Overview
The ADA Plate Method is a visual meal planning strategy for diabetics that emphasizes portion control and balanced nutrition by filling half the plate with non-starchy vegetables, a quarter with lean protein, and a quarter with healthy carbohydrates. The article supports this by detailing a step-by-step guide and highlighting research that shows this method improves glycemic control, making it an effective tool for managing blood sugar levels.
Introduction
The ADA Plate Method offers a structured approach to meal planning that is particularly beneficial for individuals managing diabetes. By visually dividing a plate into sections dedicated to non-starchy vegetables, lean proteins, and carbohydrates, this method simplifies the process of creating balanced meals while promoting stable blood sugar levels.
Research has shown that adhering to this method can significantly enhance glycemic control, making it a practical tool for effective diabetes management.
This article delves into the key components of the ADA Plate Method, providing:
- A step-by-step guide for implementation
- Tips for successful meal planning
- Strategies to overcome common challenges associated with dietary adherence
By understanding and utilizing this method, individuals can take proactive steps toward better health and improved quality of life.
Understanding the ADA Plate Method for Diabetes Management
The ada plate method acts as a useful visual aid that helps individuals with blood sugar issues in creating balanced dishes intended to support stable glucose levels. This method places a strong emphasis on portion control and the inclusion of diverse food groups. According to recent studies, this approach promotes:
- Filling half of your plate with non-starchy vegetables, which are essential for nutrient density and low calorie intake.
- One-quarter with lean proteins to aid in muscle maintenance and overall health.
- One-quarter with carbohydrates, which should be chosen carefully to manage blood sugar effectively.
This organized system not only streamlines the food preparation process but also guarantees the intake of suitable amounts of vital nutrients, in accordance with management strategies for blood sugar. Notably, findings from the Diabetes Nutrition Education Study (DINES) indicate that both carbohydrate counting and the modified plate method significantly improved glycemic control in patients with an initial HbA between 7–10%, with a change in HbA from baseline to 6 months for high numeracy patients in the plate method being −0.88% (−1.54, −0.21). This underscores the effectiveness of Certified Diabetes Educator (CDE) delivered self-management education and support (DSME/S) for individuals with the condition.
As Luohua Jiang, PhD, from the Department of Epidemiology and Biostatistics at the University of California, Irvine, mentions, ‘The ADA Plate Method provides an effective framework for managing the condition through visual meal planning.’ Therefore, the adoption of the ada plate method can be a key benefit for those managing blood sugar levels. Additionally, it is recommended that individuals with blood sugar issues choose water over sweetened beverages to further support their dietary goals.
Step-by-Step Guide to Implementing the Plate Method
- Visualize Your Plate: Begin by conceptualizing your plate as divided into three distinct sections: half designated for non-starchy vegetables, a quarter for lean protein, and a quarter for carbohydrates. The ada plate method aids in maintaining balanced nutrition and portion control, which are essential for managing diabetes.
- Choose Your Vegetables: Fill the larger half of your plate with a diverse array of non-starchy vegetables, including options such as leafy greens, broccoli, and bell peppers. Opting for colorful varieties not only enhances visual appeal but also maximizes nutrient intake, which is crucial for overall health.
- Select Lean Proteins: For the quarter allocated to protein, select lean sources such as grilled chicken, fish, tofu, or legumes. Aim for a serving size of approximately 3-4 ounces to ensure you meet protein needs without excess calories.
- Add Carbohydrates: In the remaining quarter of your plate, incorporate healthy carbohydrates like whole grains or starchy vegetables such as brown rice, quinoa, or sweet potatoes. The typical carbohydrate needs per sitting are approximately 45-60 grams for women and 60-75 grams for men, based on personal energy requirements. It is essential to keep portion sizes in check to maintain stable blood glucose levels.
- Incorporate Healthy Fats: Consider adding a small amount of healthy fats, such as olive oil or avocado, which can enhance flavor and promote satiety. Portion control is vital; for instance, two tablespoons of olive oil is approximately the size of a shot glass, as noted by portion control expert Dr. Lisa Young.
- Monitor Portions: Initially, utilize measuring cups or a food scale to accurately gauge portion sizes. This practice, utilizing the ada plate method, will help you develop the skill of estimating portions visually over time, which is beneficial for effective management of blood sugar.
- Timing of Insulin and Meals: Remember that the timing of insulin administration in relation to meals is critical to prevent hypoglycemia. Aligning insulin action with postprandial glucose peaks is essential for effective blood sugar management.
