Overview
Managing blood glucose levels can feel overwhelming for individuals with Type 2 diabetes. It’s important to recognize that you’re not alone in this journey. The article outlines four essential steps to help you navigate this challenge:
- Understanding normal glucose levels
- Establishing a testing routine
- Implementing dietary guidelines
- Incorporating regular physical activity
Each step is backed by evidence and practical strategies. For instance, many patients find that a balanced diet and regular monitoring are crucial to their success. Engaging in exercise not only benefits your body but also empowers you to take control of your health and improve your overall well-being. Remember, these steps are not just guidelines; they are tools to help you thrive on your path to better health. You have the strength to make these changes, and support is available every step of the way.
Introduction
In the realm of diabetes management, it’s important to recognize that understanding and maintaining normal blood glucose levels is paramount for promoting overall health and preventing complications. Many individuals face rising costs associated with diabetes care, making effective strategies more crucial than ever.
By establishing consistent blood sugar testing routines and adopting a balanced diet rich in whole foods, you can take proactive steps toward controlling your glucose levels. Engaging in regular physical activity not only enhances insulin sensitivity but also fosters a sense of community and motivation.
This article explores actionable insights and practical tools that empower you to reclaim your health, navigate your diabetes journey, and ultimately improve your quality of life.
Understand Normal Blood Glucose Levels
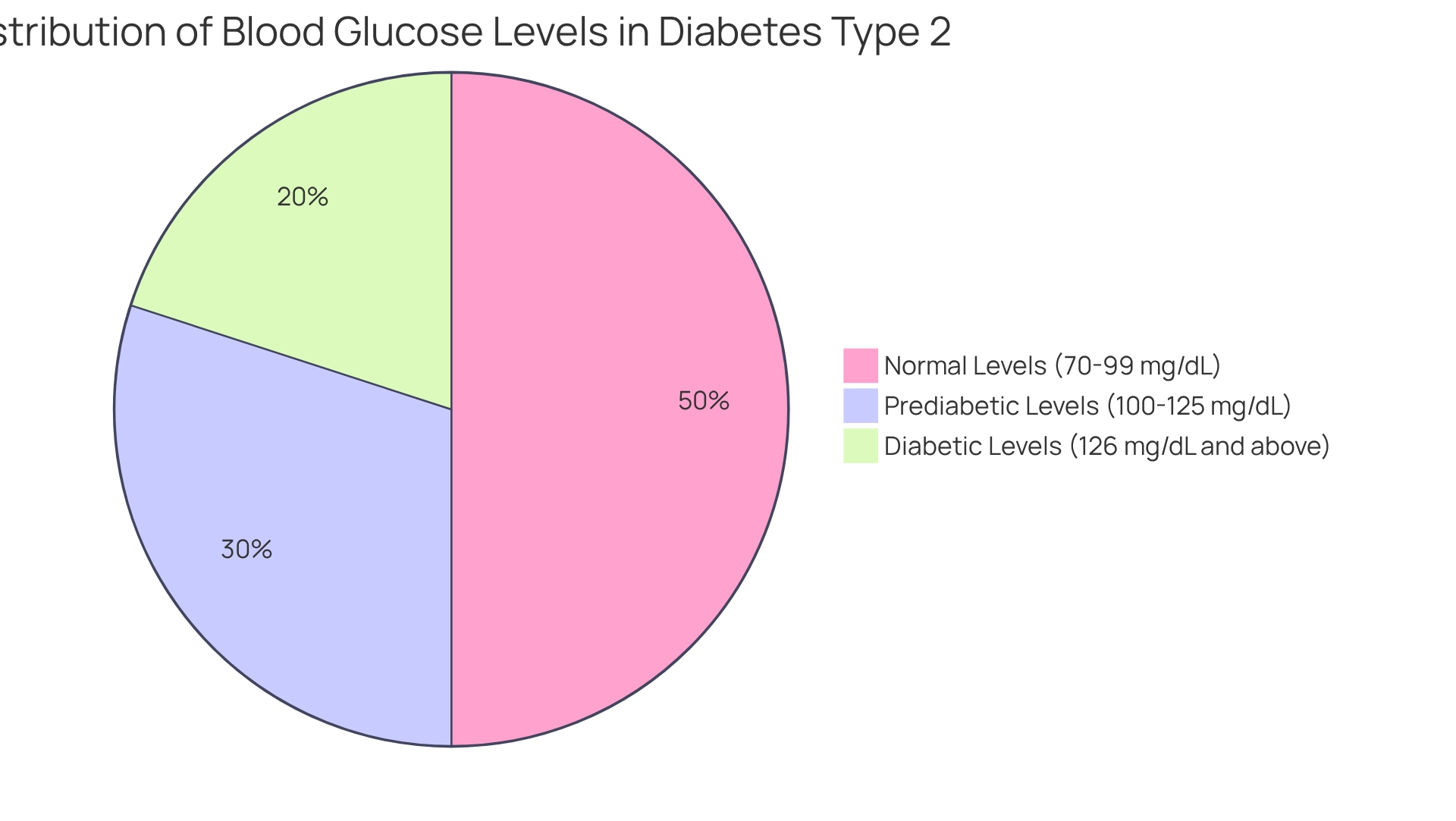
Understanding typical fasting sugar readings is crucial for effectively managing blood sugar conditions. The standard range for blood glucose levels for diabetes type 2 is 70-99 mg/dL (3.9-5.5 mmol/L), while post-meal sugar concentrations for individuals with the condition should ideally remain below 180 mg/dL (10.0 mmol/L). By consistently examining charts of blood glucose levels for diabetes type 2, patients can differentiate among normal, prediabetic, and diabetic ranges, which empowers them to make informed choices.
