Overview
A diabetes nurse educator (DNE) is a specialized nurse who provides education and support to individuals with diabetes, focusing on self-management techniques such as blood glucose monitoring and dietary adjustments. The article emphasizes that the DNE’s role is crucial in improving patient outcomes through personalized education and ongoing support, which has been shown to enhance self-care skills and reduce complications associated with diabetes.
Introduction
The role of Diabetes Nurse Educators (DNEs) has become increasingly critical in the management of diabetes, particularly as the prevalence of Type 2 Diabetes continues to rise. These specialized nurses are not only responsible for educating patients about their condition but also for fostering a supportive environment that empowers individuals to take charge of their health.
Through tailored educational strategies, DNEs help patients navigate the complexities of diabetes management, addressing both practical self-care techniques and the emotional challenges that accompany the disease.
As research highlights the effectiveness of diverse educational approaches, the demand for skilled diabetes educators is surging, underscoring the need for a well-trained workforce to meet the evolving healthcare landscape.
This article delves into the essential functions of DNEs, the qualifications required for this role, and the profound impact they have on patient outcomes, ultimately illustrating the value of comprehensive diabetes education in promoting healthier lifestyles.
Defining the Role of a Diabetes Nurse Educator
A diabetes nurse educator (DNE) is a specialized nurse dedicated to the instruction and support of individuals with the condition, particularly those impacted by Type 2 Diabetes. Their key responsibilities as a diabetes nurse educator encompass:
- Assessing individuals’ understanding of their condition
- Formulating personalized educational strategies
- Offering guidance on essential self-management techniques, including:
- Blood glucose monitoring
- Insulin administration
- Dietary adjustments
This role of the diabetes nurse educator is essential in fostering a collaborative connection between the instructor and the individual, enabling them to effectively manage their diabetes, reduce anxiety associated with potential complications, and cultivate a sense of tranquility regarding their health.
Recent studies have highlighted the effectiveness of a comprehensive method for instruction by a diabetes nurse educator. Patients who obtain information through both individual and group methods, guided by a diabetes nurse educator, achieve the highest self-care scores and maintain lower HbA1c levels. The research named ‘Comparison of Instruction Techniques’ assessed the effectiveness of individual, group, and combined teaching methods on outcomes for individuals, revealing that those who engaged in both formats had the most favorable results, much like the comprehensive approach of a diabetes nurse educator.
Moreover, a descriptive study published in BMC Nurs in August 2022 highlighted the benefits of online learning for medical staff, particularly during social distancing restrictions, suggesting that such methods could enhance education for individuals with chronic blood sugar issues, especially when guided by a diabetes nurse educator.
In regions where the roles of nurses in providing support for patients with chronic blood sugar issues are ambiguous, such as Saudi Arabia, the need for recognized groups like Diabetes Integrated Support Nurses (DISNs) becomes evident. By emphasizing education on the condition, a diabetes nurse educator can significantly enhance health outcomes, challenge prevalent myths, and demonstrate the crucial influence of their expertise on individual knowledge and self-management. This holistic approach not only addresses the root causes of the condition but also empowers patients to overcome misconceptions and manage their health confidently.
