Overview
This article delves into the vital resources and strategies for effective meal planning, especially for those managing diabetes. It’s important to recognize the challenges you may face, and using tools like diabetic diet PDFs can significantly support your dietary choices. Structured meal planning not only aids in maintaining stable blood sugar levels but also empowers you to make informed food selections. Many patients find that this approach fosters a sense of control over their health, leading to improved outcomes. Testimonials and statistical improvements in blood sugar stability highlight the positive impact of these strategies, encouraging you to take action toward a healthier lifestyle.
Introduction
In the journey of managing diabetes, it’s important to recognize that effective meal planning plays a crucial role. This vital tool empowers individuals to take control of their dietary choices, ensuring balanced nutrition while maintaining stable blood sugar levels. Many patients find that as the landscape of diabetes care evolves, strategies such as:
- Carbohydrate counting
- Portion control
- The incorporation of healthy fats
become essential components of a successful management plan. With the right resources and support, individuals can navigate the complexities of their dietary needs, leading to transformative health outcomes. This article explores the multifaceted approach to meal planning for diabetes, delving into effective dietary patterns, essential resources, and the critical role of education and support in fostering sustainable lifestyle changes. Together, we can work towards a healthier future.
The Importance of Meal Planning for Diabetes Management
Meal planning is a cornerstone of effective diabetes management, as highlighted in the diabetic diet pdf. It enables individuals to exert greater control over their carbohydrate intake and maintain stable blood sugar levels. By thoughtfully planning dishes in advance, patients can ensure they consume balanced diets that include appropriate portions of carbohydrates, proteins, and healthy fats. This proactive strategy not only minimizes the risk of impulsive eating but also promotes healthier food choices, ultimately leading to better health outcomes.
It’s important to recognize that diets rich in monounsaturated fats (MUFA) are associated with a lower risk of cardiovascular disease. This emphasizes the importance of choosing healthy fat sources in planning meals. Dietary fat intake should primarily come from healthy sources of mono and polyunsaturated fats while limiting saturated and trans fats. Resources such as dining planning templates and comprehensive food lists, along with a diabetic diet pdf, can significantly simplify this process, helping individuals adhere to their dietary goals.
