Overview
The article titled “10 Key Insights on Type 1 & 2 Diabetes Management” seeks to offer essential guidance for effectively managing both types of diabetes. It’s important to recognize that successful management involves understanding the unique characteristics of each type. Many patients find that making lifestyle changes, such as adopting a healthier diet and incorporating regular exercise, can significantly improve their well-being. Additionally, utilizing available educational resources empowers individuals to take control of their health and enhance their quality of life.
By focusing on these key insights, we aim to nurture a supportive environment that encourages individuals to embrace their journey toward better health. Remember, you are not alone in this process; many have walked this path and found success. Together, we can foster a community of understanding and encouragement, guiding each other toward a healthier future.
Introduction
In a world where diabetes affects millions, it’s important to recognize the struggles that many individuals face. Understanding the nuances between Type 1 and Type 2 diabetes is crucial for effective management and prevention. The Integrative Wellness Center offers a holistic approach to diabetes care, featuring programs that empower individuals to take charge of their health through education, lifestyle changes, and community support.
Many patients find that by exploring the underlying mechanisms, symptoms, treatment differences, and long-term complications associated with each type, they can uncover transformative strategies that lead to lasting health improvements. With expert guidance and a focus on personalized care, individuals can navigate their diabetes journey with confidence and resilience, ultimately reclaiming their well-being.
Are you ready to take the first step towards a healthier future?
