Overview
The article focuses on the American Diabetes Association (ADA) guidelines for managing gestational diabetes, emphasizing the importance of timely diagnosis, classification, and comprehensive care strategies for affected women. It supports this by detailing the types of gestational diabetes, the significance of early screening, and the need for personalized management approaches that include lifestyle modifications and continuous monitoring to mitigate risks for both mothers and infants.
Introduction
Gestational diabetes mellitus (GDM) poses significant challenges for expectant mothers, characterized by elevated blood sugar levels that can have lasting implications. This condition is not only prevalent—affecting approximately 14.2% of women in high-income countries—but also complex, requiring a nuanced understanding of its classifications and management strategies.
With two primary types, A1 and A2, each necessitating different treatment approaches, the stakes are high for both maternal and fetal health. As healthcare professionals strive to navigate the intricacies of GDM, the importance of timely screening, effective management, and comprehensive postpartum care cannot be overstated.
This article delves into the classifications of gestational diabetes, the guidelines set forth by the American Diabetes Association, and the essential lifestyle modifications that can empower women to maintain their health during and after pregnancy.
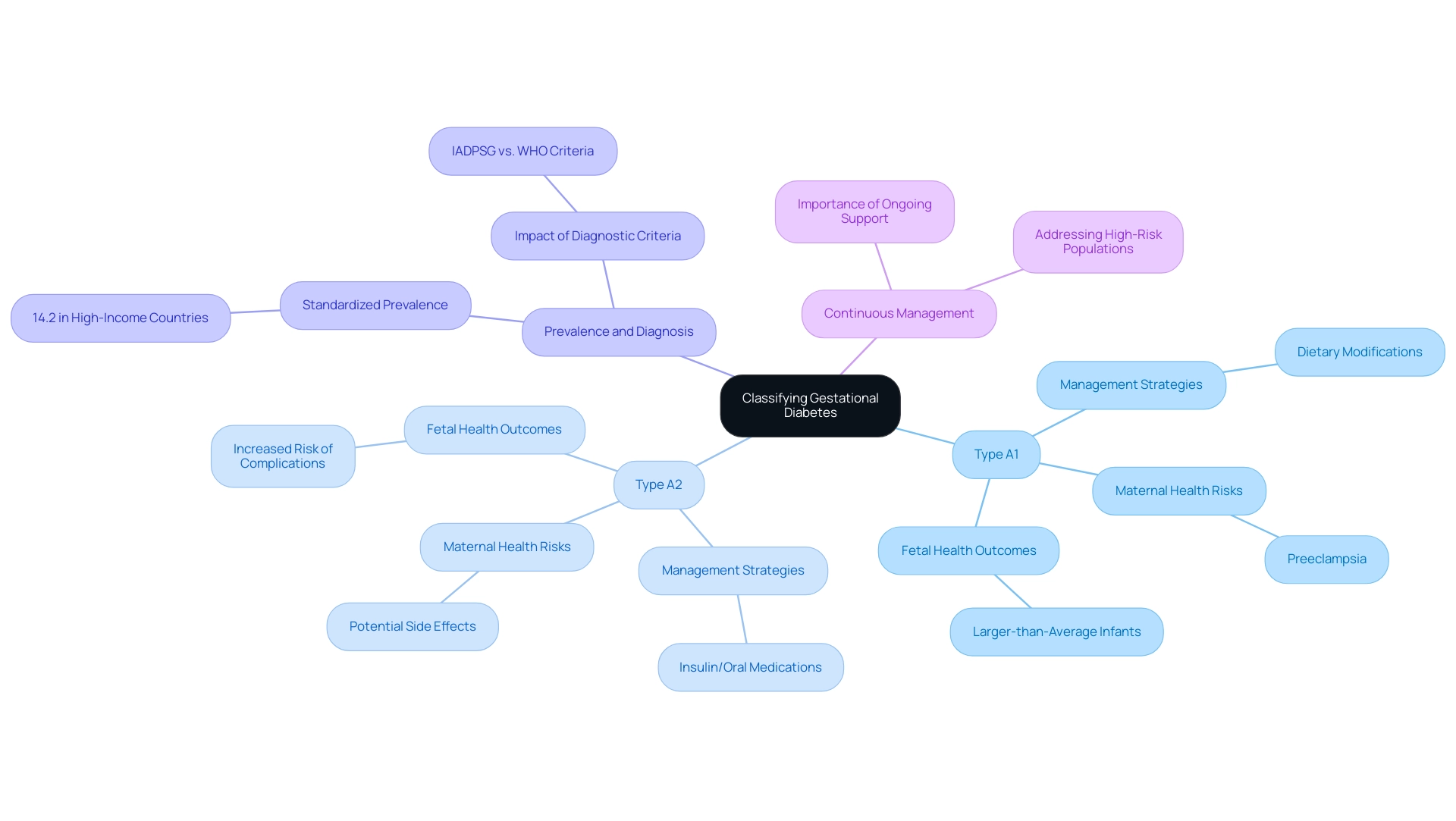
Classifying Gestational Diabetes: Understanding the Types and Their Implications
Gestational diabetes is a condition that arises during pregnancy, characterized by elevated blood sugar levels, and is often referred to as ada gestational diabetes, which typically resolves postpartum. The condition is classified into two distinct categories:
- Type A1, which is managed through dietary modifications,
- Type A2, which necessitates insulin or oral hypoglycemic agents.
Understanding these classifications is crucial, as they directly influence treatment protocols and monitoring strategies, thereby affecting both maternal and fetal health outcomes.
