Overview
The article titled “7 Side Effects of Diabetes Type 2 You Need to Manage” sheds light on the significant health challenges that come with type 2 diabetes. These include:
- Neuropathy
- Cardiovascular disease
- Vision impairment
- Foot ulcers
- Fatigue
- An increased risk of stroke
It’s important to recognize that these concerns can feel overwhelming, but there is hope.
Many patients find that proactive management strategies can make a meaningful difference. Maintaining stable glucose levels is crucial, and adopting a heart-healthy lifestyle can further support your well-being. Engaging in regular check-ups not only helps in monitoring your health but also provides an opportunity to discuss any concerns you may have.
By taking these steps, you can mitigate these side effects and enhance your overall quality of life. Remember, you are not alone in this journey, and there are resources available, such as the 30-Day Diabetes Reset program, to help you thrive.
Introduction
Managing type 2 diabetes involves navigating complexities that go well beyond just controlling blood sugar levels. Many individuals encounter a range of side effects that can significantly affect their quality of life. From neuropathy and cardiovascular disease to vision impairment and fatigue, these challenges can feel overwhelming.
It’s important to recognize that proactive management strategies are essential in mitigating these effects. In this article, we will explore seven critical side effects of type 2 diabetes, offering insights and practical tips for effective management.
How can you navigate these challenges and reclaim your health in the ongoing battle with diabetes? Together, we can find a path forward.
Integrative Wellness Center: 30-Day Diabetes Reset Program for Effective Management
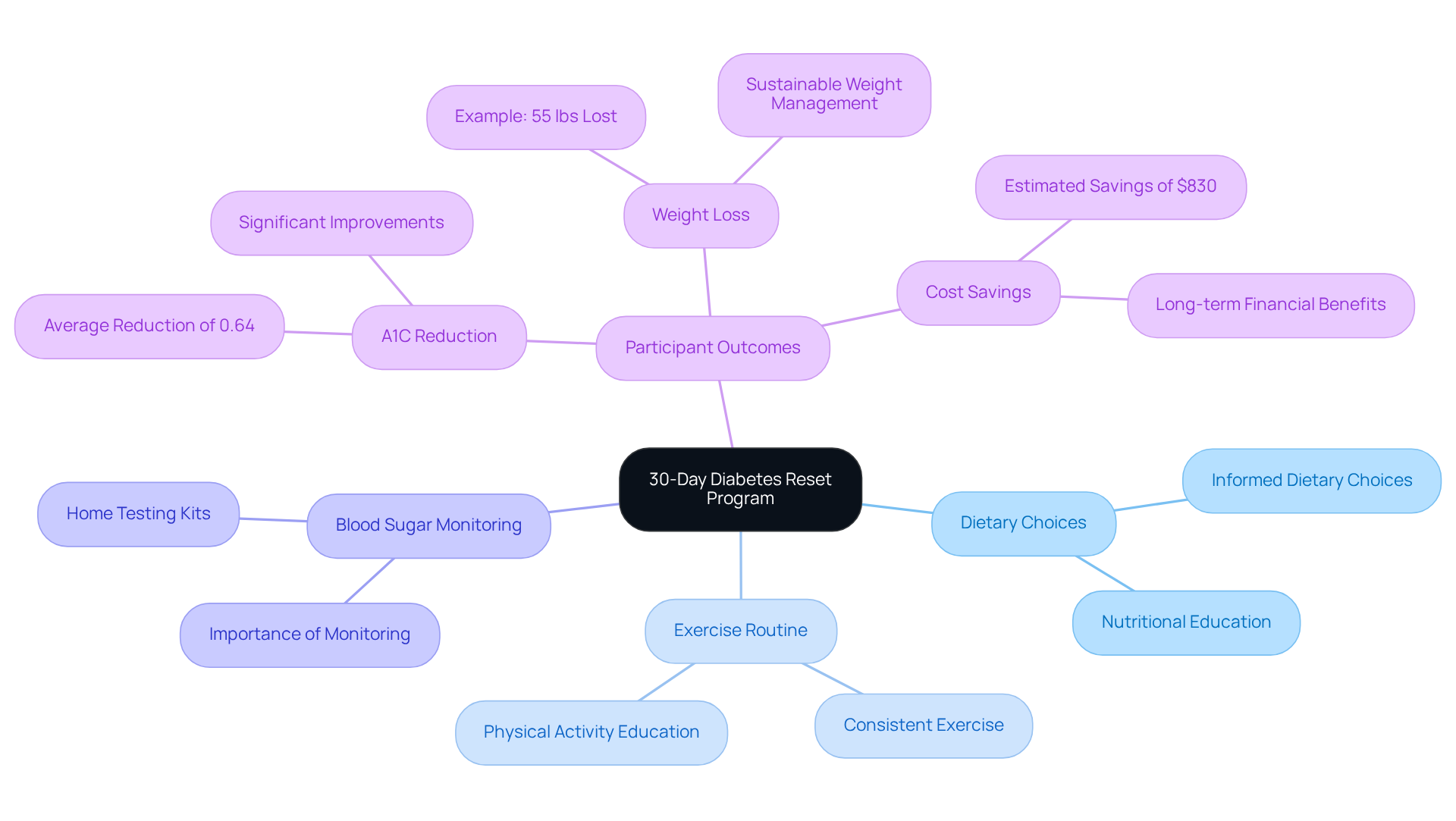