Integrative Wellness Center: 30-Day Diabetes Reset Program for Lasting Health Transformation
Are you or someone you know struggling with type 1 & 2 diabetes? The 30-Day Diabetes Reset Program at the Integrative Wellness Center offers a compassionate approach to help you take charge of your health. This transformative method is designed to empower you to manage your condition effectively.
With a blend of nutritional education, physical activity, and behavioral coaching, this extensive program provides the tools you need to rejuvenate your metabolic well-being. Many participants discover that focusing on whole foods, balanced meals, and regular exercise helps stabilize their blood sugar levels while also renewing their energy.
It’s important to recognize that support is key. The program offers ongoing assistance through seminars and educational resources, ensuring you have a community backing you in your journey toward lasting health transformation. Under the caring guidance of Dr. Jason Shumard, who brings nearly two decades of experience in helping patients recover from type 1 & 2 diabetes, this program stands as a beacon of hope. If you’re ready to reclaim your well-being, the 30-Day Diabetes Reset Program could be the first step toward a healthier, more vibrant life.
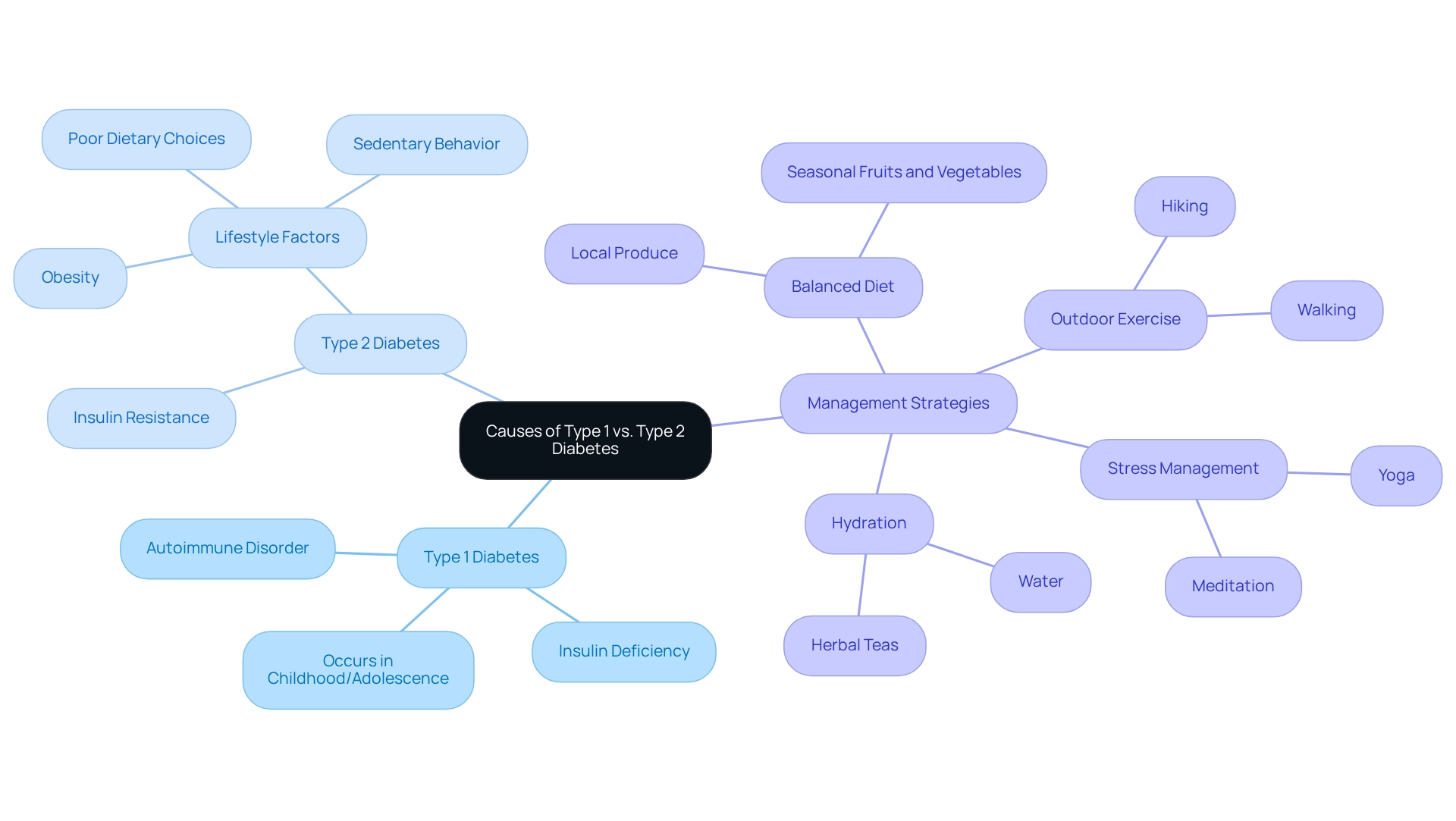
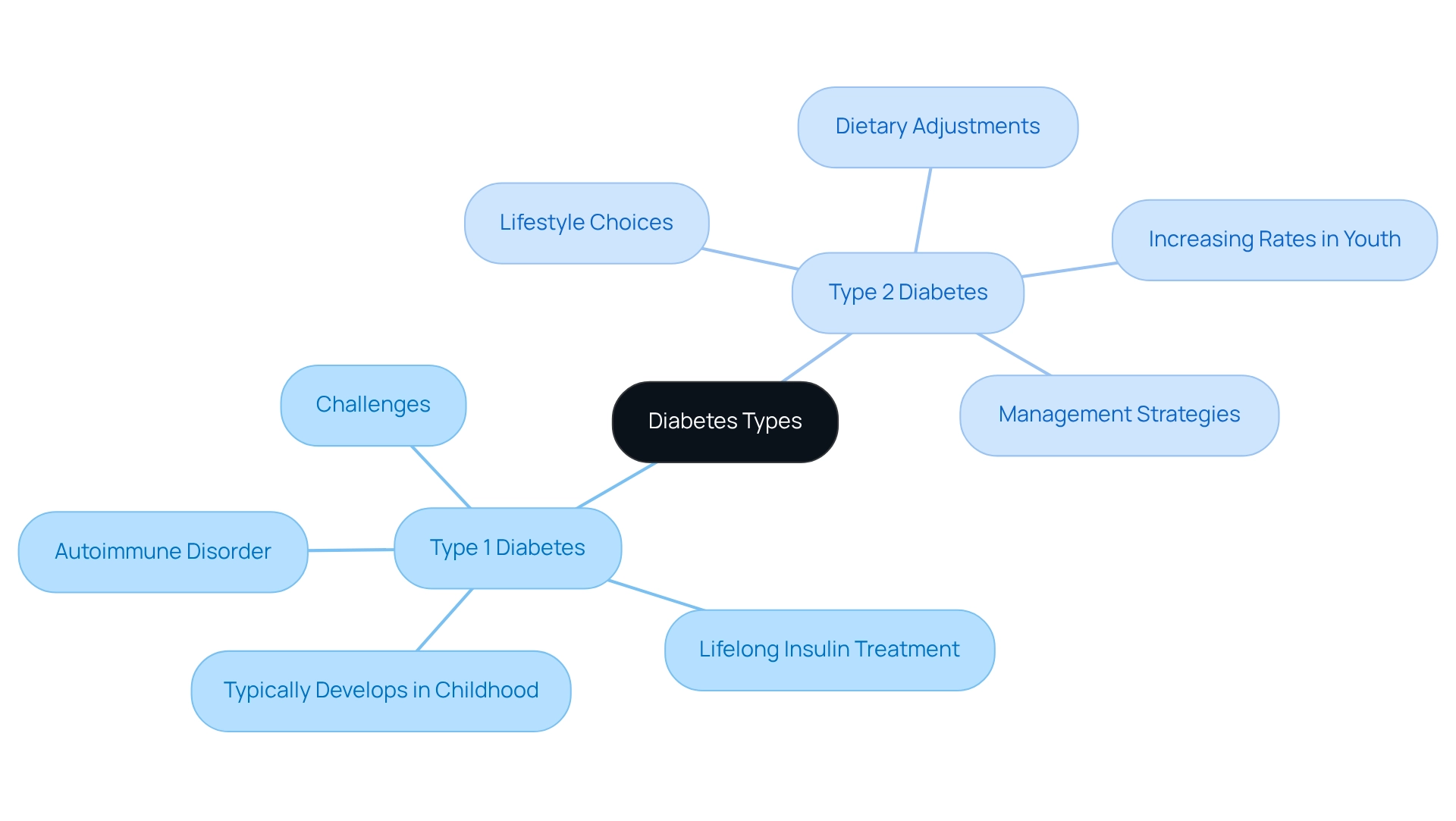
Causes of Type 1 vs. Type 2 Diabetes: Understanding the Underlying Mechanisms
Type 1 & 2 diabetes is fundamentally an autoimmune disorder, where the immune system mistakenly targets and destroys the insulin-producing beta cells in the pancreas, leading to a critical insulin deficiency. This type of condition usually appears during childhood or adolescence. On the other hand, type 1 & 2 diabetes is marked by insulin resistance, particularly in type 2 diabetes, where the body’s cells do not respond sufficiently to insulin. This condition is frequently associated with lifestyle factors such as obesity, sedentary behavior, and poor dietary choices.
