Overview
The Glucose Management Indicator (GMI) serves as a vital tool for those navigating the challenges of diabetes management. It estimates an individual’s average hemoglobin A1c (HbA1c) level by utilizing data from continuous glucose monitoring (CGM) over a minimum of 14 days.
It’s important to recognize that GMI offers a more immediate reflection of blood sugar control compared to traditional A1c tests. This timely insight empowers patients to make informed health decisions, ultimately enhancing their overall diabetes management and health outcomes.
Many patients find that this proactive approach significantly improves their quality of life.
Introduction
In the realm of diabetes management, many individuals face daily challenges that can feel overwhelming. It’s important to recognize that the Glucose Management Indicator (GMI) emerges as a groundbreaking tool, transforming how you can monitor your health. Unlike traditional methods, GMI leverages continuous glucose monitoring (CGM) data to provide a real-time snapshot of your glucose levels. This empowers you to make informed decisions about your lifestyle and treatment plans.
Many patients find that this innovative metric not only enhances their understanding of glucose control but also fosters a proactive approach to managing diabetes, especially for those navigating the complexities of type 2 diabetes. As you strive for better health outcomes, integrating GMI into personalized care models signifies a shift towards more dynamic and responsive diabetes management strategies. Through actionable insights and tailored treatment plans, GMI helps you reclaim your health and improve your quality of life. Imagine feeling more in control and supported on your journey to wellness.
Defining the Glucose Management Indicator (GMI)
The Glucose Management Indicator (GMI) is a groundbreaking measure that helps answer the question of what GMI is by estimating a person’s average hemoglobin A1c (HbA1c) level through continuous monitoring (CGM) data. Specifically, GMI works by determining the anticipated A1c level based on average sugar levels recorded over a minimum period of 14 days. For those managing type 2 diabetes, especially under the personalized care model at Dr. Jason Shumard’s Integrative Wellness Center, this metric is invaluable. It provides a more immediate reflection of blood control compared to traditional HbA1c tests, which evaluate sugar levels over a three-month timeframe.
Calculating GMI is straightforward, represented by the formula:
GMI (%) = 3.31 + 0.02392 × (mean sugar in mg/dL).
This approach allows patients to gain a dynamic perspective on their glucose levels, empowering them to make informed decisions about their health management. It’s crucial to recognize that recent studies emphasize the significance of GMI and its correlation with glycemic control, further enhancing this tool’s importance in managing blood sugar levels.
Many patients find that a recent study demonstrated a significant improvement in mean EGV from 205 mg/dL to 172 mg/dL (< 0.001), highlighting the effectiveness of CGMs in managing blood sugar. Dr. Jason Shumard emphasizes, ‘By providing individuals with actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being.’ The center’s approach also includes comprehensive assessments and diagnostic tests that identify individual factors contributing to the condition. This allows for tailored treatment plans that address not just symptoms but also root causes.
Furthermore, a case study on the effectiveness of continuous blood sugar monitors supports the use of GMI. It suggests that increased accessibility and prescription of CGMs could lead to better health outcomes for patients with type 2 conditions. This exemplifies the holistic and personalized treatment strategies central to reversing type 2 conditions. Remember, you are not alone on this journey—support is available to help you thrive.
How to Calculate the Glucose Management Indicator
Understanding what GMI is can feel overwhelming, but it’s essential for effective diabetes management. At its core, the Management Indicator (GMI) is calculated using data from continuous monitoring devices that track sugar levels in real-time. To accurately grasp what GMI entails, patients should begin by gathering their average sugar readings over a minimum of 14 days. The formula for determining GMI is straightforward:
GMI (%) = 3.31 + 0.02392 × (average sugar in mg/dL).
For instance, if an individual’s average blood sugar level is recorded at 150 mg/dL, their GMI would be approximately 6.9%. This calculation is vital as it provides a more immediate perspective on sugar management, especially when compared to traditional A1c tests. Understanding GMI allows for timely adjustments to management strategies, empowering patients to respond effectively to their blood sugar levels.
