Overview
This article highlights the compassionate approach to crafting an effective diabetes questionnaire, aimed at improving patient management and health outcomes. It’s important to recognize that including key components—such as demographic information, medical history, and self-monitoring practices—can significantly empower individuals in their journey to manage diabetes. Clarity and relevance in the questions are essential, as they help patients feel understood and supported.
Many patients find that when they can share their experiences and challenges, it leads to better health outcomes. By thoughtfully considering the questions we ask, we can create a dialogue that fosters trust and encourages self-reflection. This not only enhances the quality of the information gathered but also nurtures a sense of collaboration in managing their health.
Ultimately, the goal is to guide individuals toward a healthier lifestyle, making it easier for them to engage with their diabetes management actively. Together, we can enhance the quality of care and support that patients receive, paving the way for a brighter, healthier future.
Introduction
In the realm of diabetes management, it’s important to recognize the profound impact a well-crafted questionnaire can have. These tools are not just forms; they are vital instruments for healthcare providers, allowing them to understand patient perspectives, identify knowledge gaps, and tailor interventions to meet individual needs. Many patients find that effective diabetes questionnaires enhance their engagement and adherence to treatment plans, fostering a collaborative relationship with their providers. This partnership can lead to significantly improved health outcomes.
As healthcare continues to evolve, the integration of comprehensive components and clear communication in these questionnaires becomes essential. This empowers individuals to take charge of their diabetes management journey. Have you ever felt overwhelmed by the complexities of diabetes? You’re not alone. This article delves into the critical elements of designing an impactful diabetes questionnaire, offering insights that can transform patient care and enhance overall well-being. Together, we can navigate this journey toward better health.
Understand the Purpose of a Diabetes Questionnaire
A health assessment tool plays a vital role in managing individuals, helping to evaluate their understanding of their condition, identify knowledge gaps, and assess self-management practices. By gathering comprehensive data, healthcare professionals can tailor interventions to meet specific needs, ultimately enhancing wellness outcomes. It’s important to recognize that recent research highlights how effective surveys for managing health conditions significantly boost individual involvement, which is crucial for adhering to treatment strategies.
Many patients find that a thoughtfully designed survey can uncover common misunderstandings about blood sugar management. This insight allows for targeted educational programs that empower individuals to take charge of their well-being. Furthermore, expert insights stress the importance of these tools in promoting healthcare education, with evidence suggesting that greater treatment satisfaction correlates with more optimal treatment behaviors. Dr. Jason Shumard emphasizes that higher treatment satisfaction is expected to be linked to more effective treatment behavior.
Real-life examples demonstrate that implementing questionnaires for blood sugar management not only enhances self-management but also underscores the importance of personalized care, leading to improved health results. Significantly, 78% of the tools used in blood sugar management were developed in the USA or the UK, indicating a level of reliability in these resources. Additionally, the case study titled ‘Patient Involvement in Health Management’ highlights the essential role of individual participation in health management, fostering a collaborative approach between individuals and healthcare professionals. This partnership contributes to better adherence to treatment plans and improved health outcomes.
The DSMQ-R has emerged as a key enhancement for self-management evaluation, showcasing how surveys can evolve to better meet individual needs. A literature review conducted from January 1985 to March 2020 across six databases, including MEDLINE and Scopus, further affirms the effectiveness of the diabetes questionnaire in enhancing the management of individuals facing blood sugar challenges.
By integrating Dr. Jason Shumard’s comprehensive wellness solutions and personalized functional medicine approaches, individuals can receive tailored support that addresses their specific wellness challenges. This ultimately empowers them to make effective lifestyle changes for managing their type 2 condition. Don’t forget, by participating in our upcoming event, you can receive Dr. Jason Shumard’s book on reversing type 2 conditions for free as a gesture of appreciation. Register now to reserve your copy!
Identify Key Components to Include
When crafting a diabetes questionnaire, it’s important to recognize the challenges patients face in managing their health. Including several key components can provide a comprehensive view of their health and management strategies, ultimately supporting their journey toward better well-being.
- Demographic Information: Gathering data on age, gender, and ethnicity is essential. These factors can significantly impact the management of diabetes and health outcomes. Many patients find that understanding these demographics helps tailor their care. For instance, studies indicate that certain demographic groups may experience higher rates of diabetes-related complications.
- Medical History: Recording prior diagnoses, family background of blood sugar issues, and any comorbid conditions is crucial. Research shows that comorbidities like hypertension and cardiovascular disease are common among individuals with diabetes, influencing treatment strategies and results. This information can help healthcare providers offer more personalized support.
