Overview
Managing diabetes can often feel overwhelming, and achieving a normal Glucose Management Indicator (GMI) requires a multifaceted approach. It’s important to recognize that dietary changes, increased physical activity, and personalized education on glucose regulation are crucial components of this journey. Many patients find that programs like the Integrative Wellness Center’s 30-Day Diabetes Reset provide essential resources and support. These programs have been shown to significantly improve health outcomes, leading to better management of diabetes.
Imagine having a community that understands your struggles and offers guidance every step of the way. The 30-Day Diabetes Reset is designed not just to inform but to empower you. Participants often share how the support they receive has made a remarkable difference in their lives, fostering a sense of hope and motivation.
If you’re looking for a way to take charge of your health, consider the benefits of this program. It’s more than just a reset; it’s a chance to reclaim your well-being with the guidance of compassionate professionals who truly care. Together, we can navigate the path to better health, one step at a time.
Introduction
In the realm of diabetes management, it’s important to recognize the significance of the Glucose Management Indicator (GMI). This innovative metric provides a more immediate glimpse into blood glucose levels compared to traditional A1C tests, allowing individuals to take proactive steps in their health journey. As we introduce the 30-Day Diabetes Reset Program at the Integrative Wellness Center, many patients find that combining personalized dietary strategies, physical activity, and comprehensive education can significantly enhance glucose control.
Imagine embracing a holistic lifestyle against the picturesque backdrop of San Marcos, CA. This program encourages participants to not only support their health but also to foster a sense of community and empowerment. This article delves into the critical components of effective diabetes management, exploring how GMI, alongside lifestyle modifications, can lead to transformative health outcomes. Together, we can navigate this journey toward better health.
Integrative Wellness Center: 30-Day Diabetes Reset Program for GMI Management
The Integrative Wellness Center’s 30-Day Diabetes Reset Program is thoughtfully designed to provide patients with essential resources for managing their condition effectively. It emphasizes crucial dietary changes, increased physical activity, and comprehensive education on glucose regulation, all aimed at helping participants achieve a normal GMI. By addressing the symptoms and underlying factors of diabetes, this program encourages a proactive approach to health, empowering individuals to take charge of their well-being.
Living in San Marcos, CA, offers unique opportunities to enhance health management through a holistic lifestyle. Participants are invited to embrace the area’s beautiful outdoor environment, utilizing local parks and trails for regular exercise, which is vital for improving insulin sensitivity and managing weight. The program also highlights the importance of a balanced diet rich in local produce, such as avocados and berries, available at vibrant farmers’ markets, which supports blood sugar regulation and overall wellness.
It’s important to recognize that personalized management programs can significantly improve participant outcomes. For instance, research from the National DPP has shown how tailored approaches have successfully helped individuals reach their weight loss goals, a key aspect of managing health. This aligns with the focus of the 30-Day Diabetes Reset Program on individualized care, ensuring participants receive the support they need to thrive. Furthermore, the DiRECT trial revealed that those in weight loss programs experienced 47% fewer serious adverse events compared to control groups, highlighting the value of structured interventions like the Reset Program in promoting health and safety.
Dr. Jason Shumard shares, “The center provides an extensive 30-Day Reset program aimed at equipping patients with the essential tools and knowledge to enhance their health and effectively manage their condition.” This holistic approach not only targets immediate health improvements but also empowers participants with lasting knowledge and skills. Additionally, ongoing monitoring of remission rates and complications within the NHS Type 2 Diabetes Path to Remission Programme reflects a commitment to long-term success in health management. The 30-Day Diabetes Reset Program has demonstrated promising success rates, with many individuals reporting significant enhancements in their overall health and normal GMI levels. By fostering a culture of learning and empowerment, the program stands out as a vital support for those navigating the complexities of health care.
Understanding GMI: What Every Diabetic Needs to Know
The Glucose Management Indicator (GMI) is a vital metric that estimates an individual’s average blood glucose levels over time, utilizing data from continuous glucose monitoring (CGM). For those managing their blood sugar levels, understanding GMI is essential, as it offers a more nuanced view of glucose regulation compared to traditional A1C assessments. A lower GMI signifies improved glucose control, which is crucial for minimizing the risk of complications associated with diabetes. Ideally, individuals should aim for a normal GMI of below 5.7%, which is considered the normal range.
