Overview
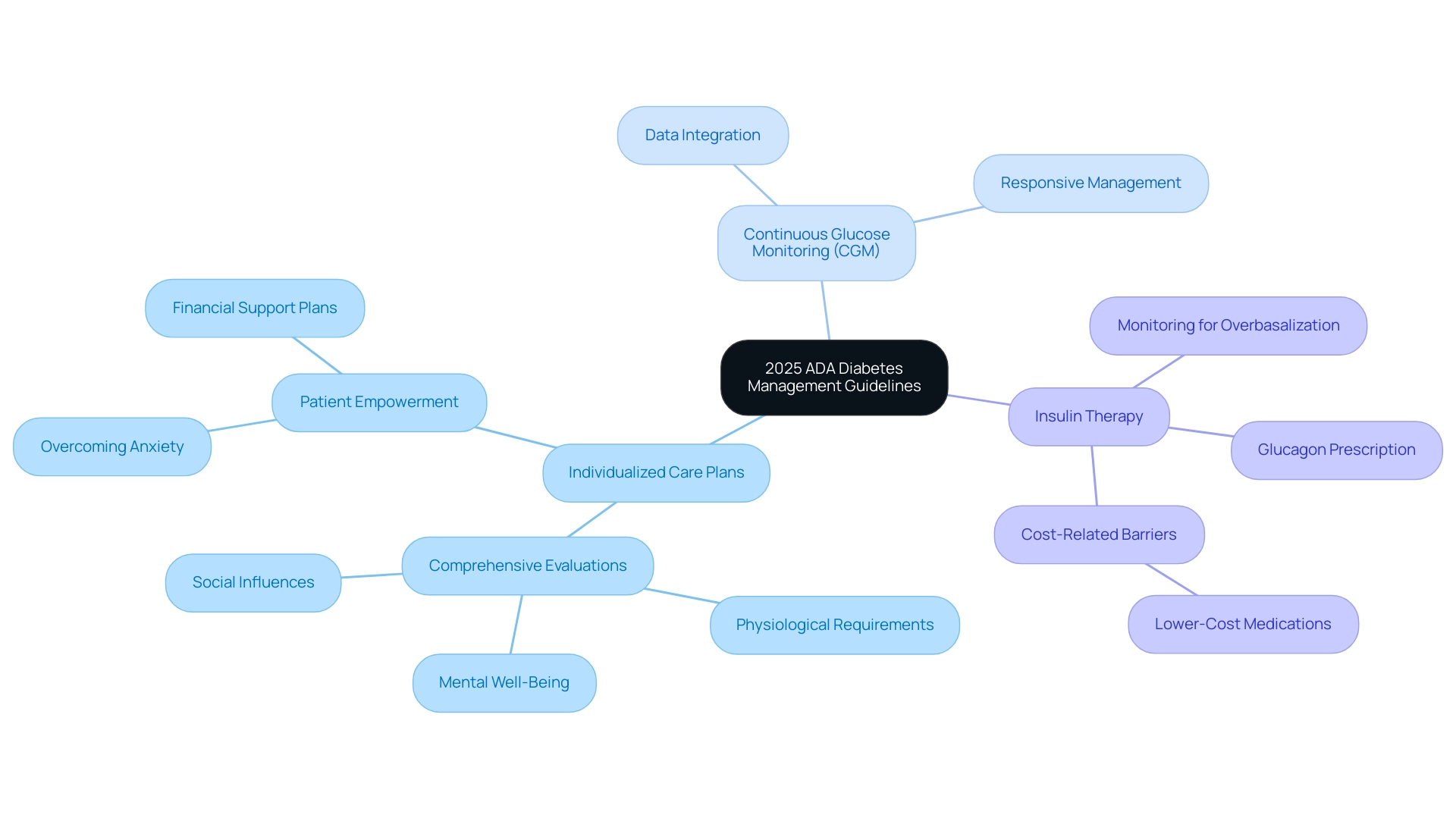
The 2025 ADA Diabetes Management (DM) Guidelines introduce significant updates aimed at enhancing individualized care, emphasizing comprehensive evaluations that include physiological, mental, and social factors. These revisions, which integrate advanced technologies like continuous glucose monitoring and highlight the importance of nutrition and behavioral health, are designed to improve patient engagement and health outcomes by addressing the unique challenges faced by individuals with diabetes.
Introduction
The 2025 American Diabetes Association (ADA) Diabetes Management Guidelines mark a significant evolution in the approach to diabetes care, emphasizing the necessity of personalized treatment plans that consider the unique needs of each patient.
With a focus on integrating comprehensive assessments that include mental health and social determinants, these guidelines aim to enhance patient engagement and improve health outcomes.
Key innovations include:
- Continuous glucose monitoring
- Advanced insulin delivery systems
These are highlighted alongside essential lifestyle strategies that address:
- Nutrition
- Exercise
- Stress management
As healthcare providers adapt to these changes, the importance of a holistic approach becomes increasingly clear, paving the way for a future where diabetes management is both effective and equitable.
Major Revisions in the 2025 ADA Diabetes Management Guidelines
The 2025 ADA DM guideline introduces pivotal revisions grounded in the latest research and clinical practices, particularly emphasizing the need for individualized care plans. Acknowledging that management of this condition is inherently distinct for each individual, the ADA DM guideline promotes comprehensive evaluations that include not only physiological requirements but also mental well-being factors and social influences. Notably, the 2024 Standards of Care, which span 42 pages, provide a comprehensive framework for the ADA DM guideline.
