Overview
Managing blood glucose levels in type 2 diabetes can feel overwhelming, but there are four essential steps that can help you regain control.
-
First, it’s vital to identify your target glucose levels. This process often begins with consulting healthcare providers who can offer personalized guidance tailored to your needs.
-
Next, establishing a routine for monitoring your levels is crucial. Many patients find that consistency in checking their glucose helps them stay informed and empowered. It’s important to recognize that this step can significantly impact your daily life.
-
Adhering to dietary guidelines is another key component. A balanced diet not only helps regulate blood sugar but also nourishes your body and spirit.
-
Incorporating regular physical activity rounds out this approach, contributing to both physical and mental well-being.
Remember, each of these steps plays a vital role in effectively managing diabetes and improving your overall health. By embracing these practices, you can embark on a journey toward a healthier lifestyle, one step at a time. You are not alone in this journey; many have found success and support through similar paths.
Introduction
Managing diabetes effectively can feel overwhelming at times, but it’s important to recognize that you are not alone in this journey. A multifaceted approach that encompasses monitoring, dietary choices, and physical activity can make a significant difference. With the right strategies in place, you can take control of your blood glucose levels and improve your overall health.
Many patients find that establishing personalized target levels with healthcare providers is a crucial first step. Adhering to dietary guidelines and incorporating regular exercise are equally vital components of effective diabetes management. Each step you take plays an essential role in navigating this path.
This article delves into practical methods for maintaining optimal blood sugar control, empowering you to approach your health journey with confidence and informed decision-making. Together, we can explore how small changes can lead to a healthier, more fulfilling life.
Identify Your Target Blood Glucose Levels
It’s important to recognize that managing diabetes can be challenging. Consult with your healthcare provider to determine your target blood glucose levels for type 2 diabetes. Typically, these are advised to be between 80-130 mg/dL before meals and under 180 mg/dL after meals. Achieving these targets is essential for effective diabetes management and can significantly influence your overall wellness outcomes. Keeping a detailed record of your blood glucose levels for type 2 diabetes is crucial; it allows you to monitor your progress towards these goals. Regular tracking can help you identify patterns and inform any necessary adjustments in your management plan.