- Advocacy for Portion Size Reduction: It is also important to consider broader public health efforts, such as the advocacy for portion size reduction in the food industry. This initiative aims to promote healthier eating habits and support management of blood sugar levels through improved portion control.
Choosing the Right Foods: Carbohydrates, Proteins, and Vegetables
When selecting foods for the ADA plate method, it is crucial to focus on the following components:
-
Carbohydrates: Prioritize whole grains such as brown rice, quinoa, and whole grain bread due to their lower glycemic index compared to refined grains. This difference is significant as those who consume whole grains tend to exhibit improved blood sugar control, as noted by Kelly LeBlanc, nutrition director at Oldways, who states,
Those who consumed whole grains, rather than the refined grains, had better blood sugar control, which was measured by insulin sensitivity and secretion following meals.
Recent research, including a study by Zhang (2012), highlights that carbohydrate intake in the highest quartile was associated with a combined hazard ratio of 3.34, emphasizing the importance of choosing quality carbohydrates for diabetes management.
Additionally, starchy vegetables like sweet potatoes and corn can be included but should be consumed in moderation to manage portion sizes effectively.
-
Proteins: Lean protein sources, such as skinless poultry, fish, legumes, and low-fat dairy, are recommended. These options not only provide essential nutrients but also limit excessive saturated fat intake, which is vital for overall health. Incorporating these proteins can enhance satisfaction while supporting better glycemic control.
-
Vegetables: Emphasizing non-starchy vegetables like leafy greens, broccoli, peppers, and zucchini is essential. These foods are low in calories yet high in fiber, making them ideal choices for filling half of your plate while supporting diabetes management. Utilizing tools and resources from Diabetes Canada can help individuals understand the glycemic index and make informed choices that align with the ADA plate method.
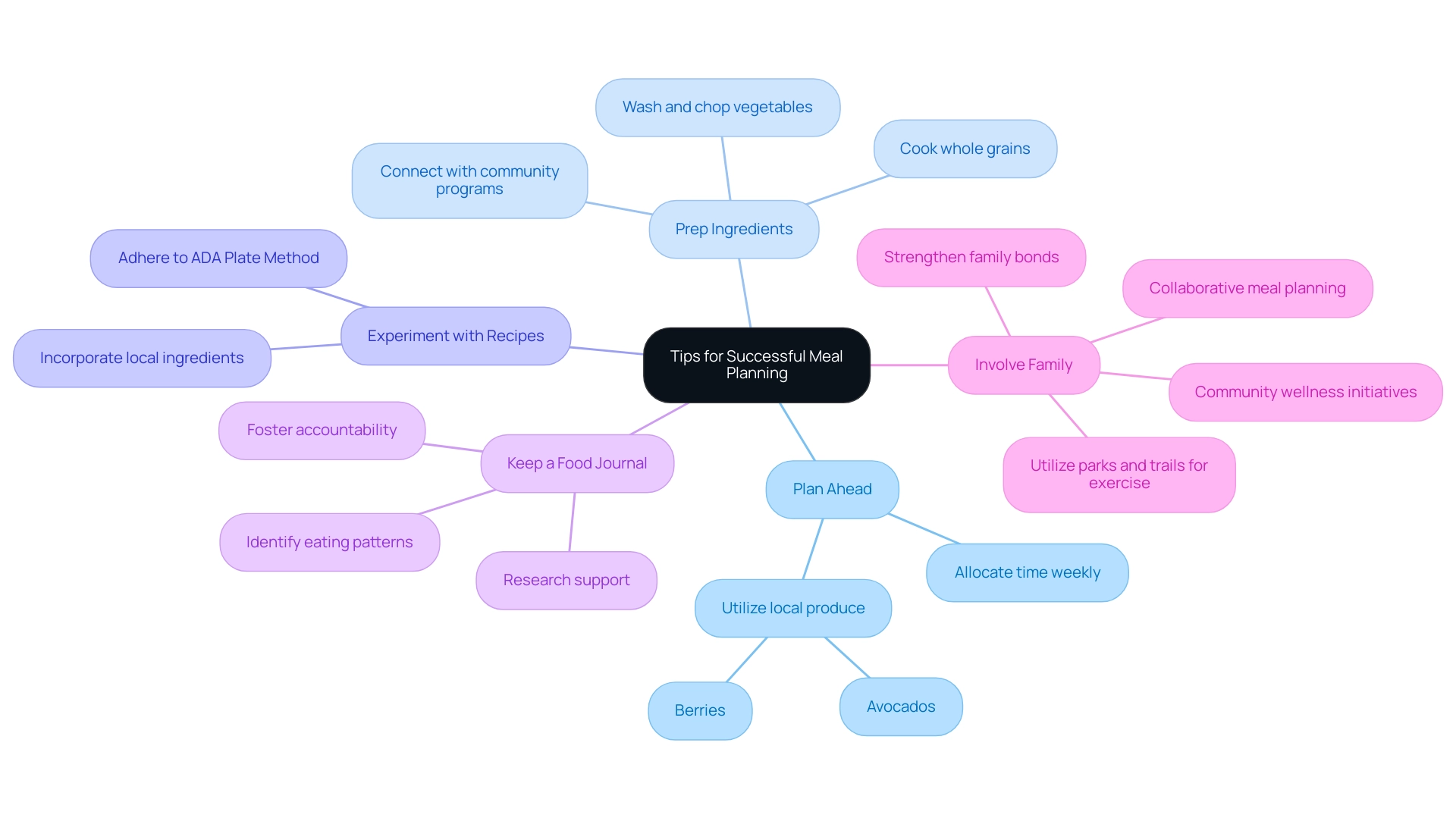
Tips for Successful Meal Planning with the Plate Method
- Plan Ahead: Allocate dedicated time each week for planning meals and snacks. This proactive approach helps prevent last-minute decisions that often lead to unhealthy choices, ensuring a well-rounded diet that adheres to the ADA guidelines. Organized food planning can result in enhanced nutritional scores, with research showing an average overall nutritional score of 63 points in control groups of recent studies. Embracing local produce, such as avocados and berries, can further enrich your planning, reflecting the vibrant food culture in San Marcos, CA.
- Prep Ingredients: Take the time to prepare ingredients in advance, such as washing and chopping vegetables or cooking whole grains. This not only streamlines the food assembly process but also encourages healthier eating by reducing the temptation to opt for processed foods. The benefits of such preparation were highlighted in a case study titled “Statistical Analysis of Outcomes,” which evaluated dietary interventions in managing diabetes. Connecting this to local community programs can enhance the effectiveness of these strategies.