A significant enhancement includes the integration of continuous glucose monitoring (CGM) data into clinical decision-making, facilitating more accurate and responsive management of blood glucose levels. By prioritizing these comprehensive approaches, the revisions aim to encourage greater involvement of individuals and significantly enhance health results for those living with type 2. As shown in transformative success stories like M.L.’s, who lost 55 lbs and significantly improved their A1C level from 9.1 to 5.7, the emphasis on comprehensive treatment and personalized attention at the Integrative Wellness Center empowers patients to overcome anxiety about complications and eliminate worries associated with their condition. The program also considers financial obstacles, ensuring that personalized support plans are both effective and accessible. As Charles ‘Chuck’ Henderson, the ADA’s chief executive officer, states, “Enhancing the lives of individuals impacted by this condition is a key part of the ADA’s mission,” which underscores the significance of the ADA DM guideline in managing this chronic issue.
Furthermore, recommendations for insulin therapy highlight the significance of monitoring for signs of overbasalization, ensuring that personalized treatment plans are both effective and accessible.
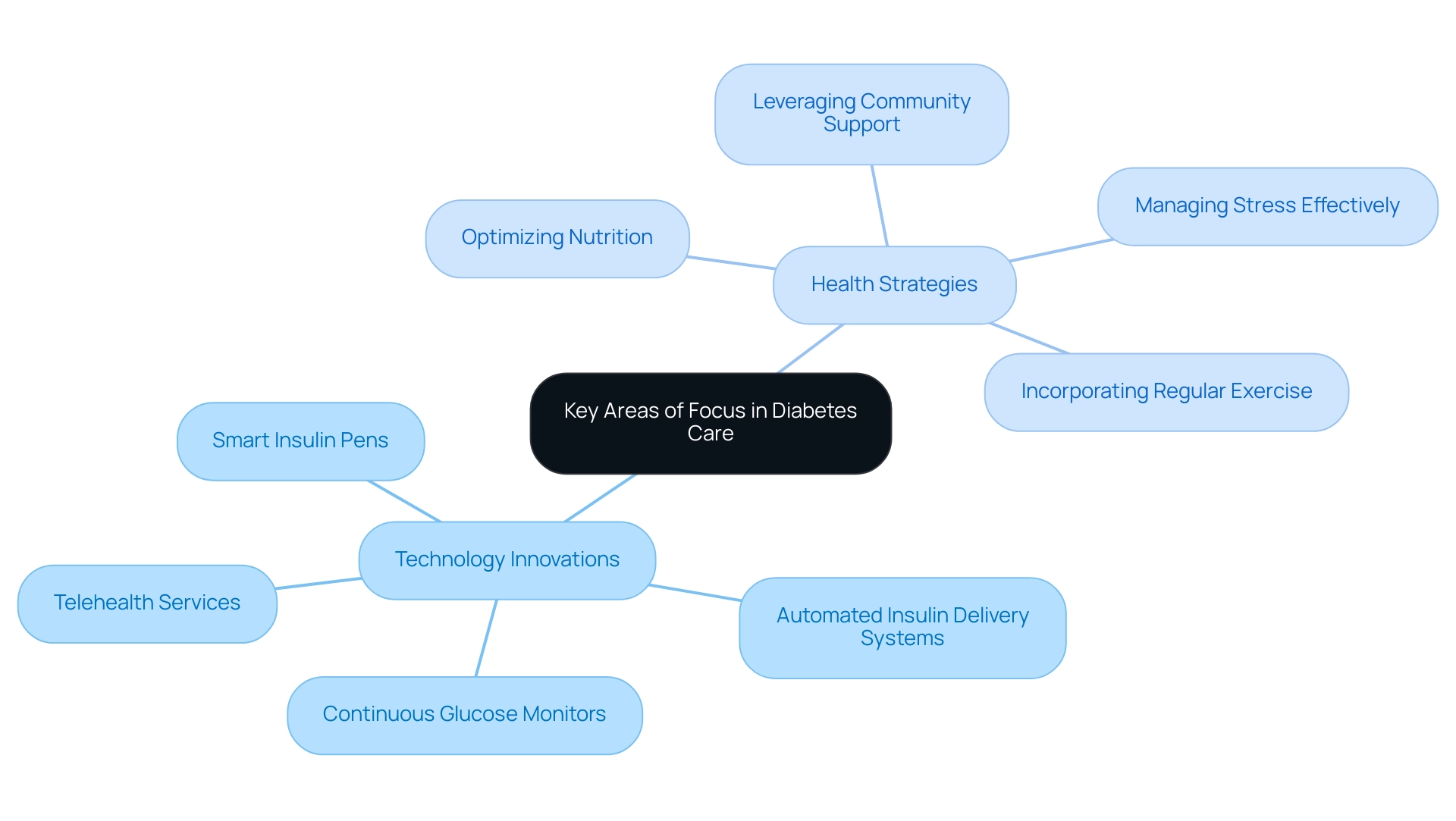
Key Areas of Focus: Technology and Treatment Innovations in Diabetes Care
Recent updates to the ada dm guideline emphasize the essential role of technology in improving care for individuals. Notable innovations such as smart insulin pens, automated insulin delivery systems, and advanced continuous glucose monitors are now recognized as essential tools in achieving optimal glycemic control. However, to truly reverse the condition and improve health, it’s vital to consider four lesser-known power-plays:
- Optimizing nutrition
- Incorporating regular exercise
- Managing stress effectively
- Leveraging community support
Healthcare providers are encouraged to familiarize themselves with these technologies while also emphasizing the importance of these strategies in their practice. Furthermore, the integration of telehealth services has emerged as a significant resource for individuals, particularly those in remote locations or facing mobility challenges. This trend not only improves accessibility to healthcare but also allows individuals to actively participate in managing their condition.
