Overview
This article highlights the importance of managing a fasting blood sugar level of 112 mg/dL, which signals a prediabetes condition. It’s important to recognize that this situation can be concerning, but with proactive health measures, you can prevent the onset of type 2 diabetes. Many patients find that making lifestyle changes can be empowering.
Adopting a balanced diet, increasing physical activity, and engaging in regular monitoring are essential steps. Evidence shows that these strategies can significantly lower health risks associated with elevated glucose levels.
Consider this: How might your life change if you took control of your health? Embracing these changes not only helps in managing your blood sugar but also enhances your overall well-being. As you embark on this journey, remember that you are not alone. Support is available, and small, consistent steps can lead to meaningful improvements.
Incorporating these practices into your daily routine can feel overwhelming at first, but it’s about progress, not perfection. Start with simple adjustments, like adding more fruits and vegetables to your meals or taking short walks. Each positive change contributes to a healthier you. Together, we can work towards a future free from the worries of diabetes.
Introduction
Understanding fasting blood sugar levels is crucial in today’s health landscape, especially as more individuals face the challenges of prediabetes. A fasting blood sugar measurement of 112 mg/dL can be concerning; it serves as a gentle reminder that lifestyle changes may be necessary to prevent the progression to type 2 diabetes. Many people find themselves overwhelmed by this diagnosis, and it’s important to recognize that you are not alone in this journey.
This article offers essential insights into the implications of this reading and explores effective strategies for management, highlighting the significant benefits of proactive health measures.
How can you leverage this knowledge not only to stabilize your blood sugar but also to enhance your overall well-being? Together, we can navigate these changes and foster a healthier future.
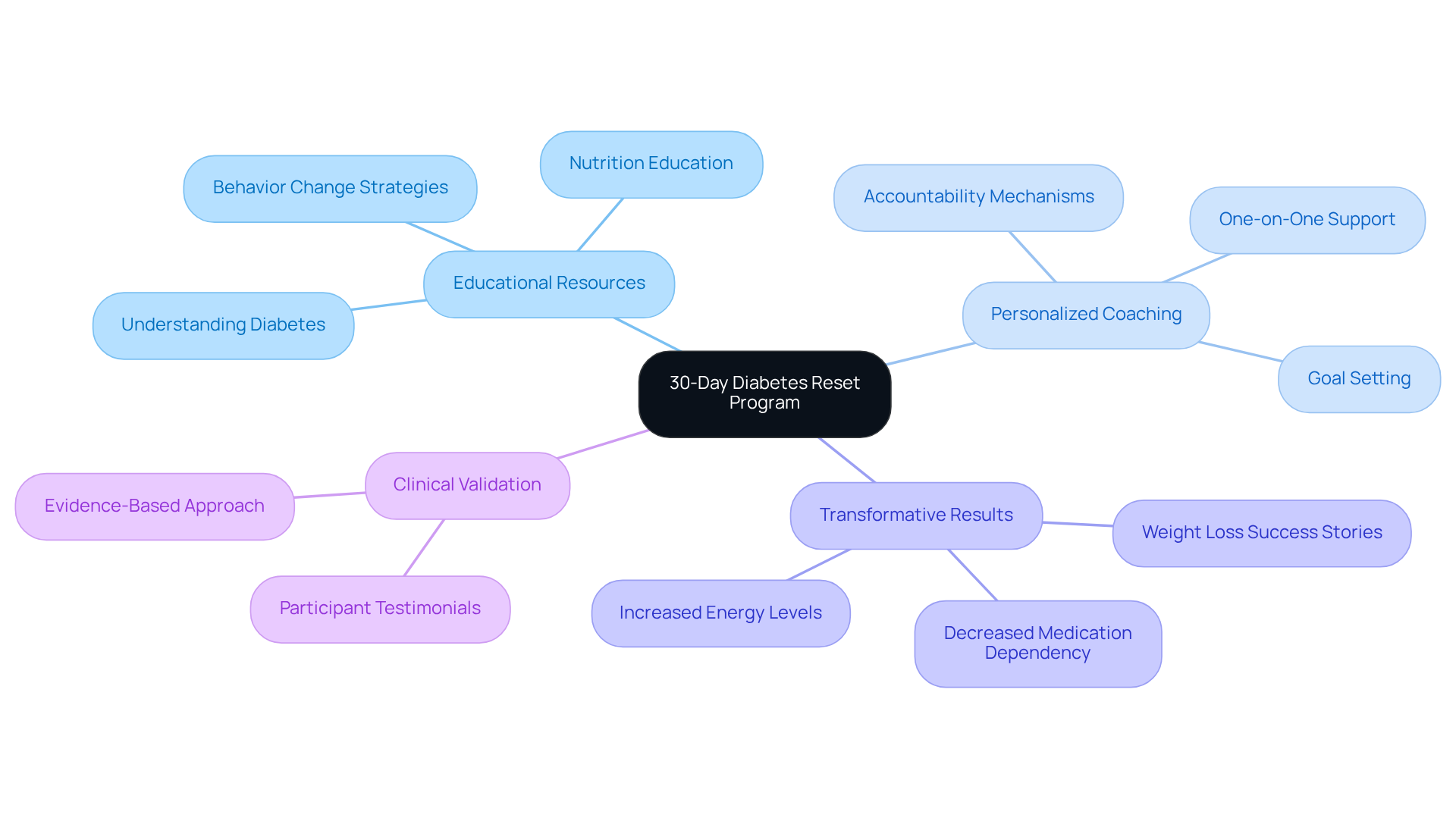
Integrative Wellness Center: 30-Day Diabetes Reset Program for Blood Sugar Management
At Dr. Jason Shumard’s Integrative Wellness Center, the 30-Day Diabetes Reset Program offers a groundbreaking, holistic approach designed to help you manage your blood sugar effectively. We understand that navigating diabetes can be challenging, and this clinically validated program combines educational resources, personalized coaching, and practical tools to empower you in understanding your condition and making sustainable lifestyle changes.
It’s important to recognize that behavior change and nutrition play crucial roles in managing diabetes. Our program equips you with the knowledge and skills necessary for long-term success. Many patients find that they experience transformative results, such as weight loss, decreased medication dependency, and increased energy. For instance, one participant shared, ‘I lost 55 lbs. My A1C started at 9.1 after 8 months; it is now 5.7.’
We believe that personalized coaching is vital for enhancing your engagement and accountability, ultimately leading to better health outcomes. This functional medicine approach positions our center as a leader in managing 112 fasting blood sugar conditions within the San Diego community. We are here to support you in reclaiming your health and overcoming the challenges of Type 2 diabetes. Together, we can navigate this journey toward a healthier, more fulfilling life.