Many patients find that they may need to adjust their targets as needed, based on their healthcare provider’s guidance and individual health objectives. Personalization is key, as each person’s needs may vary. Have you discussed your specific goals with your healthcare team?
Using a glucose meter or a continuous glucose monitor (CGM) can greatly assist you in regularly checking your levels. The American Diabetes Association suggests CGMs for adults with type 2 diabetes to help monitor their blood glucose levels when using non-insulin glucose-lowering agents. These devices offer real-time data that can improve your management strategies, making it easier to stay on track. Remember, you are not alone on this journey, and there are tools and support available to help you succeed.
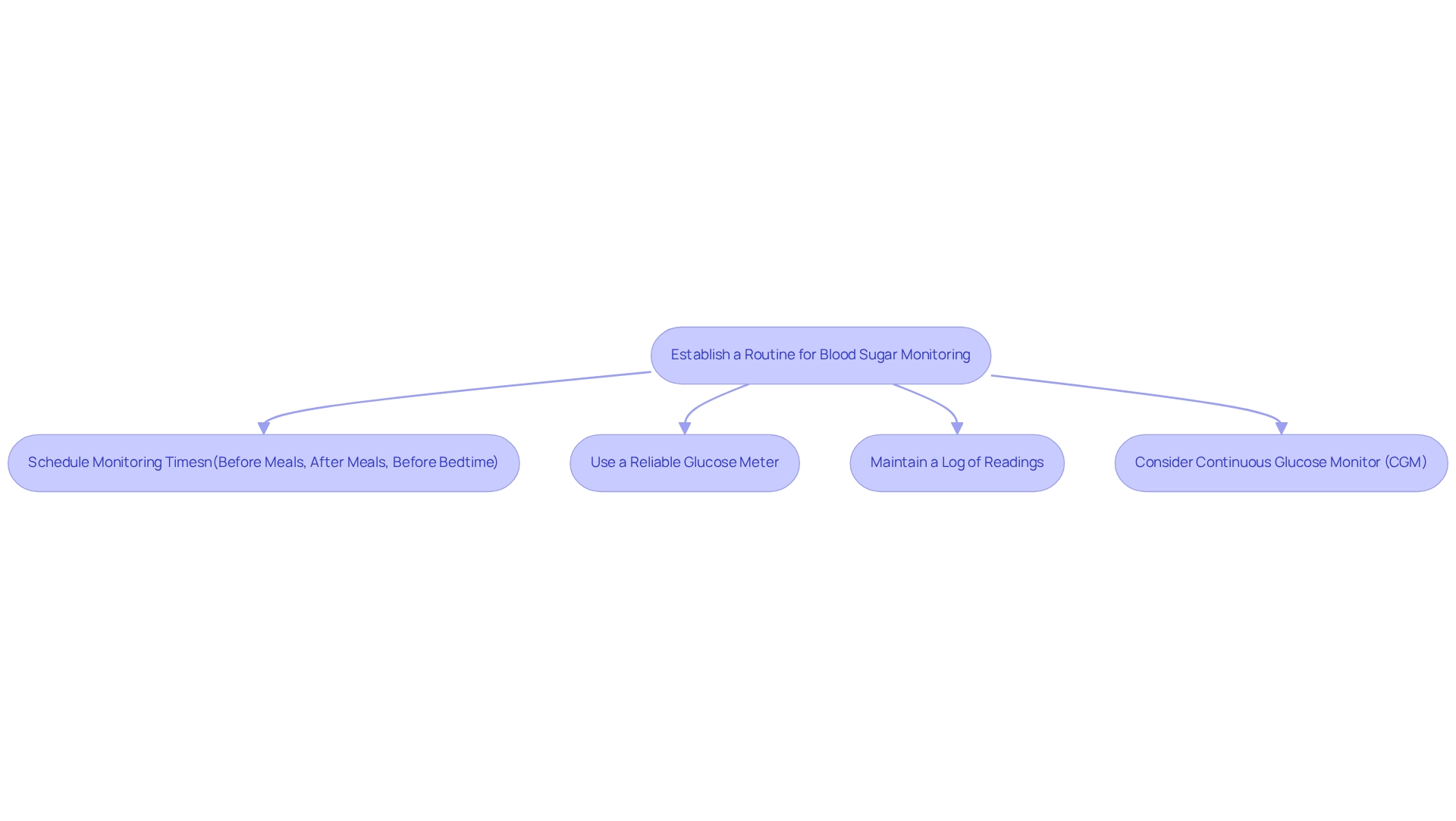
Establish a Routine for Blood Sugar Monitoring
It’s important to recognize that managing your glucose levels can be challenging. Scheduling specific times for checking your glucose, such as before meals, after meals, and before bedtime, can help create a consistent monitoring routine. Research shows that consistent monitoring can greatly enhance blood glucose levels in type 2 diabetes among individuals with this metabolic disorder. Many patients find that using a dependable glucose meter, calibrated accurately for precise readings, is crucial. After all, the effectiveness of your monitoring depends on the precision of the device used.
Maintaining a log of your readings is another helpful practice. This not only aids in identifying trends in blood glucose levels in type 2 diabetes over time but also facilitates meaningful discussions with your healthcare provider, enhancing your diabetes management strategy. Have you considered how this could impact your understanding of your health?
If suggested by your healthcare provider, you might think about utilizing a continuous glucose monitor (CGM) for real-time insights into your sugar levels. Devices like the Stelo CGM, which can be purchased for approximately $99 and are not included by insurance, can provide prompt feedback. Many individuals consider this essential for making informed choices regarding their well-being. Remember, taking these steps can empower you on your journey to better health.