With the market for AI health technologies projected to grow significantly, the necessity for effective management solutions becomes increasingly evident. According to the case study titled ‘Future of AI in Diabetes Care,’ this market is expected to expand, highlighting the urgency of incorporating innovative solutions. Specialists in glucose management highlight the significance of reducing entry obstacles and showcasing evident advantages; as Interviewee 9 mentioned, ‘what’s in it for me (healthcare provider) and also illustrate the additional value for the support team and individuals.’
Additionally, understanding the dynamics of value creation in ecosystems is crucial, particularly the distinction between open networks that prioritize overall value and closed networks that emphasize individual actor value. As we approach 2025, the effective execution of these technological innovations, coupled with an emphasis on nutrition, physical activity, stress reduction, and community wellness programs, will be crucial in transforming health management and aiding patients in areas such as San Marcos. Don’t forget to sign up for more insights on how to enhance your health and reverse the condition!
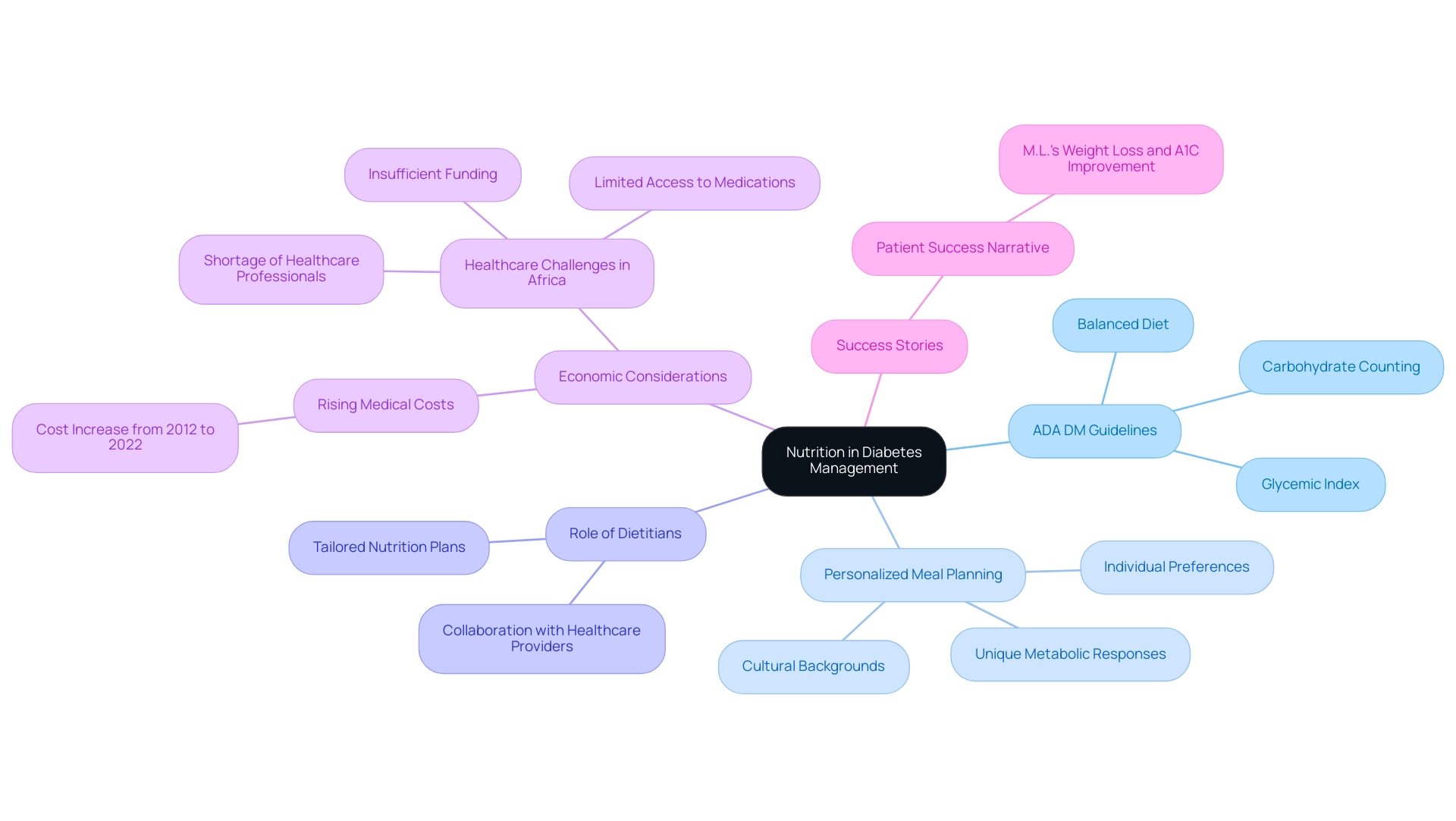
The Role of Nutrition in Diabetes Management
The 2025 ADA DM guideline emphasizes nutrition as a cornerstone of effective diabetes care, advocating for a balanced diet rich in whole foods—fruits, vegetables, whole grains, and lean proteins. These guidelines emphasize the importance of personalized meal planning that adheres to the ADA DM guideline, taking into account individual preferences, cultural backgrounds, and unique metabolic responses. Carbohydrate counting and understanding the glycemic index are essential practices outlined in the ADA DM guideline that enable individuals to make informed dietary choices conducive to stabilizing blood sugar levels.