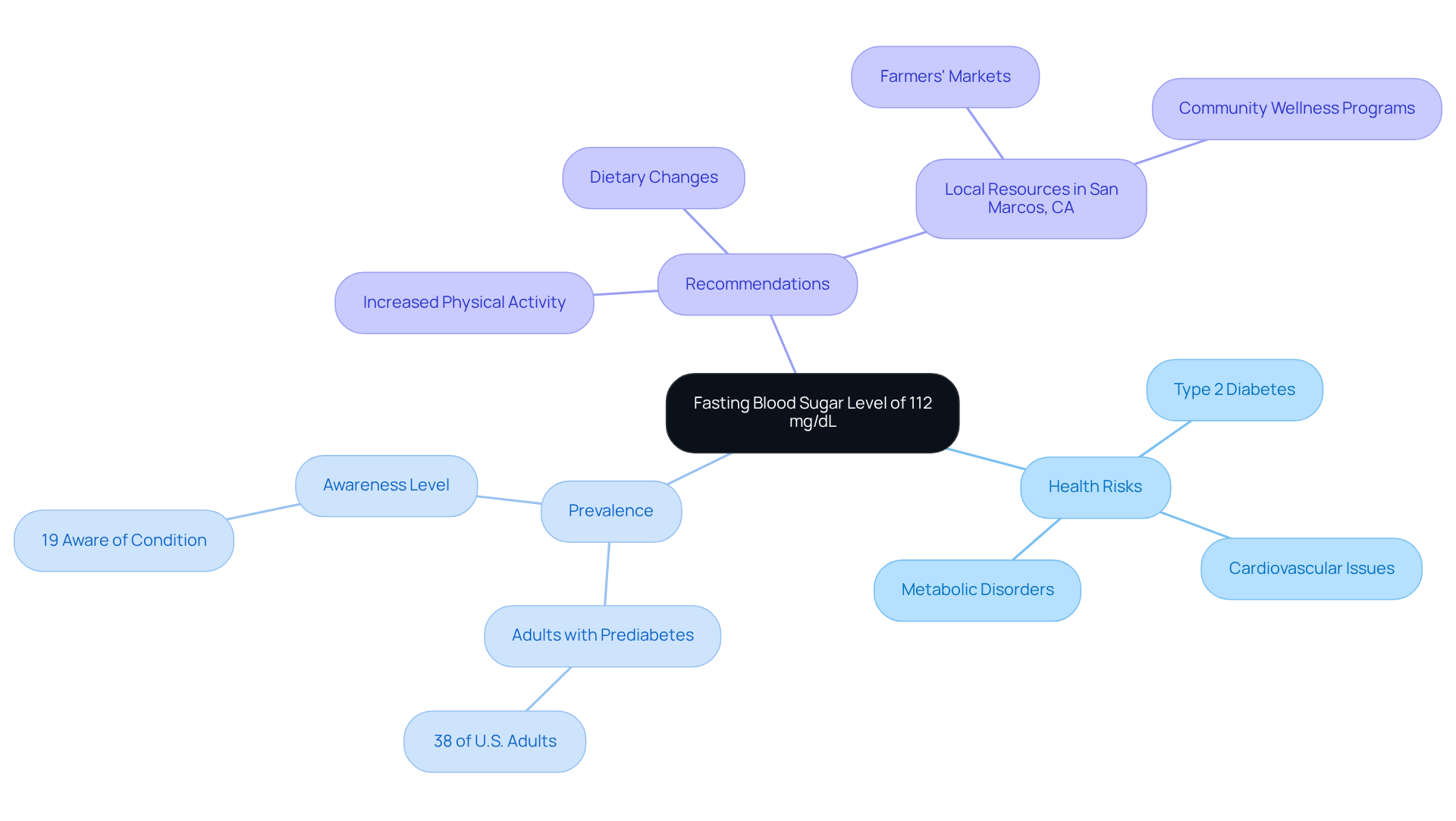
Understanding Fasting Blood Sugar: What Does a Level of 112 Indicate?
A measurement of 112 fasting blood sugar at 112 mg/dL falls within the prediabetes spectrum. This indicates that while you may not yet have been diagnosed with the condition, your glucose readings are higher than what is typically considered normal. It’s important to recognize that this stage serves as a crucial alert, signaling the need for prompt measures to prevent the onset of type 2 diabetes. Research shows that approximately 38% of U.S. adults had prediabetes as of 2021, yet many remain unaware of their condition—only 19% of those diagnosed have been informed by healthcare professionals.
Health risks associated with 112 fasting blood sugar levels include:
- An increased likelihood of developing type 2 diabetes
- Cardiovascular issues
- Other metabolic disorders
Many patients find that individuals with prediabetes often face complications such as chronic kidney disease and vision impairment. This highlights the urgency of addressing elevated glucose levels.
Endocrinologists emphasize the importance of monitoring fasting glucose measurements, noting that even slight increases can lead to serious health repercussions. They recommend lifestyle adjustments, including:
- Dietary changes
- Increased physical activity
to help lower glucose levels and reduce health risks. In San Marcos, CA, you can take a holistic approach by utilizing local resources such as farmers’ markets for fresh produce, engaging in outdoor activities at beautiful parks, and joining community wellness programs.
By taking proactive steps, including personalized advice from Dr. Jason Shumard, you can effectively manage your health and lower the chances of developing diabetes-related complications. Remember, small changes can make a significant difference in your journey toward better health.
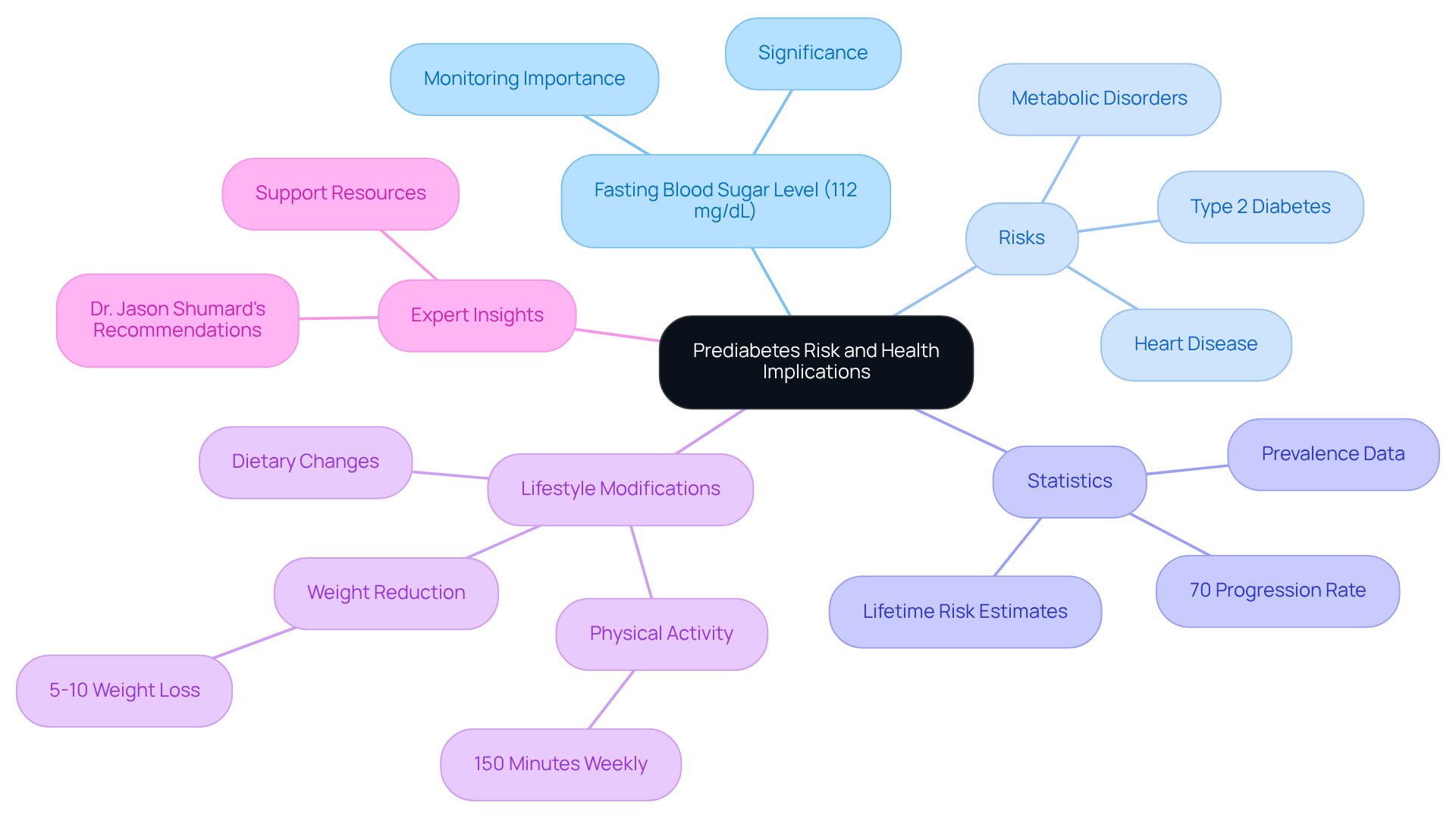
Prediabetes Risk: Health Implications of a Fasting Blood Sugar Level of 112
A 112 fasting blood sugar level of 112 mg/dL signifies a heightened risk for developing type 2 conditions, heart disease, and other metabolic disorders. It’s important to recognize that prediabetes often presents without symptoms, highlighting the necessity for regular monitoring. Many patients find that understanding their health status can be a pivotal moment in their journey. Research indicates that almost 70% of individuals with prediabetes will ultimately advance to the condition, making proactive health management crucial.
