Overview
This article highlights the essential CPT codes vital for effective diabetes management, underscoring their significance in ensuring accurate billing and optimal patient care. It’s important to recognize that precise coding—like using 99213 for office visits and 99490 for chronic care management—plays a crucial role in preventing claim denials and enhancing healthcare outcomes. Many patients find that this attention to detail not only supports their care but also contributes to the financial sustainability of diabetes management programs. By understanding these codes, we can better navigate the complexities of care, ultimately leading to improved health and well-being.
Introduction
In the complex landscape of diabetes management, accurate coding serves as a vital cornerstone for ensuring both optimal patient care and the financial health of healthcare providers. It’s important to recognize that millions of individuals live with undiagnosed diabetes, making the stakes incredibly high. Missteps in coding can lead not only to claim denials but also to compromised patient outcomes, which can be distressing for both patients and providers alike.
This article delves into the critical role of precise CPT coding. Many patients find that understanding these codes can empower them in their journey toward better health. We will highlight key codes essential for effective diabetes management, the importance of meticulous documentation, and strategies for staying updated with evolving coding guidelines. By embracing and implementing these practices, healthcare professionals can enhance the quality of care they provide, while also ensuring the financial sustainability of their services. Together, we can navigate this challenging landscape with compassion and understanding.
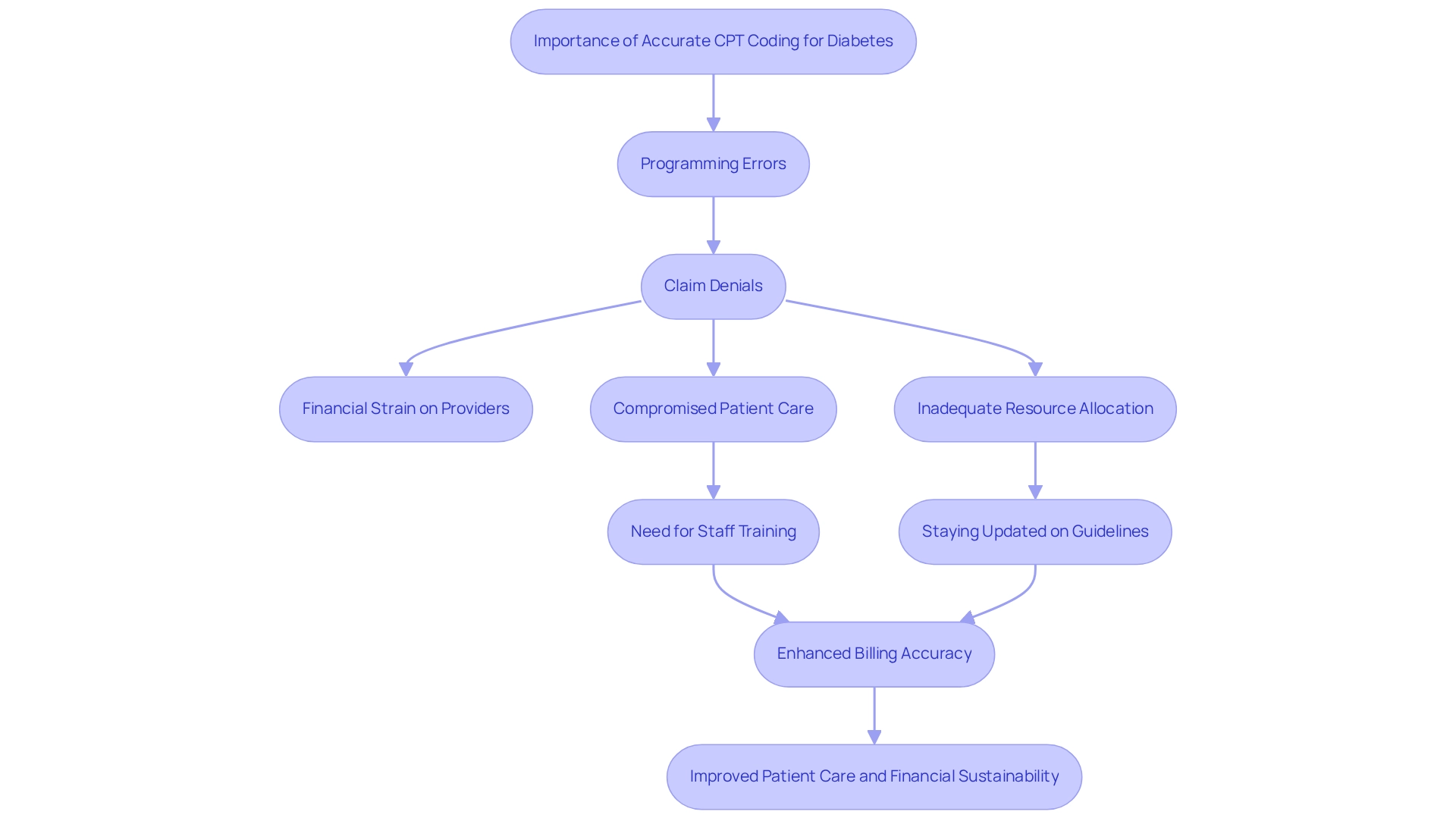
Understand the Importance of Accurate CPT Coding for Diabetes
Precise programming plays a vital role in ensuring optimal reimbursement rates associated with the CPT code for diabetes management. When programming errors occur, they can lead to claim denials, causing significant financial strain for healthcare providers. With approximately 7.3 million individuals living with undiagnosed diabetes, the need for accurate classification, specifically the correct CPT code for diabetes, becomes even more pressing, as it directly influences the quality of care and reimbursement available.