To maximize the success of these dietary strategies, healthcare providers are encouraged to collaborate with registered dietitians in crafting tailored nutrition plans that adhere to the ADA DM guideline and address each patient’s specific needs. Financially, the burden of managing this condition is substantial, with medical costs per person rising from $10,179 to $12,022 between 2012 and 2022, underscoring the critical need for effective dietary management to alleviate some of these costs. Patient success narratives, such as that of M.L., who lost 55 lbs and greatly enhanced their A1C from 9.1 to 5.7 through personalized support at the Integrative Wellness Center, illustrate the transformative potential of this integrative approach.
M.L. experienced reduced medication needs and better overall health, showcasing how holistic care can alleviate anxiety over complications related to blood sugar management. This program not only addresses the physical aspects of managing the condition but also offers support that helps alleviate anxiety related to it.
These insights are particularly relevant in areas experiencing healthcare difficulties, where personalized nutrition plays a crucial role in comprehensive management.
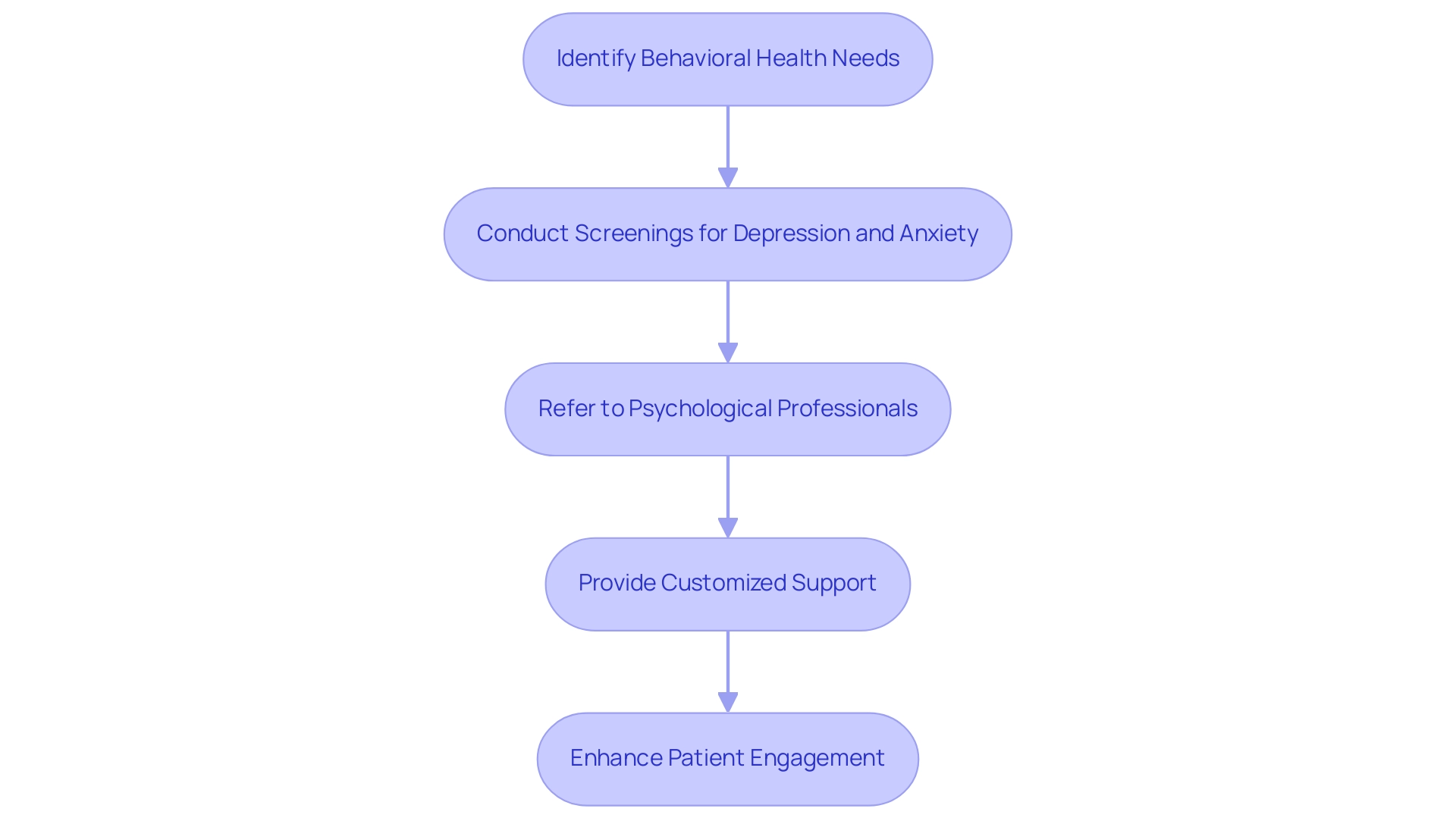
Incorporating Behavioral Health into Diabetes Care
The 2025 ADA DM guideline emphasizes the crucial significance of behavioral wellness in managing the condition, promoting regular screenings for depression and anxiety that can greatly impede a patient’s capacity to follow their management plan. According to the ADA DM guideline, individuals with blood sugar issues are advised to obtain support from a diverse group of specialists, including psychological professionals. However, the absence of mental wellness assessments in numerous clinics emphasizes a crucial gap in support.