Lifestyle modifications can significantly reduce these risks. For instance, adopting a balanced diet and increasing physical activity are powerful steps toward better health. Did you know that a weight reduction of only 5-10% can result in a remarkable 58% decrease in the risk of developing type 2 diabetes? Furthermore, engaging in at least 150 minutes of moderate exercise weekly can enhance insulin sensitivity and improve overall metabolic health.
Dr. Jason Shumard, a leader in functional medicine at Integrative Wellness Center, emphasizes that effective management of blood sugar conditions involves personalized nutrition plans and lifestyle changes. By understanding the consequences of increased fasting glucose levels and adopting beneficial lifestyle modifications, individuals can make substantial progress toward achieving a 112 fasting blood sugar and better health outcomes.
For those seeking guidance, Dr. Shumard offers various resources and events designed to empower patients on their journey toward reversing diabetes and achieving holistic health. Remember, you are not alone in this journey, and there are supportive paths available to help you thrive.
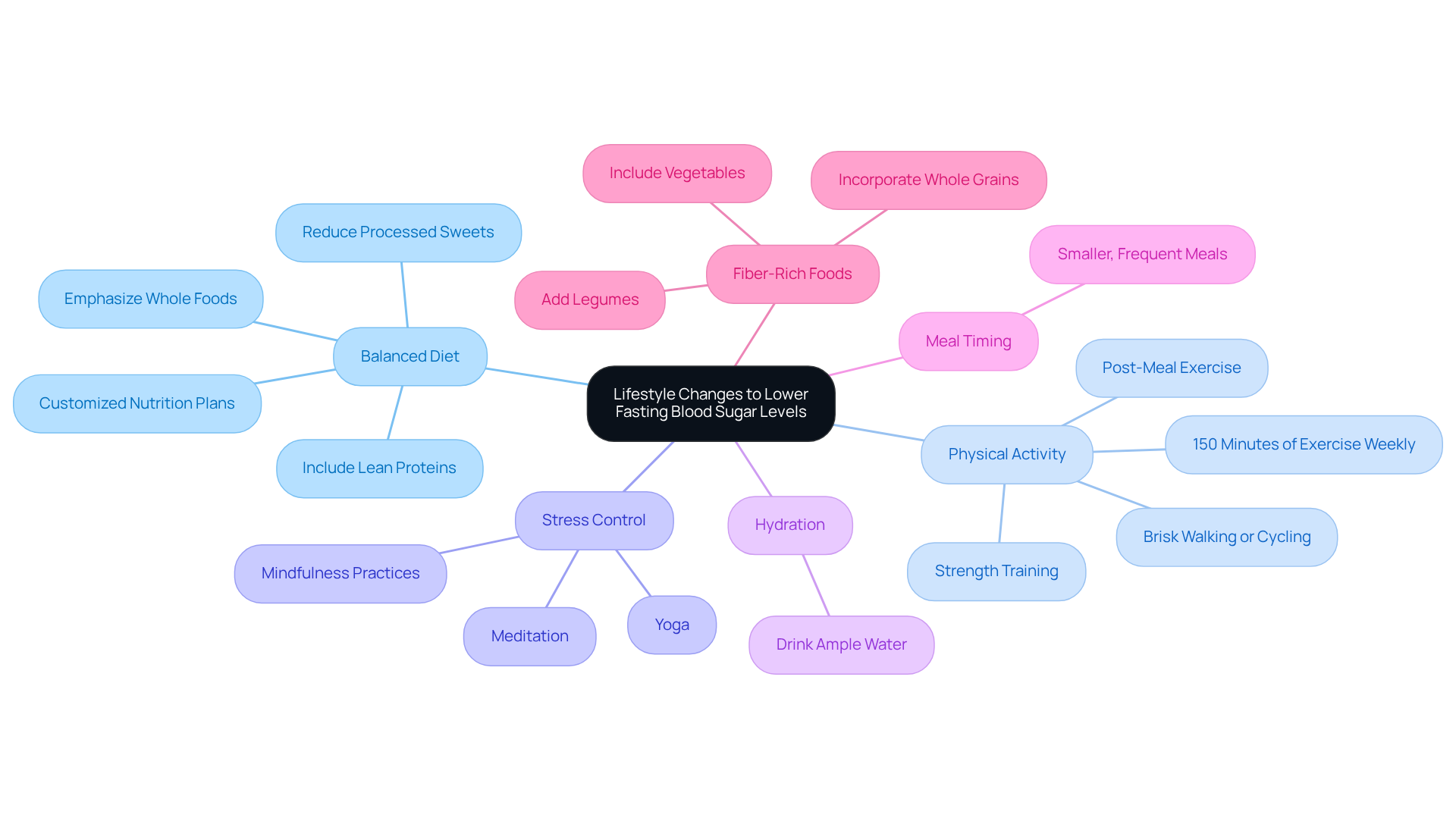
Lifestyle Changes: Effective Strategies to Lower Fasting Blood Sugar Levels
To effectively lower fasting glucose amounts, it’s important to recognize that adopting impactful lifestyle changes can make a significant difference. Here are some supportive strategies you can embrace:
-
Embrace a balanced diet that emphasizes whole foods, lean proteins, and healthy fats while reducing processed sweets and refined carbohydrates. This approach not only stabilizes glucose levels but also promotes your overall well-being. Customized nutrition plans designed for your personal needs can further enhance this journey, focusing on nutrient-rich foods that stabilize blood sugar and improve metabolic function.