Many patients find that a well-organized dietary plan, typically including three courses and two snacks per day, spaced evenly, helps prevent blood sugar spikes. Including a range of foods—like non-starchy vegetables, lean proteins, and whole grains—guarantees a balanced diet that promotes overall well-being. Case studies have demonstrated that individuals who participate in planning their food experience improved blood sugar control and a greater sense of empowerment over their health.
Transformative patient testimonials from Dr. Jason Shumard’s 30-Day Diabetes Reset program highlight life-changing outcomes. Patients report significant weight loss, reduced medication needs, and improved overall well-being. One patient remarked, “I lost 55 lbs and my A1C decreased from 9.1 to 5.7, thanks to the organized dietary planning and support I received.”
In 2025, the importance of meal planning for managing blood sugar levels is further emphasized by statistics showing that structured meal planning can lead to a 30% improvement in blood sugar stability among patients. This approach not only assists in managing blood sugar levels but also promotes a comprehensive understanding of nutrition. Referring to the diabetic diet pdf can enhance this understanding, as highlighted by Dr. Jason Shumard’s dedication to individualized care and education. Dr. Shumard states, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their well-being, ultimately leading to improved quality of life and reduced reliance on conventional medical interventions.”
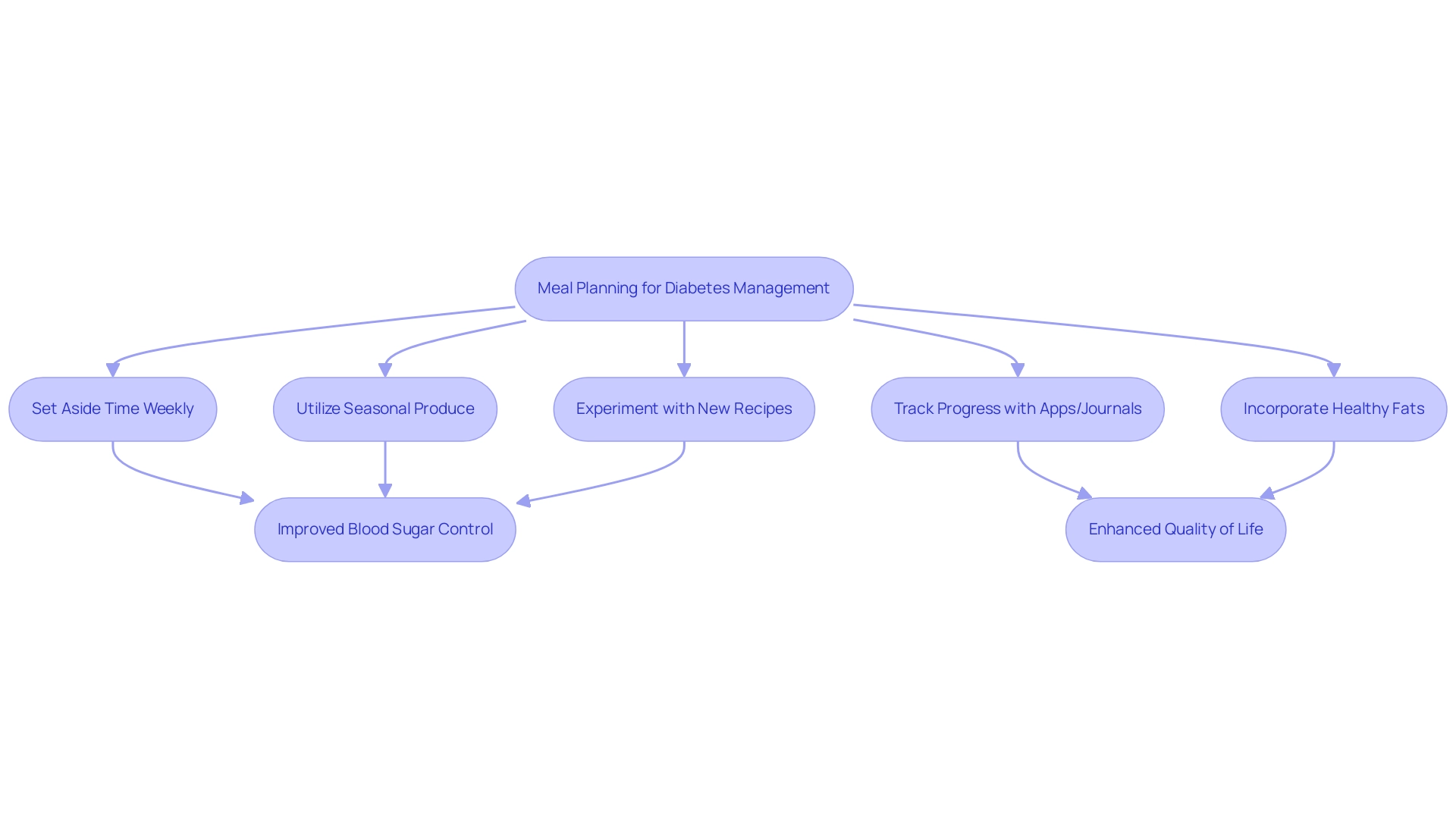
Effective planning strategies for type 2 diabetes patients involve:
- Setting aside time each week to prepare dishes
- Utilizing seasonal produce for variety
- Experimenting with new recipes that align with dietary needs
Incorporating tracking methods such as fitness apps and journals can further enhance accountability and progress monitoring. Moreover, including plant sterols and stanols in the diet can assist in reducing LDL cholesterol, promoting overall well-being.
By prioritizing goal-setting and consistent progress tracking within their meal planning practices, patients can cultivate a sense of achievement, maintain engagement in their health journey, and enhance their quality of life.
Exploring Effective Dietary Patterns for Diabetics
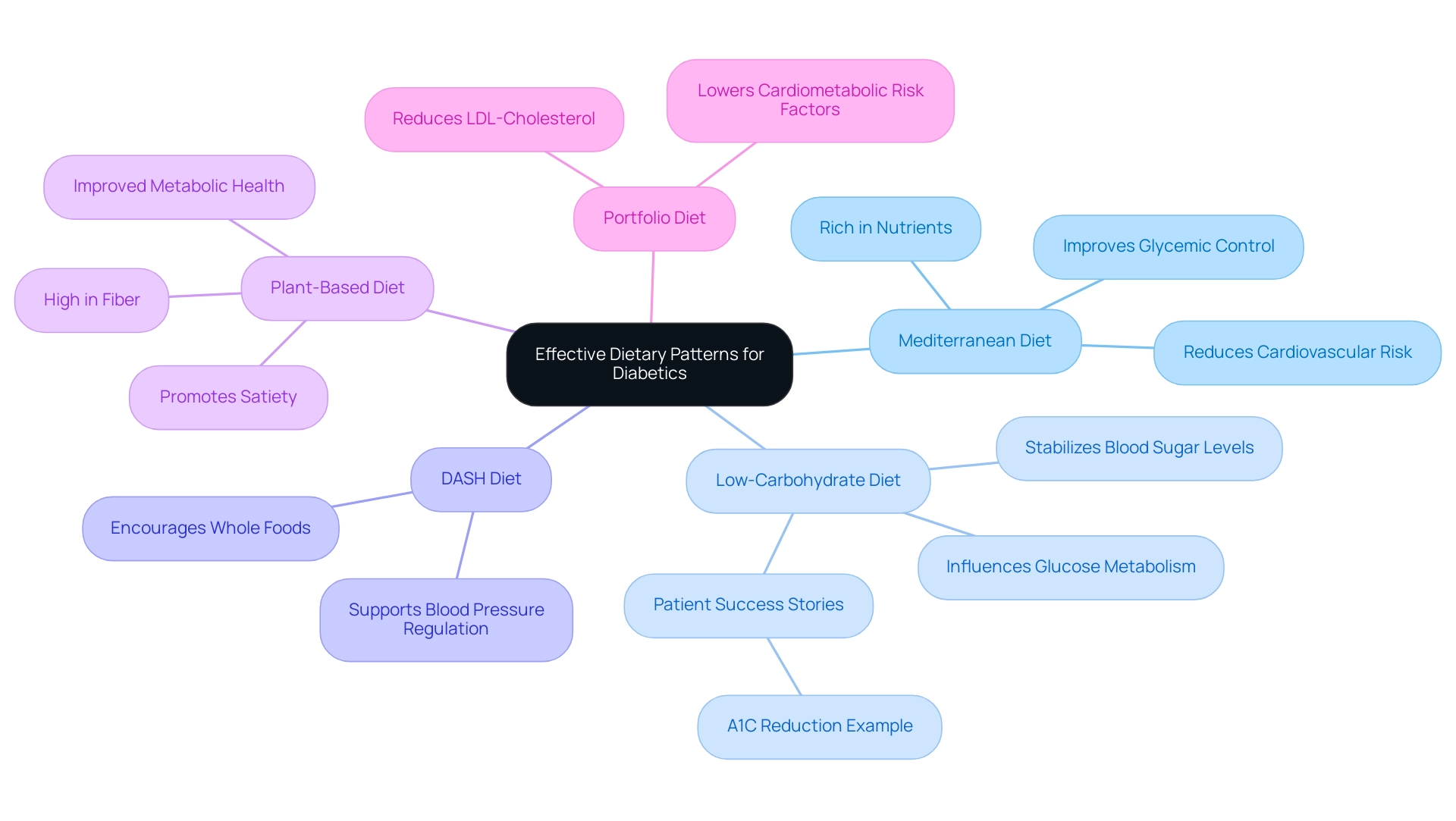
Managing type 2 diabetes can be challenging, but a range of dietary patterns offers effective strategies tailored to individual needs. The Mediterranean diet, rich in fruits, vegetables, whole grains, and healthy fats, stands out for its potential to enhance glycemic control and reduce cardiovascular risk. Recent statistics indicate that following this diet can lead to significant improvements in blood sugar levels, making it a compelling choice for those looking to manage their blood sugar effectively in 2025.