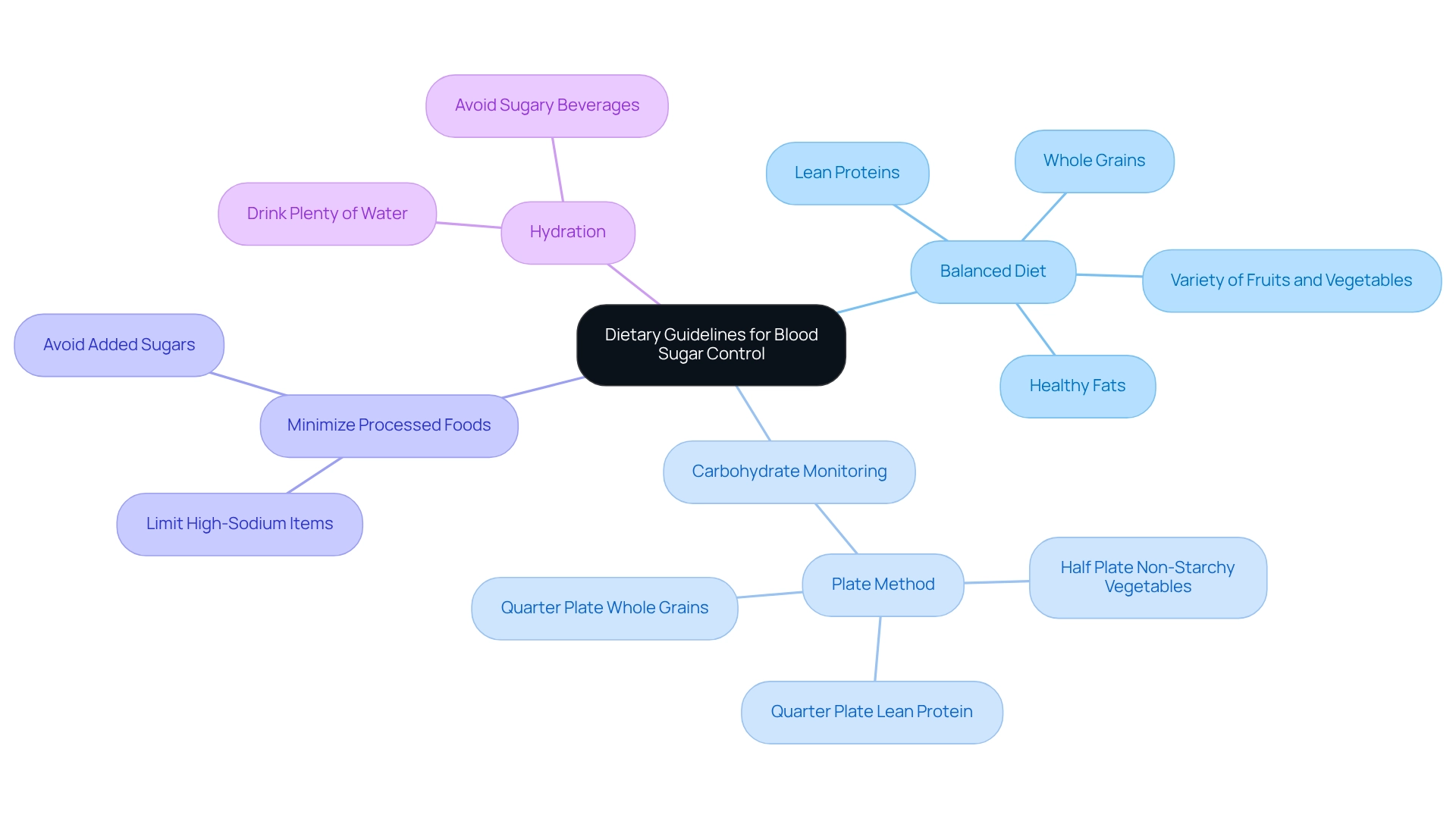
Adhere to Dietary Guidelines for Blood Sugar Control
- It’s essential to prioritize a balanced diet that includes whole grains, lean proteins, healthy fats, and a variety of fruits and vegetables. This approach not only supports your overall well-being but also plays a crucial role in regulating glucose levels. Dr. Jason Shumard‘s transformative diabetes care program has helped many individuals achieve significant improvements in their health, offering a compassionate path toward wellness.
- Monitoring carbohydrate intake is another vital step. Many find the plate method helpful: fill half your plate with non-starchy vegetables, a quarter with lean protein, and the remaining quarter with whole grains. This visual guide can assist you in maintaining balanced meals and stabilizing glucose levels, empowering you to take charge of your health and reduce reliance on medications.
- It’s important to minimize the consumption of processed foods, added sugars, and high-sodium items. These foods can lead to spikes in sugar levels, making it essential to opt for whole, nutrient-rich options. By making informed dietary choices, you can lower your risk of complications related to diabetes, including the potential risk of pancreatic cancer.
- Maintaining proper hydration is crucial. Drinking plenty of water and steering clear of sugary beverages supports your overall health and can aid in regulating blood sugar levels.