With advancements in CGM technology and its growing adoption—82.2% of individuals using CGM in endocrinology are on both basal and prandial insulin—grasping and applying GMI becomes increasingly important for those managing type 2 conditions in 2025. As noted by Author Mayberry, automated interpretation of CGM data is crucial for alerting users to specific patterns and recommending necessary therapy changes. This raises an important question: what role does GMI play in effectively managing diabetes?
Incorporating holistic lifestyle strategies can further enhance glucose control. For example, regular outdoor exercise in the beautiful parks of San Marcos and maintaining a balanced diet rich in local produce can make a significant difference. Patients can utilize various tracking methods, such as fitness apps, journals, and pedometers, to monitor their progress effectively. A SMART goal might be to achieve an average GMI of less than 7% within three months by increasing physical activity and adjusting dietary habits.
Engaging with community wellness programs offers additional support, fostering accountability and motivation. These programs often provide valuable resources for establishing and monitoring health goals, ensuring individuals stay focused on their objectives. By prioritizing these strategies alongside understanding GMI monitoring, individuals can achieve more effective diabetes management, ultimately leading to improved health outcomes and a better quality of life.
GMI vs. A1C: Understanding the Differences
Both the Glucose Management Indicator (GMI) and hemoglobin A1c (A1C) are essential metrics for assessing sugar management. Understanding what GMI is crucial, as each differs in methodologies and implications for healthcare. While A1C measures glycated hemoglobin to indicate average blood sugar levels over a three-month period, GMI relates to data derived from continuous monitoring (CGM), providing a real-time snapshot of sugar levels. One notable benefit of GMI is its responsiveness; it can swiftly reflect changes in sugar management, facilitating timely interventions that improve health outcomes.
For instance, a recent study showed participants improved their GMI from 8.2% to 7.4% over six months. This raises the question of GMI’s effectiveness in tracking progress. Dr. Jason Shumard’s holistic approach emphasizes that by offering individuals actionable insights, the center fosters an environment where they can reclaim their health and well-being. This ultimately enhances their quality of life while reducing dependence on conventional medical interventions. Understanding what GMI enables individuals to monitor their sugar trends in real-time, resulting in informed choices regarding their health.
However, discrepancies can arise between A1C results and GMI due to factors like red blood cell turnover and individual variations in glucose metabolism. This underscores the need for a comprehensive approach that considers both indicators in managing blood sugar levels. Personalized functional medicine approaches are essential in this context, as demonstrated by testimonials reflecting transformative health journeys at Dr. Shumard’s center. One individual remarked, ‘Thanks to Dr. Shumard’s guidance, I have taken control of my diabetes and feel healthier than ever.’
Furthermore, statistics reveal that in hospitals, 7,000 incorrect medications are administered to individuals, and 80,000 infections are acquired annually. These alarming figures emphasize the critical need for personalized care that Dr. Shumard offers, contrasting sharply with conventional treatments that can often overlook individual needs. Additionally, POCT-HbA1c is recommended for rapid results, enhancing glucose management.
The case study on customized management plans for blood sugar control demonstrates the importance of understanding GMI along with laboratory A1C values. This understanding helps create individualized strategies that prioritize individual safety and effective management.