Qualifications and Skills Required for Diabetes Nurse Educators
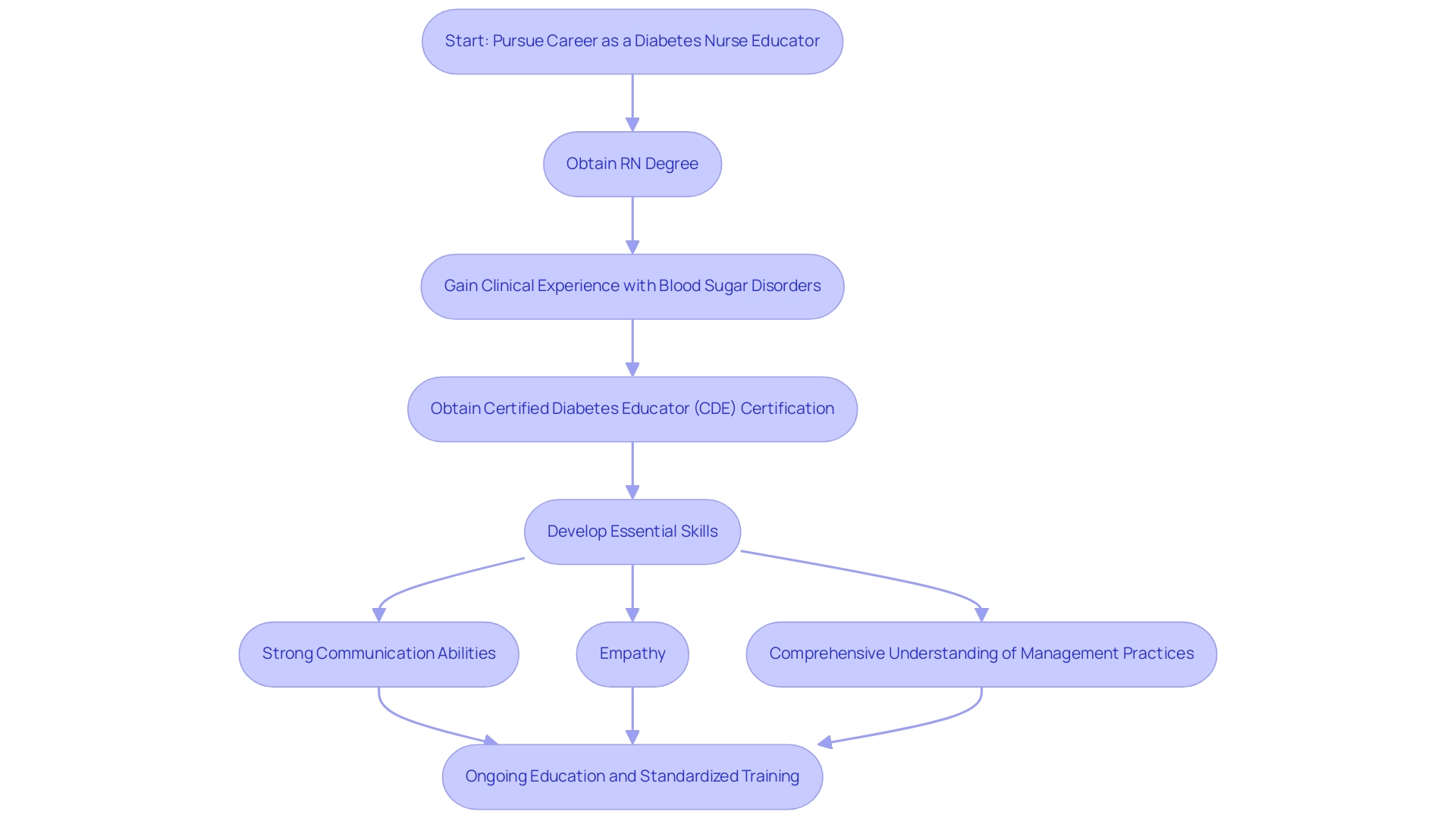
To pursue a career as a diabetes nurse educator, candidates must first obtain a registered nursing (RN) degree, which serves as the foundational qualification. Following this, relevant clinical experience in managing blood sugar disorders is essential to develop practical skills and insights. One of the key certifications that significantly enhances a nurse’s credentials is the Certified Diabetes Educator (CDE) designation, which is highly recommended and increasingly sought after.
Statistics indicate that certification rates among educators in managing blood sugar conditions are rising, reflecting the growing recognition of the value of specialized training in management. Crucial skills for a diabetes nurse educator include:
- Strong communication abilities, which enable effective interactions with individuals
- Empathy to establish trust and rapport with clients
- A comprehensive understanding of management practices related to the condition
Moreover, ongoing education is essential; keeping informed about the most recent studies in care not only preserves a nurse educator’s efficiency but also directly affects outcomes for those receiving treatment.
A recent study emphasized that educational interventions can positively influence the beliefs, behaviors, and quality of life of patients with blood sugar issues, highlighting the critical role that diabetes nurse educators play in this process. The reliability of the CHC test across all items was found to be 0.88, underscoring the need for standardized instruction and training. Furthermore, a case study named ‘Comparison of Teaching Techniques’ showed that instruction provided through both individual and group methods resulted in the highest self-care scores and the lowest HbA1c levels, suggesting that a combined approach may be the most effective for managing blood sugar.