-
Enhance physical activity by incorporating regular exercise, such as brisk walking, cycling, or strength training. Many patients find that engaging in at least 150 minutes of moderate-to-vigorous aerobic activity weekly can significantly improve insulin sensitivity and glycemic control. Starting a systematic walking program can be especially beneficial; consider beginning by assessing your current fitness level and setting achievable goals, like dedicating just 10-15 minutes to a daily walk. Research shows that engaging in 5-7 hours of physical activity weekly is inversely related to the risk of developing type 2 diabetes.
-
Control stress through mindfulness practices, yoga, or meditation. Persistent stress can lead to increased glucose concentrations, but research indicates that stress management techniques can positively influence your metabolic health.
-
Prioritize hydration by drinking ample water throughout the day. Proper hydration is essential for maintaining optimal glucose balance and can support your metabolic processes and overall well-being.
-
Think about meal timing and frequency. Consuming smaller, more frequent meals can assist in regulating glucose amounts, helping to prevent spikes and crashes in glucose levels, which contributes to better management of diabetes.
-
Incorporate fiber-rich foods into your diet. Foods rich in fiber, like vegetables, legumes, and whole grains, can slow down glucose absorption and improve satiety, making them advantageous for managing your glucose levels.
-
Participate in post-meal exercise. Engaging in physical activity after meals can effectively reduce glucose concentrations. Even mild exercise, like a brief stroll, can help lower post-meal increases in glucose levels.
By applying these strategies, you can take proactive steps to manage your health and enhance your fasting glucose readings. As U.S. Afsheen Syeda wisely stated, “Exercise is a first-line therapy recommended for patients with type 2 diabetes (T2D),” highlighting the crucial role of physical activity in managing this condition.
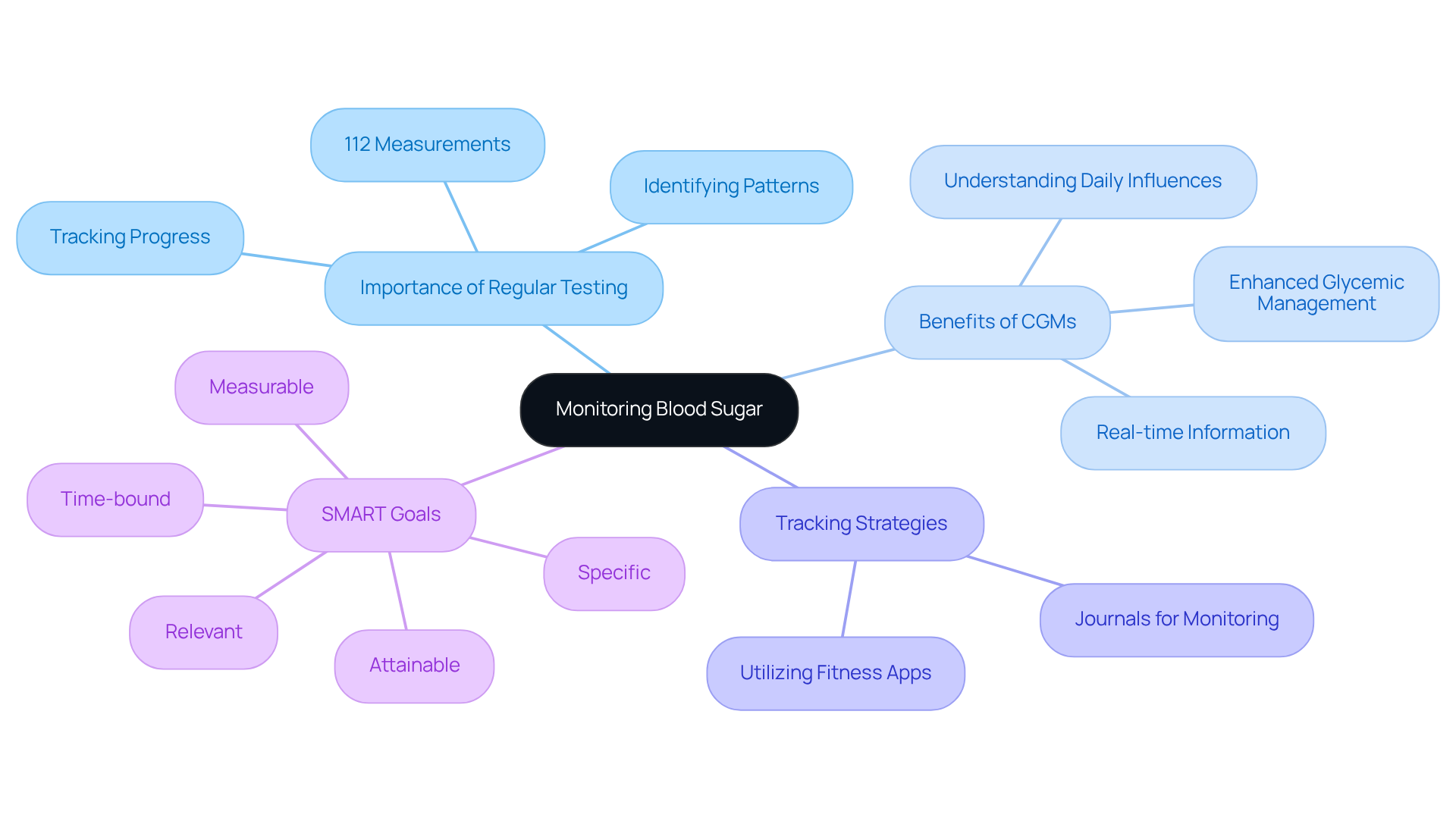
Monitoring Blood Sugar: The Importance of Regular Testing for Fasting Levels
Consistent observation of 112 fasting blood sugar measurements is essential for individuals managing diabetes or prediabetes. Have you ever felt overwhelmed by your health journey? This practice not only helps track your progress but also identifies patterns that can inform necessary adjustments to your diet and lifestyle. It’s important to recognize that monitoring 112 fasting blood sugar levels at least once a week—or more often as suggested by your healthcare professional—can make a significant difference.
Many patients find that continuous glucose monitors (CGMs) provide substantial benefits. They deliver real-time information, improving the accuracy of glucose management. For instance, individuals utilizing CGMs have reported enhanced glycemic management and a greater understanding of how their daily activities influence their glucose levels. Diabetes educators stress that regular testing, particularly of 112 fasting blood sugar levels, is crucial; research indicates that patients who consistently track their glucose are more likely to reach their target HbA1c values.
Furthermore, integrating effective strategies for progress tracking, such as utilizing fitness apps and journals, can empower you on your health management journey. By setting SMART goals—specific, measurable, attainable, relevant, and time-bound—you can cultivate a sense of achievement. This approach helps maintain your engagement in your health programs. Remember, by integrating these monitoring strategies and goal-setting techniques, you can take proactive steps toward better health outcomes. You’re not alone in this journey; many have walked this path and found success.
