Overview
The glucose to A1C conversion chart is essential in diabetes care as it helps patients understand the correlation between their average blood sugar levels and A1C percentages, thereby facilitating better management of their condition. The article emphasizes that regular A1C testing, informed by this chart, allows individuals to track their long-term glucose control and make necessary adjustments to their treatment plans, ultimately improving health outcomes and reducing the risk of complications associated with diabetes.
Introduction
In the realm of diabetes management, understanding the nuances of A1C testing is paramount for individuals striving to maintain optimal health. The A1C conversion chart emerges as a crucial tool, bridging the gap between daily blood glucose readings and long-term glucose control. By translating these figures into comprehensible A1C percentages, patients can gain valuable insights into their overall health and make informed decisions regarding their treatment plans.
Regular A1C testing not only aids in monitoring diabetes but also empowers individuals to engage actively in their care, fostering better communication with healthcare providers. As misconceptions surrounding A1C testing persist, it becomes essential to clarify its significance and integrate effective monitoring strategies into daily routines.
This article delves into the importance of A1C testing, the effective use of conversion charts, and the lifestyle changes that can lead to improved diabetes management.
Understanding the A1C Conversion Chart: A Key Tool in Diabetes Management
The glucose to A1C conversion chart serves as a vital tool in managing health conditions, helping individuals understand the relationship between average blood sugar levels and A1C percentages. The A1C test, often called glycated hemoglobin, measures the percentage of sugar bound to hemoglobin in the bloodstream over the past two to three months. The American Diabetes Association (ADA) recommends that individuals consistently meeting diabetes goals undergo an A1C test at least two times a year, emphasizing the importance of regular testing in diabetes management.
By utilizing the glucose to A1C conversion chart, patients can convert their routine readings into estimated A1C values, thereby enhancing their understanding of long-term control. For instance, a blood glucose level of 154 mg/dL is approximately equivalent to an A1C of 7%. This association is particularly vital for individuals managing type 2 conditions, as it enables them to assess their overall health and make informed adjustments to their treatment plans.
Kari Garner, a Certified Care & Education Specialist, notes that understanding these metrics is crucial for engaging in effective health management. Furthermore, the anxiety and worry surrounding the potential complications of this condition can be alleviated by employing a holistic approach that addresses the root causes of the disease, including understanding insulin resistance. This approach enables individuals to take charge of their health.
By understanding this chart and the implications of insulin resistance, individuals are better prepared to participate actively in their care, leading to enhanced communication with healthcare providers about their progress and required adjustments in management strategies. Additionally, it is important to recognize that traditional treatments can pose dangers, further underscoring the need for a more integrative approach. Initiatives such as the eAG/A1C Conversion Calculator, endorsed by the ADA, emphasize how converting A1C results into recognizable units can improve comprehension and conversations regarding blood sugar management.
By re-evaluating the origin of the condition, patients can adopt strategies that promote better health outcomes.
The Importance of A1C Testing in Diabetes Care
The A1C test acts as a key element of blood sugar control, providing essential information about a person’s average blood sugar levels over a prolonged duration. For individuals with type 2 conditions, regular A1C testing is essential, as it allows tracking of long-term sugar regulation and the assessment of management strategies’ effectiveness. As of 2024, the American Diabetes Association recommends that individuals with the condition undergo A1C testing at least twice a year if their blood glucose levels remain stable, or quarterly if treatment adjustments are necessary.
Significantly, at the Integrative Wellness Center, individuals like John Smith have successfully reached an A1C below 6.5% through personalized care and lifestyle modifications, including customized meal plans and exercise routines, highlighting the potential for substantial enhancement in managing blood sugar. Optimal A1C levels for most adults are generally considered to be below 7%. Levels exceeding this threshold may warrant lifestyle modifications or medication adjustments.
Roopa Naik emphasizes the significance of A1C testing, stating, ‘Regular monitoring is essential for effective management of blood sugar levels and preventing complications.’ Comprehending A1C results and referring to a glucose to A1C conversion chart enables individuals to recognize the significance of sustaining healthy blood sugar levels, thus reducing the likelihood of issues like cardiovascular disease, neuropathy, and kidney damage. Additionally, transformative experiences shared at the Integrative Wellness Center, such as those of Maria Lopez, who successfully managed her condition during pregnancy through specialized care, illustrate the need for personalized care approaches.