Research indicates that increasing understanding of dietary guidelines significantly enhances compliance among individuals with diabetes. A study from Debre Tabor General Hospital in Ethiopia highlighted the challenges faced by those with type 2 diabetes in adhering to dietary recommendations, revealing a concerning trend of poor eating habits. This underscores the necessity for comprehensive dietary education and resources to help individuals manage their diabetes effectively. By following these dietary recommendations, you can take proactive steps toward better blood sugar regulation and overall wellness. As Dr. Jason Shumard beautifully states, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can regain their wellness and well-being.” It’s also crucial to recognize that type 2 diabetes can increase the risk of pancreatic cancer, emphasizing the importance of effective management through adherence to these dietary guidelines.
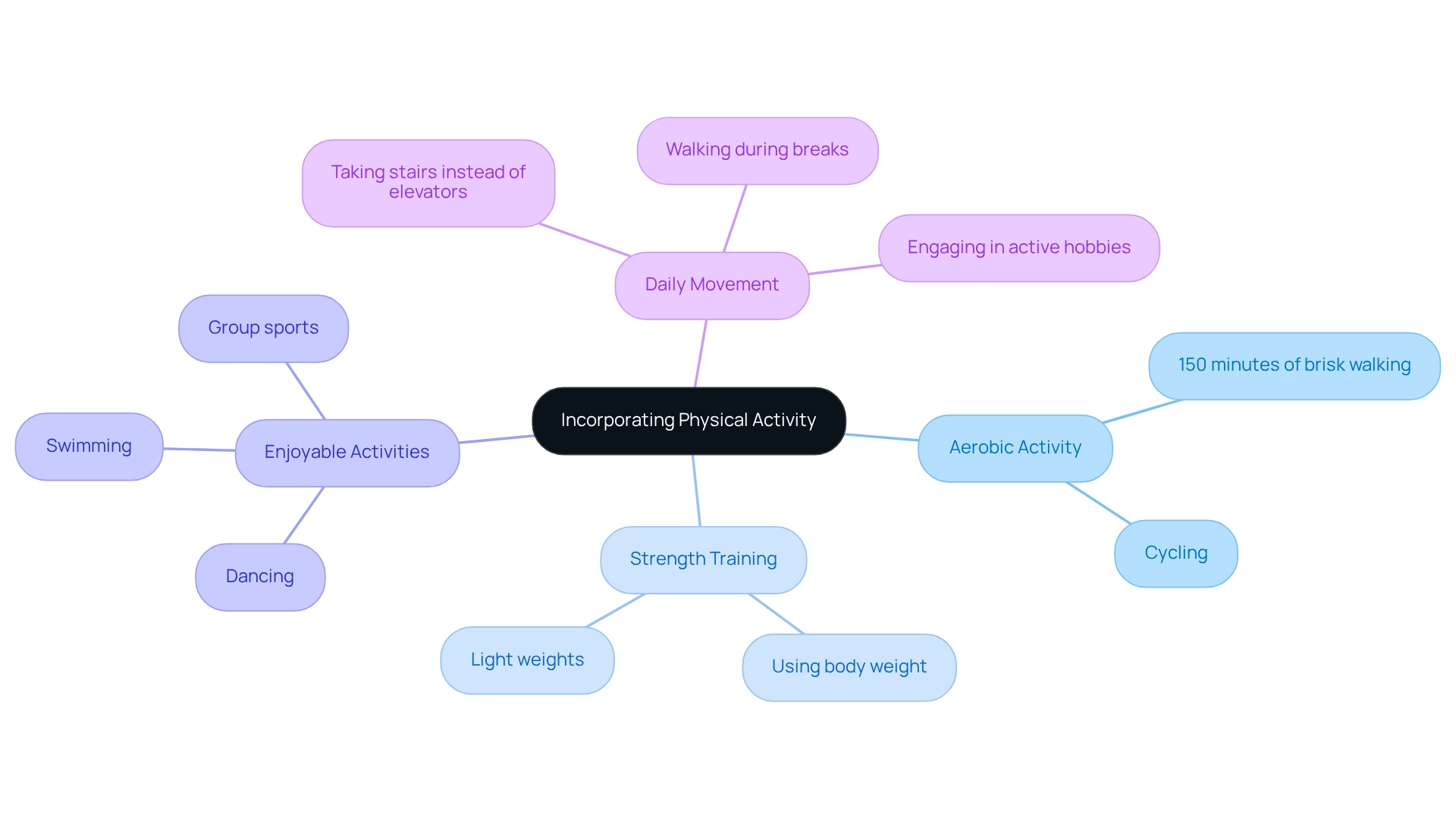
Incorporate Regular Physical Activity into Your Routine
It’s important to recognize that incorporating physical activity into your routine can feel challenging, especially when managing diabetes. Aim for at least 150 minutes of moderate-intensity aerobic activity each week, such as brisk walking or cycling. This can significantly improve your cardiovascular health and help regulate blood glucose levels in type 2 diabetes. To get started, refer to the walking program PDF for a structured method that can ease you into this new habit.