With a staggering 50% nonadherence rate observed among individuals with schizophrenia receiving treatment, there is a pressing need to integrate behavioral support into metabolic condition management. The case study titled ‘Schizophrenia and Diabetes’ illustrates that individuals with schizophrenia are at a higher risk of developing type 2 diabetes due to lifestyle factors and the effects of antipsychotic medications, making it essential to recognize this link for providing comprehensive care and improving well-being outcomes. By proactively addressing psychological barriers—such as the fear of hypoglycemia or stress associated with lifestyle adjustments—healthcare providers can enhance engagement, alleviate anxiety about complications, and ultimately improve well-being outcomes.
Moreover, it is essential for individuals to discuss their mental well-being issues with healthcare professionals, which can result in more customized assistance. As Dr. Douglas Villarroel, a medical expert located in Bolivia, wisely pointed out, ‘If we do that with every individual, the world can change.’ This sentiment illustrates the transformative potential of a comprehensive strategy for managing the condition, especially for individuals facing the dual challenges of this illness and mental well-being issues.
By incorporating mental health assistance, individuals can discover new tranquility in life and lessen their concerns about experiencing traumatic and debilitating complications related to blood sugar issues.
Strengthening Patient Engagement and Self-Management
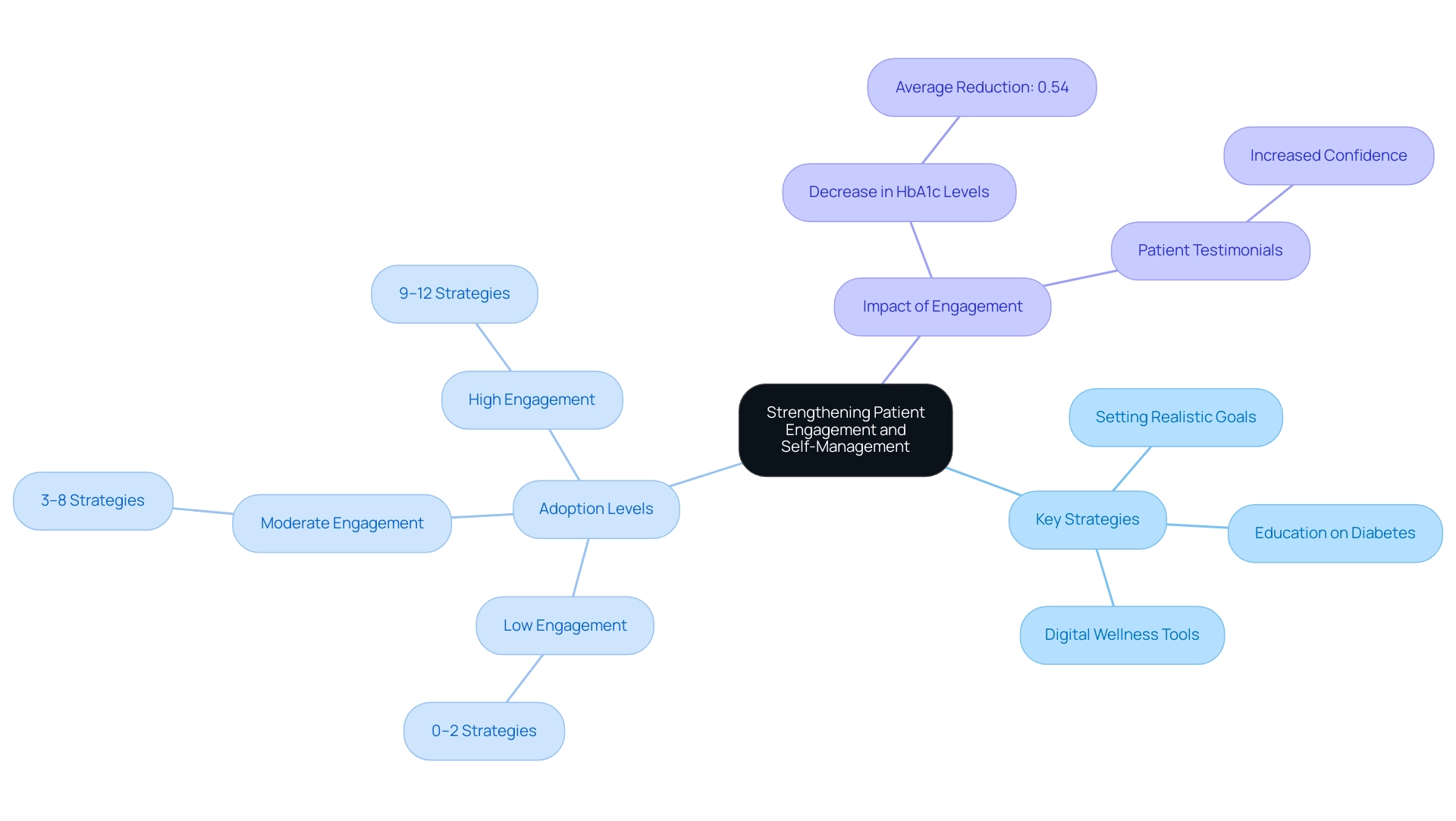
The revised ada dm guideline highlights the essential role of enabling individuals to actively engage in their health management, reflecting a comprehensive strategy for reversing the condition at the Integrative Wellness Center. Key strategies for enhancing client engagement include:
- Setting realistic goals tailored to individual needs.