As we move into 2025, maintaining typical fasting sugar readings is more important than ever. The rising healthcare costs associated with high blood sugar have significantly increased, from $10,179 to $12,022 per individual between 2012 and 2022. This financial burden highlights the urgent need for effective management strategies.
Effective methods for sustaining normal fasting blood glucose levels for diabetes type 2 include incorporating regular physical activity. Many patients find that 31.9% of adults with this condition report being physically inactive. Engaging in outdoor activities, like walking or hiking in the beautiful parks and trails of San Marcos, can greatly improve insulin sensitivity and help manage sugar levels. This reinforces the importance of promoting physical activity as a vital component of managing and preventing blood glucose levels for diabetes type 2.
Additionally, embracing a balanced diet rich in local produce is essential for controlling blood glucose levels for diabetes type 2. San Marcos offers vibrant farmers’ markets where you can discover fresh, nutritious options such as avocados and berries, which are beneficial for sugar regulation. These foods are packed with fiber and nutrients, which can help support overall health and regulate blood glucose levels for diabetes type 2.
Stress management techniques, such as yoga and meditation, are also critical for maintaining blood sugar levels. Many find that participating in these activities can help reduce stress, which is essential for maintaining stable blood glucose levels for diabetes type 2.
It’s essential to consult with healthcare providers to establish personalized target ranges based on individual health status. Dr. Jason Shumard, an expert in functional medicine, emphasizes the importance of tailored nutrition and lifestyle modifications. He notes, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being.” Specialist insights highlight that understanding and regulating blood glucose levels for diabetes type 2 can lead to improved health outcomes for individuals. By equipping patients with actionable insights and practical tools, they can take charge of their health and well-being.
Establish a Blood Sugar Testing Routine