Statistics indicate that the standardized prevalence of GDM in high-income countries stands at 14.2%, underscoring its significance as a public health concern. Women diagnosed with ada gestational diabetes encounter potential complications, including preeclampsia and the likelihood of delivering larger-than-average infants, which reinforces the necessity for timely and precise classification. As highlighted by healthcare expert Khan, ‘This issue does not resolve with the pregnancy and is truly one that we need to concentrate on before, during, and after pregnancy for those affected.’
This viewpoint emphasizes the significance of continuous management and assistance for women with ada gestational diabetes. Bottalico talked about the implications of recurrent gestational conditions, emphasizing the significance of understanding contributing factors, diagnosis, and management strategies. Additionally, it is essential to recognize the role of insulin resistance in ada gestational diabetes, as it can complicate treatment and increase the risk of adverse outcomes.
Traditional treatments may pose dangers, including potential side effects that could lead to severe health issues. Therefore, an integrative approach to managing the condition is critical, offering safer alternatives that prioritize overall well-being. Furthermore, the case study titled ‘Impact of Diagnostic Criteria on GDM Prevalence’ revealed that the prevalence of GDM diagnosed using IADPSG’s criteria is significantly higher than that diagnosed by other criteria, highlighting the influence of diagnostic criteria on reported prevalence rates.
These findings suggest that adopting the IADPSG’s criteria could lead to a more accurate representation of GDM prevalence, which is crucial for effective public health planning and resource allocation. Recent studies also indicate a pressing need for more medical resources to address GDM in high-risk populations, emphasizing the urgency of the issue in the context of healthcare planning.
Diagnostic Testing and Screening for Gestational Diabetes: ADA Guidelines Explained
The American Diabetes Association (ADA) strongly promotes the testing of all expectant mothers for ADA gestational diabetes between 24 and 28 weeks of pregnancy. The predominant method employed for this screening is the glucose challenge test, which involves the collection of a blood sample after the ingestion of a sugary drink. Should the initial results indicate elevated glucose levels, a follow-up oral glucose tolerance test is administered to confirm a definitive diagnosis.