It’s important to recognize that low-carbohydrate diets also play a crucial role in stabilizing blood sugar levels. By reducing carbohydrate intake, these diets can directly influence glucose metabolism, which is especially beneficial for individuals with type 2 diabetes. Many patients at Dr. Jason Shumard’s center share inspiring success stories, reporting remarkable improvements in their glycemic control and overall well-being after adopting a low-carb lifestyle.
One patient shared, ‘I lost 55 lbs. My A1C started at 9.1 after 8 months; it is now 5.7.’ This represents a 37% decrease in A1C, highlighting the power of dietary changes.
Furthermore, the DASH diet, which emphasizes whole foods and limits sodium intake, has shown promise in managing blood sugar levels. This approach not only supports blood pressure regulation but also encourages the consumption of nutrient-dense foods that can aid in glycemic control. Many patients find that incorporating plant-based diets, which are high in fiber, leads to better health outcomes, promoting satiety and improved metabolic health.
A patient remarked, ‘I feel so much better and going through the cleanse helped in so many ways. I lost a lot of weight and have more energy.’ Additionally, the Portfolio dietary pattern, which focuses on cholesterol-lowering foods, has proven effective in reducing LDL-cholesterol and cardiometabolic risk factors, further supporting blood sugar management.
Moreover, a study found that omega-3 supplementation in participants with T2DM resulted in a significant 25% reduction in cardiovascular events, underscoring the importance of dietary choices in overall health.
Each of these dietary patterns can be customized to fit personal preferences, as outlined in a diabetic diet pdf, ensuring they remain sustainable long-term solutions for managing blood sugar. As research continues to evolve, the importance of a balanced diet tailored to individual needs becomes increasingly clear. Effective dietary management is indeed a cornerstone of successful diabetes care. Dr. Jason Shumard’s 30-Day Diabetes Reset program is designed to empower patients with actionable insights and practical tools, fostering an environment where individuals can reclaim their wellness and well-being.
This program emphasizes customized dietary planning and ongoing support, helping participants achieve their wellness goals efficiently.
Essential Printable Resources for Diabetic Meal Planning
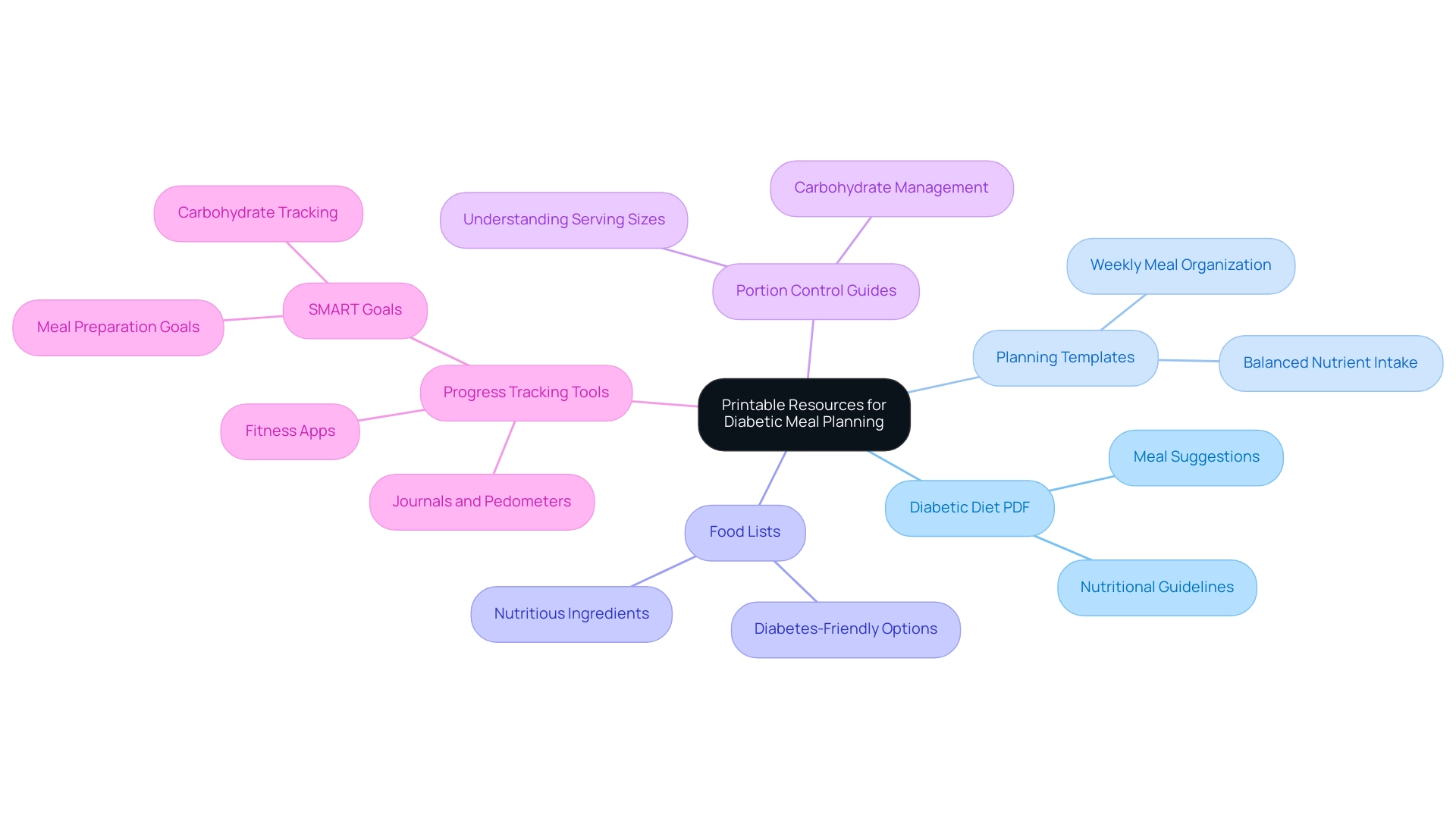
Printable resources, including a diabetic diet PDF, planning templates, food lists, and portion control guides, are essential tools for those managing type 2 diabetes. These resources not only simplify the planning process but also empower patients to make informed dietary choices that support their health goals. For instance, a well-structured printable food list enables individuals to quickly identify diabetes-friendly options while grocery shopping, ensuring they select nutritious ingredients.