This corresponds with the rising need for standardized programs related to blood sugar management and an increase in the number of diabetes nurse educators to enhance teaching efficiency.
The Growing Demand for Diabetes Nurse Educators
The demand for diabetes nurse educators is experiencing significant growth, driven by the rising prevalence of type 2 conditions and the urgent need for effective management strategies. Recent statistics show that this condition persists in impacting a growing number of individuals, heightening the demand for healthcare professionals adept in delivering specialized guidance and support. At the Integrative Wellness Center, we concentrate on empowering patients to remove anxiety regarding complications from blood sugar issues through comprehensive support and information.
Our unique approach includes:
- Personalized coaching
- Group workshops
- Community wellness programs that emphasize nutrition and lifestyle changes
Significantly, 61.6% of the instruction offered concentrates on foot care, emphasizing vital aspects within sugar-related health awareness. Job postings for diabetes nurse educators have surged, particularly within outpatient settings, hospitals, and community health organizations, indicating a robust job market for professionals in this field.
Moreover, perspectives from different specialists, including Katy Davenport, highlight the essential function of health awareness in improving patient results. For example, the International Diabetes Mellitus Practices Study demonstrated that better knowledge and self-management techniques significantly improved the quality of support for individuals with type 1. This relationship between learning and quality of care highlights the significance of strengthening the workforce of diabetes nurse educators to address the changing healthcare requirements of a growing affected population.
Additionally, online education has been shown to increase training uptake among nursing staff, illustrating the evolving methods of education and their impact on the workforce. This aligns perfectly with our mission to challenge misconceptions and promote transformative health solutions at the Integrative Wellness Center, where we are dedicated to discovering real solutions that empower individuals in their management journey.
Impact of Diabetes Nurse Educators on Patient Health Outcomes
Extensive research underscores the pivotal role of a diabetes nurse educator in enhancing health outcomes, particularly within the holistic framework of the Integrative Wellness Center. These experts greatly enhance self-management abilities and broaden individual comprehension of the condition, which are essential for effective disease management. Evidence indicates that individuals who work with a diabetes nurse educator not only attain better glycemic control but also face fewer hospital admissions and enjoy an overall enhanced quality of life.
Significantly, 61.6% of the instruction given emphasizes vital components like foot maintenance, underscoring an important aspect of managing blood sugar. Transformative success stories from the Integrative Wellness Center, such as those of individuals who have successfully reversed their type 2 condition through personalized care, empower individuals to eliminate anxiety over potential complications. A randomized study comparing group versus individual training for managing blood sugar showed that although both methods produce beneficial outcomes, group instruction provides extra support and encouragement, creating a cooperative atmosphere for patients.
Additionally, as S.C. wisely pointed out, further research is suggested to identify the elements that could impact the effectiveness of instruction given by diabetes nurse educators focused on managing blood sugar. This emphasizes the continual requirement to investigate the different aspects of health awareness effectiveness. Furthermore, recent studies on closed-loop insulin delivery in hospitalized individuals with type 2 metabolic disorder have demonstrated potential in enhancing outcomes.
Ultimately, personalized learning and ongoing assistance offered by diabetes nurse educators aid individuals in managing the intricacies of their condition, paving the way for healthier lifestyles and more effective control while alleviating worries about the debilitating complications of the illness.
Continuing Education and Professional Development for Diabetes Nurse Educators
Ongoing training is vital for diabetes nurse educators, as it allows them to stay updated on the latest developments in blood sugar management and treatment. This continuous learning empowers patients to eliminate anxiety over potential complications through holistic care and knowledge at the Integrative Wellness Center. The center emphasizes a holistic approach to managing the condition, addressing root causes and providing comprehensive support.
Different organizations offer workshops, webinars, and certification programs designed for the changing environment of health instruction, concentrating on new research and best practices. As noted by Esra Uğur, PhD at Okan University School of Health Sciences, the need for education in medication regimens (69.0%) and special care applications like wound care (54.0%) is critical. Additionally, a recent case study titled ‘ABCs of Diabetes Management’ revealed that:
- Only 11.1% of individuals met all recommended criteria for A1C, blood pressure, cholesterol, and smoking status.