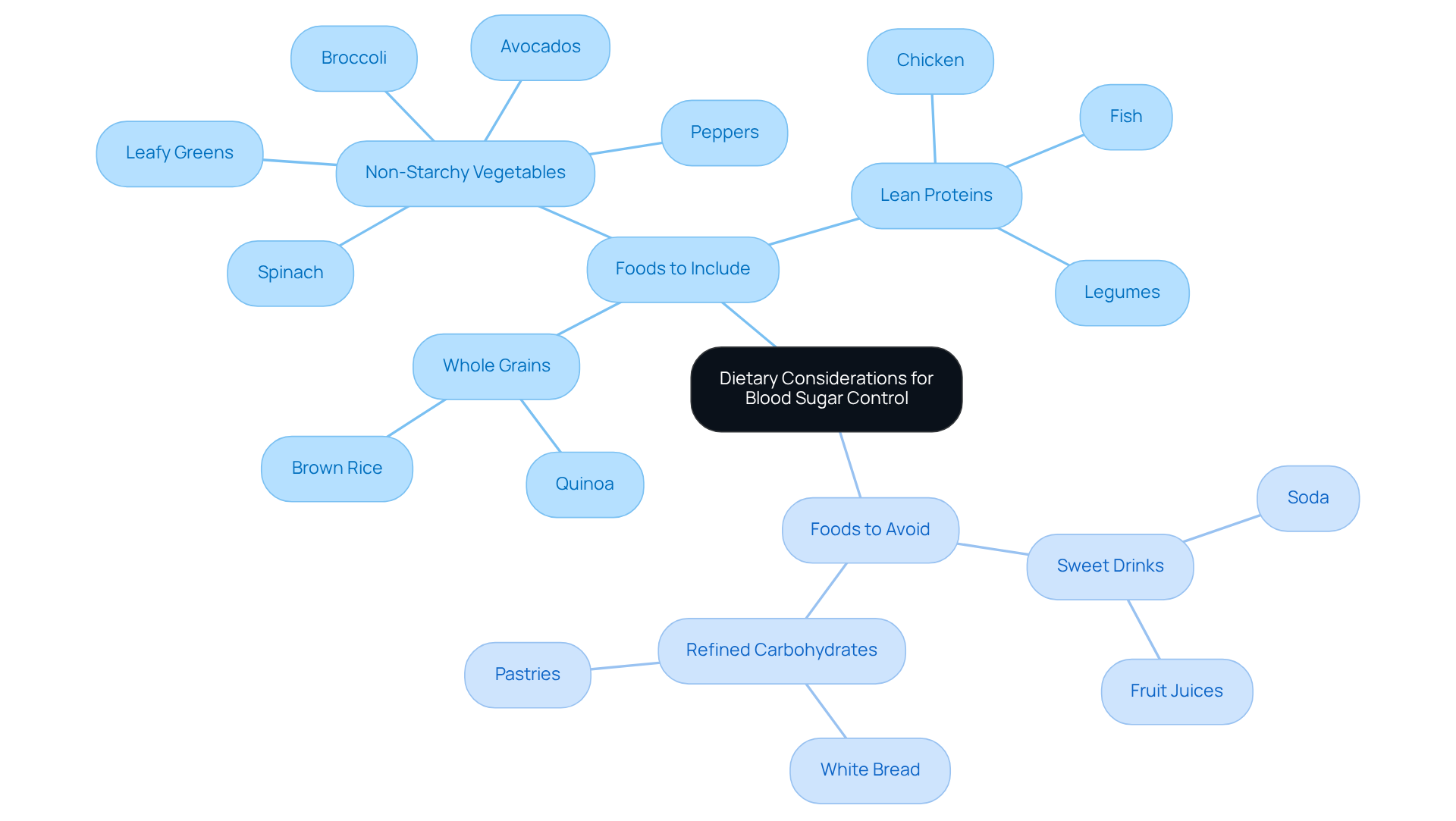
Dietary Considerations: Foods to Include and Avoid for Blood Sugar Control
To maintain stable glucose levels, it’s essential to prioritize incorporating certain foods into your diet. First, consider non-starchy vegetables like spinach, broccoli, and peppers. These are low in carbohydrates and high in fiber, which can assist in glucose regulation. If you’re in San Marcos, think about adding local produce such as leafy greens and avocados. Not only are they nutritious, but they also support a diabetes-friendly diet.
Next, whole grains like quinoa and brown rice are wonderful options. They provide fiber and slow-digesting carbohydrates that help prevent spikes in glucose levels. Many local restaurants and farmers’ markets offer these choices, making it easier to include them in your meals.
Lean proteins, such as chicken, fish, and legumes, are also vital. They help maintain stable levels by enhancing fullness and reducing cravings. Look for local eateries that focus on fresh, whole ingredients to align your meals with your health goals.
It’s important to recognize that proper hydration plays a crucial role in glucose regulation. Opt for water or herbal teas instead of sweet drinks. Staying adequately hydrated can help stabilize your glucose levels.
On the other hand, certain foods should be avoided to support ideal glucose management. Sweet drinks like soda and fruit juices can lead to quick increases in glucose due to their high fructose content. Additionally, refined carbohydrates, such as white bread and pastries, are rapidly digested and can cause significant rises in glucose.
Dietitians emphasize that thoughtful food selections—like adding more non-starchy vegetables and lean proteins while limiting refined carbohydrates—can greatly enhance glucose management, helping to achieve a 112 fasting blood sugar. For instance, a well-rounded meal containing protein and carbohydrates can help reduce glucose spikes, which is beneficial for maintaining a 112 fasting blood sugar throughout the day. Consistently consuming fiber-rich foods, such as whole grains and vegetables, is associated with improved glucose regulation, which can help achieve a 112 fasting blood sugar by slowing the absorption of carbohydrates into the bloodstream.
Understanding carbohydrates is essential for maintaining a healthy 112 fasting blood sugar. The balance between insulin levels and carbohydrate intake directly impacts the 112 fasting blood sugar. Effective management of glucose levels is key to maintaining a healthy 112 fasting blood sugar. As noted by the American Diabetes Association, intentional food choices—like increasing non-starchy veggies and opting for lean proteins—will help you meet your health goals. Moreover, including a high-protein diet has been shown to lead to a 40% reduction in the average 24-hour integrated glucose area response, highlighting its effectiveness in managing glucose levels.