Are you finding it difficult to manage the side effects of diabetes type 2? The 30-Day Diabetes Reset Program at the Integrative Wellness Center offers a compassionate and comprehensive approach to help you regain control of your health. This program equips you with the essential tools and knowledge to stabilize your glucose readings and reduce reliance on medications. By focusing on nutrition, physical activity, and behavior modification, participants learn to:
- Make informed dietary choices
- Develop a consistent exercise routine
- Understand the importance of monitoring their blood sugar
Imagine feeling empowered on your health journey. With educational resources like engaging seminars and Dr. Jason Shumard’s insightful books, you’ll find the support needed to take charge of your well-being. Many participants have shared their transformative experiences, showcasing the program’s profound impact. One participant lost 55 lbs and improved their A1C levels from 9.1 to 5.7 in just eight months. Another, who had battled diabetes for fourteen years, felt revitalized and no longer needed medications after participating. These stories highlight the program’s effectiveness in promoting sustainable wellness improvements.
It’s important to recognize that participants in diabetes self-management education (DSME) interventions have shown an average A1C reduction of 0.64%, which is crucial in mitigating the side effects of diabetes type 2. This illustrates the program’s success in fostering stable glucose levels and renewed energy. Additionally, the program can lead to significant cost savings, with an estimated mean savings of $830 per participant in the first year. This comprehensive approach not only addresses urgent wellness concerns but also encourages long-term lifestyle modifications that enhance overall well-being, particularly for older adults who often experience greater decreases in A1C values.
Are you ready to transform your health? To learn more about how the 30-Day Diabetes Reset Program can support you, register now!
Neuropathy: Understanding Nerve Damage Associated with Diabetes
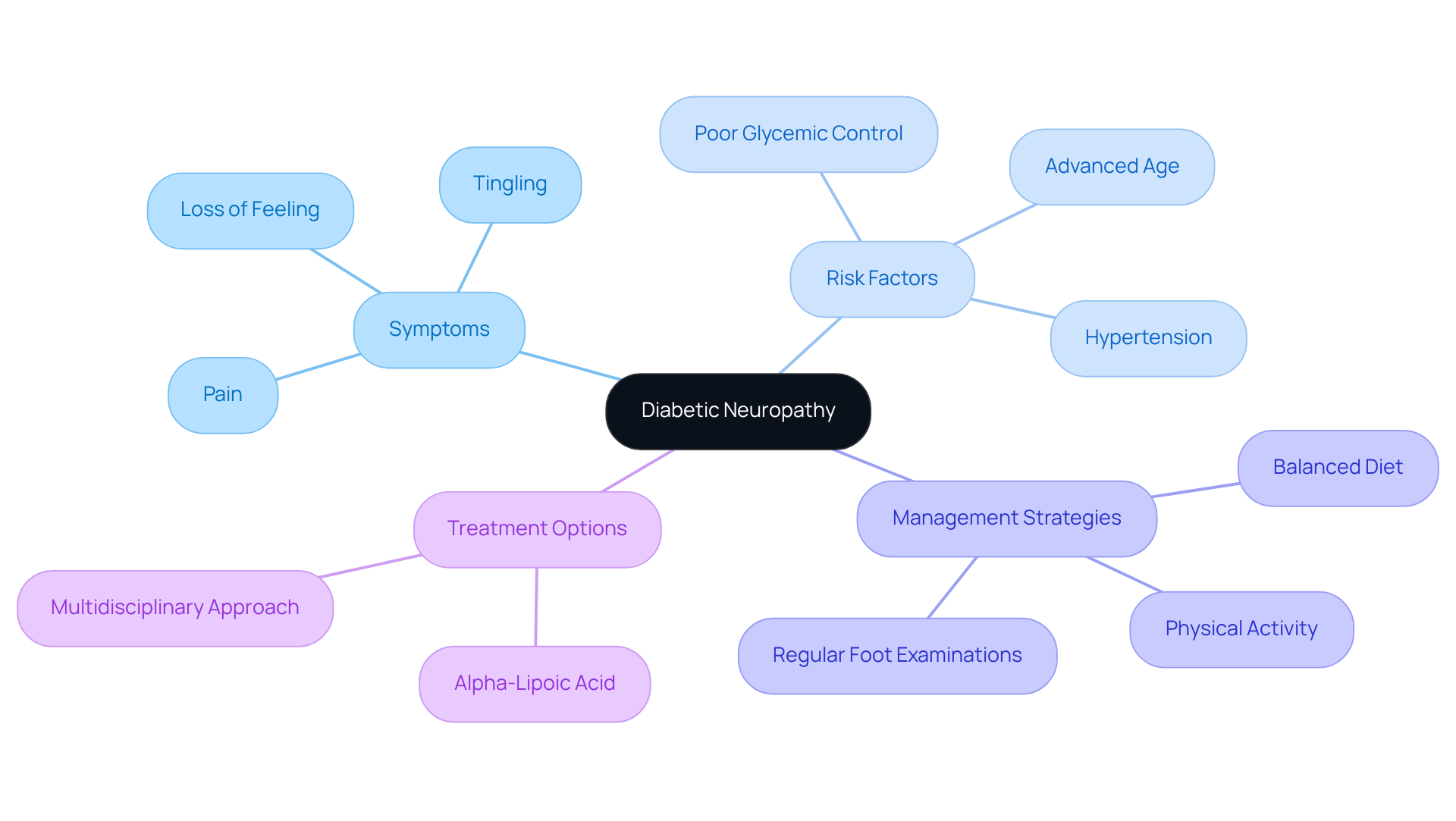