This two-step process is crucial, as the ADA guidelines emphasize that early identification of ADA gestational diabetes is vital for reducing possible complications for both the mother and the child. Furthermore, understanding insulin resistance and the dangers associated with traditional treatments, such as increased risk of complications and potential adverse effects, is crucial in this context. It is crucial to recognize that the U.S. Preventive Services Task Force (USPSTF) does not suggest any particular screening test for pregnancy-related sugar issues, which adds complexity to the screening landscape.
Currently, a systematic review by the Office of Medical Applications of Research (OMAR) and the USPSTF is underway to evaluate the effectiveness of these screening methods and their impact on treatment outcomes. According to recent findings, 71% of pregnancy-related glucose intolerance cases diagnosed as ADA gestational diabetes resulted in infants with a birth weight of 3.5 kg or more (macrosomia), compared to only 43% diagnosed by World Health Organization (WHO) criteria. This statistic highlights the increased likelihood of neonatal complications linked to the ADA’s diagnostic criteria.
As noted by Latika Sahu from the Department of Obstetrics & Gynecology at the Jawaharlal Institute of Postgraduate Medical Education and Research in Puducherry, India, “Thus, neonatal complications were higher in those diagnosed with ADA gestational diabetes when compared with those diagnosed by WHO criteria.” Together, these recommendations and insights highlight the essential significance of prompt screening and a comprehensive method for managing blood sugar levels during pregnancy, which involves recognizing the dangers of conventional treatments, to avoid pregnancy-related glucose issues.
Managing Gestational Diabetes: Treatment Options and Lifestyle Recommendations
The management of ada gestational diabetes and other pregnancy-related blood sugar issues requires crucial lifestyle changes, including a balanced diet abundant in whole grains, lean proteins, and healthy fats. Regular physical activity, such as walking or swimming, is highly encouraged, as it plays a crucial role in enhancing glucose tolerance, particularly in the context of insulin resistance. Evidence from the Health and Human Services, USA indicates that physical activity significantly improves abnormal glucose tolerance, which is often more related to insulin resistance than merely insufficient circulating insulin levels.
It is important to recognize that traditional therapies for insulin resistance can pose significant dangers, potentially leading to severe consequences, including death. If lifestyle changes prove insufficient for controlling blood glucose levels, healthcare providers may consider insulin therapy or oral medications as additional treatment options. Continuous monitoring of blood glucose is vital to gauge the effectiveness of these interventions and to refine the management plan as necessary.
The American Diabetes Association (ADA) emphasizes the importance of a personalized approach for managing ada gestational diabetes, tailoring strategies to each individual’s unique needs and circumstances. Recent intervention studies highlight that effective management of ada gestational diabetes requires a synergistic combination of lifestyle changes and, when warranted, medical interventions to safeguard the health of both mother and child. Furthermore, ongoing studies emphasize the importance of enhanced reporting on intervention attributes and adherence assessment, which are crucial for refining pregnancy-related prevention strategies.
It is also critical to recognize that pregnant individuals with blood sugar issues are at heightened risk for new-onset retinopathy and the progression of existing retinopathy, particularly during periods of rapid glycemic control. Therefore, close monitoring and management of retinopathy during pregnancy are imperative to avert complications, illustrating the importance of a comprehensive management approach that addresses both lifestyle and medical needs.