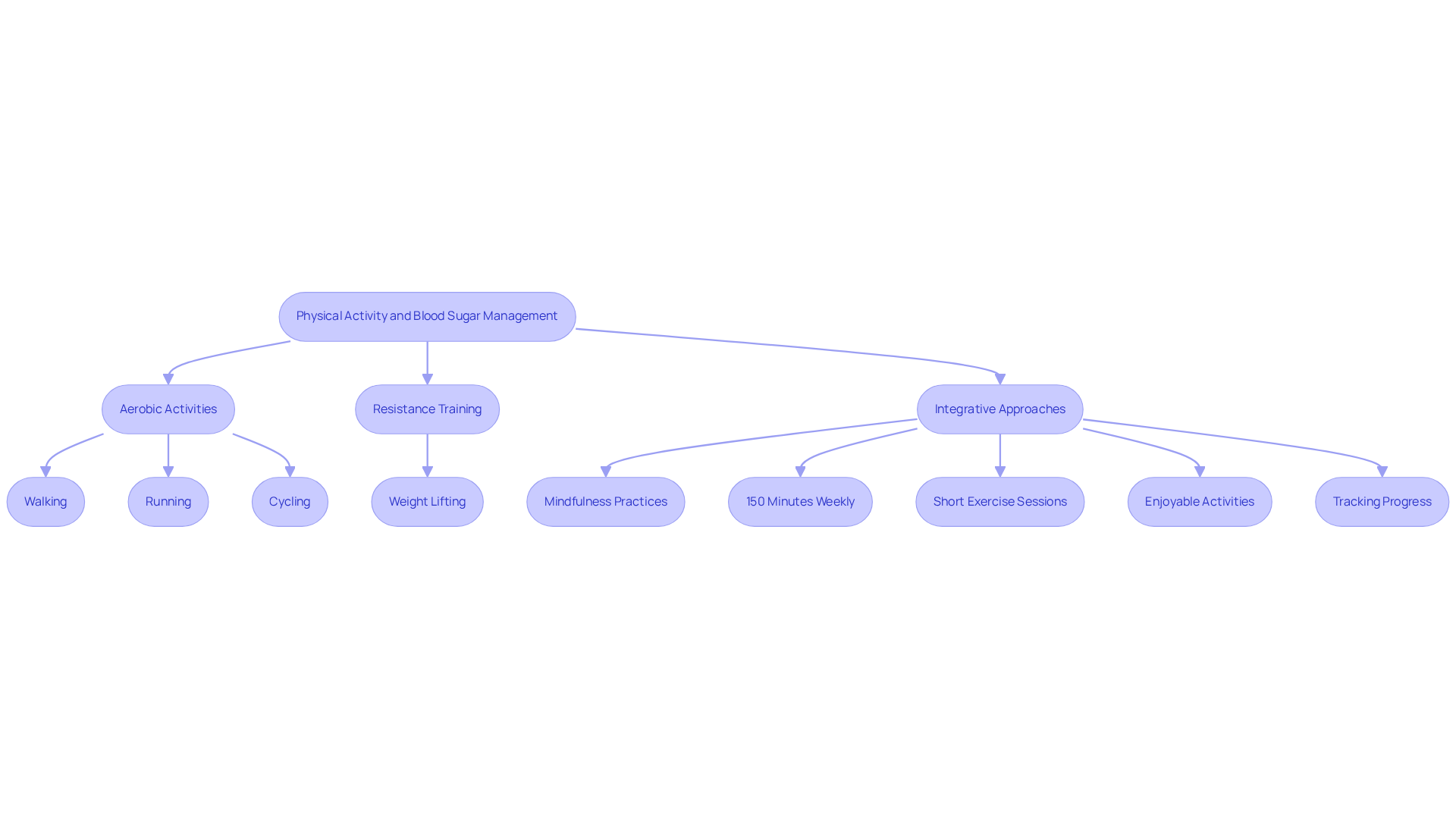
Physical Activity: How Exercise Impacts Fasting Blood Sugar Levels
Physical activity is crucial for effectively managing fasting glucose concentrations. Engaging in regular exercise enhances insulin sensitivity, enabling the body to utilize glucose more efficiently. It’s important to recognize that aerobic exercises like walking, running, and cycling can significantly lower sugar levels. Resistance training, including weight lifting, also plays a positive role in glucose management. Current guidelines recommend aiming for at least 150 minutes of moderate-intensity exercise each week, complemented by strength training exercises at least twice weekly.
Integrative functional medicine approaches, such as personalized nutrition plans, targeted supplements, and stress management techniques, can further enhance the effectiveness of physical activity in diabetes management. Many patients find that integrating mindfulness practices, yoga, and relaxation techniques can assist in alleviating stress, which is essential for sustaining stable glucose concentrations. Real-life examples illustrate the impact of physical activity on blood sugar control. Individuals who incorporate regular exercise into their routines often report improved fasting blood sugar levels along with overall health. Fitness professionals emphasize that even short bouts of activity can be beneficial; for example, three 10-minute sessions of moderate exercise throughout the day can yield similar cardiovascular benefits as a continuous 30-minute workout.
Furthermore, the American Diabetes Association emphasizes that physical activity is a changeable risk factor for type 2 conditions, significantly affecting insulin sensitivity. As one expert noted, ‘It’s easy to brush exercise aside if you don’t have a 30 to 60-minute chunk of time, but you don’t need a wide-open schedule to meet your fitness goals.’ This highlights the significance of incorporating movement into everyday activities, making it a practical method for managing blood sugar levels effectively. Additionally, tracking workout progress can help individuals visualize their fitness journey and stay committed to their goals. Finding enjoyable activities can also enhance motivation, making it easier to stick to an exercise routine. By adhering to a structured walking program and establishing SMART goals, patients can take control of their health management journey.
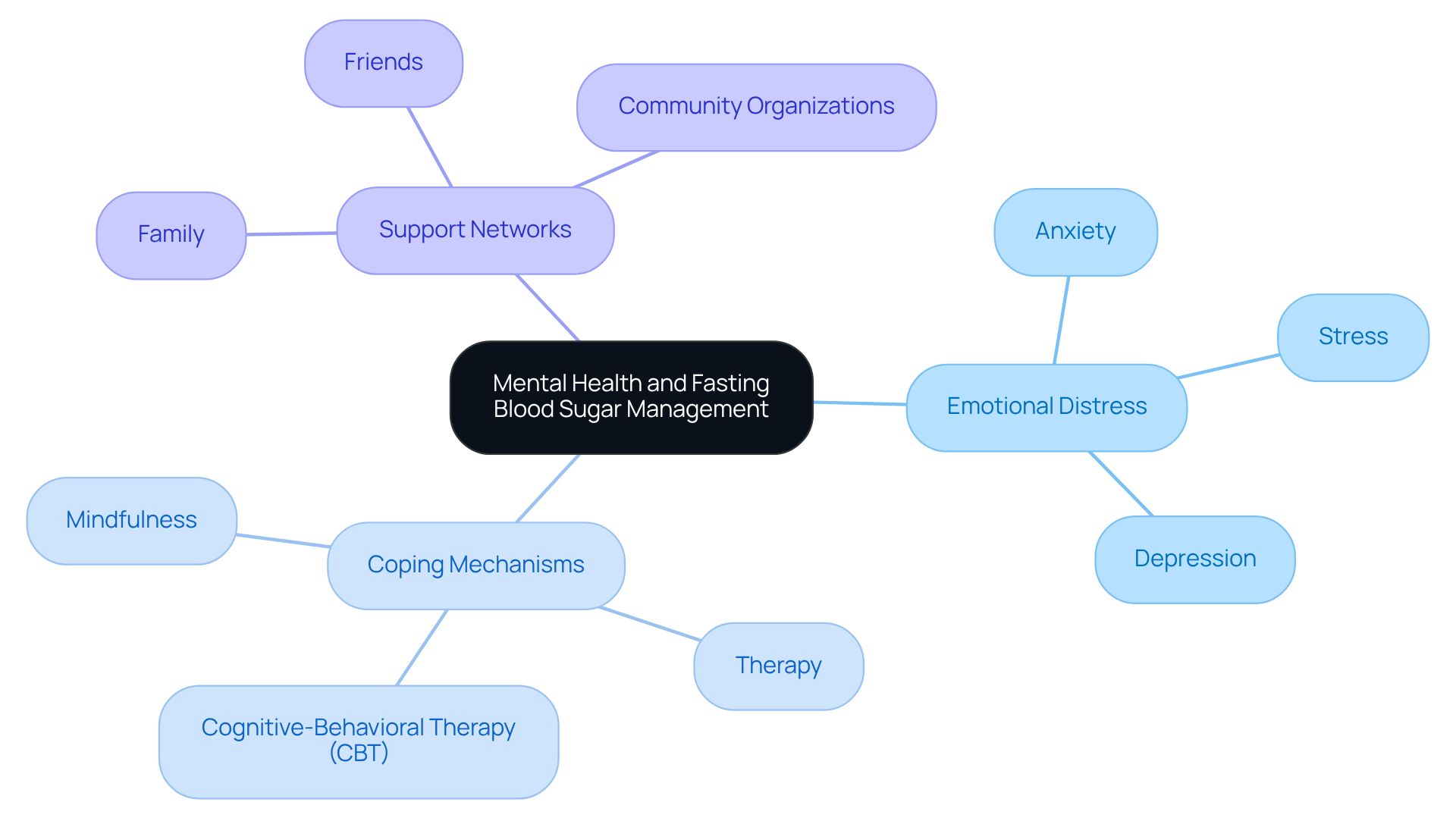
Mental Health: The Psychological Impact of Managing Fasting Blood Sugar Levels
Managing 112 fasting blood sugar levels can significantly affect mental health, often leading to increased feelings of anxiety, stress, or depression. It’s important to recognize that studies show more than half of US adults with this condition experience some form of distress, with 7% indicating severe distress. Acknowledging these emotional challenges is essential for effectively managing the condition. Many patients find that engaging in stress-reducing activities—such as mindfulness practices, therapy, or support groups—can provide vital coping mechanisms. For instance, cognitive-behavioral therapy (CBT) has been shown to improve mental health outcomes, helping individuals develop positive beliefs and healthier behaviors.