Diabetic neuropathy is one of the side effects of diabetes type 2, and it is a significant concern for many living with the condition, often presenting as pain, tingling, or loss of feeling, particularly in the extremities. Did you know that this condition affects up to 50% of individuals who experience the side effects of diabetes type 2? This statistic underscores the critical need for effective management strategies. It’s important to recognize that maintaining optimal glucose levels is essential in preventing or slowing the progression of neuropathy, which is one of the side effects of diabetes type 2. Research shows that poor glycemic control, advanced age, and hypertension are key risk factors for severe neuropathy symptoms, which are among the side effects of diabetes type 2.
To mitigate these risks, patients should prioritize:
- Regular foot examinations
- Adhering to a balanced diet
- Engaging in consistent physical activity
These lifestyle modifications not only support overall health but also play a crucial role in protecting nerve health. Many patients find that promptly reporting any symptoms to their healthcare providers can facilitate timely exploration of treatment options and lifestyle adjustments that may alleviate discomfort.
Recent advancements in treatment options for diabetic neuropathy include the use of alpha-lipoic acid, which has shown promise in improving neuropathic symptoms. Additionally, healthcare professionals emphasize the importance of a multidisciplinary approach, combining medication, physical therapy, and patient education to enhance outcomes. As our understanding of diabetic neuropathy evolves, ongoing research continues to uncover new strategies for effective management, reinforcing the significance of proactive blood sugar control in preventing nerve damage and mitigating the side effects of diabetes type 2. Remember, you are not alone in this journey, and taking these steps can make a meaningful difference in your health.
