails for regular exercise can significantly enhance physical activity levels. Engaging in activities like hiking at Lake San Marcos or walking the trails at Discovery Lake not only boosts mood but also helps manage blood sugar levels.
Furthermore, environmental conditions impact health outcomes; for instance, urban areas may benefit from better air quality and more green spaces, promoting physical activity and overall well-being. In San Marcos, the gentle climate and scenic views make outdoor activities pleasant and sustainable throughout the year, further aiding in health management.
Research indicates that rural residents face significant barriers to healthcare access, including transportation challenges and fewer healthcare facilities. These obstacles can exacerbate the diabetes type 2 prevalence, as timely medical intervention and education are essential for effective management of the disease. Community wellness initiatives in San Marcos provide invaluable assistance, offering personalized guidance and resources designed to help manage blood sugar levels effectively.
The support from the WHO Western Pacific Regional Office for community engagement initiatives underscores the importance of addressing healthcare disparities, especially in remote regions. Case studies illustrate these differences; for example, the mDengue Mobile Application Initiative demonstrates how technology and community-based projects can enhance healthcare access and education, which is relevant for managing blood sugar levels in both city and countryside environments. By addressing the unique challenges faced by both populations, healthcare providers can develop more effective strategies to combat the rising incidence of diabetes type 2 prevalence. As one expert noted, “Understanding how these interfaces influence outcomes remains a major research need,” highlighting the necessity for ongoing research in this area.
For personalized assistance and support tailored to your individual needs, consider reaching out to Dr. Jason Shumard in San Marcos, CA. He is dedicated to helping you navigate your health journey with care and expertise.
Comparative Analysis of Diabetes Prevalence Statistics
Recent research indicates that the occurrence of diabetes in countryside regions can be significantly higher than in urban environments, with estimates suggesting that 9% to 17% more individuals are affected. According to CDC data, the prevalence of diabetes in rural areas varies widely, with some states reporting figures as high as 14.3%, while others drop to 8.4%. In contrast, urban areas show an average prevalence of approximately 11.2%. It’s important to recognize that this disparity underscores the urgent need for targeted public health interventions that address the unique challenges faced by countryside communities.
Moreover, the economic implications of diabetes are substantial. Excess medical expenses per individual linked to this condition have risen from $10,179 to $12,022 between 2012 and 2022. This financial burden further highlights the necessity for effective interventions in both urban and rural regions.
Globally, while urban areas account for a larger number of diabetes cases, populations in the countryside face an increased risk for complications due to limited access to healthcare services. Many patients find that incorporating technology with community wellness initiatives presents a promising approach to address these disparities, especially in rural areas where medical resources are scarce. As Dr. Jason Shumard emphasizes, “In light of the alarming statistics surrounding hospital safety, including 7,000 incorrect medications and 80,000 infections acquired in hospitals, it is crucial for patients to explore comprehensive wellness solutions that prioritize their well-being.”
By offering patients actionable insights and practical tools, the center fosters an environment where individuals can reclaim their wellness, ultimately enhancing their quality of life and reducing dependence on traditional medical interventions. Utilizing regional expertise and technological advancements, public initiatives can more effectively tackle the significant challenge posed by high blood sugar levels in these areas. Expanded healthcare access is essential for ensuring equitable health opportunities for all individuals.