At Integrative Wellness Center, we recognize that effectively managing diabetes requires a personalized approach. Our clinic offers advanced testing to identify your unique dietary needs, enabling us to craft a treatment plan tailored specifically for you. This individualized care is vital for achieving glucose stabilization and reducing reliance on insulin.
It’s important to recognize that recent studies have shed light on the intricate relationship between GMI and HbA1c, highlighting the importance of careful interpretation by healthcare providers. A p-value lower than 0.05 was deemed statistically significant in these studies, underscoring the necessity for accurate GMI assessment. Evaluating GMI alongside other indicators, such as time in range (TIR), provides a comprehensive perspective on glucose management, empowering individuals and healthcare providers to make informed treatment decisions.
Many patients find that integrating holistic lifestyle approaches is also essential for managing type 2 diabetes in San Marcos, CA. Engaging in regular outdoor activities, like hiking or walking in local parks, can enhance insulin sensitivity and improve overall well-being. Additionally, focusing on a balanced diet rich in local produce, such as avocados and berries, supports blood sugar regulation. Community wellness initiatives can further provide invaluable support, offering resources and motivation for individuals on their health management journey.
Real-life examples illustrate the profound impact of GMI on health management. For instance, individuals who actively monitor their GMI often report significant improvements in their overall health and well-being. Current statistics indicate that understanding normal GMI is becoming increasingly important for patients facing blood sugar challenges, as it aids in diagnosing prediabetes and diabetes when used alongside A1C and TIR metrics. The research concerning GMI was sanctioned by the autonomous Ethics Committee (Approval Number 50 from 19 October 2021), lending credibility to its findings.
In summary, comprehending how GMI is calculated—by analyzing CGM data to assess average glucose levels—and its significance can greatly enhance strategies for managing diabetes. By prioritizing personalized nutrition, regular exercise, and community support, individuals can achieve better health outcomes and lessen reliance on conventional medical interventions.
GMI vs. A1C: Key Differences and Implications for Diabetes Care
Managing blood sugar can be a challenging journey, and understanding the roles of GMI and A1C is essential for effective control. GMI, which is derived from continuous glucose monitoring (CGM) data, reflects average glucose levels over a shorter timeframe, providing valuable insights into daily fluctuations. On the other hand, A1C measures average blood glucose over the preceding two to three months, offering a broader perspective on long-term control. Recognizing this distinction is crucial, as GMI can indicate rapid changes in glucose levels, enabling quicker adjustments to management strategies.
For patients, it’s vital to aim for a GMI below 7% to support effective management of their condition. Recent findings highlight the significance of this statistic in fostering better health outcomes. Moreover, a study that evaluated the discrepancies between GMI and A1C in individuals without diabetes revealed notable differences, suggesting that GMI may not always accurately estimate A1C levels in healthy individuals. Understanding this discordance is essential, as it can influence treatment decisions and care strategies.
The implications of GMI versus A1C go beyond mere numbers; they empower individuals to take an active role in their health management. By comprehending how GMI provides timely feedback, individuals can feel more equipped to engage in their health journey. As Dr. Jason Shumard beautifully puts it, “By offering individuals actionable insights and practical tools, the center cultivates an environment where people can reclaim their health and well-being, ultimately resulting in improved quality of life and reduced dependence on conventional medical interventions.” This proactive approach, grounded in functional medicine strategies, can lead to better outcomes and a greater sense of control over one’s health.
Given the concerning statistics surrounding hospital safety—such as 7,000 incorrect medications and 80,000 infections acquired by patients—it becomes even more crucial for individuals to seek safe and effective solutions. Are you ready to take the next step toward reclaiming your health? Call 858-564-7081 to discover how Dr. Shumard can help you restore your health and get your life back!