Cardiovascular Disease: Risks and Prevention Strategies for Diabetic Patients
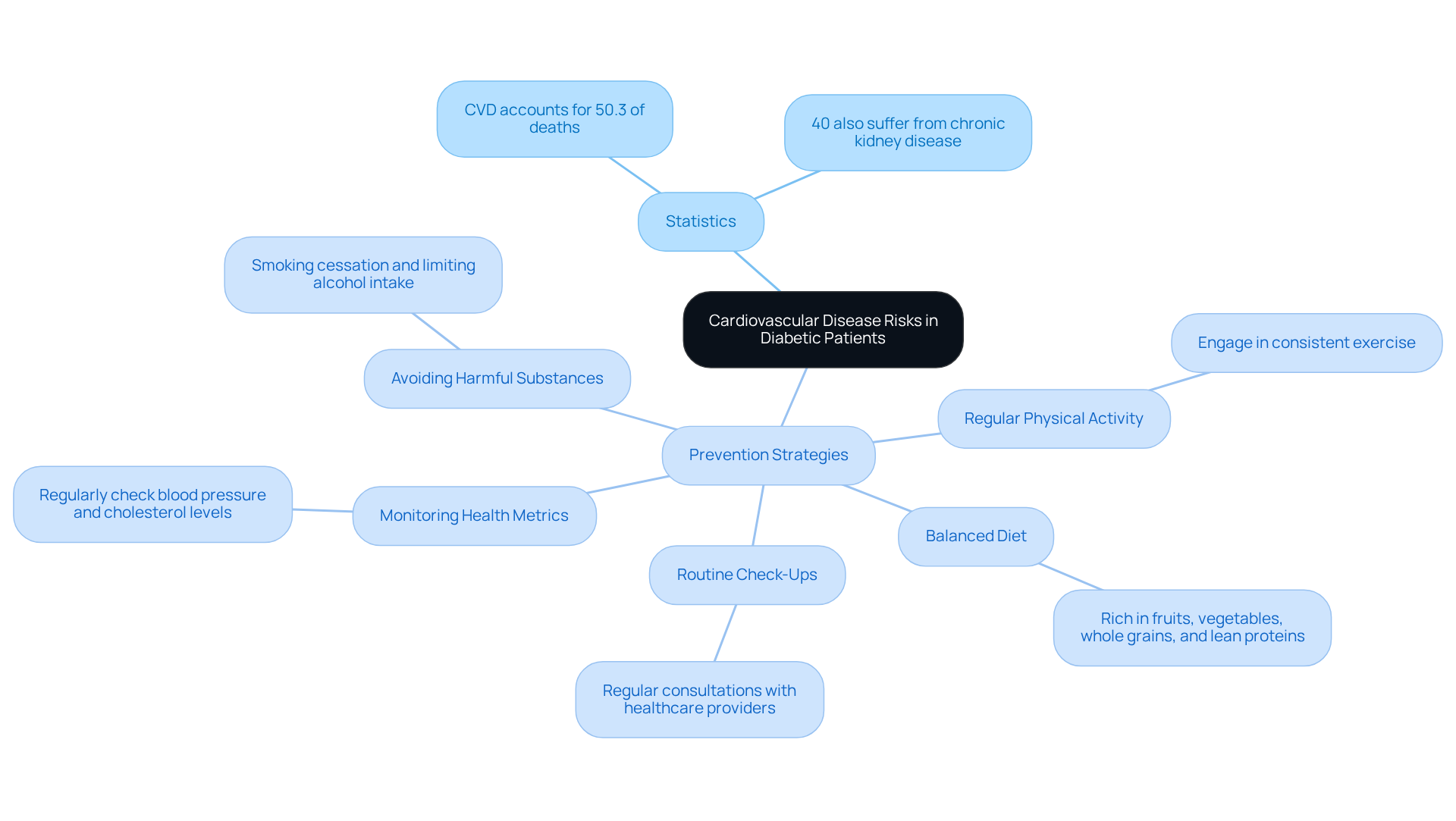
Individuals with type 2 sugar intolerance often grapple with significant health challenges, including an elevated risk of cardiovascular diseases like heart attacks and strokes. It’s important to recognize that cardiovascular disease (CVD) accounts for approximately 50.3% of all deaths in patients with diabetes. This statistic underscores the urgency of effective management strategies. To help mitigate this risk, adopting a heart-healthy lifestyle is essential. Here are some key components to consider:
- Regular Physical Activity: Engaging in consistent exercise can improve cardiovascular health and aid in weight management. Have you found activities that you enjoy?
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins is vital. This approach not only promotes general well-being but also helps in controlling sugar concentrations. What are some of your favorite healthy meals?
- Monitoring Health Metrics: Regularly checking blood pressure and cholesterol levels is crucial, as hypertension and dyslipidemia are common among diabetic patients. Many patients find that keeping track of these metrics provides peace of mind.
- Avoiding Harmful Substances: Smoking cessation and limiting alcohol intake are critical steps in reducing cardiovascular risk. Remember, every small step counts.