It’s important to recognize that planning templates play a crucial role in organizing meals for the week, promoting a balanced intake of essential nutrients. Furthermore, portion control guides help individuals understand appropriate serving sizes, which is vital for effectively managing carbohydrate intake. A healthier breakfast alternative is generally about 400 calories, demonstrating practical nutritious choices for managing blood sugar levels.
Many patients find that utilizing structured templates significantly enhances nutritional values and user satisfaction compared to traditional planning methods. This emphasizes the influence of food planning templates on managing blood sugar levels, streamlining the process while improving dietary compliance. Additionally, the AI food planner has shown improved nutritional outcomes and satisfaction, further supporting the effectiveness of structured planning tools.
To enhance progress tracking, individuals are encouraged to utilize fitness apps, journals, and pedometers to monitor their dietary choices and physical activity levels. Implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can further empower patients in their condition management. For example, a patient might set a goal to prepare at least three diabetes-friendly meals each week or to track their daily carbohydrate intake using a journal.
Dr. Jason Shumard highlights the significance of patient education and empowerment in managing chronic conditions such as type 2 diabetes. He promotes the use of these printable resources to create a setting where individuals feel prepared to regain their wellness and well-being. As demonstrated in the case study ‘Patient Empowerment through Education,’ this comprehensive approach not only addresses the symptoms of the condition but also enables patients to gain control over their dietary decisions, ultimately resulting in enhanced well-being.
‘By offering patients actionable insights and practical tools,’ Dr. Shumard states, ‘the center promotes an environment where people can reclaim their health and well-being.
Mastering Carbohydrate Counting and Portion Control
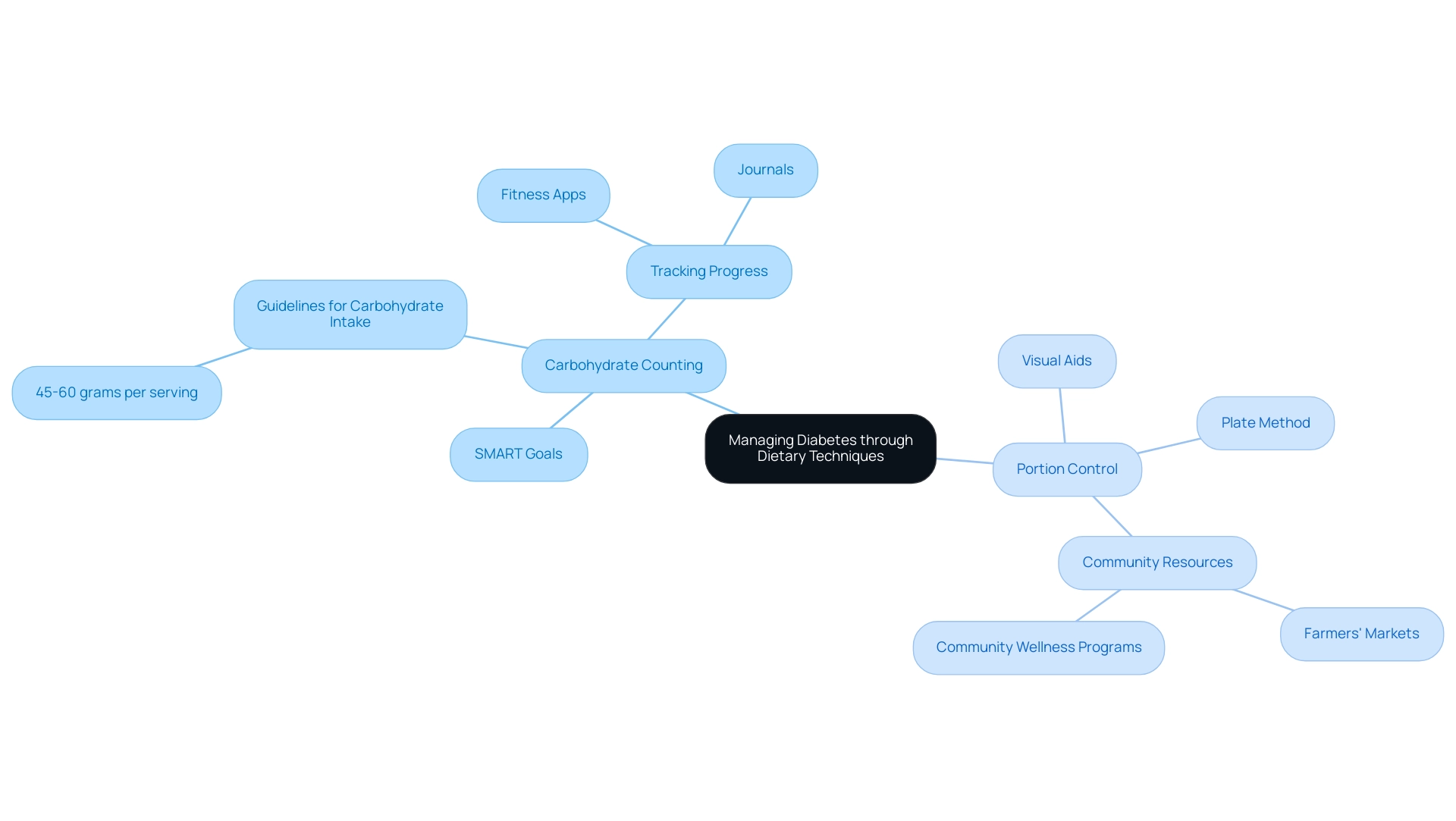
Carbohydrate counting is an essential skill for those managing diabetes. Many people find it challenging to understand how different foods affect their blood sugar levels. By accurately counting carbohydrates and setting SMART goals for dietary management, individuals can optimize their insulin doses and maintain stable blood glucose levels. Current guidelines suggest aiming for 45-60 grams of carbohydrates per serving, tailored to personal dietary needs and wellness objectives, which can significantly enhance their overall wellness journey.