It’s important to recognize that understanding these differences is crucial for creating effective management approaches tailored to each type, particularly in San Marcos, CA, where managing type 1 & 2 diabetes can be greatly improved through comprehensive lifestyle strategies. Embracing a balanced diet rich in local produce, engaging in regular outdoor exercise, and participating in community wellness programs can empower individuals to take control of their health. For instance, many patients find that incorporating seasonal fruits and vegetables from local farmers’ markets supports blood sugar regulation. Outdoor activities like hiking and walking can improve insulin sensitivity and overall well-being. Furthermore, focusing on hydration by choosing water or herbal teas and managing stress through methods such as yoga or meditation can further assist in maintaining healthy blood sugar levels.
Recent studies show that insulin resistance accounts for around 92% of cases among insured adults in the U.S., emphasizing its commonality and the pressing necessity for specific interventions. Moreover, ongoing studies into the autoimmune mechanisms underlying type 1 & 2 diabetes continue to illuminate the intricacies of both conditions, highlighting the significance of tailored treatment strategies. By acknowledging the distinct causes and traits of each type, particularly type 1 & 2 diabetes, healthcare providers can enhance their support for patients in effectively managing their conditions.
For individualized guidance and assistance tailored to your specific needs, consider reaching out to Dr. Jason Shumard in San Marcos, CA. He is committed to helping you navigate your health management journey with care and expertise. Remember, taking that first step can lead to a healthier, more fulfilling life.