By integrating A1C testing into routine health assessments and employing specific techniques like continuous sugar monitoring, individuals can embrace a proactive strategy for managing their condition, ultimately promoting better health results and reducing the financial burdens linked to the illness in the U.S., which were particularly substantial in 2022.
How to Use the A1C Conversion Chart Effectively
To use the A1C conversion chart effectively, individuals must first establish a consistent blood sugar monitoring routine. Routine documentation of sugar readings allows individuals to identify patterns and fluctuations in their levels, which is vital for comprehending insulin resistance and its effects on diabetes management. Once a sufficient set of readings is compiled, individuals can consult the glucose to A1C conversion chart to estimate their A1C percentage.
It is crucial to understand that while the chart offers estimates, laboratory testing remains essential for obtaining accurate A1C results. Furthermore, sharing sugar readings and estimated A1C values with healthcare providers during routine check-ups fosters informed discussions about potential treatment adjustments. This proactive strategy enables individuals to participate actively in their health management, especially concerning Type 2 conditions and the holistic method promoted by the Integrative Wellness Center in San Diego.
By understanding the relationship between daily sugar levels and A1C outcomes, individuals can make informed decisions regarding their diet, exercise, and medication compliance, which are crucial approaches for controlling blood sugar levels, particularly during pregnancy to avert gestational complications. Recent findings indicate that at least 90% of individual patients’ calculated arithmetic mean sugar (AG) should align within ±15% of the study-wide AG, highlighting the significance of regular monitoring. Furthermore, a study highlighted that depending only on fasting plasma levels could postpone the diagnosis of the condition, stressing the importance of utilizing the glucose to A1C conversion chart.
David M. Nathan’s research further strengthens this relationship, stating, ‘Our results strongly support a simple linear relationship between mean blood sugar and A1C levels in a clinically relevant range of glycemia.’ It is also important to recognize that traditional treatments for blood sugar regulation, if not managed properly, can lead to severe health consequences, including insulin resistance and even death. Thus, consistent tracking of blood glucose readings is invaluable for accurate A1C estimation, providing a clearer index of chronic glycemia that supports effective management and addresses the dangers associated with traditional treatment methods.
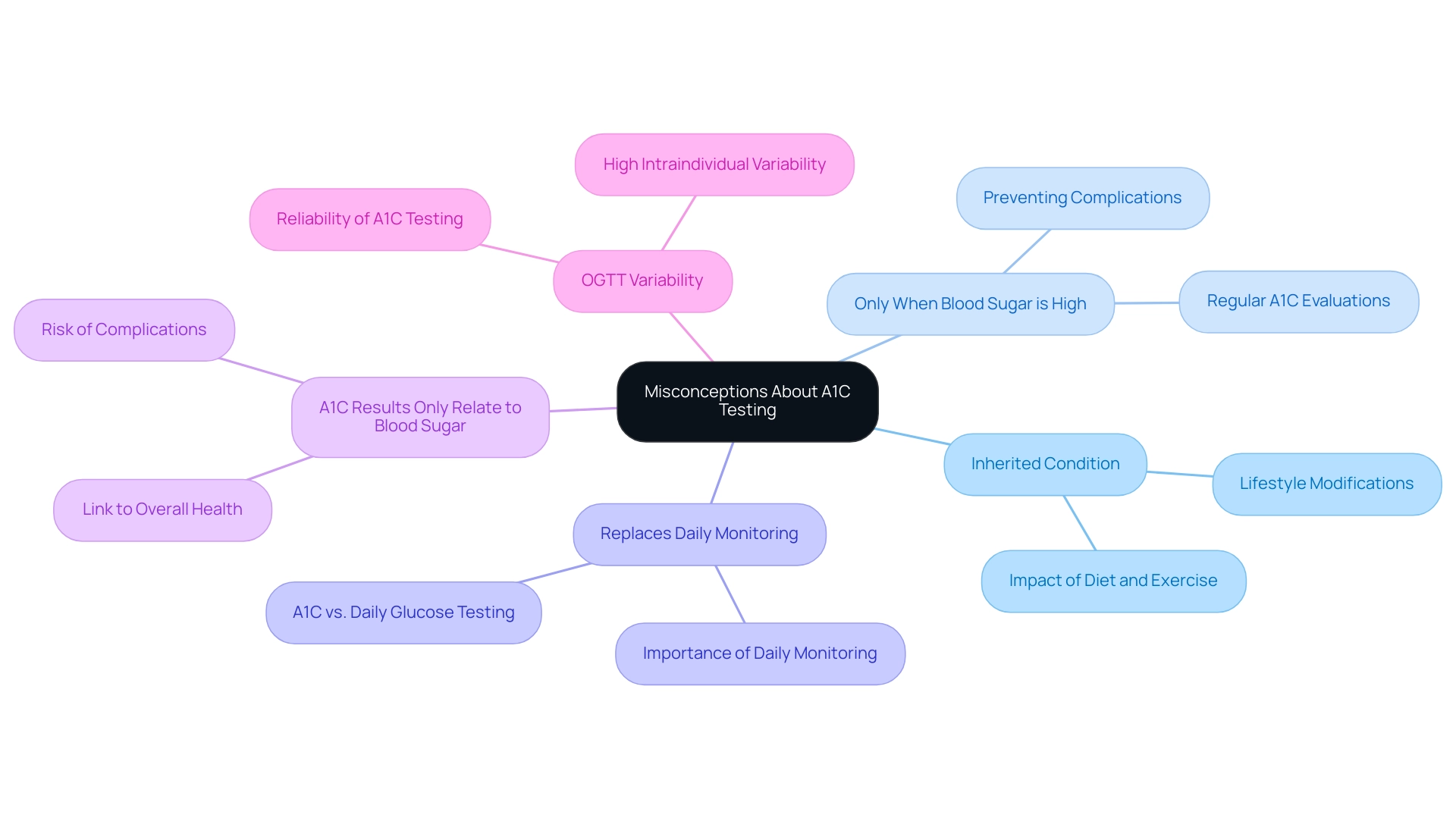
Common Misconceptions About A1C Testing
Misconceptions regarding A1C testing and management of blood sugar can significantly impact patient understanding and health outcomes. A prevalent myth is that this condition is solely inherited, leading many to believe there is nothing they can do to change their situation. In reality, lifestyle modifications, such as diet and exercise, can play a crucial role in reversing type 2 conditions.