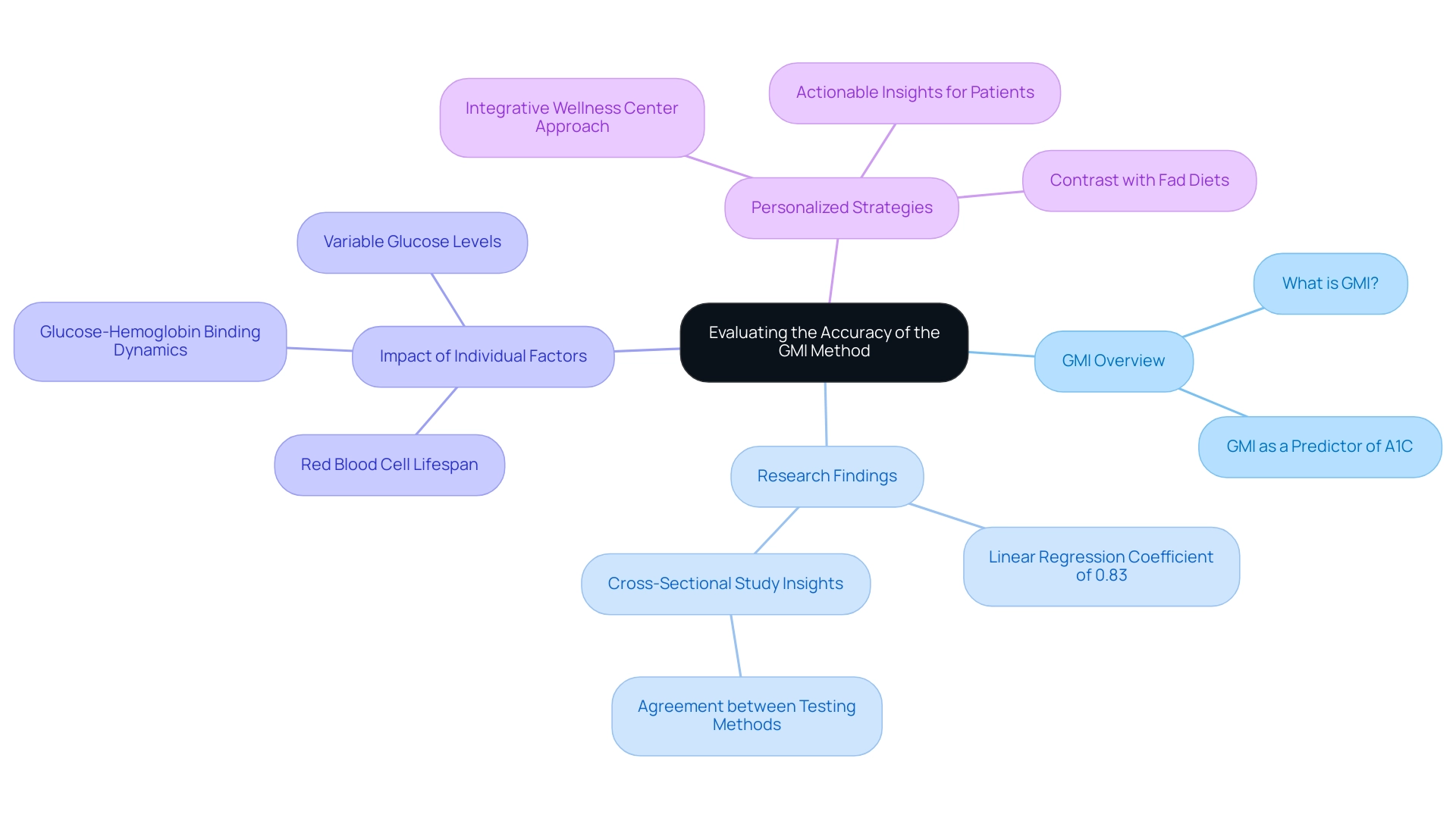
Evaluating the Accuracy of the GMI Method
The accuracy of the Glucose Management Indicator (GMI) has garnered significant attention within the healthcare community as an emerging tool for diabetes management. Many patients find themselves asking, ‘What is GMI?’ Recent research explores this question, revealing how GMI can consistently assess A1C levels for numerous individuals, particularly those using continuous monitoring systems. A univariate linear regression analysis has shown a significant linear relationship between Lab-HbA1c and POCT-HbA1c in the conventional SMBG group, with a coefficient of 0.83. This provides a quantitative basis for GMI’s reliability.