- Experiment with a variety of recipes that adhere to the ADA Plate Method. This variety keeps dishes exciting and enjoyable, which is crucial for maintaining adherence to dietary recommendations over time. Incorporating different recipes can enhance the overall dietary experience and improve health outcomes, especially when they utilize local ingredients from farmers’ markets.
- Keep a Food Journal: Regularly monitor your foods and snacks in a food journal. This practice allows you to identify eating patterns, make necessary adjustments, and foster accountability in your dietary choices. Research indicates that individuals who engage in food journaling are more successful in managing their condition, aligning with the improvements noted after dietary interventions in clinical studies.
- Involve Family: Encourage family members to participate in meal planning and preparation. This collaborative effort not only strengthens family bonds but also reinforces healthy eating habits, creating an environment conducive to effective health management. Additionally, make sure to embrace the outdoor lifestyle by utilizing the parks and trails in San Marcos for regular exercise, which can significantly benefit your health. Community wellness initiatives in San Marcos can offer additional assistance, emphasizing the importance of a life course, contextual, and food agency-based strategy for future diabetes prevention efforts. Consider visiting local farmers’ markets for fresh produce, which can further enhance your nutrition and support local agriculture.
Overcoming Challenges in Adopting the Plate Method
-
Lack of Variety: Boredom with food can lead to unhealthy choices. To combat this, experiment with diverse recipes or cooking techniques, such as grilling, steaming, or slow cooking, to maintain excitement in your meal planning. Embracing variety not only satisfies taste preferences but also ensures a balanced intake of nutrients, which is crucial for addressing the underlying factors of this condition. By re-evaluating the origin of your condition, you can customize these options to better suit your wellness requirements.
-
Time Constraints: Busy schedules can hinder healthy eating. To alleviate this challenge, consider batch cooking or food prepping on less hectic days. By preparing several servings of food ahead of time, you can easily oversee your nutrition throughout the week without the pressure of everyday cooking, enabling you to concentrate on a comprehensive strategy for managing your condition that considers your individual wellness needs.
-
Social Situations: Navigating dining out or social gatherings can be tricky. To make informed choices, review the menu beforehand and select options that are in accordance with the ADA Plate Method. Planning your meals in advance helps in making healthier choices while allowing you to enjoy social interactions without compromising your dietary goals, further empowering your health and reducing anxiety related to potential complications.