Time in Range (TIR): Enhancing GMI Insights for Better Diabetes Control
Time in Range (TIR) is a vital metric that measures the percentage of time a person’s glucose levels remain within a specified target range. This measurement is essential for effective blood sugar management, as it has a direct correlation with the normal GMI. It’s important to recognize that elevated TIR percentages are associated with better glucose management and a lower risk of complications related to the condition.
Individuals are encouraged to strive for a TIR of at least 70%, which means they should aim to spend the majority of their day within the target glucose range. Monitoring TIR alongside normal GMI provides valuable insights into daily glucose patterns, enabling individuals and healthcare providers to make informed treatment adjustments.
Many patients find that case studies demonstrate how consistently maintaining a TIR above 70% can lead to significant improvements in overall blood sugar management, resulting in better health outcomes. For instance, one individual, after engaging in Dr. Jason Shumard’s 30-Day Diabetes Reset program, reported feeling considerably improved, shedding pounds, and no longer requiring medications. This showcases the transformative potential of such holistic methods.
Experts in glucose care highlight that concentrating on TIR not only boosts normal GMI but also contributes to a more thorough understanding of glucose dynamics throughout the day. Incorporating effective strategies for progress tracking and goal setting can empower individuals in their health management journey. Consider utilizing fitness apps, journals, and SMART goals. For example, establishing a target to boost daily TIR by a certain percentage can encourage individuals to participate more actively in their health management.
By emphasizing TIR, individuals can regain their health and wellness, ultimately resulting in an enhanced quality of life and a decreased dependence on traditional medical treatments. Dr. Jason Shumard emphasizes that by providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being. Moreover, using devices such as the Simplera sensor, which can be worn for as long as 14 days, enables ongoing observation of TIR, improving the overall control of blood sugar levels.
Calculating GMI: How to Measure Your Glucose Management Indicator
Calculating your normal GMI can feel overwhelming, but it’s a straightforward process that uses data from your continuous glucose monitor (CGM). The formula for GMI is:
GMI (%) = 3.31 + 0.02392 x (mean glucose in mg/dL).
For instance, if your average glucose level is 150 mg/dL, your GMI would be approximately 6.9%. Regularly calculating your normal GMI can assist you in tracking your progress and guiding your efforts in managing blood sugar levels.
It’s important to recognize that research shows a sample size of 131 individuals revealed a median difference of 0.2 between GMI and HbA1c, with an interquartile range of 0.15 percentage points. This highlights how valuable tracking normal GMI can be in understanding your glucose control.
Many patients find that incorporating expert guidance on normal GMI calculations enhances their diabetes strategy, providing them with actionable insights. As Dr. Jason Shumard wisely notes, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being.”
To further enhance your health oversight, consider setting SMART goals—specific, measurable, attainable, relevant, and time-bound—related to your normal GMI. For example, you might aim to reduce your average glucose level by a certain percentage over the next month. Additionally, think about utilizing various tracking methods such as fitness apps, journals, and pedometers to monitor your progress effectively. Regularly reviewing your progress fosters accountability and allows you to adapt your goals as your health conditions change. By prioritizing normal GMI calculations alongside organized goal-setting, you can cultivate a sense of accomplishment and stay engaged in your health journey.