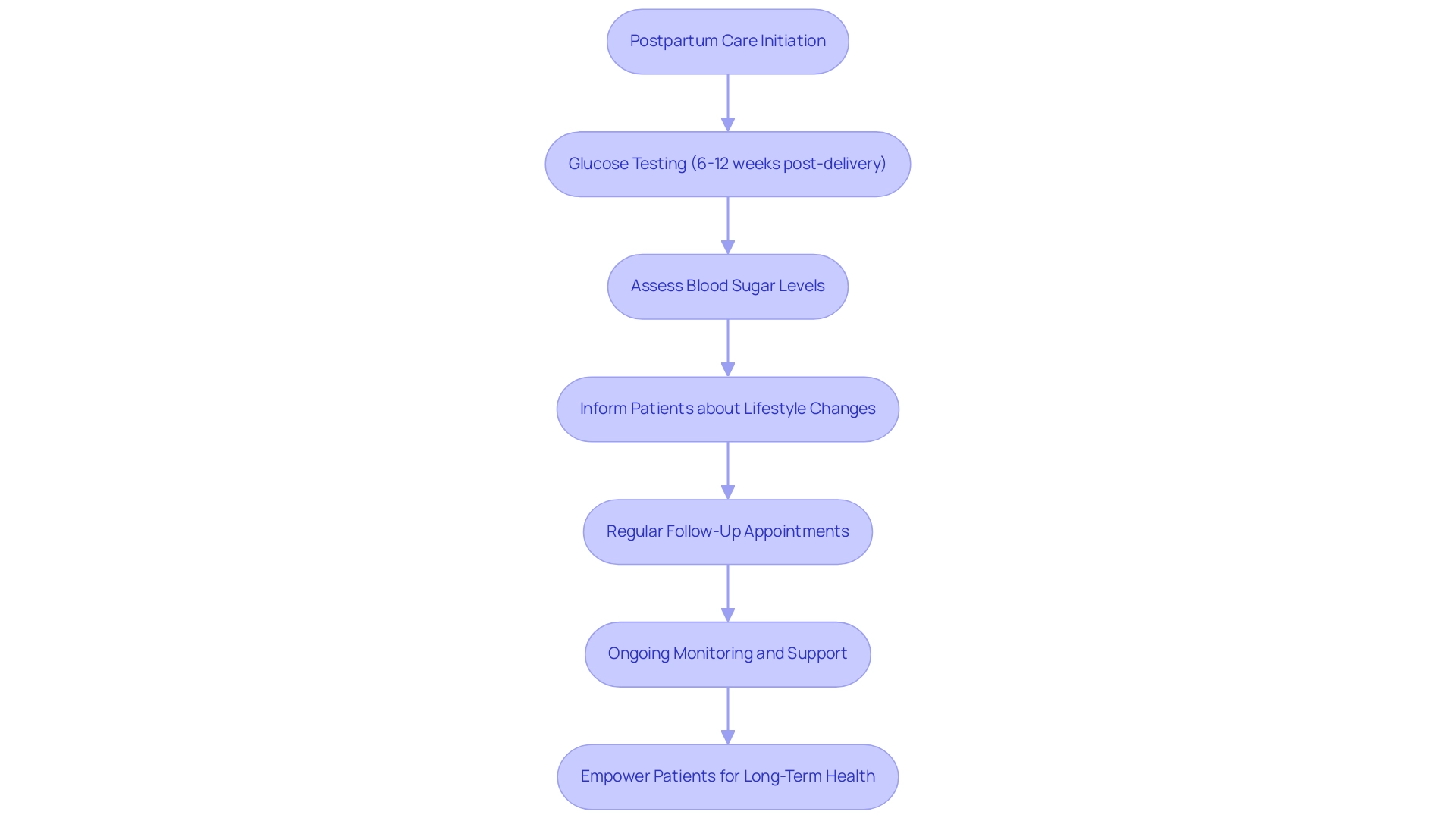
Postpartum Care for Gestational Diabetes: Ensuring Long-Term Health
Postpartum care is crucial for women who have experienced ada gestational diabetes, as it involves glucose testing to assess whether their blood sugar levels have returned to normal. The American Diabetes Association (ADA) recommends that testing for ada gestational diabetes should occur between 6 to 12 weeks after delivery. Timely assessments are crucial, as women with ada gestational diabetes are 8.3 times more likely to develop type 2 health issues compared to those with normoglycemic pregnancies.