It’s important to recognize that the link between programming precision and healthcare quality is profound. Errors in programming can compromise the care individuals receive, resulting in delays in treatment or inadequate resource allocation. Many patients find that inconsistencies in programming standards among providers can lead to unreliable forecasts for resource distribution, ultimately affecting their outcomes and the financial health of the provider. Specific examples of programming errors, such as misclassifying a patient’s condition or relying on outdated codes, can lead to claim denials that complicate patient care further, particularly when it involves the CPT code for diabetes.
To address these challenges, conducting regular training sessions for staff on the importance of precise documentation is essential. Such training helps unify practices across facilities, reducing the likelihood of errors that lead to claim denials. Moreover, staying updated on the latest programming guidelines from organizations like the American Medical Association is crucial. As the AMA advises, “Stay informed about the latest regulations from leading entities such as the American Medical Association (AMA) to ensure appropriateness.” This commitment helps healthcare providers maintain compliance and accuracy in their billing practices.
Looking ahead to 2025, the impact of programming precision on healthcare reimbursement is more significant than ever. Frequent updates to diagnostic and procedural classifications are enhancing billing accuracy. This evolution in coding practices is vital for ensuring that 80% of reimbursements align with the services rendered, thereby supporting the financial sustainability of chronic condition management programs. Together, we can navigate these complexities to ensure that patients receive the care they deserve.
Identify Key CPT Codes for Diabetes Management
Familiarize yourself with essential CPT codes for diabetes management, including:
- 99213: Established patient office visit, crucial for routine check-ups.
- 95251: Continuous glucose monitoring (CGM) data analysis, vital for tracking glucose levels.
- 99490: Chronic care management services, which support ongoing patient care.
- 97803: Medical nutrition therapy, individual, focusing on dietary management.
It’s important to recognize that managing diabetes goes beyond regular physician appointments and blood sugar tracking. As Skye wisely pointed out, this condition requires thorough oversight that involves comprehension and effective use of CPT references. This comprehensive approach aligns with the principles of functional medicine, emphasizing personalized strategies that address not just symptoms but also the root causes of blood sugar issues through detailed assessments and diagnostic tests.
Many patients find it helpful to keep an updated list of identifiers related to blood sugar management. This ensures precise billing and adherence. For instance, the ICD-10 designation for type 2 diabetes mellitus with unspecified diabetic retinopathy without macular edema is 319, highlighting the significance of accurate classification in managing blood sugar conditions.
It is essential that all staff members obtain training on these regulations to reduce billing mistakes, which data indicate can greatly affect revenue cycles. In reality, billing mistakes related to the CPT code for diabetes can result in significant financial losses for practices. Consistently examining programming materials and updates is crucial to remain informed about any alterations in CPT codes, ensuring that your practice continues to be compliant and effective in managing health care.
Furthermore, integrating efficient methods for progress monitoring—like using fitness applications, journals, and pedometers—can empower individuals in their health management journey. Setting goals fosters a sense of accomplishment and involvement. Testimonials from individuals emphasize the effectiveness of precise coding and management practices, fostering trust and encouraging new clients to seek treatment.
Document Patient Information Accurately for Coding Compliance
Documenting all patient encounters meticulously is essential. Begin by ensuring you include a comprehensive patient history and current health status. Provide detailed accounts of the specific services rendered during each visit, along with any modifications to treatment plans or medications. Remember, excellent documentation facilitates effective communication of care plans to other providers, which is crucial in diabetes management, particularly when using the CPT code for diabetes.
It’s important to recognize that implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can significantly enhance participant engagement and motivation. For instance, an individual might establish a goal to track their glucose levels daily or seek to enhance their physical activity progressively. Frequently assessing one’s progress not only promotes accountability but also helps in adjusting objectives in response to evolving health conditions.
Many patients find that utilizing various tracking methods, such as fitness applications, journals, and pedometers, can effectively monitor their progress. Additionally, implementing standardized templates can enhance the efficiency of documentation processes. Providing training for staff on best practices in documentation ensures adherence to classification requirements.