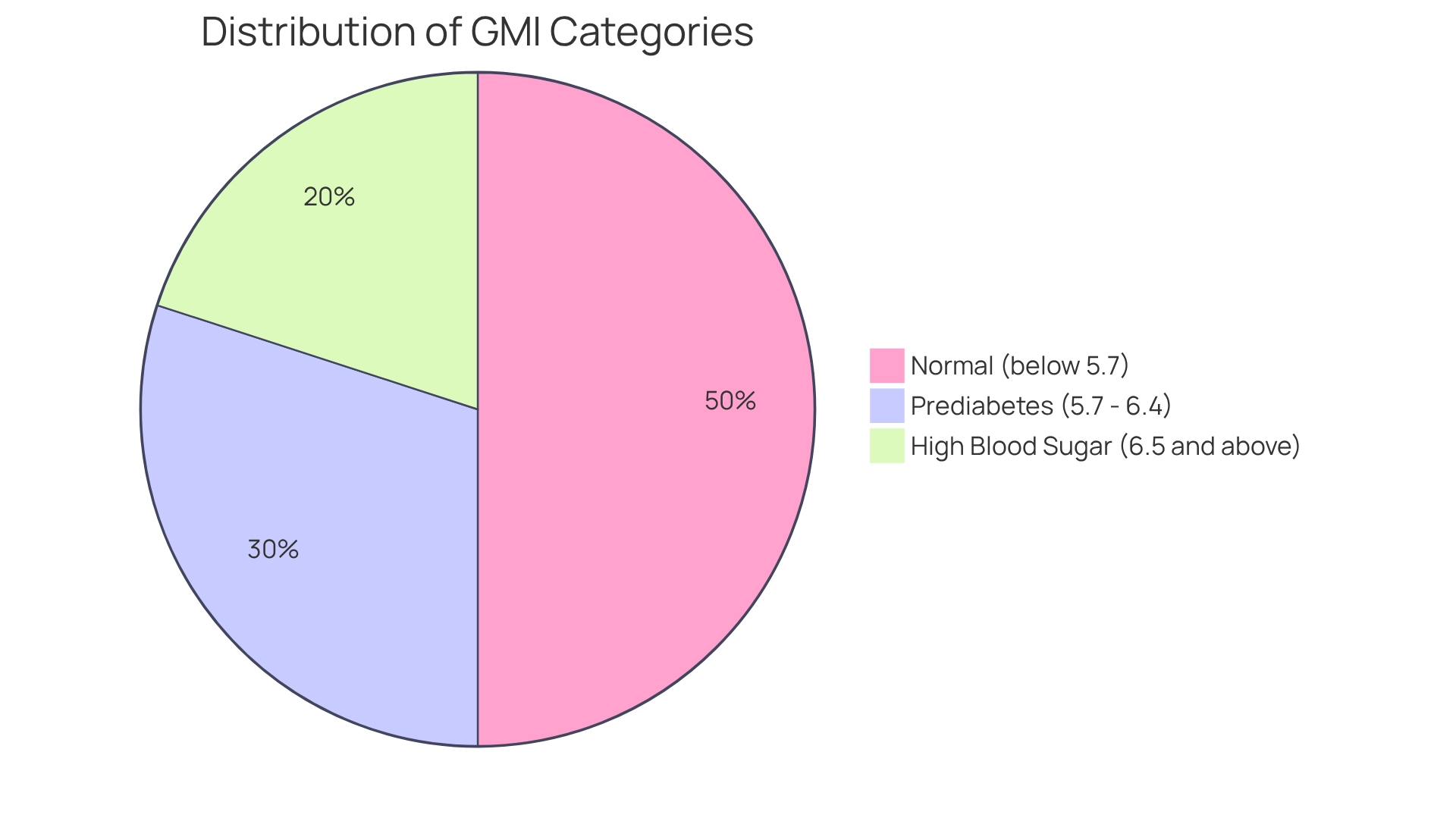
Optimal Glucose Levels: What GMI Reveals About Your Health
Optimal glucose levels are essential for effective management of blood sugar and overall health. It’s important to recognize that a normal GMI is categorized as below 5.7%, while levels between 5.7% and 6.4% suggest prediabetes. A GMI of 6.5% or above denotes high blood sugar. Maintaining a normal GMI within the normal range is crucial, as it correlates with a significantly reduced risk of complications, including cardiovascular disease, neuropathy, and kidney damage.
Many patients find that a GMI of 7.0% corresponds to a mean glucose level of approximately 146 mg/dL, highlighting the importance of regular monitoring. Those who consistently maintain their normal GMI within the normal range often report better health outcomes and a lower incidence of diabetes-related complications. One individual shared, “I have lost 55 lbs. My A1C started at 9.1, and after 8 months, it is now 5.7.” This underscores the program’s effectiveness in reversing type 2 diabetes.