Another prevalent misunderstanding is that A1C testing is only required when blood sugar levels are elevated. Regular A1C evaluations, which can be understood through a glucose to A1C conversion chart, are crucial for all individuals diagnosed with this condition, regardless of their current glucose readings. Health institutions promote regular A1C testing to avert complications, as shown by the University of Virginia Health System’s launch of a more precise version of the A1C test, which enables individuals with blood sugar issues to monitor their control more accurately.
Furthermore, some individuals mistakenly believe that A1C results pertain only to the management of blood sugar levels and do not influence overall health; however, elevated A1C levels can be better understood using a glucose to A1C conversion chart, as they are linked to a heightened risk of related complications, making it vital for patients to interpret their A1C results within the broader context of their health. According to David B Sacks from the National Institutes of Health, ‘The significant reduction in microvascular complications with lower A1C and the absence of sample liability… have led to the recommendation by some organizations that A1C be used for screening and diagnosis of this condition.’
Another misconception is that A1C testing can replace daily sugar monitoring. While the glucose to A1C conversion chart provides valuable insights into long-term sugar control, it cannot replace regular self-monitoring, which is crucial for effective daily management of the condition. Additionally, it is important to note that the Oral Glucose Tolerance Test (OGTT) has a high degree of intraindividual variability, with a coefficient of variation of 16.7%. This statistic highlights the reliability of A1C testing as a more stable measure of glucose control.
By dispelling these myths and incorporating innovative strategies, such as personalized care plans and continuous education, individuals can empower themselves and gain a clearer understanding of the significant role A1C testing plays in their comprehensive health strategy and its potential in reversing type 2 conditions.
Integrating A1C Monitoring into Daily Lifestyle Changes
Incorporating A1C monitoring into daily lifestyle modifications is a crucial element for individuals managing type 2. At the Integrative Wellness Center, we promote a holistic approach that re-evaluates the underlying causes of this condition, empowering patients to take control of their health. Patients are encouraged to establish realistic health goals regarding their dietary choices and physical activity, as these factors significantly influence blood glucose levels, which can be tracked with a glucose to A1C conversion chart.
Additionally, addressing the anxiety that often accompanies the worry surrounding potential complications of diabetes is crucial for overall well-being. The American Diabetes Association (ADA) recommends referring individuals at high risk to weight loss and physical activity programs for support, highlighting the importance of structured interventions. For instance, increasing the intake of whole foods—such as fruits, vegetables, and whole grains—can enhance nutritional quality and aid in stabilizing blood sugar levels.