Implications for Diabetes Management in Diverse Settings
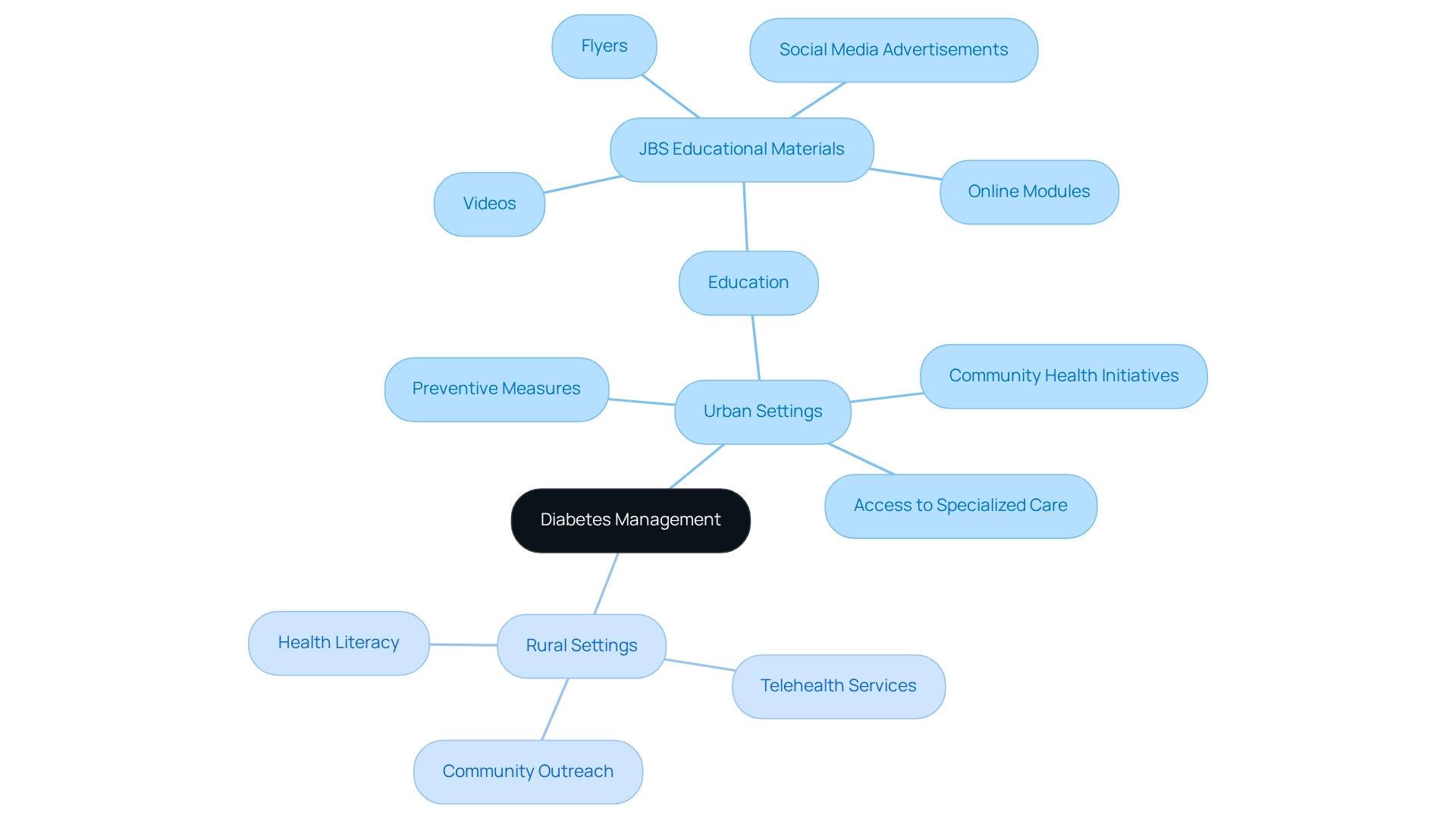
The varying rates of diabetes type 2 prevalence have profound implications for management strategies across different settings. In urban environments, healthcare providers often prioritize preventive measures and education, taking advantage of the wealth of resources and facilities available. This proactive approach can include community health initiatives and access to specialized care, which are vital for effective diabetes management. For example, educational materials developed by JBS to promote the Medicare Diabetes Prevention Program (MDPP) underscore the significance of expanded healthcare access in urban areas.
It’s important to recognize that countryside regions face unique challenges that call for innovative solutions. Many patients find that telehealth services emerge as a crucial tool, bridging the gap in healthcare access for underserved populations. These services empower individuals in remote areas to receive timely consultations and ongoing support, greatly enhancing their ability to manage their condition. Community outreach initiatives also play an essential role, addressing transportation barriers and improving health literacy among rural inhabitants. As Dr. Griffin Rodgers, Director of the National Institute of Diabetes and Digestive and Kidney Diseases, emphasizes, “Take Charge of Tomorrow,” highlighting the importance of proactive diabetes management.