Expert opinions emphasize the significance of optimal glucose levels. As endocrinologist Yogish Kudva states, “Individuals with type 1 diabetes must use insulin to regulate blood sugar to survive.” This highlights the vital importance of blood sugar control for all individuals with this illness. However, it’s important to recognize that conventional treatments often fail to address the underlying issues of insulin resistance, leading to increased insulin levels and further complications. This raises concerns about relying solely on medications, as they may exacerbate insulin resistance rather than resolve it.
Recent discoveries indicate that GMI might not be a trustworthy measure for glycemic control in middle-aged and older individuals, emphasizing the necessity for personalized strategies in managing the condition. Regular consultations with healthcare providers can help patients develop effective strategies for maintaining optimal glucose levels, ultimately leading to improved health and quality of life. By prioritizing GMI monitoring and understanding its implications, individuals can take proactive steps toward managing their condition effectively.
Lifestyle Factors Influencing GMI: Tips for Diabetic Management
Several lifestyle factors can significantly influence your normal GMI. It’s important to recognize that managing diabetes can be challenging, but incorporating effective strategies can lead to positive changes. Here are essential tips for effective diabetes management:
- Diet: Prioritize a balanced diet abundant in whole foods, such as vegetables, lean proteins, and whole grains. Reducing processed sugars and carbohydrates is crucial, as studies indicate that lifestyle interventions can lead to a notable reduction in body weight, enhancing overall metabolic health. Many patients find that following a low GI diet positively influences their health results, highlighting the significance of food selections in managing blood sugar levels. Engaging with local farmers’ markets in San Marcos can provide access to fresh, seasonal produce that supports a diabetes-friendly diet.
- Physical Activity: Aim for at least 150 minutes of moderate exercise each week. Regular physical activity not only improves insulin sensitivity but also helps lower blood glucose levels, which contributes to achieving normal GMI outcomes. Consider starting a walking program as outlined in the Integrative Wellness Center’s guide, which emphasizes gradually increasing your walking duration and frequency. Studies indicate that lifestyle changes resulted in a notable decrease in body weight of -3.99% in contrast to standard treatment, emphasizing the efficacy of exercise in managing blood sugar levels. Joining a local hiking group or walking with a companion can enhance accountability and enjoyment.