- Current Medications: A thorough list of all medications, including insulin and oral hypoglycemics, is necessary to assess adherence and effectiveness. Understanding medication regimens is vital, as it helps identify potential barriers to optimal management. Patients often feel empowered when they have clarity about their treatments.
- Self-Monitoring Practices: Inquiring about the frequency and techniques of blood glucose monitoring can provide insights into individual engagement and self-management capabilities. Effective self-monitoring is linked to improved glycemic control. Many patients find that utilizing tracking methods, like fitness apps or journals, enhances their practice, allowing them to monitor their progress effectively.
- Dietary Habits: Questions regarding meal patterns, carbohydrate intake, and understanding nutrition labels are essential. Dietary choices play a critical role in diabetes management, and awareness of nutrition can empower patients to make healthier decisions. Integrative functional medicine highlights customized nutrition strategies that address personal requirements, improving metabolic function and overall wellness.
- Physical Activity: Assessing the type, frequency, and duration of physical activities helps evaluate lifestyle choices. Consistent physical activity is linked to improved blood sugar regulation and general well-being. Setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost motivation and adherence to exercise routines.
- Emotional Well-being: Including questions about stress levels and mental condition can help identify areas needing support. Emotional well-being is increasingly acknowledged as a vital element of effective management of blood sugar levels. Dr. Jason Shumard emphasizes that addressing mental health is crucial for comprehensive care of blood sugar conditions, stating, “His innovative methodologies offer a unique value proposition in the healthcare landscape.”
In addition to these components, utilizing tools like the Diabetes Self-Management Questionnaire-Revised (DSMQ-R) can enhance the effectiveness of the questionnaire. The DSMQ-R possesses good clinimetric properties, making it valuable for identifying barriers and facilitators of self-management in individuals with a metabolic disorder. The reference period for the tool’s responsiveness is eight weeks, adjustable to four weeks for identifying short-term changes, which is crucial for tracking progress in managing blood sugar levels.
Ethical factors in studies involving human subjects are crucial, guaranteeing that the creation and execution of health management surveys comply with the highest standards of integrity and regard for individual rights. By combining these elements, the survey will not only capture a comprehensive perspective of the patient’s condition management but also aid in identifying areas for improvement, ultimately leading to enhanced health results.
Draft the Questionnaire with Clear and Concise Questions
When drafting your diabetes questionnaire, it’s essential to keep clarity and conciseness in mind. Here are some helpful guidelines that can make a difference:
- Use Simple Language: It’s important to steer clear of medical jargon and complex terms. For instance, instead of asking, “What is your glycemic control strategy?” you might say, “How do you manage your blood sugar levels?”
- Be Specific: Frame your questions to elicit precise information. Rather than simply asking, “Do you exercise?” specify, “How many days a week do you engage in physical activity?”
- Limit Response Options: Offering multiple-choice answers or scales (e.g., 1-5) can streamline responses. For example, consider asking, “How often do you check your blood sugar? (Never, Rarely, Sometimes, Often, Always)”
- Avoid Leading Questions: Ensure your questions remain neutral and do not imply a preferred answer. Instead of asking, “Don’t you think it’s important to eat healthy?” consider, “How important is healthy eating to you?”
- Pilot Test the Survey: Conducting a pilot test with a small group before finalizing the survey can help identify any confusing questions and allow for necessary adjustments.
Incorporating these guidelines is crucial, especially in light of the findings from the case study titled ‘Need for Rigorous Diabetes Education.’ This study emphasizes the prevalence of misconceptions about diabetes management and highlights the necessity for effective educational efforts, including the use of a diabetes questionnaire. By ensuring clarity in your questionnaire, you can help mitigate these misconceptions and enhance understanding.
As Dr. Jason Shumard states, “By offering individuals with actionable insights and practical tools, the center promotes a setting where they can regain their health and well-being, ultimately resulting in enhanced quality of life and decreased dependence on traditional medical interventions.” This quote underscores the importance of clear communication in empowering patients.
Additionally, consider the significance of monitoring progress and establishing SMART objectives in managing health. Utilizing various tracking methods such as fitness apps, journals, and pedometers can significantly enhance motivation and accountability. For instance, setting specific targets, such as aiming for a certain number of steps daily or gradually increasing physical activity, can greatly boost your motivation. Research indicates that goal-setting persistence scores can positively impact performance; for instance, scores improved from 3.4 (SD = 2.0) to 3.8 (SD = 1.9) in specific conditions, demonstrating the effectiveness of structured goal-setting. Regularly reviewing your progress not only fosters a sense of achievement but also allows for the adaptation of goals in response to changing health conditions. By following these recommendations, you can create a survey that efficiently collects important information from individuals, ultimately improving their involvement and comprehension of managing blood sugar.