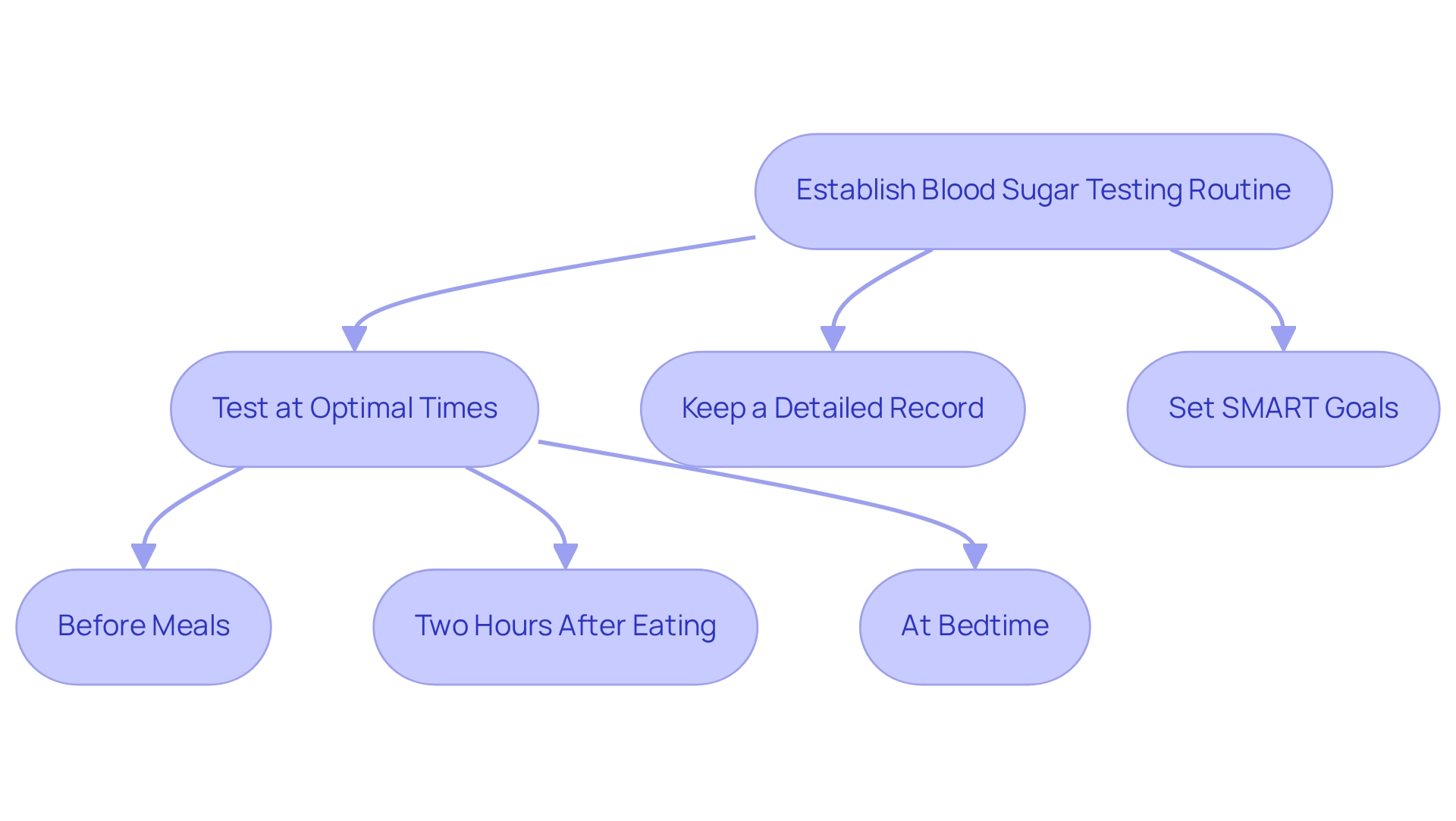
Managing your sugar readings can feel overwhelming, but creating a testing schedule can truly make a difference. Have you considered testing your levels at optimal times, like before meals, two hours after eating, and at bedtime? This approach helps you gain a comprehensive understanding of your levels throughout the day. Regular checks of blood glucose levels for diabetes type 2 are essential for effective management. Many patients find that using a mix of tracking methods—like fitness apps, journals, and pedometers—can enhance their monitoring experience.
It’s important to have a reliable glucose meter and ensure that all your essential supplies, such as test strips and lancets, are readily available. Keeping a thorough record of your readings, whether through a journal or an app, can assist you in recognizing trends over time that can help manage blood glucose levels for diabetes type 2. This awareness can guide your treatment choices and conversations with your healthcare provider about managing blood glucose levels for diabetes type 2. Consider implementing SMART goals—specific, measurable, attainable, relevant, and time-bound. For instance, you might set a goal to check your glucose readings regularly at the specified times for a month.
Consulting with your healthcare provider is key to determining the right frequency of testing for blood glucose levels for diabetes type 2 in your individual treatment plan. Recommendations may vary based on your specific needs and goals. For those on long-acting insulin, measuring sugar levels twice daily is usually sufficient. According to the American Diabetes Association, your doctor may have different goals in mind for you, highlighting the importance of personalized care. By focusing on goal-setting and regular progress monitoring, you can cultivate a sense of accomplishment and stay engaged in your health management journey.
Key Tips for Effective Monitoring:
- Test your glucose at optimal times.
- Keep a detailed record of your readings.
- Set SMART goals to stay motivated.
Remember, you’re not alone in this journey. Many have walked this path and found success by taking small, manageable steps. It’s all about finding what works best for you!