Furthermore, creating a strong support network—consisting of friends, family, and community organizations—can offer encouragement and motivation, making the experience of managing this condition feel less isolating. Mental health experts emphasize that addressing psychological factors is crucial, as proper management of 112 fasting blood sugar can reduce the likelihood of encountering additional mental health issues. By focusing on both physical and mental health, individuals can enhance their overall quality of life while navigating the challenges of this condition. Remember, you are not alone in this journey, and seeking support can make a significant difference.
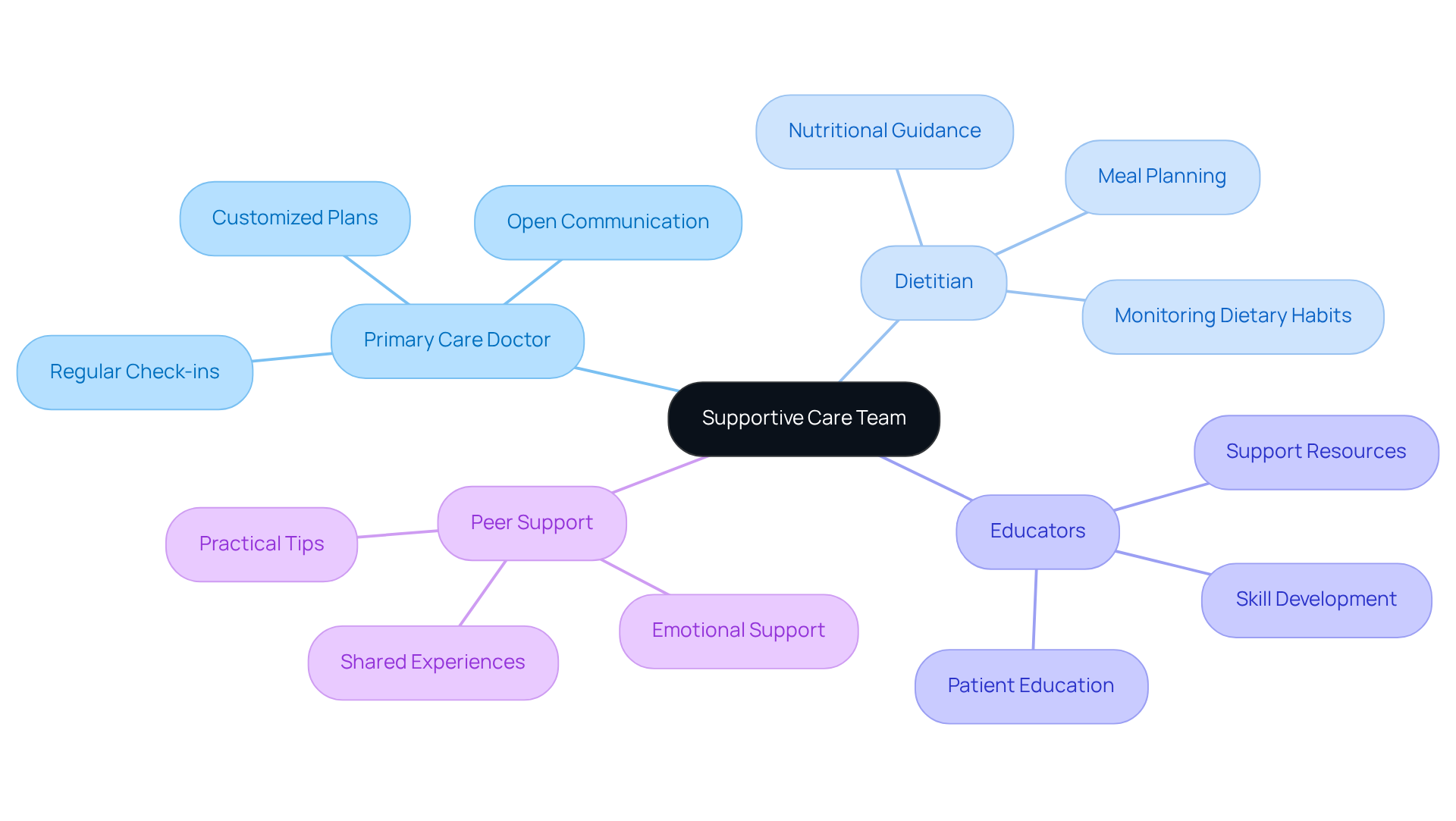
Collaboration with Healthcare Providers: Building a Supportive Care Team
Creating a supportive care team is essential for effectively managing your condition. It’s important to recognize that working closely with healthcare providers—like your primary care doctor, dietitian, and educators—ensures a comprehensive approach to your care. At Integrative Wellness Center, we believe in the power of detailed testing that goes beyond typical lab work. This allows us to craft customized plans tailored just for you.
Many patients find that regular check-ins with their care team help them stay on track with their management plans. These interactions provide personalized advice and empower you to make informed decisions about your health. Open communication with your care team nurtures a sense of responsibility and support, helping you conquer Type 2 diabetes and enhance your overall well-being.
To maximize your diabetes management, consider scheduling regular appointments with your care team. This time together allows you to review your progress and adjust your plan as needed. Remember, you are not alone on this journey; your care team is here to support you every step of the way.