Engaging in regular physical activities, including walking or cycling, not only supports weight management but also improves insulin sensitivity. Recent studies indicate that the median exercise training attendance among participants was 84%, underscoring the effectiveness of structured support in achieving these health goals. Moreover, leveraging technology, such as mobile applications and glucose monitoring devices, enables individuals to effectively track their glucose readings with the help of a glucose to A1C conversion chart.
This real-time data provides motivation and accountability, helping individuals remain committed to their health objectives. By recognizing the correlation between daily lifestyle choices and A1C outcomes, patients can develop a comprehensive management plan that fosters long-term health and well-being. Furthermore, the need for further research into lifestyle modifications is essential, as highlighted by Mathias Ried-Larsen, PhD, who noted that among adults with type 2 condition diagnosed for less than 10 years, a lifestyle intervention compared with standard care resulted in a change in glycemic control that did not reach the criterion for equivalence, but was in a direction consistent with benefit.
This reflects the ongoing need for further research and the potential benefits of lifestyle modifications in managing diabetes effectively.
Conclusion
Understanding the significance of A1C testing is crucial for effective diabetes management. The A1C conversion chart serves as an invaluable tool, allowing individuals to correlate their daily blood glucose readings with long-term glucose control, thereby fostering a deeper understanding of their health. Regular A1C testing, as recommended by the American Diabetes Association, empowers patients to make informed decisions about their treatment plans and engage proactively in their health management.
Dispelling misconceptions about A1C testing is essential for improving patient outcomes. Many individuals mistakenly believe that A1C testing is unnecessary unless glucose levels are high or that it can replace daily monitoring. However, consistent A1C assessments are vital for all patients with diabetes, providing insights that can help mitigate the risk of serious complications. Moreover, integrating A1C monitoring into daily lifestyle changes, including healthy eating and regular exercise, can significantly improve overall health and well-being.
In conclusion, by embracing A1C testing and understanding its implications, individuals can enhance their diabetes management strategies. This proactive approach not only facilitates effective communication with healthcare providers but also empowers patients to take charge of their health. Through informed decision-making and lifestyle modifications, it is possible to achieve better health outcomes and improve the quality of life for those living with diabetes.
Frequently Asked Questions
What is the purpose of the glucose to A1C conversion chart?
The glucose to A1C conversion chart helps individuals understand the relationship between average blood sugar levels and A1C percentages, which is vital for managing health conditions, particularly diabetes.
What does the A1C test measure?
The A1C test measures the percentage of sugar bound to hemoglobin in the bloodstream over the past two to three months, providing insight into long-term blood sugar control.
How often should individuals with diabetes undergo A1C testing?
The American Diabetes Association recommends that individuals meeting diabetes goals have an A1C test at least twice a year if their blood glucose levels are stable, or quarterly if treatment adjustments are needed.
How can patients use the glucose to A1C conversion chart?
Patients can convert their routine blood glucose readings into estimated A1C values using the chart, enhancing their understanding of their long-term blood sugar control.
Why is understanding A1C levels important for individuals managing type 2 diabetes?
Understanding A1C levels allows individuals to assess their overall health, track long-term sugar regulation, and make informed adjustments to their treatment plans.
What are the optimal A1C levels for most adults?
Optimal A1C levels for most adults are generally considered to be below 7%. Levels above this may require lifestyle modifications or medication adjustments.
What role does personalized care play in managing diabetes?
Personalized care, including customized meal plans and exercise routines, has shown success in helping individuals achieve better A1C levels, as demonstrated by cases at the Integrative Wellness Center.
How can regular A1C monitoring benefit individuals with diabetes?
Regular A1C monitoring is essential for effective blood sugar management and can help prevent complications such as cardiovascular disease, neuropathy, and kidney damage.
What is the significance of the eAG/A1C Conversion Calculator?
The eAG/A1C Conversion Calculator, endorsed by the ADA, helps convert A1C results into more recognizable units, improving comprehension and discussions about blood sugar management.
How can integrating A1C testing into routine health assessments impact diabetes management?
Integrating A1C testing into routine assessments allows individuals to adopt proactive strategies for managing their condition, leading to better health outcomes and potentially reducing healthcare costs associated with diabetes.