It’s equally important to master portion control. Have you ever tried using visual aids, like the plate method? This technique recommends filling half of your plate with non-starchy vegetables, a quarter with lean protein, and the remaining quarter with whole grains. Such a balanced approach not only supports effective management of diabetes but also promotes overall health. Local resources in San Marcos, such as farmers’ markets and community wellness programs, can further encourage healthy eating and physical activity.
To effectively monitor and enhance your progress, consider utilizing various tracking methods, including fitness apps and journals. Research shows that these strategies can be quite effective. For example, participants in the Look AHEAD trial achieved a weight loss of 6.0% in the intervention group compared to 3.5% in the control group over 9.6 years. This highlights the long-term benefits of structured dietary management.
Moreover, evidence indicates that diets high in fiber and low in saturated fats can improve glycemic control. This underscores the importance of macronutrient quality in managing diabetes. A case study titled “The Role of Macronutrients in Diabetes Management” points out the need for balanced diets that include appropriate amounts of carbohydrates, proteins, and fats.
Experts agree that portion control is vital for maintaining healthy blood sugar levels. In recent discussions, many healthcare professionals have emphasized its role in diabetes management. One participant shared, “I believe the app ought to be configured so that you can have multiple objectives,” highlighting the importance of customized strategies in managing blood sugar levels and setting realistic goals that fit individual lifestyles.
Success stories from individuals who have embraced portion control techniques reveal transformative outcomes. Mindful eating, combined with community support and engagement in outdoor activities, can empower patients to take charge of their well-being.
In summary, merging carbohydrate counting with effective portion control and SMART goal-setting, as outlined in the diabetic diet pdf, creates a strong framework for managing diabetes. By equipping themselves with these skills and utilizing local resources, individuals can navigate their dietary choices with confidence, leading to improved wellness outcomes. Additionally, ongoing research into less intensive dietary self-monitoring strategies and initiatives like Project Accelerate Cell Therapies (Project ACT) aim to enhance care for those on their wellness journeys.
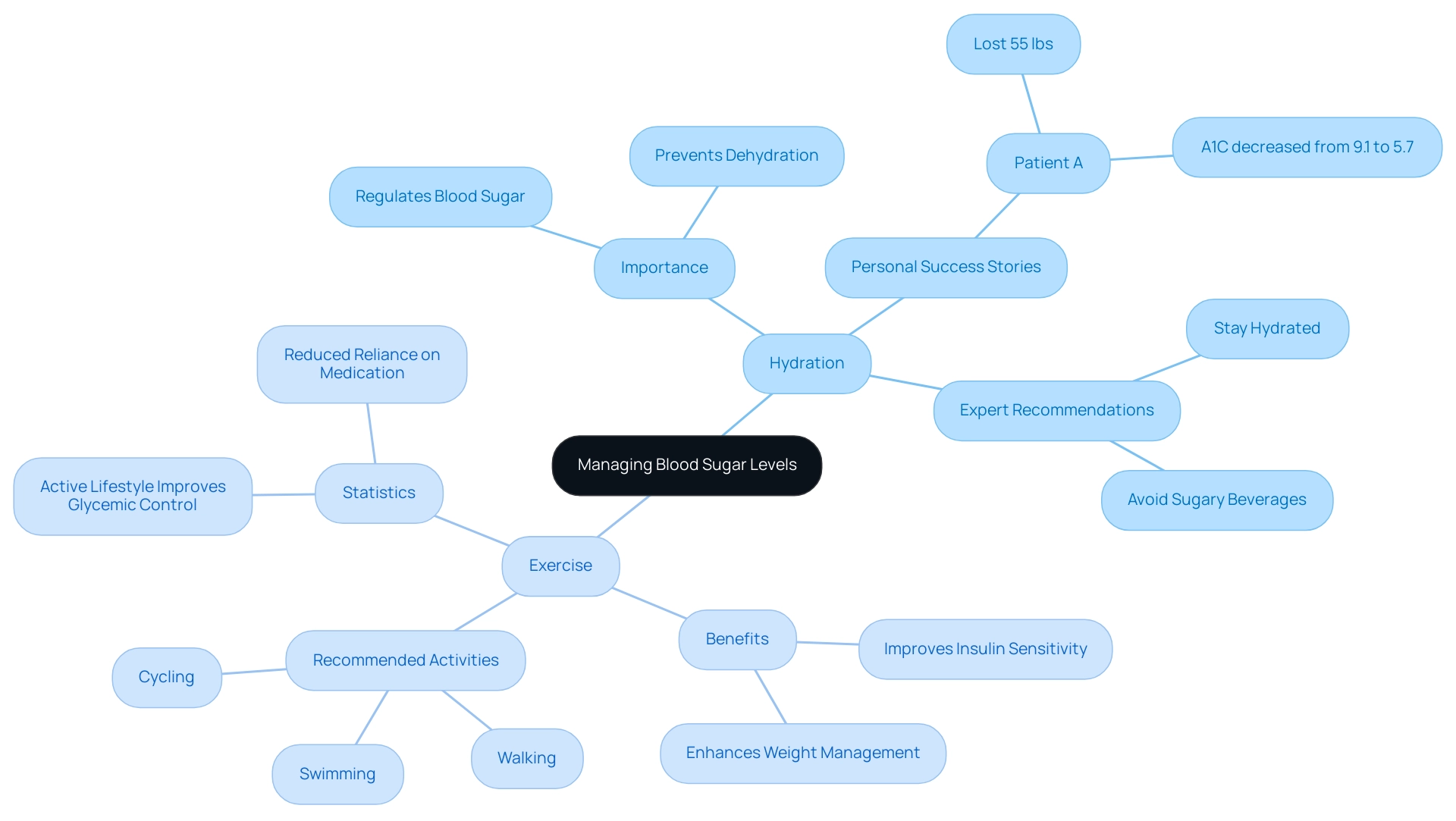
Incorporating Hydration and Exercise into Your Diabetic Diet
Hydration is truly a cornerstone of effectively managing blood sugar levels. It plays a vital role in regulating these levels and promoting your overall well-being. If you’re someone dealing with high blood sugar, it’s essential to prioritize drinking plenty of water throughout the day while avoiding sugary beverages that can lead to those frustrating spikes in blood glucose. Remember, sufficient hydration not only supports your metabolic processes but also helps prevent dehydration—a state that can complicate blood sugar management and lead to further challenges.