Conducting regular audits of medical records is another important step to verify completeness and accuracy, thereby minimizing documentation errors that can impact compliance. Remember, complying with medical record documentation requirements is essential for maintaining high standards in care. Furthermore, recognizing that Modifier 59 signifies a procedure was separate or independent from other services conducted on the same day emphasizes the importance of precise documentation practices.
Insights from Dr. Jason Shumard’s Functional Medicine Approach demonstrate how effective documentation and structured goal-setting can lead to life-changing outcomes for individuals. This highlights the holistic strategy to managing blood sugar, reminding us that every step taken toward better health is a step worth celebrating.
Stay Informed on Updates to CPT Coding Guidelines
- Subscribe to updates from the American Medical Association (AMA) to receive timely information on CPT alterations that affect the CPT code for diabetes and blood sugar management. Staying informed is crucial for your health journey.
- Have you considered attending workshops and seminars dedicated to updates and best practices? These can provide valuable insights and networking opportunities that may inspire you.
- It’s beneficial to designate a staff member responsible for monitoring changes and sharing relevant information with the entire team. This way, everyone remains aligned and informed.
- Regularly reviewing updates during staff meetings can help keep the team prepared for any changes that may affect care. This practice fosters a culture of awareness and readiness.
- Utilize online resources and forums to stay connected with the community. Engaging in discussions can enrich your knowledge and experiences regarding best practices.
- As noted by Thomas K. Varghese Jr., MD, it’s important to stay in sync with changes in medical practices. This awareness is essential for healthcare providers to thrive in our ever-evolving landscape.
- Dr. Jason Shumard’s Functional Medicine Approach highlights the importance of education and empowerment. Staying informed about the CPT code for diabetes can lead to improved outcomes for individuals. His commitment to helping patients reverse type 2 diabetes through personalized guidance and lifestyle changes showcases the transformative power of informed healthcare practices.
- With 30% of new codes in the CPT 2025 code set being Category III CPT codes for emerging medical services, it is crucial for providers to remain vigilant and informed about these updates. Remember, knowledge is a powerful tool in your health management journey.
Conclusion
Accurate CPT coding is essential in the effective management of diabetes, significantly influencing patient outcomes and the financial stability of healthcare providers. It’s important to recognize that precise coding directly correlates with the quality of care delivered. Coding errors can lead to claim denials and adverse experiences for patients, highlighting the urgency for accurate coding practices, especially with millions potentially living with undiagnosed diabetes.
Identifying key CPT codes and understanding their application is vital for optimizing diabetes management. Many healthcare professionals find that familiarizing themselves with essential codes and participating in regular training can minimize billing errors while enhancing the overall quality of care. Furthermore, meticulous documentation of patient encounters is crucial, as it facilitates seamless communication among providers and ensures compliance with coding requirements.
Staying informed about updates to CPT coding guidelines is equally important. Engaging with resources from the American Medical Association and participating in relevant workshops can empower healthcare teams to adapt effectively to changes in the coding landscape. This proactive approach not only supports accurate billing practices but also enhances the overall care provided to patients.
In conclusion, embracing precise coding practices is a pivotal step towards improving diabetes management. By prioritizing education, documentation, and communication, healthcare providers can navigate the complexities of coding while fostering a supportive environment for patients. Together, these efforts contribute to better health outcomes and sustainable practices in diabetes care, underscoring the profound impact of accurate coding on the healthcare ecosystem.
Frequently Asked Questions
Why is precise programming important for diabetes management reimbursement?
Precise programming is crucial as it ensures optimal reimbursement rates associated with the CPT code for diabetes management. Errors in programming can lead to claim denials, which create financial strain for healthcare providers.
What are the consequences of programming errors in healthcare?
Programming errors can compromise patient care, leading to delays in treatment and inadequate resource allocation. They can also result in claim denials that complicate patient care, particularly concerning the CPT code for diabetes.
How many individuals are living with undiagnosed diabetes?
Approximately 7.3 million individuals are living with undiagnosed diabetes, highlighting the need for accurate classification and coding.
What role does training play in reducing programming errors?
Regular training sessions for staff on the importance of precise documentation help unify practices across facilities, reducing the likelihood of errors that lead to claim denials.
Why is it important to stay updated on programming guidelines?
Staying updated on the latest programming guidelines from organizations like the American Medical Association (AMA) is crucial for maintaining compliance and accuracy in billing practices.
What is the expected impact of programming precision on healthcare reimbursement by 2025?
The impact of programming precision on healthcare reimbursement is expected to be significant, with frequent updates to diagnostic and procedural classifications enhancing billing accuracy and ensuring that 80% of reimbursements align with the services rendered.
How does programming precision affect patient care and provider financial health?
Inaccurate programming can lead to unreliable forecasts for resource distribution, affecting patient outcomes and the financial sustainability of healthcare providers. Accurate coding is vital for ensuring patients receive the care they deserve.