- 36.8% met less stringent goals.
Such statistics highlight the challenges faced in achieving optimal management of the condition, reinforcing the importance of continued professional development for diabetes nurse educators in this field. Participating in these educational opportunities not only enhances their skill sets but also prepares them to apply the most effective strategies for those they serve, ultimately leading to improved health outcomes and a greater understanding of insulin resistance and its management. Furthermore, with 19.0% of adults with prediabetes reporting they were informed of their condition by a health professional, the role of education becomes even more crucial in managing this condition effectively.
By integrating holistic care practices, the Integrative Wellness Center aims to alleviate patient concerns about diabetes complications and promote overall well-being.
Conclusion
The role of Diabetes Nurse Educators is indispensable in the fight against the rising prevalence of Type 2 Diabetes. These specialized professionals not only provide essential education on diabetes management but also foster a supportive environment that empowers patients. By implementing tailored educational strategies, DNEs enhance patients’ self-management skills, leading to improved health outcomes and a better quality of life.
The qualifications and skills required for DNEs, including strong communication and empathy, are critical in establishing trust and effectively conveying complex information. As the demand for these educators continues to grow, it is evident that their specialized training and ongoing professional development are vital in adapting to the evolving healthcare landscape. The increasing recognition of their role reflects the urgency of addressing the diabetes epidemic through comprehensive education.
Research consistently demonstrates that patients who engage with Diabetes Nurse Educators achieve better glycemic control and experience fewer complications. By integrating both individual and group educational methods, DNEs create a collaborative learning atmosphere that enhances motivation and support among patients. As the healthcare system adapts to meet the challenges posed by diabetes, the importance of well-trained diabetes educators cannot be overstated.
In summary, the contributions of Diabetes Nurse Educators are fundamental to improving diabetes management and patient health outcomes. Their expertise not only equips patients with the necessary tools to manage their condition but also plays a crucial role in mitigating the anxiety associated with diabetes complications. As the need for effective diabetes education continues to rise, investing in the training and development of these professionals will be key to fostering healthier communities and combating the diabetes epidemic.
Frequently Asked Questions
What is the role of a diabetes nurse educator (DNE)?
A diabetes nurse educator is a specialized nurse who instructs and supports individuals with diabetes, particularly those with Type 2 Diabetes. Their key responsibilities include assessing individuals’ understanding of their condition, formulating personalized educational strategies, and offering guidance on self-management techniques such as blood glucose monitoring, insulin administration, and dietary adjustments.
How do diabetes nurse educators improve patient outcomes?
Diabetes nurse educators foster a collaborative relationship with individuals, helping them manage their diabetes effectively, reduce anxiety about potential complications, and feel more at ease regarding their health. Studies show that patients who receive education through both individual and group methods achieve better self-care scores and lower HbA1c levels.
What educational methods do diabetes nurse educators employ?
Diabetes nurse educators utilize a comprehensive approach that includes both individual and group teaching methods to enhance patient education and engagement. This dual approach has been shown to yield favorable health outcomes for individuals with diabetes.
What qualifications are needed to become a diabetes nurse educator?
To become a diabetes nurse educator, candidates must first obtain a registered nursing (RN) degree, followed by relevant clinical experience in managing blood sugar disorders. Obtaining the Certified Diabetes Educator (CDE) certification is highly recommended to enhance credentials.
What skills are essential for a diabetes nurse educator?
Essential skills for a diabetes nurse educator include strong communication abilities, empathy to build trust with clients, and a comprehensive understanding of diabetes management practices. Ongoing education is also crucial for staying informed about the latest care studies.
What impact do diabetes nurse educators have on patients’ beliefs and behaviors?
Educational interventions by diabetes nurse educators can positively influence patients’ beliefs, behaviors, and quality of life regarding their diabetes management, highlighting their critical role in improving health outcomes.
Why is there a growing need for diabetes nurse educators?
There is an increasing recognition of the value of specialized training in diabetes management, reflected in rising certification rates among educators. The demand for standardized programs and effective teaching methods in blood sugar management further emphasizes the need for more diabetes nurse educators.