Transformative experiences from Dr. Jason Shumard’s 30-Day Diabetes Reset program illustrate this beautifully. Many individuals who commit to proper hydration report significant improvements in their overall health. For instance, one patient shared, ‘I lost 55 lbs and my A1C decreased from 9.1 to 5.7 after beginning this program.’ This highlights just how impactful hydration can be when combined with the program’s guidelines.
In addition to staying hydrated, consistent physical exercise is crucial for managing your condition effectively. Engaging in at least 150 minutes of moderate-intensity exercise each week can enhance your insulin sensitivity and assist in weight management. Activities like walking, swimming, and cycling are not only beneficial but can also be easily integrated into your daily routine, making them accessible for most individuals.
Many patients have shared how regular exercise has transformed their lives. One participant expressed, ‘I feel so much better, have more energy, and I’m not depressed anymore.’ This underscores the positive effect that a structured exercise regimen can have on managing blood sugar levels.
Recent studies reveal the significant influence of exercise on blood sugar management. Those who maintain an active lifestyle often experience improved glycemic control and a reduced reliance on medication. Success stories from patients in structured exercise programs further highlight the transformative effects of physical activity. As one patient noted, ‘I feel so much better, have more energy, and I’m not depressed anymore.’
Experts emphasize the importance of hydration in managing blood sugar levels, noting that staying well-hydrated can lead to better metabolic outcomes. Statistics suggest that individuals who maintain proper hydration levels are less likely to face issues related to blood sugar conditions, reinforcing the necessity for consistent water consumption as part of a comprehensive management strategy. It’s crucial to note that starting doses greater than 0.6 – 0.8 units/kg/day have been associated with three-fold higher odds of hypoglycemia than doses lower than 0.2 U/kg/day, highlighting the critical role of hydration and exercise in managing your condition effectively.
Dr. Jason Shumard states, ‘By providing patients with actionable insights and practical tools, the center cultivates an environment where people can reclaim their wellness and well-being.’ This commitment to patient empowerment is further illustrated by the case study of Dr. Shumard’s Functional Medicine Approach, where patients report life-changing outcomes and express gratitude for the empowerment they feel in taking control of their health.
Additionally, maintaining target glucose levels between 140 and 180 mg/dl in non-ICU settings is essential, and proper hydration and exercise contribute significantly to achieving these goals. Recent recommendations regarding the management of metabolic dysfunction-associated liver diseases (MASLD and MASH) in adults with type 2 conditions also emphasize the importance of an interprofessional team approach, further underscoring the need for comprehensive strategies in managing this health issue.
By combining hydration with regular exercise, you can take proactive steps toward reclaiming your health and improving your quality of life.