Public wellness programs must be tailored to meet the specific needs of both urban and rural communities. While urban strategies may focus on leveraging technology and local health resources, rural approaches should prioritize accessibility and education. A relevant example is the Adolescent Pre-Diabetes Prevention Program, which encourages young people to adopt healthier lifestyles, potentially preventing the progression to type 2 diabetes. By customizing diabetes management strategies to the unique characteristics of these environments, healthcare providers can enhance patient outcomes and reduce the overall burden of diabetes, especially in relation to diabetes type 2 prevalence.
Moreover, incorporating effective methods for monitoring progress and establishing objectives, such as utilizing fitness applications and creating SMART goals, can empower patients to take charge of their health. The necessity of expanded healthcare access is crucial in this context, ensuring equitable health opportunities for all individuals. Remember, you are not alone in this journey; support is available, and taking small steps can lead to meaningful changes.
Conclusion
The disparities in type 2 diabetes prevalence between urban and rural populations highlight an urgent need for tailored health strategies. With rural areas facing higher rates of diabetes—up to 14.3% compared to around 10.8% in urban settings—it’s important to recognize that socioeconomic factors, access to healthcare, and lifestyle choices significantly influence health outcomes. Understanding these factors is crucial for creating effective management approaches that cater to the unique needs of different communities.
Many patients find that innovative solutions, such as telehealth services and community outreach programs, emerge as critical tools in combating the challenges faced by rural populations. These strategies not only enhance access to healthcare but also foster education and support, which are essential for empowering individuals to manage their diabetes effectively. By leveraging technology and local resources, healthcare providers can bridge the gap in service delivery, ensuring that all individuals, regardless of their geographical location, have the opportunity to improve their health.
Ultimately, addressing the complexities of diabetes management requires a comprehensive and adaptable approach. By focusing on customized interventions informed by the diverse experiences of both urban and rural populations, healthcare systems can make significant strides in reducing the prevalence and impact of type 2 diabetes. The journey towards better health is a collective effort. With the right support and resources, individuals can reclaim their well-being and thrive.
Frequently Asked Questions
What is Type 2 diabetes mellitus?
Type 2 diabetes mellitus is a persistent condition characterized by insulin resistance and increased blood sugar levels, accounting for roughly 90-95% of all occurrences of this illness.
What percentage of the U.S. population is affected by Type 2 diabetes?
Recent estimates indicate that about 11.6% of the U.S. population is affected by Type 2 diabetes.
Are there geographic disparities in Type 2 diabetes prevalence in the U.S.?
Yes, there are notable geographic disparities; in urban settings, the prevalence is approximately 10.8%, while in rural areas, it can be as high as 14.3%.
What health concern is highlighted regarding non-HDL levels among U.S. adults with blood sugar conditions?
About 8.0% of U.S. adults with diagnosed blood sugar-related conditions have a non-HDL level of 190 mg/dL or higher.
How does physical activity relate to Type 2 diabetes management?
Recent research shows that 31.9% of U.S. adults with Type 2 diabetes are physically inactive, engaging in less than 10 minutes of moderate or vigorous activity weekly. Regular physical activity of 150 to 300 minutes weekly can significantly postpone the onset of prediabetes or Type 2 diabetes.
Why is understanding diabetes prevalence differences between urban and rural populations important?
Understanding these distinctions is essential for developing effective treatment strategies and addressing the unique challenges faced by different communities regarding diabetes management.
What is the 30-Day Diabetes Reset program?
The 30-Day Diabetes Reset program, exemplified by Dr. Jason Shumard, focuses on reversing chronic conditions, helping patients achieve significant health improvements.
Can you share testimonials from patients who have participated in wellness programs?
Yes, one patient reported losing 55 lbs and improving their A1C from 9.1 to 5.7 after 8 months, while another noted feeling better, losing weight, having more energy, and feeling great.
How does the Integrative Wellness Center support individuals with Type 2 diabetes?
The Integrative Wellness Center provides patients with actionable insights and practical tools to help them reclaim their health and well-being.