Many patients find that integrating strength training exercises at least twice a week is beneficial. These exercises can greatly enhance muscle mass and insulin sensitivity, which are crucial for effective diabetes management. Remember, strength training doesn’t have to be daunting; it can be as simple as using your own body weight or light weights.
Choosing enjoyable activities is key to fostering a consistent exercise routine. Think about options like dancing, swimming, or participating in group sports. These can make physical activity not only more appealing but also sustainable in the long run. What activities do you love that could get your body moving?
Select a safe and comfortable environment for your walks, whether indoors or outdoors, to ensure a positive experience. You can also incorporate movement into your daily life by opting for stairs instead of elevators, taking walks during breaks, or engaging in active hobbies. These small changes can collectively contribute to better management of blood glucose levels in type 2 diabetes. Remember, every little bit helps, and you’re not alone on this journey.
Conclusion
Taking control of diabetes is a journey that many people find challenging. It’s important to recognize that effective management involves multiple strategies, each playing a vital role. Establishing personalized target blood glucose levels in consultation with healthcare providers is essential. This lays the groundwork for monitoring progress and making necessary adjustments. Regularly tracking these levels, whether through traditional meters or continuous glucose monitors, empowers individuals to stay informed and proactive about their health.
Dietary choices are equally crucial in this process. Many patients find that emphasizing a balanced diet rich in whole grains, lean proteins, and a variety of fruits and vegetables can significantly influence blood sugar control. Understanding carbohydrate intake and minimizing processed foods can further enhance management efforts. Education on dietary guidelines is paramount, as it equips individuals with the knowledge needed to make informed choices that support their health.
Incorporating regular physical activity cannot be overlooked. Striving for at least 150 minutes of moderate-intensity exercise each week, along with strength training, fosters not only better blood glucose levels but also overall well-being. Finding enjoyable activities can transform exercise from a chore into a sustainable and fulfilling part of daily life.
Ultimately, managing diabetes effectively requires a holistic approach that combines monitoring, nutrition, and physical activity. By embracing these strategies, individuals can take meaningful steps toward improved health outcomes, reclaiming control over their lives and well-being. A proactive mindset, supported by education and lifestyle changes, is instrumental in navigating the complexities of diabetes management. Remember, you are not alone on this journey, and every small step you take is a step toward a healthier future.
Frequently Asked Questions
What are the target blood glucose levels for managing type 2 diabetes?
The target blood glucose levels for type 2 diabetes are typically advised to be between 80-130 mg/dL before meals and under 180 mg/dL after meals.
Why is it important to track blood glucose levels?
Keeping a detailed record of your blood glucose levels is crucial as it allows you to monitor your progress towards your target levels, identify patterns, and inform any necessary adjustments in your management plan.
Can target blood glucose levels be adjusted?
Yes, many patients may need to adjust their targets based on their healthcare provider’s guidance and individual health objectives. Personalization is key as each person’s needs may vary.
What tools can help in monitoring blood glucose levels?
Using a glucose meter or a continuous glucose monitor (CGM) can greatly assist in regularly checking blood glucose levels. The American Diabetes Association suggests CGMs for adults with type 2 diabetes to help monitor levels effectively.
How does a continuous glucose monitor (CGM) benefit diabetes management?
A CGM provides real-time data that can improve management strategies, making it easier for individuals to stay on track with their blood glucose levels.
Who should I consult to determine my target blood glucose levels?
It is important to consult with your healthcare provider to determine your specific target blood glucose levels for effective diabetes management.