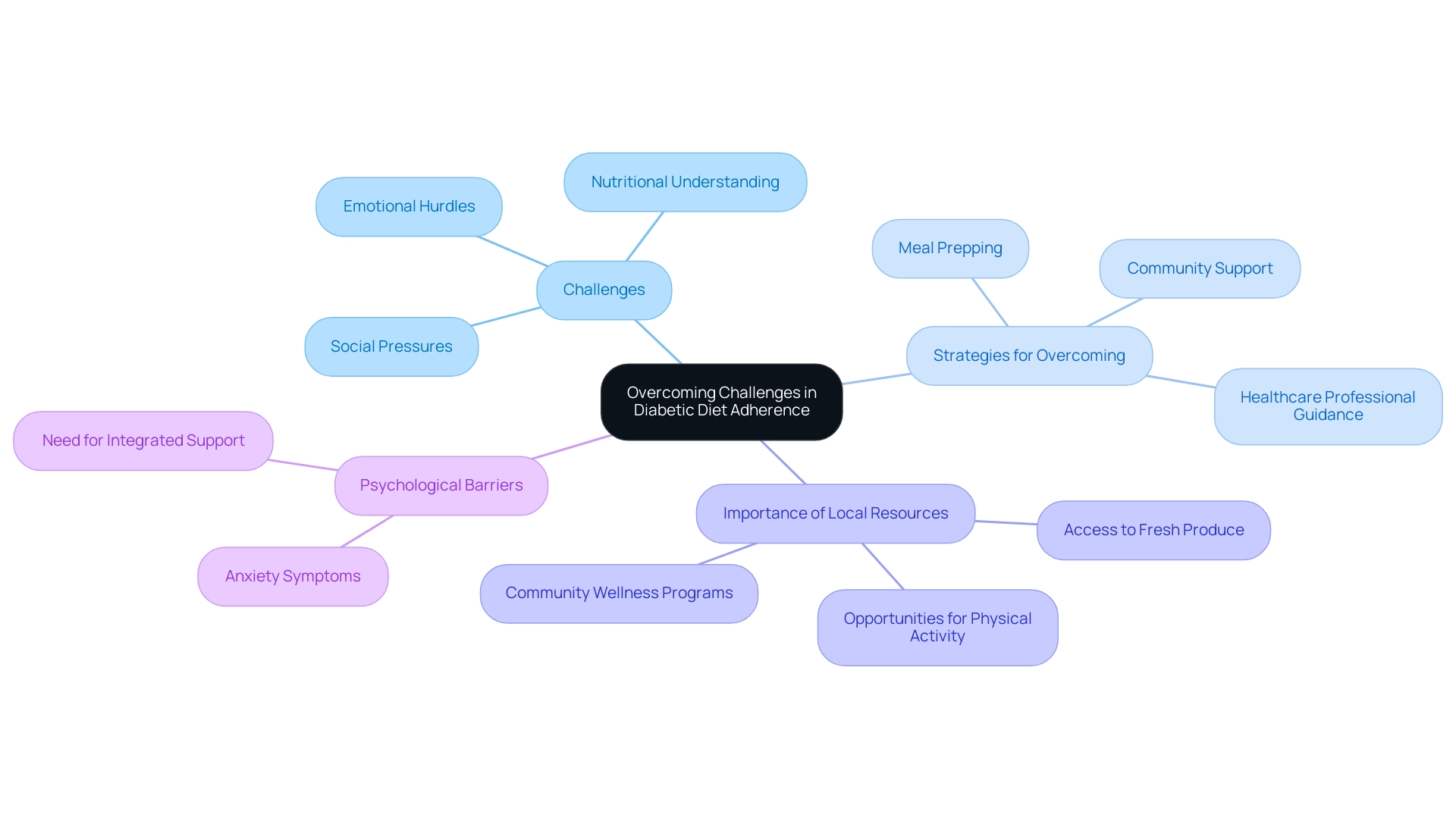
Overcoming Challenges in Diabetic Diet Adherence
Navigating a diabetic diet can present numerous challenges, including social pressures, a lack of nutritional understanding, and emotional hurdles that may hinder effective management of type 2 diabetes. It’s important to recognize that by 2030, over 10.2% of the population in certain regions will be affected by this condition, highlighting the urgent need to address dietary adherence issues. To help overcome these obstacles, setting realistic, achievable goals and actively seeking support from healthcare professionals or support groups can be incredibly beneficial for individuals managing blood sugar levels.
In San Marcos, CA, embracing the local lifestyle can significantly enhance diabetes management. Many patients find that living in an area rich with parks and trails provides ample opportunities for regular physical activity, which is crucial for improving insulin sensitivity and controlling blood sugar levels. Moreover, the vibrant farmers’ markets offer access to fresh, local produce, making it easier to incorporate nutrient-dense foods into daily meals. Meal prepping emerges as a powerful strategy to alleviate the daily stress of cooking and reinforce adherence to dietary plans.
By preparing dishes in advance, individuals can ensure they have healthy choices readily available, reducing the temptation to stray from their dietary guidelines. Additionally, creating a supportive home environment—such as involving family members in meal planning and preparation—can significantly enhance adherence to a diabetic diet. Community wellness programs in San Marcos can also provide invaluable support for managing blood sugar levels, offering education and resources tailored to local needs.
Understanding that setbacks are a natural part of the journey is crucial. Having a proactive plan to address these setbacks can empower individuals to stay on track. For instance, a systematic review has highlighted that psychosocial interventions can lead to modest but significant improvements in A1C levels and overall behavioral well-being outcomes, emphasizing the importance of integrated support in managing blood sugar conditions.
Success stories abound, with many individuals sharing that food prepping not only simplifies their daily routines but also fosters a sense of control over their health. Patients at the Integrative Wellness Center have successfully eliminated their dependency on insulin and improved their blood sugar management, illustrating the center’s transformative approach to diabetes care.
Moreover, addressing psychological barriers is essential, as case studies show that anxiety symptoms can interfere with self-management behaviors. In light of these insights, it is clear that overcoming barriers to adherence to a diabetic diet requires a multifaceted approach, combining education, community support, and practical strategies like meal prepping.
By customizing nutrition interventions to personal situations and tackling these challenges directly, individuals can regain their well-being and enhance their quality of life. The Integrative Wellness Center provides tailored support from Dr. Jason Shumard, assisting patients in managing their condition and reaching their wellness objectives.