- Offering thorough education on diabetes according to the ada dm guideline, ensuring individuals comprehend their condition and treatment choices, which aids in reducing anxiety regarding possible complications.
- Utilizing digital wellness tools that facilitate self-monitoring of blood glucose levels, leading to improved outcomes.
Practices are categorized based on their adoption of patient-engagement strategies as ‘low’ (0–25th percentile; range: 0–2 strategies), ‘moderate’ (26–75th percentile; range: 3–8 strategies), or ‘high’ (>75th percentile; range: 9–12 strategies).
Furthermore, evidence indicates that messages related to healthy eating, glucose monitoring, or medication adherence can significantly decrease hemoglobin A1c (HbA) levels by an average of 0.54 percentage points. Regular follow-up appointments are essential for evaluating progress and making necessary adjustments to management plans, supporting a transformative approach to client support. A case study titled ‘Statistical Analysis of Diabetes Management Groups’ found that the good management group was more likely to achieve better self-management outcomes compared to the poor management group, reinforcing the need for customized participant engagement based on demographics and wellness status.
By promoting a cooperative connection between healthcare providers and individuals—as highlighted by Cheryl Pritlove, Partner in Research, who stated, ‘The research team will, therefore, consist of an individual, clinicians, and researchers, who will co-create the scoping review to ensure that the focus incorporates end-user values’—the ada dm guidelines aim to enhance adherence to treatment regimens and ultimately improve wellness outcomes, underscoring the significance of self-management in managing blood sugar.
Patient testimonials further illustrate the effectiveness of these strategies. For example, one patient expressed, ‘Since I began interacting with my healthcare team and using the resources at the Integrative Wellness Center, my anxiety about complications related to my condition has greatly diminished, and I feel more in command of my well-being.’
This emphasizes the center’s dedication to not only managing the condition but also alleviating the concerns that accompany it.
Advocating for Health Equity in Diabetes Care
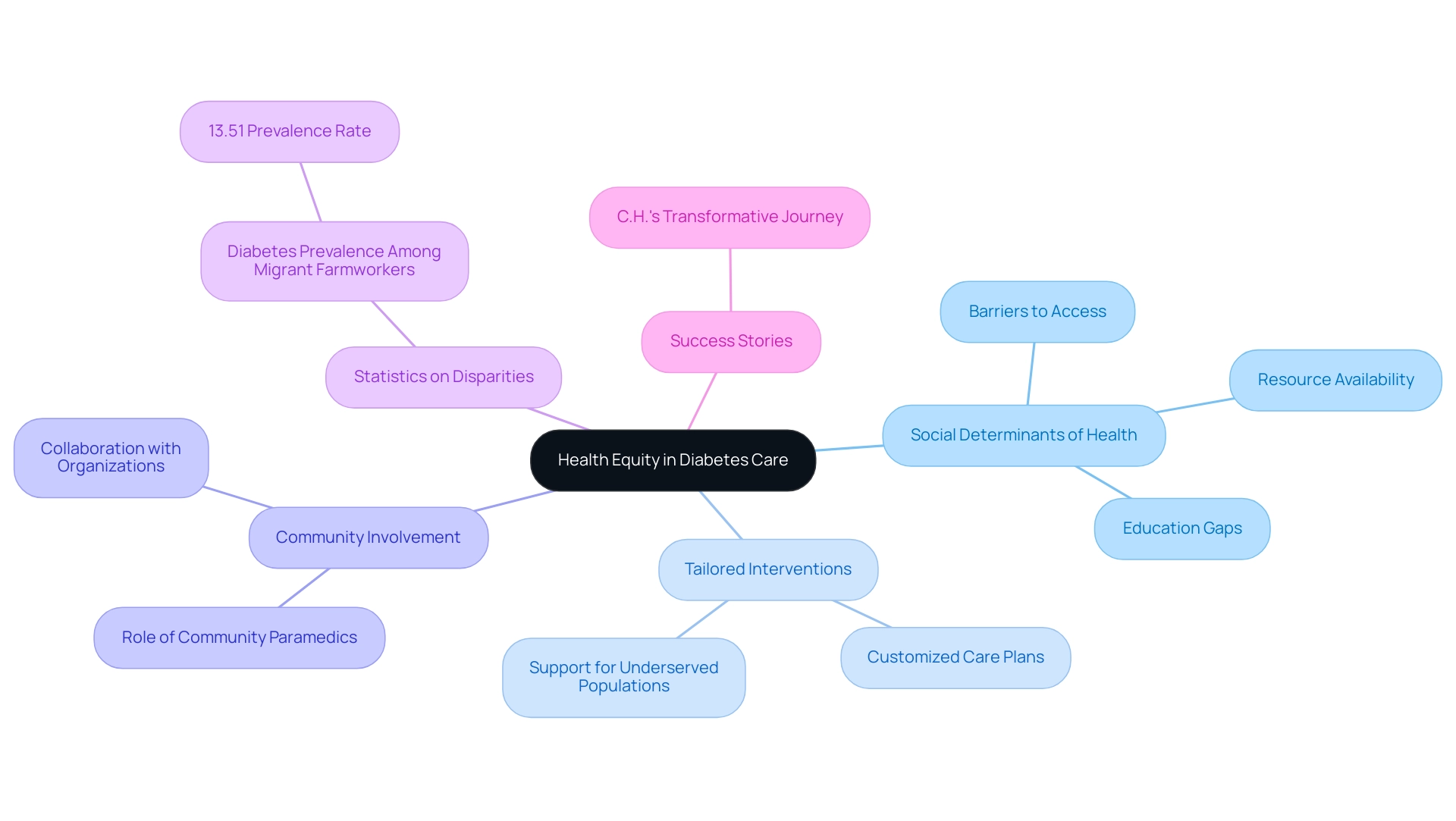
The 2025 ADA DM guideline emphasizes the vital importance of health equity in managing the condition, acknowledging that social determinants of health greatly affect outcomes. These ADA DM guidelines advocate for customized interventions that specifically address the unique challenges faced by underserved populations, including barriers to access, education, and essential resources. Community paramedics play a vital role in this effort by engaging and supporting individuals with blood sugar issues through education and care coordination.