- Stress Management: Implement stress-reducing techniques like mindfulness, yoga, or meditation. Chronic stress can negatively influence glucose levels, making stress control an essential part of managing blood sugar conditions. Many individuals find that participating in relaxation and mindfulness practices available in San Marcos can support better blood sugar control.
- Sleep: Prioritize quality sleep, as inadequate rest can disrupt glucose metabolism and increase insulin resistance. Studies indicate that sleep quality is closely connected to effective management of blood sugar.
Incorporating these lifestyle changes can lead to significant improvements in overall health and normal GMI. Real-world examples show that individuals who embrace these practices often experience improved well-being and better management of their condition. As highlighted by nutritionist Xinye Zou, “Making informed dietary choices is crucial for managing blood sugar levels effectively.
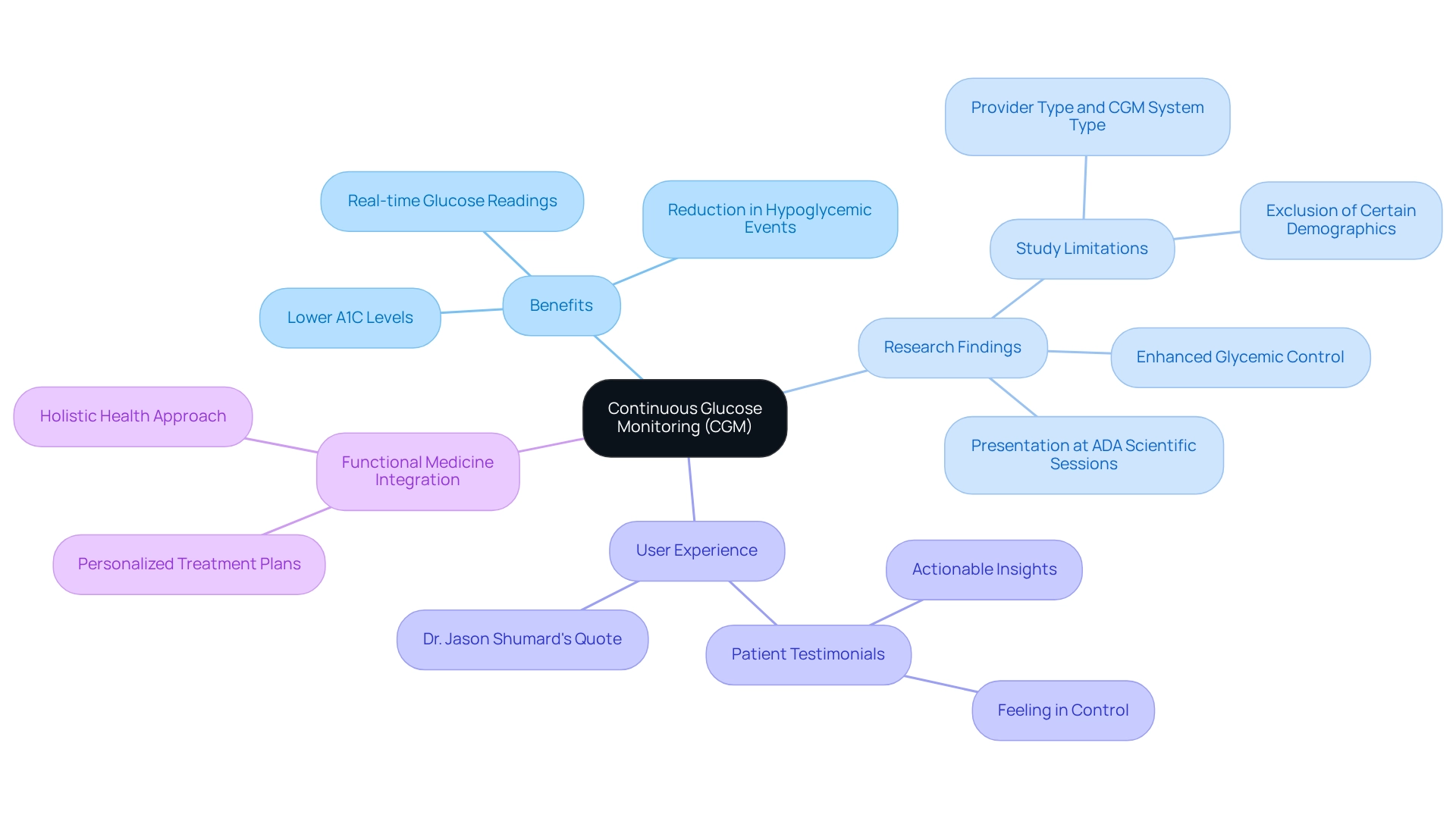
Continuous Glucose Monitoring (CGM): A Tool for Tracking Your GMI
Continuous Glucose Monitoring (CGM) has emerged as a groundbreaking tool for individuals managing blood sugar levels, especially within the context of integrative functional medicine. Have you ever wondered how your daily choices impact your glucose levels? By providing real-time glucose readings, CGMs empower individuals to understand these effects. This technology allows users to monitor their normal GMI with greater precision, facilitating timely adjustments to diet, exercise, and medication. The insights gained from CGM can lead to significant improvements in blood sugar control, as individuals become more attuned to their glucose trends.
Research shows that individuals using CGM experience enhanced glycemic control. Studies indicate that CGM users achieve lower A1C levels compared to those relying solely on traditional monitoring methods. Additionally, CGM technology has been linked to a reduction in hypoglycemic events, offering an extra layer of safety for patients. As CGM technology evolves, the latest advancements promise even greater precision and user-friendliness, making it an invaluable resource for effective blood sugar management.
In the realm of functional medicine, CGM is complemented by comprehensive evaluations and diagnostic tests that help identify the underlying factors contributing to the condition. This personalized approach ensures that treatment plans are tailored to each individual’s unique health profile, addressing not just symptoms but root causes. Many patients find that this holistic perspective provides them with a clearer path to better health.