- Routine Check-Ups: Regular consultations with healthcare providers facilitate early detection of potential issues and allow for timely interventions. Have you scheduled your next appointment?
Recent statistics indicate that almost 40% of people with this condition also suffer from chronic kidney disease, further complicating cardiovascular well-being. Therefore, implementing these heart-healthy strategies is not just beneficial but necessary for improving quality of life and reducing the risk of serious complications. Remember, you are not alone in this journey, and taking proactive steps can lead to a healthier future.
Vision Impairment: Protecting Your Sight from Diabetes-Related Damage
The side effects of diabetes type 2 can lead to severe eye conditions, particularly diabetic retinopathy (DR), which is a leading cause of vision loss among adults. It’s important to recognize that in 2021, around 9.6 million individuals in the U.S. were living with DR, with a prevalence rate of 26.43% among those with blood sugar issues. Furthermore, 1.84 million faced vision-threatening types of the disease. Regular eye examinations are crucial for early detection and timely intervention, as the early stages of DR often present no symptoms. Many patients find that ophthalmologists recommend undergoing dilated eye exams at least once a year to monitor eye health effectively. Early detection through these exams can prevent serious complications.
Controlling glucose concentrations is vital to avoiding the side effects of diabetes type 2, particularly concerning eye issues. Elevated glucose levels can harm the fragile vessels in the retina, which can be considered as some of the side effects of diabetes type 2, leading to conditions like diabetic macular edema and proliferative diabetic retinopathy. Managing glucose levels can sometimes enhance eyesight by allowing the lens to revert to its initial form. By making changes in lifestyle, such as:
- Maintaining a nutritious diet rich in local produce
- Participating in consistent outdoor exercise in San Marcos
- Avoiding smoking
- Managing blood pressure and cholesterol levels
Individuals can significantly lower the likelihood of the side effects of diabetes type 2. Additionally, protective measures like wearing sunglasses to shield against harmful UV rays can further safeguard vision.
To effectively monitor and enhance progress in managing their condition, individuals are encouraged to utilize various tracking methods, including:
- Fitness apps
- Journals
- Pedometers
Implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly boost focus and motivation. For instance, consider setting a target to maintain blood sugar levels within a specific range or to engage in a certain amount of physical activity each week. Recent studies have highlighted the effectiveness of interventions like laser therapy and intravitreal injections in managing advanced stages of diabetic eye disease. Most treatments for DR aim to prevent further vision loss, although they do not restore lost vision. Thus, proactive management of the condition, including tailored advice from healthcare experts like Dr. Jason Shumard, and consistent eye care are essential for maintaining vision and improving the quality of life for those affected. Engaging with community wellness programs can also provide invaluable support, helping individuals integrate healthy habits into their daily lives.
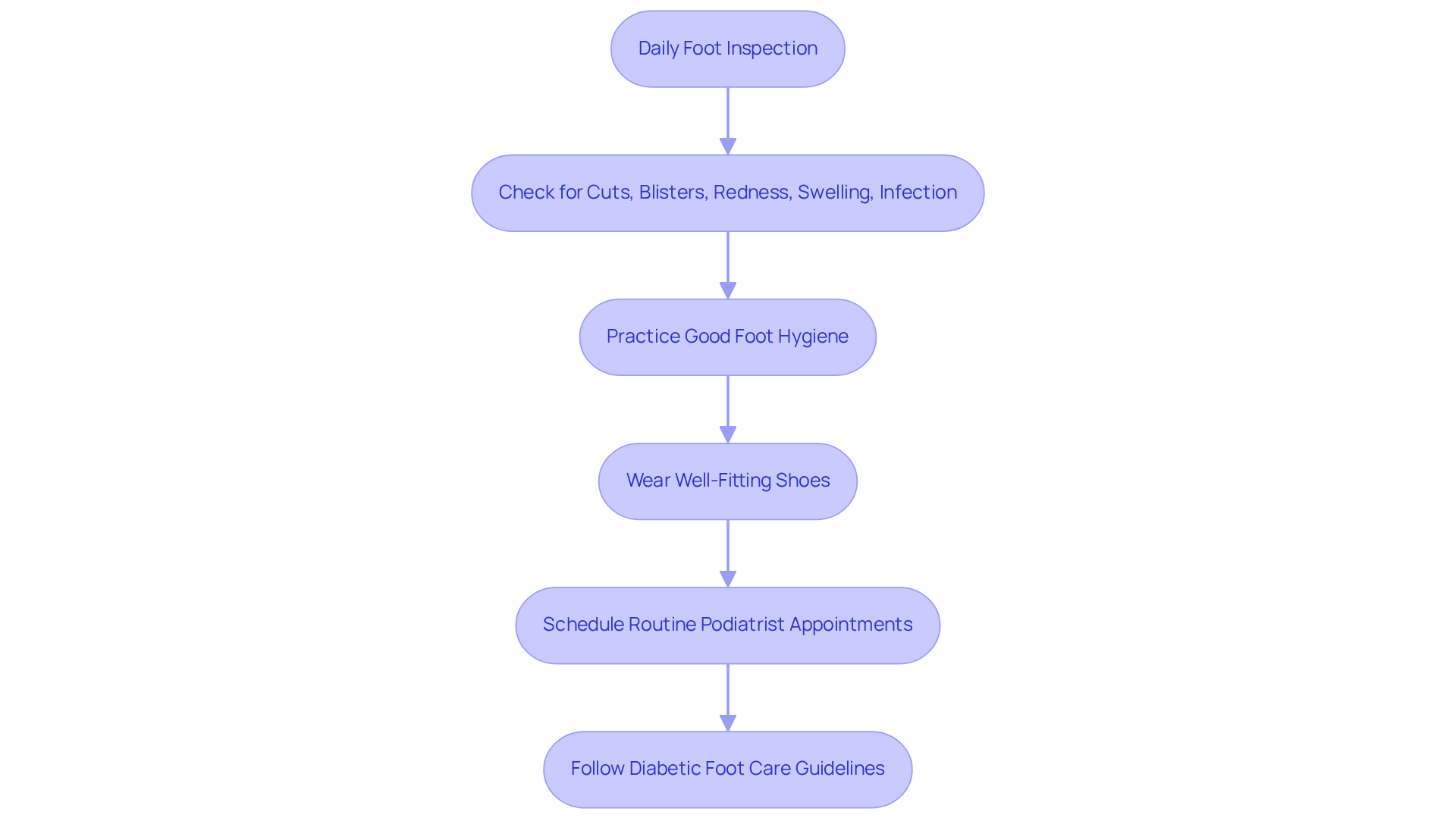
Foot Ulcers: Prevention and Care for Diabetic Foot Health
Foot ulcers can be a significant concern for those managing high blood sugar levels, often stemming from neuropathy and impaired circulation, which are common side effects of diabetes type 2. It’s important to recognize that daily foot inspections are crucial. Patients should take a moment each day to check for:
- Cuts
- Blisters
- Redness
- Swelling
- Any signs of infection
Wearing well-fitting shoes and practicing good foot hygiene—like washing and moisturizing—are essential steps in prevention.
Many patients find that routine appointments with a podiatrist are vital for maintaining foot health. These visits allow for early identification and intervention of potential issues, preventing them from escalating into serious complications. With around 50% of individuals with blood sugar challenges experiencing some form of nerve damage, proactive foot care becomes even more critical. By following the latest guidelines for diabetic foot care, including daily temperature checks and choosing the right footwear, you can significantly enhance your foot health and reduce the risk of severe complications that are among the side effects of diabetes type 2, such as amputation.
Remember, taking these steps not only helps in managing your condition but also supports your overall well-being. You deserve to feel confident and secure in your health journey.