-
Emotional Eating: Identifying triggers that result in emotional eating is essential for managing blood sugar levels. Developing coping strategies, such as mindfulness practices, can aid in navigating these challenges. Interacting with healthcare experts for advice can also offer extra assistance. As one participant poignantly expressed,
I’m not going to walk around starving myself…my mother, she’s a diabetic…she went into bad health because she didn’t eat enough…
This highlights the importance of balanced eating to avoid negative health outcomes, a fundamental aspect of a holistic management strategy that addresses both emotional and physical health.
-
Assistance Network: Establishing a robust assistance network is crucial in managing diabetes. Participating in community groups or assistance networks can promote shared experiences and mutual encouragement. Research indicates that family assistance plays a critical role in dietary management. Participants in a qualitative study noted that family members often assist with meal preparation, significantly contributing to better health outcomes and adherence to dietary recommendations. Significantly, 16% of participants were uninsured, which can affect access to resources and assistance. Insights from Jager MJ et al.’s study on ethnic minority patients with blood sugar issues emphasizes the need for culturally sensitive dietary management, highlighting the importance of family involvement as shown in the case study titled ‘Family Support in Dietary Management of Diabetes.’ This comprehensive approach not only addresses the individual’s dietary needs but also empowers them through community and familial support, ultimately contributing to a holistic regimen that can alleviate anxiety surrounding diabetes complications.
Conclusion
The ADA Plate Method serves as a valuable framework for individuals managing diabetes, offering a structured approach to meal planning that emphasizes balance and portion control. By visually dividing the plate into sections for non-starchy vegetables, lean proteins, and carbohydrates, this method simplifies meal construction while promoting stable blood sugar levels. The evidence supporting its effectiveness underscores the importance of this visual tool, with studies demonstrating significant improvements in glycemic control among those who adhere to the method.
Implementing the ADA Plate Method involves practical steps that can enhance dietary adherence:
- Selecting the right foods
- Preparing meals in advance
Individuals can create a sustainable eating plan that aligns with their health goals. Additionally, overcoming common challenges such as lack of variety and time constraints can be addressed through proactive strategies, ensuring that meal planning remains enjoyable and manageable.
Ultimately, adopting the ADA Plate Method empowers individuals with diabetes to take control of their dietary choices. By prioritizing balanced nutrition and engaging in thoughtful meal planning, the path towards improved health and quality of life becomes more attainable. This method not only aids in diabetes management but also fosters a holistic approach to well-being, encouraging individuals to make informed decisions that will benefit their overall health.
Frequently Asked Questions
What is the ADA Plate Method?
The ADA Plate Method is a visual aid designed to help individuals with blood sugar issues create balanced meals that support stable glucose levels. It emphasizes portion control and the inclusion of diverse food groups.
How should I divide my plate using the ADA Plate Method?
According to the ADA Plate Method, you should fill half of your plate with non-starchy vegetables, one-quarter with lean proteins, and one-quarter with carefully chosen carbohydrates.
What types of vegetables should I include in my meals?
You should fill the larger half of your plate with a variety of non-starchy vegetables, such as leafy greens, broccoli, and bell peppers. Choosing colorful options can enhance nutrient intake.
What are some examples of lean proteins to include?
For the quarter of your plate allocated to protein, you can choose lean sources such as grilled chicken, fish, tofu, or legumes, aiming for a serving size of approximately 3-4 ounces.
What carbohydrates should I add to my plate?
In the remaining quarter of your plate, incorporate healthy carbohydrates like whole grains (e.g., brown rice, quinoa) or starchy vegetables (e.g., sweet potatoes). Typical carbohydrate needs per sitting are about 45-60 grams for women and 60-75 grams for men.
Can I include fats in my meals, and if so, how much?
Yes, you can add a small amount of healthy fats, such as olive oil or avocado, to enhance flavor and promote satiety. For instance, two tablespoons of olive oil is approximately the size of a shot glass.
How can I monitor my portion sizes effectively?
Initially, you can use measuring cups or a food scale to accurately gauge portion sizes. Over time, this practice will help you develop the skill of estimating portions visually.
Why is the timing of insulin administration important?
The timing of insulin relative to meals is crucial to prevent hypoglycemia. Aligning insulin action with postprandial glucose peaks is essential for effective blood sugar management.
What is the significance of portion size reduction advocacy?
Advocating for portion size reduction in the food industry aims to promote healthier eating habits and support blood sugar management through improved portion control.