Implement Dietary Guidelines for Blood Sugar Control
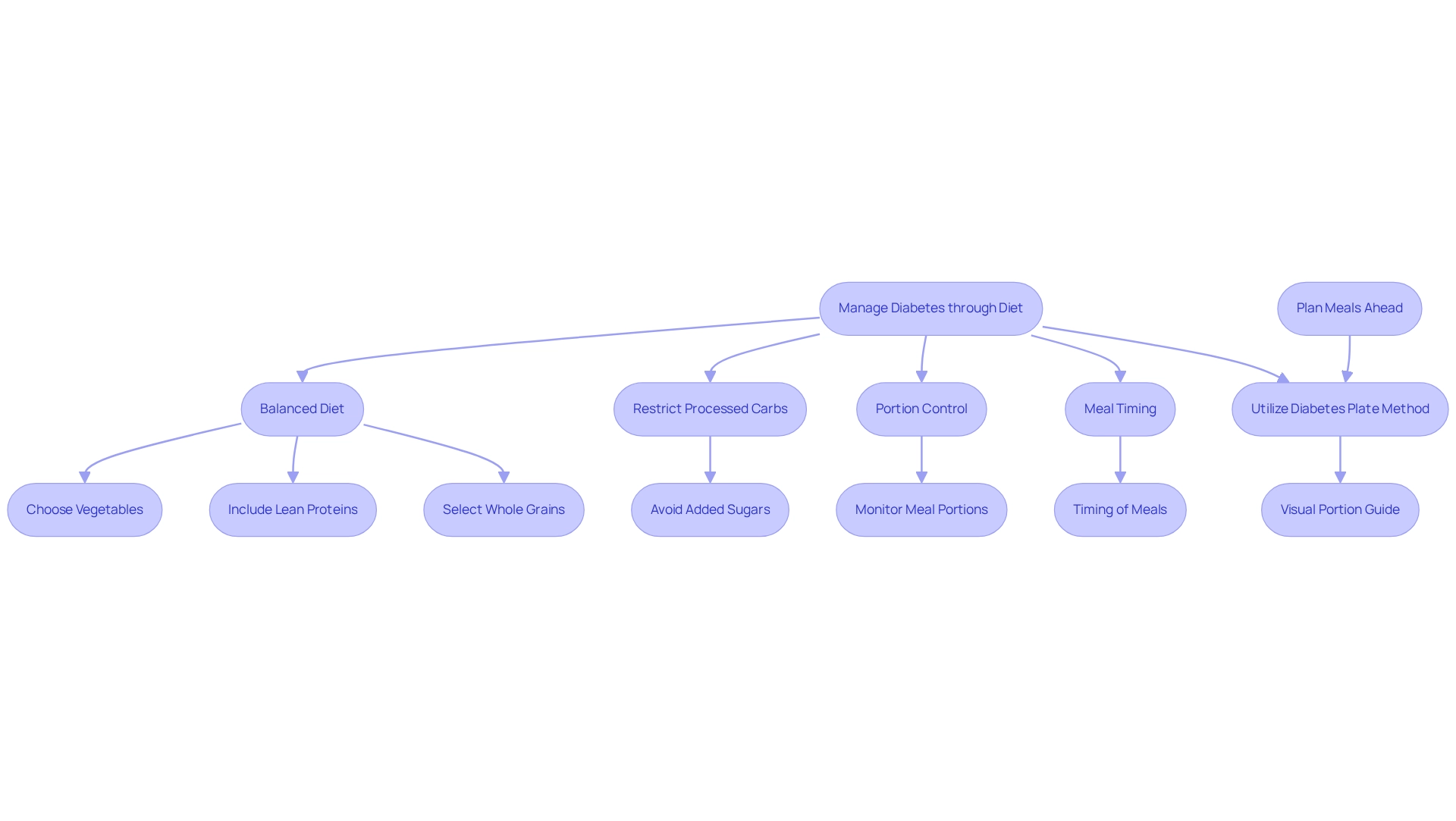
Managing diabetes can be challenging, but a balanced diet rich in whole foods—like vegetables, lean proteins, and whole grains—plays a crucial role in maintaining healthy blood glucose levels for diabetes type 2. It’s important to recognize that research shows a modest correlation of 0.29 between diet-attributable type 2 health issues and diet quality, emphasizing the significance of our dietary choices.
Many patients find that restricting processed carbohydrates and added sugars can significantly help. These foods often lead to spikes in glucose concentrations, making it more complicated to manage blood glucose levels for diabetes type 2. By applying portion control and being mindful of meal timing, you can help maintain stable blood glucose levels for diabetes type 2 throughout the day, thereby reducing the risk of fluctuations.
Consider utilizing meal planning strategies, such as the Diabetes Plate method, to effectively manage blood glucose levels for diabetes type 2. This approach simplifies healthy eating by visually guiding portion sizes and food choices, making it easier to stay on track. The center offers valuable educational resources, including books and seminars, to empower you with actionable insights and practical tools for managing your diabetes effectively.