For instance, the age-adjusted self-reported prevalence of the condition was found to be 13.51% among migrant farmworkers, highlighting significant disparities faced by specific populations. Healthcare providers are encouraged to collaborate with community organizations to establish outreach programs that enhance awareness and offer support to high-risk individuals. Recent advocacy efforts have resulted in improved ADA DM guidelines for managing the condition across various settings, reinforcing the significance of addressing equity in wellbeing.
This commitment aims to ensure that every individual has the opportunity for effective management of their condition, irrespective of their socioeconomic status or background. By addressing these disparities, the ADA DM guideline establishes a foundation for improved wellness outcomes and promotes a more equitable healthcare system. Transformative patient success stories, like that of C.H., demonstrate the potential for reversing type 2 conditions and overcoming chronic wellness challenges through a holistic approach at the Integrative Wellness Center.
C.H. moved from ineffective, conventional treatments to tailored support that enabled him to take control of his health, ultimately reducing anxiety about complications and discovering new tranquility in life.
Future Directions in Diabetes Research and Management
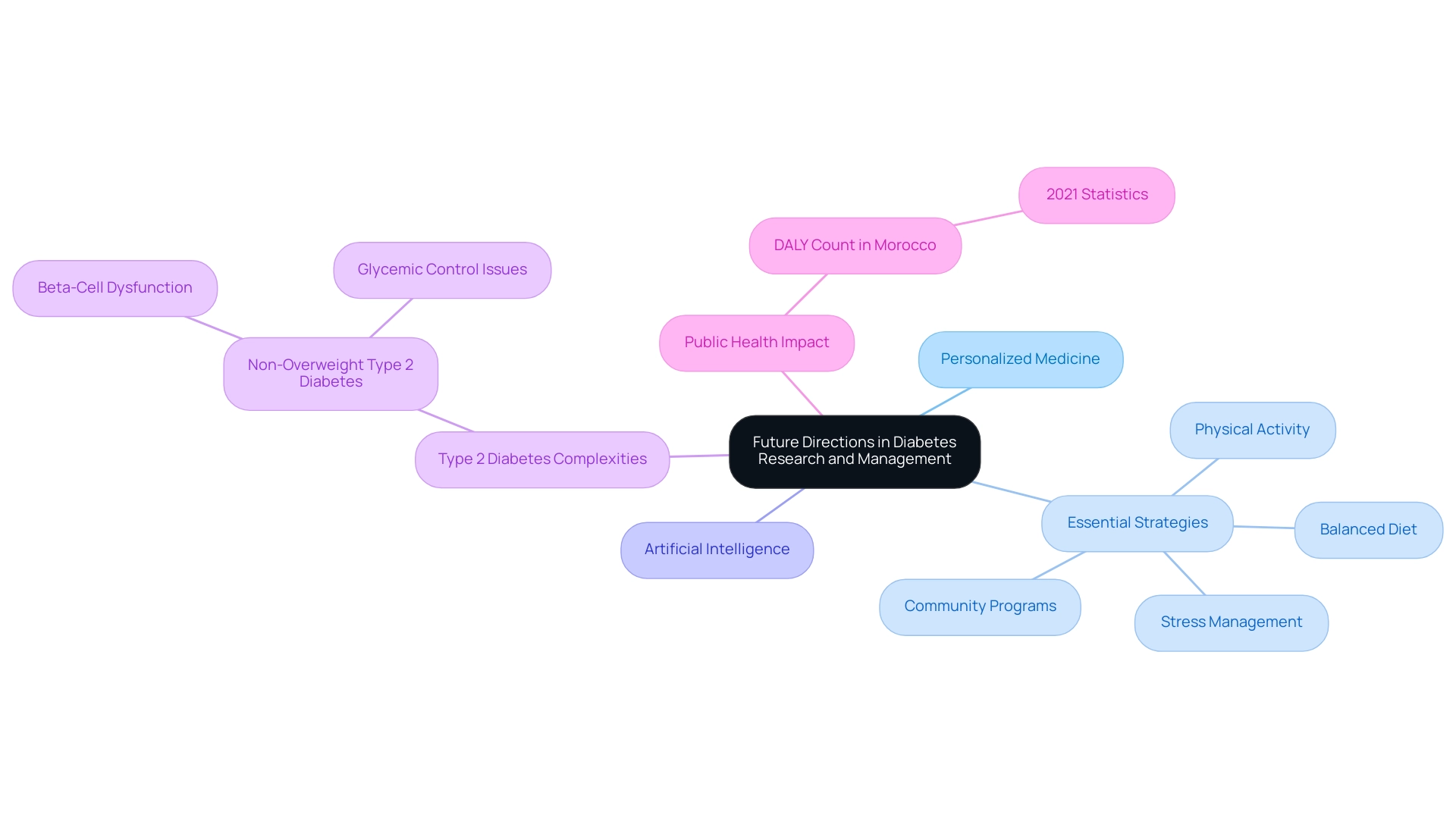
The American Diabetes Association (ADA) DM guideline highlights several promising avenues for future research and management strategies in blood sugar care. A key area of focus is the exploration of personalized medicine approaches, which customize treatment based on individual genetic and metabolic profiles, empowering individuals with tailored strategies that address their unique needs. To improve health and reverse blood sugar issues, individuals can adopt four essential strategies:
- Embracing a balanced diet abundant in whole foods
- Engaging in regular physical activity
- Managing stress through mindfulness practices
- Participating in community wellness programs that offer education and support
Moreover, the incorporation of artificial intelligence into health management tools signifies a considerable progression, improving clinical decision-making and individual involvement. Recent studies suggest that such tools can result in more accurate treatment plans and enhanced outcomes for individuals, aligning with holistic methods to reversing the condition by tackling root causes. Notably, ongoing research into the long-term effects of newer medications is crucial, especially considering the complexities associated with non-overweight Type 2 conditions, which can manifest due to beta-cell dysfunction rather than insulin resistance.