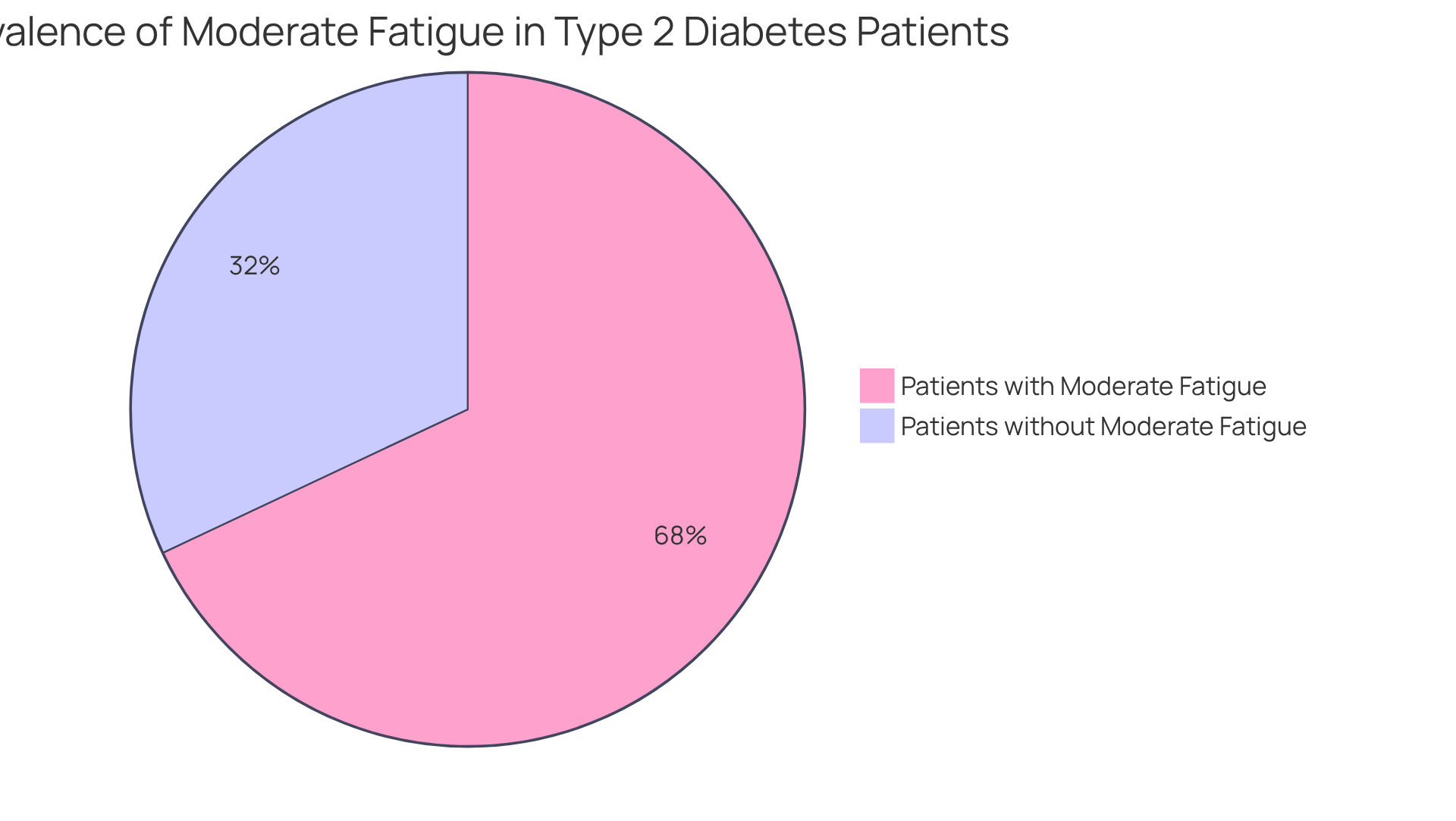
Fatigue: Managing Energy Levels When Living with Diabetes
Fatigue is a common and concerning issue for many living with type 2 diabetes, and it is one of the side effects of diabetes type 2 that is often exacerbated by fluctuations in glucose levels. Did you know that research shows 68% of diabetes patients experience moderate fatigue? This can significantly impact daily activities. To help regulate energy levels, it’s crucial for patients to maintain stable glucose through balanced meals rich in whole grains, lean proteins, and healthy fats, complemented by regular physical activity. Many find that taking short breaks throughout the day can alleviate feelings of exhaustion. Additionally, ensuring 7 to 9 hours of quality sleep is vital for recovery and restoring energy.
It’s important to recognize that incorporating stress management techniques, such as mindfulness practices and relaxation exercises, can further enhance overall well-being and energy. Endocrinologists highlight the significance of monitoring blood glucose levels, as both hypo- and hyperglycemia are important side effects of diabetes type 2 that contribute to fatigue. Successful energy management strategies also include building a supportive social network. This connection has been shown to reduce feelings of fatigue and improve mental health outcomes. By embracing these strategies, individuals with type 2 diabetes can reclaim their energy and enhance their quality of life.