It’s important to recognize that while GMI serves as a solid predictor of A1C, individual factors—such as red blood cell lifespan and the dynamics of glucose-hemoglobin binding—can substantially impact the correlation with A1C measurements. Discrepancies may occur, particularly among individuals experiencing variable glucose levels or those with specific medical conditions. Insights from a cross-sectional study conducted at the Diabetes Treatment Center in Riyadh further illustrate this point, assessing the agreement between point-of-care testing for HbA1c and standard laboratory measurements among individuals with diabetes.
As Dr. Jason Shumard aptly states, ‘By providing individuals with actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being.’ This highlights the significance of understanding what GMI is as a component of a thorough management strategy that incorporates personalized functional medicine methods customized to individual health profiles. Such an integrated approach not only considers GMI alongside other assessment methods but also includes state-of-the-art testing techniques to identify each patient’s unique dietary and lifestyle needs.
By contrasting these personalized strategies with the often ineffective fad diets available online, the Integrative Wellness Center emphasizes the necessity of individualized care in managing diabetes effectively. Remember, your journey to better health is unique, and having the right support can make all the difference.
Target GMI Ranges: What Patients Should Aim For
Effective management of blood sugar begins with understanding the Glucose Management Indicator (GMI), a crucial tool that aligns with your personal health objectives and medical advice. It’s important to recognize that a GMI value below 5.7% is considered normal, while levels between 5.7% and 6.4% indicate prediabetes. If your GMI reaches 6.5% or higher, it signifies diabetes. Given the concerning statistics about hospital safety—such as 7,000 incorrect medications and 80,000 infections—it’s essential to collaborate closely with your healthcare provider to create personalized target ranges tailored to your unique situation, which may include factors like age, duration of the condition, and overall health status.
Understanding what GMI means can significantly aid in achieving and maintaining target levels, thereby reducing the risk of diabetes-related complications. Many patients find that time in range is linked to a lower chance of developing serious health issues. Dr. Jason Shumard emphasizes that by equipping individuals with actionable insights and practical tools, our center fosters an environment where you can reclaim your health and well-being. This journey ultimately leads to an enhanced quality of life and less dependence on conventional medical interventions. Our holistic health solutions, including tailored nutrition and comprehensive testing, are designed to support your diabetes management effectively.
To establish personalized targets, consider engaging in open discussions with your healthcare provider about what GMI means in relation to your specific health conditions and goals. This collaborative approach not only deepens your understanding but also empowers you to take charge of your health journey. Reach out to us today at (858) 564-7081 or visit DrShumard.com to discover how our holistic health solutions can assist in managing your condition.
Our clinic is located at 7094 Miramar Road, Suite 109, San Diego, CA 92121. We look forward to helping you achieve your health goals!
Empowering Patients: The Role of GMI in Diabetes Management
The Glucose Management Indicator (GMI) is an essential tool that empowers individuals managing their diabetes by providing actionable insights into glucose regulation. It’s important to recognize that understanding what GMI is enables individuals to make informed decisions about their diet, exercise routines, and medication adherence. This knowledge is crucial in overcoming the challenges of type 2 diabetes. By cultivating a sense of ownership over their health, patients can engage proactively in their management, especially considering the risks associated with elevated insulin levels and traditional treatment methods.
Many patients find that GMI enhances communication with their healthcare providers, facilitating constructive discussions that lead to collaborative goal-setting and personalized treatment strategies tailored to their unique needs. As individuals deepen their understanding of their sugar levels and what GMI entails, they often feel more equipped to navigate the complexities of managing their condition, moving away from a one-size-fits-all approach. Notably, the use of continuous glucose monitoring (CGM) has surged, increasing from 7% in 2010-2012 to 30% in 2016-2018. This reflects a growing acceptance of glucose management tools in the journey of managing blood sugar conditions.
This empowerment not only contributes to improved health outcomes but also enhances overall quality of life. It exemplifies the transformative impact of informed engagement in health management. As Dr. Jason Shumard beautifully states, ‘By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being, ultimately leading to improved quality of life and reduced reliance on conventional medical interventions.’ Patients like Jane Doe share their success stories, expressing, ‘Thanks to the Integrative Wellness Center, I finally understand my condition and feel empowered to manage it effectively.’