A case study emphasizes that non-overweight individuals with Type 2 may experience worse glycemic control despite lower insulin resistance, underscoring the need for further investigation into Type 2 pathogenesis, irrespective of obesity. Additionally, statistics from Morocco reveal a DALY count of 559 (thousands) in 2021, illustrating the significant impact of this condition on public health. As Sir Zumla, a UK-NIHR Senior Investigator, highlights, ‘Grasping the intricacies of managing metabolic disorders is crucial for enhancing outcomes for individuals.’
As the landscape of diabetes care continues to evolve, healthcare professionals are encouraged to remain informed about the ADA DM guideline and adapt their practices based on the latest evidence and innovations, ensuring the highest quality of care for their patients.
Conclusion
The 2025 American Diabetes Association (ADA) Diabetes Management Guidelines represent a transformative shift in diabetes care, emphasizing the importance of personalized treatment plans that cater to the individual needs of patients. By integrating comprehensive assessments that include mental health and social determinants, these guidelines not only aim to enhance patient engagement but also to improve overall health outcomes. The incorporation of advanced technologies, such as continuous glucose monitoring and automated insulin delivery systems, marks a significant advancement in managing diabetes effectively.
Nutrition and lifestyle strategies are equally critical, with a strong focus on creating tailored dietary plans that consider each patient’s unique preferences and metabolic responses. The guidelines advocate for a holistic approach to diabetes management, recognizing that emotional and behavioral health plays a vital role in treatment adherence. By addressing psychological barriers and fostering patient empowerment, healthcare providers can significantly improve the quality of life for those living with diabetes.
As the healthcare landscape evolves, the commitment to health equity remains paramount. The ADA guidelines call for targeted interventions that address the specific challenges faced by underserved populations, ensuring that all individuals have access to effective diabetes care. With ongoing research into personalized medicine and innovative management tools, the future of diabetes care looks promising. Embracing these comprehensive strategies will not only enhance individual patient outcomes but also contribute to a more equitable healthcare system for all. The journey towards effective diabetes management is ongoing, and these guidelines provide a robust framework for achieving that goal.
Frequently Asked Questions
What are the key revisions introduced in the 2025 ADA DM guideline?
The 2025 ADA DM guideline emphasizes individualized care plans, comprehensive evaluations of physiological, mental, and social factors, and integrates continuous glucose monitoring (CGM) data into clinical decision-making.
How does the 2024 Standards of Care relate to the ADA DM guideline?
The 2024 Standards of Care provide a comprehensive framework for the ADA DM guideline, detailing essential practices for managing diabetes effectively.
What impact do the revisions aim to have on individuals with type 2 diabetes?
The revisions aim to encourage greater involvement of individuals in their care and significantly enhance health outcomes, as demonstrated by success stories of patients who have improved their health metrics.
What role does technology play in the updated ADA DM guideline?
The guideline recognizes innovations such as smart insulin pens, automated insulin delivery systems, and advanced continuous glucose monitors as essential tools for achieving optimal glycemic control.
What additional strategies are emphasized alongside technology in diabetes management?
The guideline highlights the importance of optimizing nutrition, incorporating regular exercise, managing stress, and leveraging community support.
How has telehealth been integrated into diabetes care according to the article?
Telehealth services have become a significant resource, improving accessibility to healthcare for individuals in remote locations or with mobility challenges, allowing for active participation in managing their condition.
What does the article suggest about the future of AI health technologies in diabetes care?
The market for AI health technologies is expected to grow significantly, underscoring the urgency for effective management solutions in diabetes care.
Why is understanding value creation dynamics important in diabetes care?
Understanding the distinction between open networks that prioritize overall value and closed networks that emphasize individual value is crucial for effective execution of technological innovations in diabetes management.
What are the four lesser-known strategies mentioned for reversing diabetes?
The four strategies are optimizing nutrition, incorporating regular exercise, managing stress effectively, and leveraging community support.