Test and Revise the Questionnaire for Clarity and Relevance
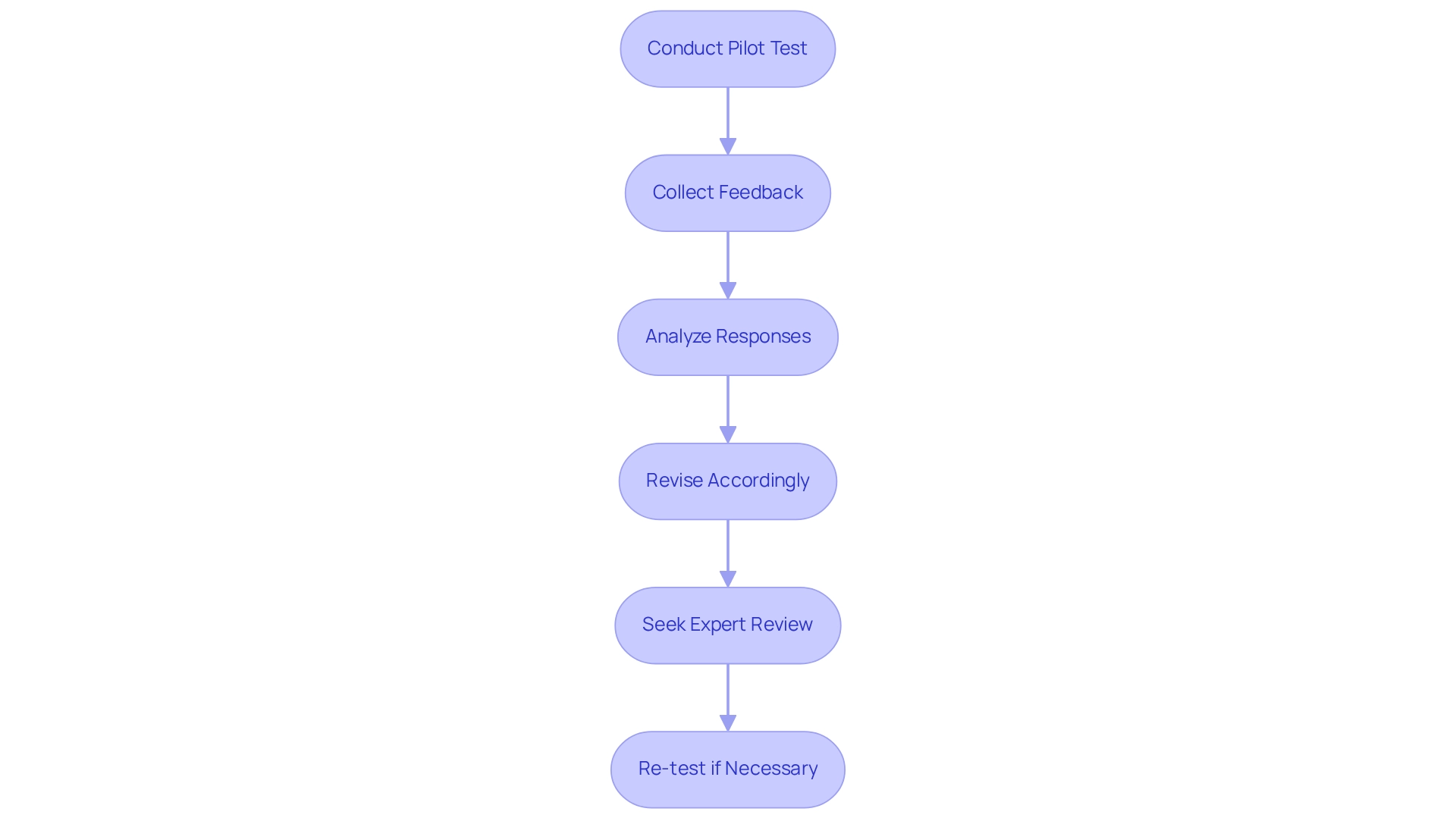
To ensure your diabetes questionnaire is truly effective, it’s essential to follow these thoughtful steps for testing and revision:
- Conduct a Pilot Test: Begin by administering the survey to a small, diverse group of patients. This initial feedback on clarity and relevance is invaluable. Research shows that pilot testing can enhance the reliability of health surveys by up to 30%.
- Collect Feedback: Engage participants in conversations about their understanding of the questions, the time it took to complete the survey, and any areas of confusion they encountered. This feedback is crucial for refining the survey to meet the needs of those managing type 2 diabetes.