Additionally, measuring blood pressure and body mass index (BMI) are key components in assessing overall health status, further influencing effective management of diabetes. By embracing a holistic approach, patients can significantly alter their diabetes journey, utilizing innovative processes such as personalized nutrition plans and lifestyle coaching offered by the center. Remember, taking these steps can lead to a healthier, more fulfilling life.
Conclusion
The Glucose Management Indicator (GMI) represents a significant advancement in diabetes management, offering a real-time perspective on glucose levels that surpasses traditional methods like A1C testing. It’s important to recognize that managing diabetes can often feel overwhelming, but GMI utilizes continuous glucose monitoring (CGM) data to empower individuals. By tracking average glucose levels over a minimum of 14 days, patients can make informed decisions about their health, fostering a proactive approach to managing type 2 diabetes. This innovative metric not only enhances understanding of glucose control but also aligns with personalized care models that prioritize individual needs.
Many patients find that as they engage with GMI, they can set targeted goals and collaborate closely with healthcare providers to tailor their management strategies. The ability to observe glucose trends dynamically facilitates timely interventions, ultimately improving health outcomes and quality of life. The evidence supporting GMI’s effectiveness, highlighted in various studies and patient testimonials, underscores its role in promoting a more responsive and personalized approach to diabetes care.
In conclusion, integrating GMI into diabetes management is not just about tracking numbers; it’s about reclaiming health and enhancing well-being. By prioritizing personalized strategies that include GMI monitoring, individuals with diabetes can navigate their health journeys with greater confidence and support. The shift towards a comprehensive understanding of glucose management heralds a new era in diabetes care, where patients are empowered to take control of their health and improve their overall quality of life.
Frequently Asked Questions
What is the Glucose Management Indicator (GMI)?
The Glucose Management Indicator (GMI) is a measure that estimates a person’s average hemoglobin A1c (HbA1c) level using continuous glucose monitoring (CGM) data, providing a more immediate reflection of blood sugar control compared to traditional HbA1c tests.
How is GMI calculated?
GMI is calculated using the formula: GMI (%) = 3.31 + 0.02392 × (mean sugar in mg/dL). This requires gathering average sugar readings over a minimum period of 14 days.
Why is GMI important for managing type 2 diabetes?
GMI is important as it allows patients to gain a dynamic perspective on their glucose levels, enabling them to make informed decisions about their health management and adjust their strategies in a timely manner.
How does GMI compare to traditional HbA1c tests?
Unlike traditional HbA1c tests that evaluate sugar levels over a three-month period, GMI provides a more immediate reflection of blood sugar control based on recent data from continuous monitoring.
What recent findings support the effectiveness of continuous glucose monitors (CGMs)?
Recent studies have shown significant improvements in mean glucose values, indicating the effectiveness of CGMs in managing blood sugar levels, with a notable reduction from 205 mg/dL to 172 mg/dL.
How does Dr. Jason Shumard’s Integrative Wellness Center utilize GMI?
The center uses GMI as part of a personalized care model that includes comprehensive assessments and tailored treatment plans to address individual factors contributing to type 2 diabetes, focusing on both symptoms and root causes.
What role does lifestyle play in managing glucose levels?
Incorporating holistic lifestyle strategies, such as regular exercise and maintaining a balanced diet, can enhance glucose control and improve overall health outcomes for individuals managing diabetes.
How can patients track their progress in managing diabetes?
Patients can utilize various tracking methods, including fitness apps, journals, and pedometers, to monitor their progress and set health goals, like achieving a GMI of less than 7% within three months.
What support options are available for individuals managing diabetes?
Engaging with community wellness programs can provide additional support, resources, and motivation, helping individuals stay focused on their health objectives and enhancing accountability in their diabetes management journey.