As Dr. Jason Shumard states, ‘By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their health and well-being, ultimately leading to improved quality of life and reduced reliance on conventional medical interventions.’ This holistic approach not only addresses dietary needs but also empowers you to take control of your health.
Transformative experiences from Dr. Jason Shumard’s 30-Day Diabetes Reset program highlight how many individuals have successfully eliminated their dependency on insulin and achieved significant health improvements. Remember, you are not alone in this journey, and with the right support and strategies, a healthier life is within reach.
Incorporate Regular Physical Activity
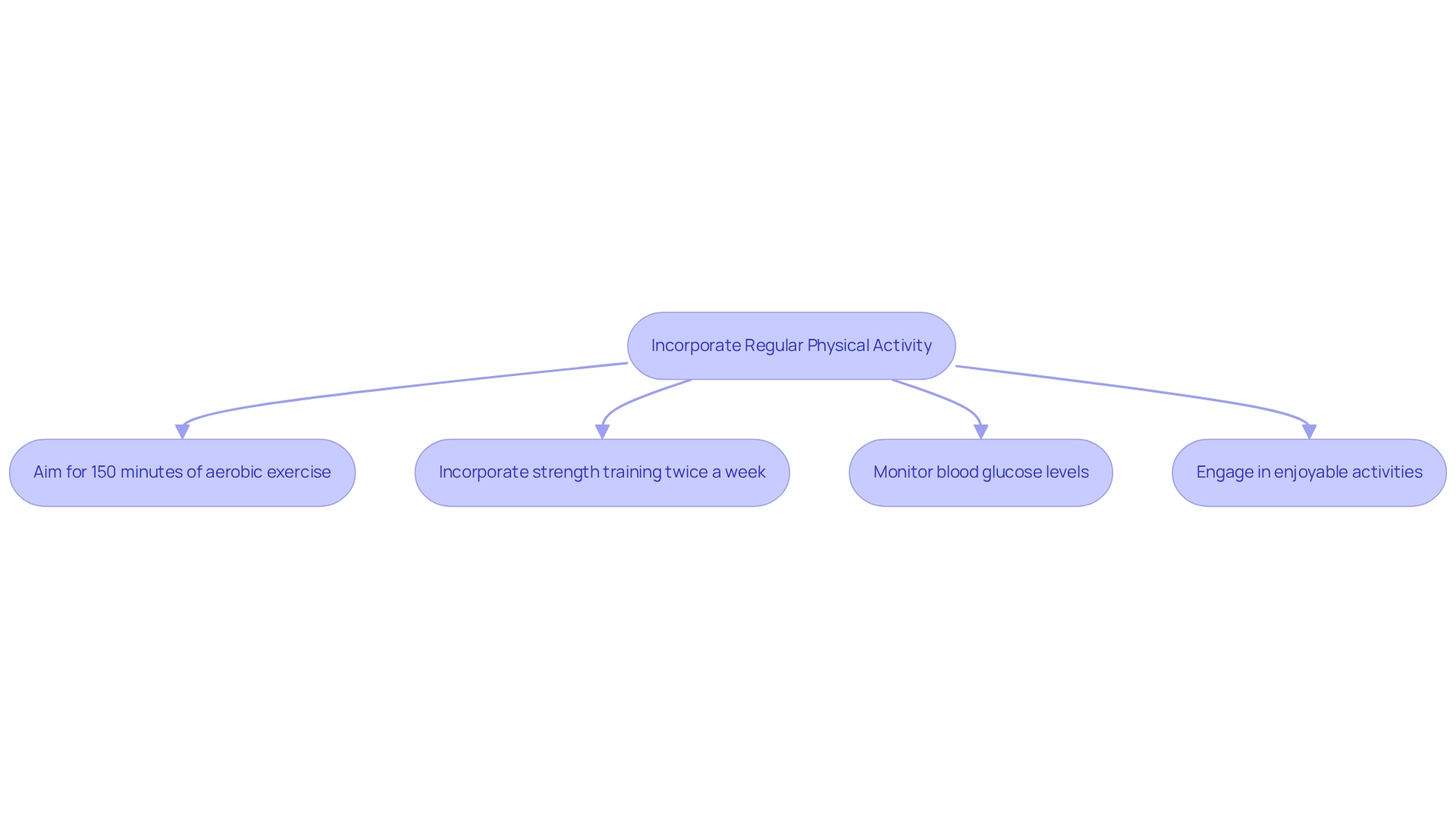
Aim for at least 150 minutes of moderate-intensity aerobic exercise each week, such as brisk walking or cycling. This can significantly enhance the control of blood glucose levels for diabetes type 2. Have you considered starting a walking routine? Utilizing the structured methods outlined in the walking program PDF can be a great first step. Begin by assessing your current fitness level and setting achievable goals, like dedicating 10-15 minutes to a daily walk. Many patients find that even small changes can lead to big improvements. Studies indicate that replacing sedentary time with standing for 2.5 hours per day can enhance insulin sensitivity even more than structured cycling activities.