Informing patients about lifestyle changes after delivery is essential to reduce the likelihood of future health issues, highlighting a comprehensive approach that considers both physical and emotional well-being. Regular follow-up appointments with healthcare providers facilitate ongoing monitoring and offer necessary support for maintaining a healthy lifestyle. As Vendula Bartáková notes, ‘The strength of the study lies in the fact that our proposed risk score identifying women with a higher risk of PGI does not require any additional tests over the ones routinely performed and is therefore easily applicable in clinical practice.’
This insight underscores the importance of incorporating simple yet effective strategies into postpartum care to improve long-term health outcomes. Furthermore, additional research is needed to confirm diagnosis and determine treatment interventions for individuals with abnormal glucose results, highlighting ongoing challenges in postpartum care. The ‘National Register Evaluation’ highlights these challenges, concentrating on screening, registration, and follow-up procedures, ultimately identifying key issues and suggesting solutions to improve the effectiveness of care for women with pregnancy-related conditions.
By adopting an integrative wellness approach, we can empower patients to take control of their health, reducing anxiety over potential complications related to blood sugar.
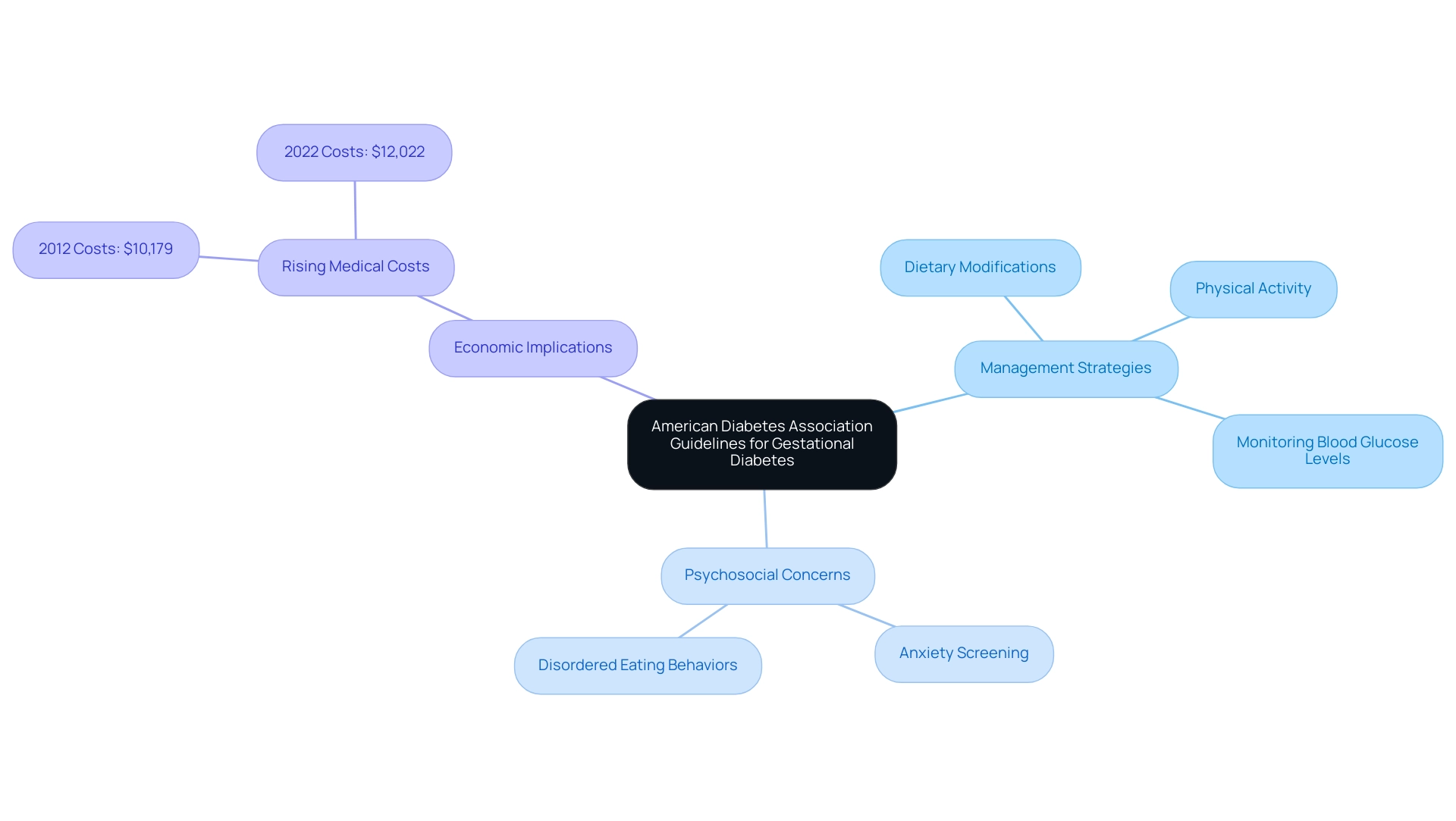
The Role of the American Diabetes Association in Guiding Gestational Diabetes Care
The American Diabetes Association (ADA) plays a crucial role in establishing evidence-based guidelines essential for managing ada gestational diabetes and other pregnancy-related blood sugar issues. These thoughtfully developed guidelines are intended to enable healthcare providers to offer optimal care to pregnant women who are at vulnerability for or diagnosed with ada gestational diabetes. Regular updates to these recommendations ensure that both patients and healthcare professionals have access to the most current and relevant information, including essential strategies for managing blood sugar levels during pregnancy, particularly for those with ada gestational diabetes, such as:
- Dietary modifications
- Regular physical activity
- Monitoring blood glucose levels