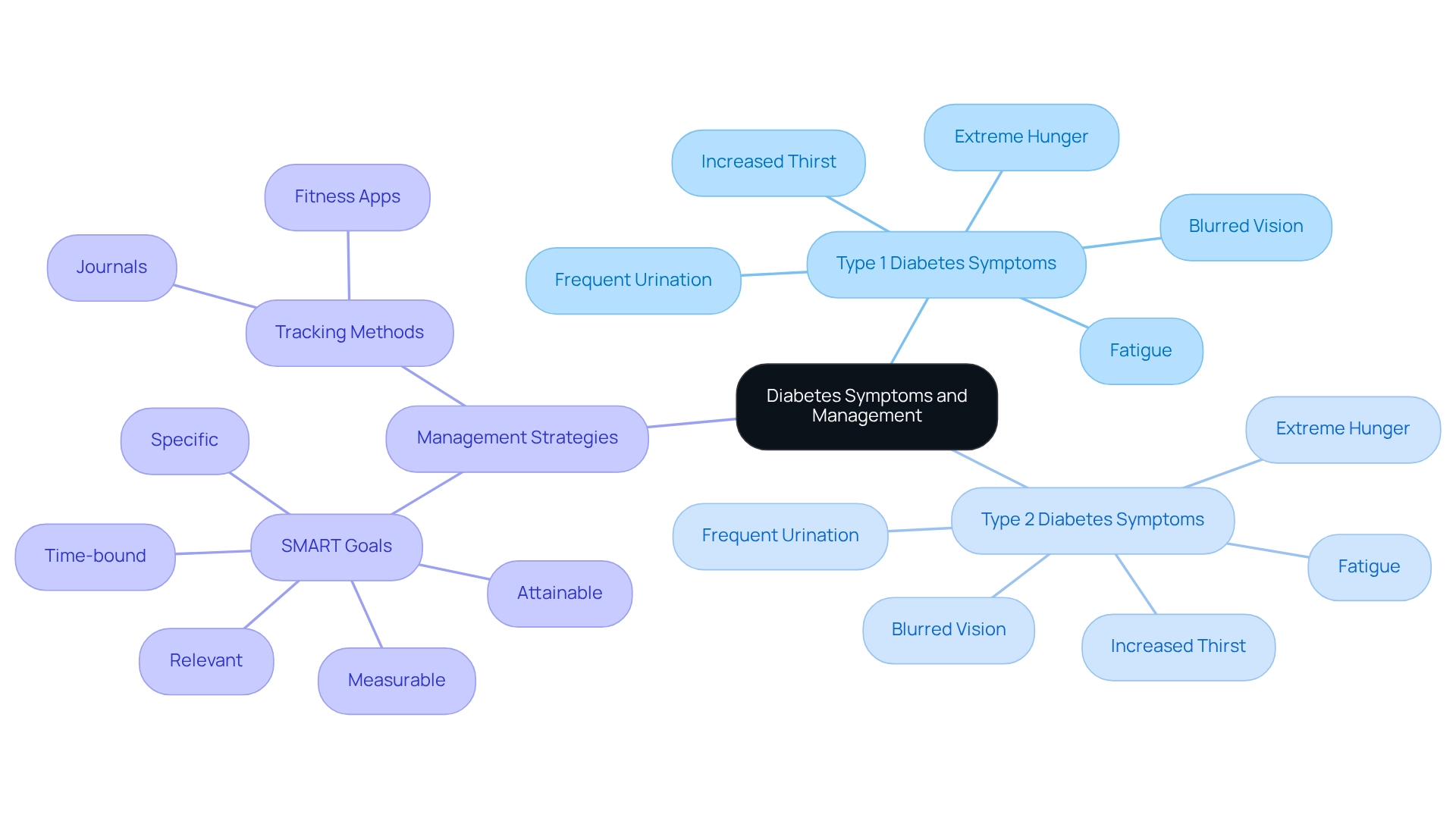
Symptoms of Type 1 and Type 2 Diabetes: Key Indicators to Recognize
Living with type 1 & 2 diabetes can be challenging, and it’s important to recognize the common symptoms that both types of the condition present. Increased thirst, frequent urination, extreme hunger, fatigue, and blurred vision are all signs to watch for. Many patients find that the emergence of insulin-dependent symptoms can happen quickly, which may lead to severe complications like diabetic ketoacidosis if not managed promptly. In contrast, type 2 symptoms often develop gradually, making them less noticeable and potentially leading to delayed diagnosis. This gradual onset highlights the critical need for regular screening to facilitate early detection.
Identifying these symptoms is crucial for everyone living with diabetes. Prompt intervention can greatly enhance management results, enabling individuals to lead full, active lives. Data suggest that those with well-managed diabetes can enjoy a quality of life similar to those free from the condition. This emphasizes the significance of awareness and preventive care in your journey.
To enhance your management, consider implementing effective tracking methods like fitness apps and journals. Setting SMART goals—specific, measurable, attainable, relevant, and time-bound—can also be incredibly beneficial. This structured approach not only fosters accountability but allows for the adaptation of goals as your health conditions change. By identifying symptoms and establishing suitable objectives, you can more effectively control your condition and enhance your overall health. Remember, you are not alone in this journey, and taking these steps can lead you toward a healthier future.