Real-life examples illustrate the effectiveness of CGM in improving health outcomes related to blood sugar management. Patients at Integrative Wellness Center often express how CGM has helped them feel more in control of their health. One patient shared, “The actionable insights from CGM have truly changed my approach to managing my diabetes.” As Dr. Jason Shumard states, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being.” This aligns with the center’s commitment to empowering individuals through education and innovative methodologies.
However, it’s important to recognize that current studies have limitations, such as the inability to differentiate between provider type and CGM system type, which may influence the generalizability of findings. Despite these limitations, the evidence supporting CGM’s role in managing blood sugar levels is compelling. For anyone seeking to enhance their health outcomes, CGM stands out as an essential tool on this journey.
Clinical Significance of GMI: Implications for Diabetes Management
The clinical significance of the normal GMI truly shines in its ability to offer a more immediate evaluation of glucose control compared to traditional A1C measurements. It’s important to recognize that GMI allows healthcare providers to identify individuals who may be at heightened risk for complications, enabling timely adjustments to treatment plans. For many, a rising trend in normal GMI can prompt proactive measures designed to prevent the advancement of their condition.
Many patients find that normal GMI serves as a strong motivational resource, providing immediate feedback that encourages active involvement in their diabetes care. This dynamic approach not only fosters a sense of ownership over their health but also aligns with recent findings indicating that individuals with reduced kidney function experience a notable increase of 0.19 percentage points in A1C and differences in normal GMI. This highlights the need for tailored management strategies.
As Dr. Jason Shumard wisely states, “By offering individuals with actionable insights and practical tools, the center cultivates an environment where people can reclaim their health and well-being, ultimately resulting in enhanced quality of life and diminished dependence on conventional medical interventions.” This sentiment resonates with individuals like Ed, who shared, “I was depressed, no energy, and had insomnia. I hated how I felt and looked.” After participating in the 30-Day Diabetes Reset program, Ed experienced significant improvements in his health metrics, including a reduction in A1C from 9.1 to 5.7 and a fasting glucose level drop from 133 to 85.
By leveraging normal GMI, healthcare professionals can enhance individual outcomes and mitigate the risk of diabetes-related complications, ultimately leading to improved quality of life. For instance, in a recent case study, an individual with a normal GMI trend was able to adjust their medication regimen effectively, resulting in better glucose control and a reduced risk of complications. This illustrates the practical application of GMI in guiding treatment adjustments, offering hope and encouragement for those navigating their diabetes journey.
Empowering Patients: The Role of Education in Understanding GMI
Enabling individuals through education is essential for effective management of blood sugar levels, especially in understanding normal GMI levels and their consequences. It’s important to recognize that when individuals comprehend the significance of normal GMI, they are better prepared to make informed choices about their health. Educational resources, including workshops, seminars, and comprehensive informational materials, play a crucial role in clarifying GMI, fostering an environment where individuals feel encouraged to actively engage in their care.
Many patients find that education and self-management are linked to enhanced health outcomes. For instance, a randomized controlled trial in China showed that a structured self-management education (DSME) program resulted in significant lifestyle changes and improved glycemic control among participants. This emphasizes the transformative influence of health education in managing the condition effectively and illustrates how educational initiatives can empower individuals.
Furthermore, healthcare providers who establish supportive learning environments can significantly improve engagement among those receiving care. By providing access to educational resources, they not only enhance understanding of normal GMI but also empower patients to take charge of their health. This empowerment is echoed by health educators who emphasize the significance of knowledge in optimizing treatment results and preventing chronic complications. Dr. Jason Shumard has observed that health authorities should dedicate efforts to improve access to education for individuals with blood sugar issues, emphasizing the vital importance of education in enhancing treatment results.
Integrating comprehensive lifestyle approaches is crucial for effectively managing type 2 blood sugar conditions. In San Marcos, CA, individuals can benefit from embracing outdoor activities, such as hiking and walking in local parks, which not only improve physical fitness but also enhance insulin sensitivity. Additionally, focusing on a balanced diet rich in local produce, like avocados and berries, can help regulate blood sugar levels. Community wellness initiatives offer essential assistance, providing resources customized for blood sugar control while promoting a sense of inclusion. Practical instances, like workshops that emphasize understanding normal GMI, demonstrate the beneficial effect of education on blood sugar control. These initiatives not only provide individuals with practical tools but also cultivate a sense of community and support, ultimately resulting in improved health outcomes and a higher quality of life. Furthermore, the latest educational resources available for understanding normal GMI, such as online courses and interactive tools, can significantly enhance patient knowledge and engagement in their diabetes management journey.