Incorporating strength training exercises at least two days a week is also beneficial. Not only does this build muscle mass, but it plays a crucial role in improving insulin sensitivity, which is vital for effective diabetes management. It’s important to consistently check your blood glucose levels for diabetes type 2 before and after exercising. Understanding how various activities influence your body can help you tailor your routine to optimize blood glucose levels for diabetes type 2.
Engaging in enjoyable activities can significantly boost your adherence to an exercise regimen. Options like dancing, swimming, or group classes can make physical activity more appealing and sustainable. Are there any activities you love? Addressing barriers to physical activity is essential, so consider seeking support or resources that encourage participation. Joining a hiking group or partnering with a friend can enhance accountability and enjoyment, making it easier to stick to your routine. Overcoming these challenges is key to maximizing the benefits of exercise in managing blood glucose levels for diabetes type 2.
Conclusion
Maintaining normal blood glucose levels is essential for effective diabetes management and overall well-being. It’s important to recognize that understanding the ideal ranges for fasting and post-meal glucose levels empowers you to make informed decisions about your health. With the rising costs of diabetes care, many find that implementing strategies such as:
- Regular physical activity
- A balanced diet
- Stress management
becomes crucial. Engaging in outdoor activities and consuming nutrient-rich foods can significantly enhance insulin sensitivity and improve blood sugar control.
Establishing a consistent blood sugar testing routine is another vital component of effective management. By identifying optimal testing times and utilizing various tracking methods, you can gain valuable insights into your glucose patterns. Setting SMART goals and working closely with healthcare providers ensures a personalized approach to diabetes care, fostering a sense of achievement and engagement in your health journey.
Furthermore, adhering to dietary guidelines and incorporating regular physical activity are key for maintaining stable blood sugar levels. A holistic approach that combines balanced nutrition with enjoyable exercise not only improves health outcomes but also enhances your quality of life. As you reclaim your health through actionable insights and practical tools, you pave the way for a more empowered and fulfilling diabetes management experience. Taking proactive steps today can lead to lasting benefits for tomorrow, transforming your diabetes journey into one of hope and resilience.
Frequently Asked Questions
What are the normal blood glucose levels for individuals with type 2 diabetes?
The standard range for fasting blood glucose levels for individuals with type 2 diabetes is 70-99 mg/dL (3.9-5.5 mmol/L). Post-meal sugar concentrations should ideally remain below 180 mg/dL (10.0 mmol/L).
Why is it important to understand blood glucose levels?
Understanding blood glucose levels is crucial for effectively managing blood sugar conditions, allowing patients to differentiate among normal, prediabetic, and diabetic ranges, which empowers them to make informed health choices.
How have healthcare costs related to high blood sugar changed recently?
Between 2012 and 2022, healthcare costs associated with high blood sugar have increased significantly, from $10,179 to $12,022 per individual, highlighting the urgent need for effective management strategies.
What methods can help maintain normal fasting blood glucose levels?
Effective methods include incorporating regular physical activity, such as walking or hiking, adopting a balanced diet rich in local produce, and practicing stress management techniques like yoga and meditation.
What role does physical activity play in managing blood glucose levels?
Engaging in regular physical activity can greatly improve insulin sensitivity and help manage blood sugar levels, as many individuals with type 2 diabetes report being physically inactive.
What dietary options are beneficial for controlling blood glucose levels?
A balanced diet rich in local produce, such as avocados and berries, is essential for controlling blood glucose levels, as these foods are packed with fiber and nutrients that support overall health.
How important is stress management for blood glucose control?
Stress management techniques, such as yoga and meditation, are critical for maintaining stable blood glucose levels, as reducing stress is essential for effective blood sugar regulation.
Should individuals consult healthcare providers regarding their blood glucose management?
Yes, it is essential to consult with healthcare providers to establish personalized target ranges based on individual health status and to receive tailored nutrition and lifestyle modifications.