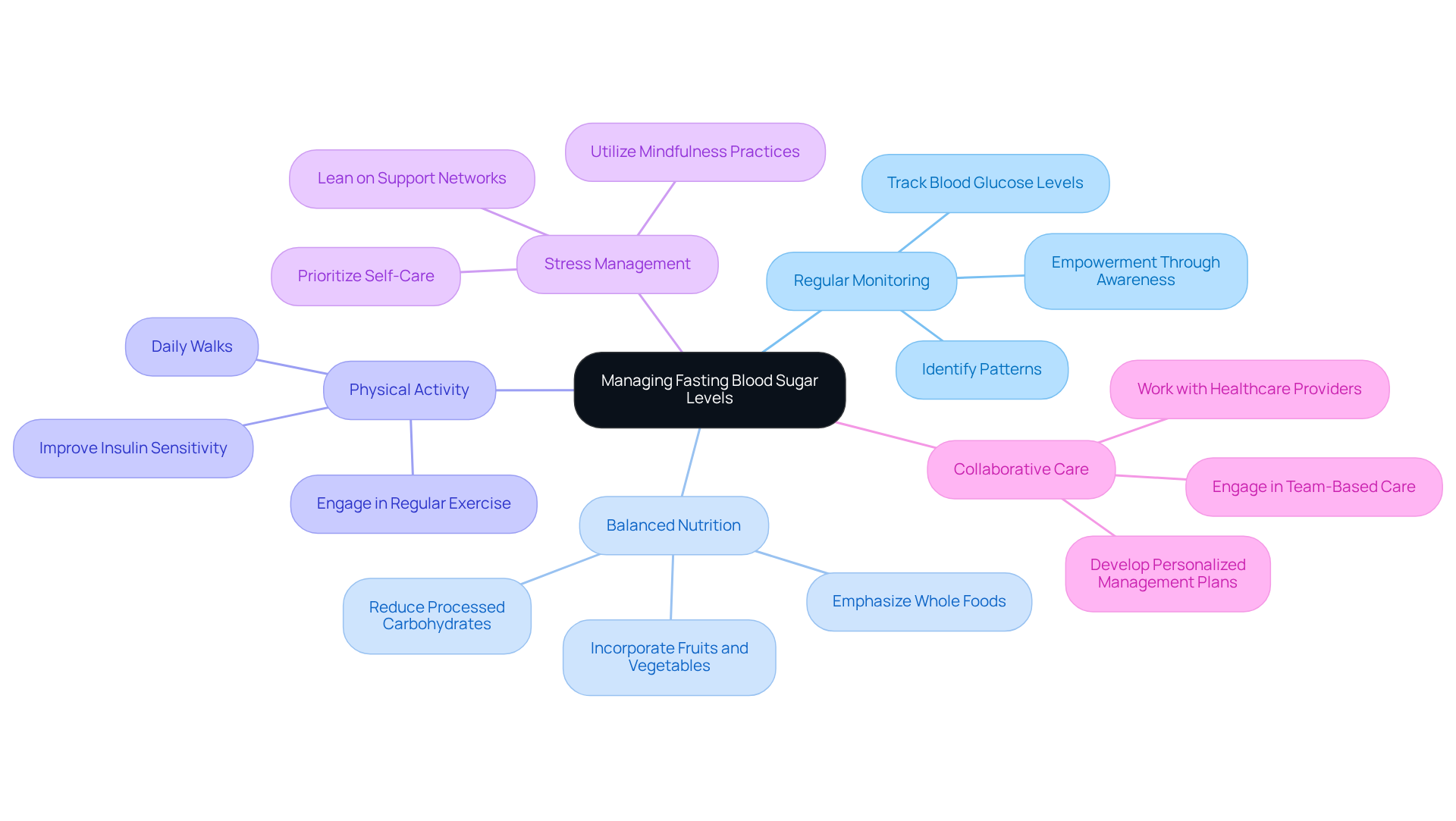
Key Takeaways: Proactive Steps for Managing Fasting Blood Sugar Levels
Managing 112 fasting blood sugar can feel overwhelming at times, but there are proactive strategies that can help you take charge of your health. First, consider Regular Monitoring. Consistently tracking your blood glucose levels allows you to identify patterns and make informed adjustments. Have you noticed any trends in your readings? This awareness can empower you.
Next, focus on Balanced Nutrition. Emphasizing a diet rich in whole foods and reducing processed carbohydrates can significantly stabilize your glucose levels. Think about incorporating more fruits, vegetables, and whole grains into your meals.
Physical Activity is another key component. Engaging in regular exercise not only improves insulin sensitivity but can also help reduce your 112 fasting blood sugar levels. Many patients find that even a daily walk makes a difference.
Don’t forget about Stress Management. Utilizing mindfulness practices and leaning on your support networks can help reduce stress, which often negatively impacts glucose regulation. It’s important to recognize that taking time for yourself is essential for your health.
Lastly, consider Collaborative Care. Working closely with your healthcare providers to develop a personalized diabetes management plan can address your unique needs. Remember, you’re not alone in this journey. By implementing these strategies, you can take meaningful steps toward achieving optimal 112 fasting blood sugar levels. You have the power to make a positive change.
Conclusion
Managing a fasting blood sugar level of 112 mg/dL is an important step in preventing the progression to type 2 diabetes and its associated health complications. It’s essential to recognize that this level indicates a need for proactive measures to maintain health. By emphasizing lifestyle changes, regular monitoring, and collaborative care with healthcare providers, individuals can feel empowered to take control of their blood sugar levels effectively.
Many patients find that making dietary adjustments—such as incorporating whole foods and reducing processed carbohydrates—can significantly impact their health. Consistent physical activity also plays a vital role in enhancing insulin sensitivity. Additionally, it’s crucial to consider the psychological aspects of managing blood sugar. Stress management and having support systems in place can greatly influence overall well-being. Engaging in these practices not only aids in stabilizing glucose levels but also promotes a healthier lifestyle.
Ultimately, understanding and managing a fasting blood sugar level of 112 mg/dL can lead to significant health improvements. By actively monitoring blood sugar, adopting a balanced diet, engaging in regular exercise, and fostering a supportive healthcare team, individuals can navigate the challenges of prediabetes and work towards a healthier future. Remember, taking these steps is not just about managing a number; it’s about reclaiming your health and enhancing your quality of life.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a holistic approach designed to help individuals manage their blood sugar effectively. It combines educational resources, personalized coaching, and practical tools to empower participants in understanding their condition and making sustainable lifestyle changes.
What are the expected outcomes of the 30-Day Diabetes Reset Program?
Participants often experience transformative results, including weight loss, decreased medication dependency, and increased energy. For example, one participant lost 55 lbs and improved their A1C from 9.1 to 5.7 after 8 months.
How does personalized coaching contribute to the program’s effectiveness?
Personalized coaching enhances engagement and accountability, which can lead to better health outcomes for participants, helping them navigate their journey toward improved health.
What does a fasting blood sugar level of 112 mg/dL indicate?
A fasting blood sugar level of 112 mg/dL falls within the prediabetes spectrum, indicating higher glucose readings than normal and signaling the need for prompt measures to prevent the onset of type 2 diabetes.
What health risks are associated with a fasting blood sugar level of 112?
Risks include an increased likelihood of developing type 2 diabetes, cardiovascular issues, and other metabolic disorders, as well as complications such as chronic kidney disease and vision impairment.
What lifestyle adjustments are recommended for managing elevated fasting blood sugar levels?
Recommended adjustments include dietary changes and increased physical activity to help lower glucose levels and reduce health risks.
How can individuals reduce their risk of developing type 2 diabetes?
Adopting a balanced diet, increasing physical activity, and achieving a weight reduction of 5-10% can significantly decrease the risk of developing type 2 diabetes. Engaging in at least 150 minutes of moderate exercise weekly can also improve insulin sensitivity.
What resources does Dr. Jason Shumard provide for managing blood sugar conditions?
Dr. Shumard offers personalized nutrition plans, lifestyle changes, and various resources and events designed to empower patients on their journey toward reversing diabetes and achieving holistic health.