- Analyze Responses: Take a close look at the collected data for patterns that may suggest questions are being misinterpreted or not yielding useful information. Continuous monitoring is vital to ensure effectiveness and sustainability over time, allowing for ongoing adjustments based on patient insights.
- Revise Accordingly: Make adjustments to the survey based on the feedback received. This could involve rephrasing questions, adding new ones, or removing those that don’t provide valuable insights. Tailoring the survey to reflect comprehensive lifestyle approaches—like incorporating local produce from San Marcos farmers’ markets and emphasizing outdoor activities such as hiking and walking—can significantly enhance its relevance.
- Seek Expert Review: It’s beneficial to have healthcare professionals review the updated survey to ensure it aligns with best practices in managing blood sugar conditions. Dr. Jason Shumard emphasizes, “By offering individuals actionable insights and practical tools, the center cultivates an atmosphere where people can regain their wellness and well-being.”
- Re-test if Necessary: Should significant changes be made, consider conducting another pilot test to validate these revisions.
By thoroughly examining and refining your survey, you can greatly enhance its effectiveness as a tool for improving diabetes management. This ultimately empowers individuals to take charge of their well-being. The positive impact of effective questionnaire design is reflected in the outcomes reported by patients at Dr. Shumard’s center, who express gratitude for the empowerment they feel in managing their health through personalized guidance, community support, and the integration of local resources.
Conclusion
A well-designed diabetes questionnaire is not just a tool; it’s a vital part of effective diabetes management. It serves to assess patient understanding, identify knowledge gaps, and tailor interventions to meet individual needs. It’s important to recognize that including key components—such as demographic information, medical history, current medications, self-monitoring practices, dietary habits, physical activity, and emotional well-being—can provide healthcare providers with a holistic view of a patient’s management strategies. This comprehensive approach is essential for optimizing care and improving health outcomes.
Many patients find that clear and concise questions in the questionnaire make a significant difference. Utilizing simple language, being specific, and limiting response options are vital strategies to enhance understanding and engagement. Pilot testing the questionnaire and revising it based on feedback ensures that it remains relevant and effective in addressing the complexities of diabetes management.
Ultimately, integrating comprehensive questionnaires into diabetes care fosters a collaborative relationship between patients and healthcare providers. It empowers individuals to take charge of their health. As patients become more engaged and informed, they are better equipped to adhere to treatment plans, leading to improved health outcomes and a better quality of life. The journey towards effective diabetes management is paved with clear communication, personalized strategies, and a commitment to patient-centered care. Remember, you are not alone in this journey; support is always available to help you thrive.
Frequently Asked Questions
What is the purpose of a health assessment tool?
A health assessment tool helps manage individuals by evaluating their understanding of their condition, identifying knowledge gaps, and assessing self-management practices. It enables healthcare professionals to tailor interventions to enhance wellness outcomes.
How do effective surveys impact individual involvement in health management?
Recent research indicates that effective surveys significantly boost individual involvement, which is crucial for adhering to treatment strategies.
What insights can surveys provide regarding blood sugar management?
Thoughtfully designed surveys can uncover common misunderstandings about blood sugar management, allowing for targeted educational programs that empower individuals to take charge of their well-being.
What correlation exists between treatment satisfaction and treatment behavior?
Evidence suggests that greater treatment satisfaction is linked to more optimal treatment behaviors, as emphasized by Dr. Jason Shumard.
What are the benefits of implementing questionnaires for blood sugar management?
Implementing questionnaires enhances self-management and underscores the importance of personalized care, leading to improved health results.
Where were most tools for blood sugar management developed?
Significantly, 78% of the tools used in blood sugar management were developed in the USA or the UK, indicating their reliability.
What does the case study titled ‘Patient Involvement in Health Management’ highlight?
The case study emphasizes the essential role of individual participation in health management, fostering a collaborative approach between individuals and healthcare professionals, which contributes to better adherence to treatment plans and improved health outcomes.
What is the DSMQ-R, and how does it enhance self-management evaluation?
The DSMQ-R is a key enhancement for self-management evaluation, showcasing how surveys can evolve to better meet individual needs in managing blood sugar challenges.
What does the literature review from January 1985 to March 2020 indicate regarding diabetes questionnaires?
The literature review affirms the effectiveness of diabetes questionnaires in enhancing the management of individuals facing blood sugar challenges.
How can individuals receive tailored support for managing their type 2 condition?
By integrating Dr. Jason Shumard’s comprehensive wellness solutions and personalized functional medicine approaches, individuals can receive tailored support that addresses their specific wellness challenges.
What opportunity is available for individuals who participate in the upcoming event?
Participants can receive Dr. Jason Shumard’s book on reversing type 2 conditions for free as a gesture of appreciation by registering for the event.