Stroke: Understanding the Increased Risk for Individuals with Diabetes
Individuals with type 2 diabetes face a significantly increased risk of stroke, which is one of the side effects of diabetes type 2, largely due to related conditions such as high blood pressure and elevated cholesterol levels. It’s concerning to note that around 28% of stroke patients have diabetes, and the risk of ischemic stroke rises by 3% for each year living with diabetes. To effectively address this risk, embracing a healthy lifestyle is essential. This means:
- Engaging in regular physical activity—aiming for at least 150 minutes each week
- Maintaining a balanced diet rich in fruits, vegetables, whole grains, and lean proteins
- Being mindful of sodium intake to help manage blood pressure
Regular check-ups are crucial for the early detection and management of hypertension and cholesterol levels.
It’s important to recognize that managing stress and avoiding tobacco use are also vital components of stroke prevention. Many healthcare professionals emphasize that lifestyle changes can significantly lower stroke risk. One neurologist noted, ‘Understanding and managing personal wellness conditions is essential for stroke prevention.’
Recognizing the signs of a stroke—such as sudden numbness, confusion, or difficulty speaking—is critical for prompt medical intervention, which can greatly enhance recovery outcomes. By prioritizing these lifestyle changes and staying vigilant about health, individuals can take proactive steps to reduce the side effects of diabetes type 2, such as stroke risk, and improve their overall well-being. Additionally, it’s wise to consider the potential risks associated with traditional diabetes treatments, like insulin resistance, and to explore personalized functional medicine approaches that may include tailored nutrition plans and targeted supplements for a more comprehensive management strategy.
Conclusion
Understanding and managing the side effects of type 2 diabetes is crucial for maintaining overall health and improving quality of life. It’s important to recognize that the complexities of this condition require a proactive approach. By focusing on lifestyle modifications and effective management strategies, individuals can mitigate risks and enhance their well-being.
Many patients find that regular monitoring, balanced nutrition, and consistent physical activity are key to their success. From addressing neuropathy and cardiovascular risks to preventing vision impairment and foot ulcers, each aspect underscores how interconnected these challenges are. Participants in programs like the 30-Day Diabetes Reset have shared transformative experiences that illustrate the potential for significant health improvements through informed choices and dedicated support.
Ultimately, taking charge of one’s health journey is essential for individuals living with type 2 diabetes. Embracing lifestyle changes and seeking educational resources can empower individuals to manage their condition effectively. By prioritizing health and wellness, it is possible to not only reduce the side effects of diabetes but also to foster a more vibrant and fulfilling life. Remember, you are not alone on this journey; support is available, and positive change is within reach.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at the Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a comprehensive approach designed to help individuals manage type 2 diabetes by providing tools and knowledge to stabilize glucose readings and reduce reliance on medications. It focuses on nutrition, physical activity, and behavior modification.
What are the main components of the program?
Participants in the program learn to make informed dietary choices, develop a consistent exercise routine, and understand the importance of monitoring their blood sugar.
What kind of support do participants receive during the program?
Participants receive educational resources such as engaging seminars and access to Dr. Jason Shumard’s books, which provide support and guidance for their health journey.
What success stories have emerged from the program?
Many participants have reported transformative experiences, such as one individual who lost 55 lbs and improved their A1C levels from 9.1 to 5.7 in eight months, and another who no longer needed medications after 14 years of battling diabetes.
How effective is the program in managing A1C levels?
Participants in diabetes self-management education (DSME) interventions, such as this program, have shown an average A1C reduction of 0.64%, which is significant for mitigating the side effects of diabetes type 2.
Are there any financial benefits to participating in the program?
Yes, the program can lead to significant cost savings, with an estimated mean savings of $830 per participant in the first year.
What is diabetic neuropathy and how is it related to diabetes type 2?
Diabetic neuropathy is a side effect of diabetes type 2 that presents as pain, tingling, or loss of feeling, particularly in the extremities. It affects up to 50% of individuals with diabetes and is linked to poor glycemic control, advanced age, and hypertension.
What strategies can help manage diabetic neuropathy?
To mitigate neuropathy risks, patients should prioritize regular foot examinations, adhere to a balanced diet, and engage in consistent physical activity.
What recent advancements exist in the treatment of diabetic neuropathy?
Recent advancements include the use of alpha-lipoic acid, which has shown promise in improving neuropathic symptoms, and a multidisciplinary approach that combines medication, physical therapy, and patient education.
Why is blood sugar control important for preventing nerve damage?
Proactive blood sugar control is essential in preventing or slowing the progression of neuropathy, thereby mitigating the side effects of diabetes type 2 and protecting nerve health.