Conclusion
The journey toward effective diabetes management can feel overwhelming, but understanding and utilizing the Glucose Management Indicator (GMI) offers a beacon of hope. This innovative metric provides a timely assessment of glucose levels, empowering you to make informed decisions about your health. By participating in the Integrative Wellness Center’s 30-Day Diabetes Reset Program, you can embrace a holistic approach that combines personalized dietary strategies, regular physical activity, and comprehensive education. These elements are crucial in achieving optimal GMI levels and improving overall health outcomes.
It’s important to recognize that incorporating lifestyle modifications, such as engaging in outdoor activities and prioritizing a balanced diet rich in local produce, further supports effective diabetes management. This program not only empowers you with the knowledge and tools necessary to manage your diabetes but also fosters a sense of community and shared experience among participants. Many patients find that this collaborative environment plays a vital role in maintaining motivation and commitment to lifestyle changes.
Ultimately, understanding GMI and its implications can lead to transformative health outcomes for those living with diabetes. By prioritizing education, personalized care, and community support, you can take proactive steps toward reclaiming your health and well-being. The integration of these strategies highlights the importance of an empowered and informed approach to diabetes management, paving the way for a healthier future. Remember, you are not alone on this journey; together, we can achieve lasting change.
Frequently Asked Questions
What is the purpose of the Integrative Wellness Center’s 30-Day Diabetes Reset Program?
The program is designed to provide patients with essential resources for effectively managing diabetes through dietary changes, increased physical activity, and comprehensive education on glucose regulation, aiming to help participants achieve a normal Glucose Management Indicator (GMI).
How does the program encourage a proactive approach to health?
By addressing the symptoms and underlying factors of diabetes, the program empowers individuals to take charge of their well-being and fosters a culture of learning and empowerment.
What lifestyle opportunities does living in San Marcos, CA, provide for participants?
San Marcos offers beautiful outdoor environments, local parks, and trails that participants can use for regular exercise, which is essential for improving insulin sensitivity and managing weight.
What dietary recommendations are emphasized in the program?
The program highlights the importance of a balanced diet rich in local produce, such as avocados and berries, which supports blood sugar regulation and overall wellness.
How does personalized management impact participant outcomes?
Personalized management programs can significantly improve outcomes, as research shows tailored approaches help individuals reach their weight loss goals, which is crucial for managing health.
What evidence supports the effectiveness of structured interventions like the Reset Program?
The DiRECT trial found that participants in weight loss programs experienced 47% fewer serious adverse events compared to control groups, demonstrating the value of structured interventions in promoting health and safety.
What is the Glucose Management Indicator (GMI)?
GMI is a metric that estimates an individual’s average blood glucose levels over time, using data from continuous glucose monitoring (CGM), providing a nuanced view of glucose regulation compared to traditional A1C assessments.
What is the ideal GMI level for individuals managing diabetes?
Individuals should aim for a normal GMI of below 5.7%, which is considered the normal range for glucose control.
How does the Integrative Wellness Center approach diabetes management?
The center offers advanced testing to identify unique dietary needs and crafts personalized treatment plans to achieve glucose stabilization and reduce reliance on insulin.
Why is understanding GMI important for managing diabetes?
Understanding GMI aids in diagnosing prediabetes and diabetes when used alongside A1C and time in range (TIR) metrics, allowing for more informed treatment decisions.
What role do community wellness initiatives play in diabetes management?
Community wellness initiatives provide resources and motivation, supporting individuals on their health management journey.
How can individuals actively engage in their health management through understanding GMI?
By comprehending how GMI provides timely feedback on glucose levels, individuals can feel more equipped to make adjustments to their management strategies and improve their health outcomes.