This commitment to education fosters a supportive environment that alleviates anxiety regarding complications, enabling women to take control of their health throughout pregnancy. With nearly 39.5% of adults with this condition having a non-HDL level of 130 mg/dL or higher, the importance of these guidelines is amplified, as they aim to mitigate risks and improve health outcomes. Furthermore, the Ada’s guidelines address psychosocial concerns, including the screening of distress related to blood sugar management, anxiety, and disordered eating behaviors, as highlighted in the case study titled ‘Psychosocial Care in Diabetes Management.’
This holistic approach is essential for the comprehensive management of ada gestational diabetes in pregnant women, ensuring that they feel supported and informed. Additionally, the financial implications of diabetes management are significant; from 2012 to 2022, excess medical costs per person increased from $10,179 to $12,022, underscoring the critical role of the Ada’s guidelines in promoting effective management strategies.
Conclusion
Gestational diabetes mellitus (GDM) is a significant health concern that demands comprehensive understanding and management. The classifications of GDM into Type A1 and A2 highlight the necessity for tailored treatment approaches, as each type presents unique challenges and implications for maternal and fetal health. Early and accurate screening, as recommended by the American Diabetes Association, is essential to mitigate potential complications and ensure the well-being of both mother and child.
Effective management of GDM revolves around crucial lifestyle modifications, including a balanced diet and regular physical activity, to enhance glucose tolerance. When these interventions are insufficient, medical treatments must be considered, reinforcing the need for continuous monitoring and personalized care plans. The integration of lifestyle changes with medical interventions is vital for safeguarding health during and after pregnancy.
Postpartum care is equally important, as women with a history of GDM are at a heightened risk for developing type 2 diabetes. Ongoing glucose testing and education on lifestyle modifications play a critical role in promoting long-term health. The American Diabetes Association’s guidelines serve as a valuable resource for healthcare providers, ensuring that they have access to the latest strategies for managing gestational diabetes effectively.
In conclusion, addressing gestational diabetes requires a multifaceted approach that encompasses timely screening, personalized management strategies, and robust postpartum care. By prioritizing these elements, healthcare providers can significantly improve health outcomes for women and their families, ultimately fostering a healthier future.