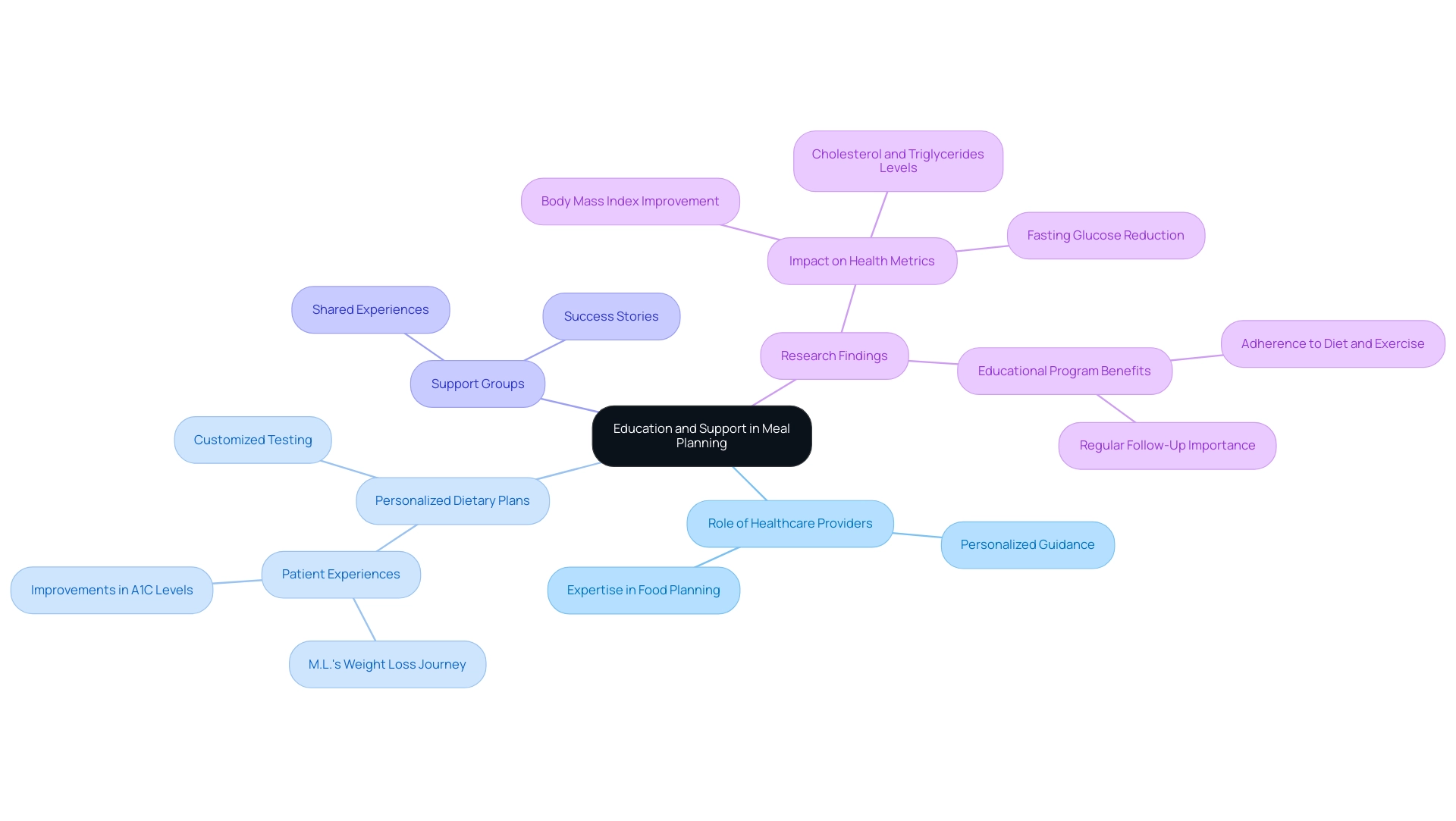
The Role of Education and Support in Successful Meal Planning
Education and support are crucial foundations for effective food planning, especially for those managing diabetes. It’s important to recognize that ongoing education about nutrition, meal planning methods, and the impact of food selections on blood sugar levels can empower individuals to take control of their well-being. Studies show that 27.6% of patients who combined antidiabetic medications with appropriate dietary practices experienced better health outcomes, highlighting how education directly contributes to these improvements.
Healthcare providers, dietitians, and diabetes educators play a vital role in offering personalized guidance and resources tailored to individual needs. Their expertise can assist patients in navigating the complexities of food planning, ensuring that dietary choices align with their health goals. The transformative experiences of patients in Dr. Jason Shumard’s 30-Day Diabetes Reset program showcase the effectiveness of such personalized care.
For instance, one participant, M.L., shared their journey of significant weight loss and improvements in A1C levels, illustrating the potential of customized dietary planning and education. Furthermore, the program includes detailed testing that goes beyond typical lab work, allowing for a personalized plan specifically designed for each participant. This holistic approach not only targets the contributing factors of diabetes but also aims to reduce dependency on insulin and other diabetes-related medications.
Participating in support groups or community initiatives nurtures a sense of connection and motivation, making it easier to stick to dietary plans and achieve wellness goals. Success stories from these support groups highlight the transformative impact of shared experiences and collective motivation, as individuals exchange practical tips and strategies for effective meal planning. As Dr. Shumard emphasizes, “What sets my program apart is its holistic approach to health, focusing on personalized care and education rather than just symptom management.”
Additionally, a recent study discovered that nutrition and lifestyle education significantly improved patients‘ body mass index, fasting glucose, triglycerides, and cholesterol levels. This reinforces the critical role of education in managing diabetes. The study concluded that educational programs emphasizing adherence to diet, exercise, and regular follow-up are more beneficial than medication compliance alone.
In summary, integrating education and support systems is vital for effective diabetes management. By prioritizing these elements, along with customized plans and detailed testing, individuals can enhance their meal planning efforts, leading to better health outcomes and a more empowered approach to managing their condition.
Conclusion
Effective meal planning is a cornerstone of successful diabetes management. It serves as a powerful tool that empowers individuals to take control of their dietary choices and maintain stable blood sugar levels. By incorporating strategies such as carbohydrate counting, portion control, and the inclusion of healthy fats, individuals can create balanced meal plans that not only support their health but also enhance their quality of life.
It’s important to recognize that evidence from various dietary patterns, including the Mediterranean and low-carbohydrate diets, highlights the significance of personalized nutrition. Tailored dietary approaches can lead to significant improvements in glycemic control and overall well-being.
Moreover, the role of education and support cannot be overstated. Access to resources like meal planning templates, food lists, and community support fosters an environment where individuals feel equipped to manage their diabetes effectively. Many patients find that structured meal planning and education have a transformative impact on their lives, with testimonials reporting significant health improvements and a reduced reliance on medication.
As we look to the future of diabetes care, it is clear that a multifaceted approach is essential. Combining effective meal planning with continuous education and community support fosters sustainable lifestyle changes. By embracing these practices, individuals not only improve their health outcomes but also reclaim their sense of agency in managing their diabetes. The journey towards better health is a collaborative effort—remember, with the right tools and support, a healthier future is within reach for those living with diabetes.