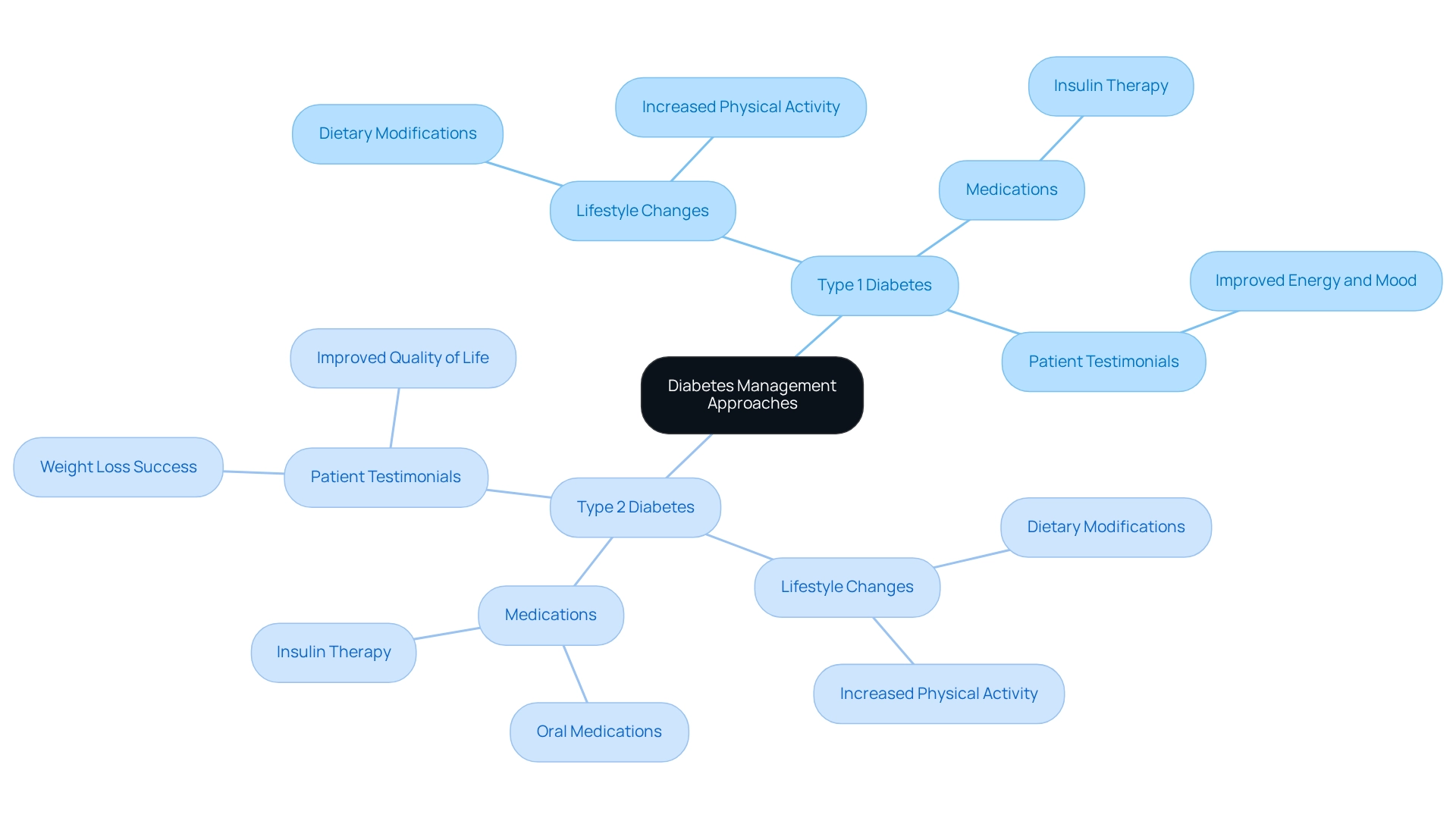
Treatment Approaches: How Type 1 and Type 2 Diabetes Are Managed Differently
Managing type 1 & 2 diabetes is a lifelong journey that requires consistent insulin treatment, especially for those who cannot produce insulin on their own. Regular blood glucose monitoring, along with thoughtful adjustments in diet and lifestyle, plays a crucial role in maintaining optimal blood sugar levels. For those managing type 1 & 2 diabetes, the journey often begins with lifestyle changes, such as dietary modifications and increased physical activity. Many patients find that these initial steps can lead to significant improvements; studies show that 20.9% of patients in specialist services achieved all three treatment targets through lifestyle interventions alone. As the condition evolves, some may need oral medications or insulin therapy to effectively manage their blood sugar levels.
It’s important to recognize that understanding these differences is vital for both patients and healthcare providers when developing personalized management plans. For instance, case studies reveal that comprehensive treatment approaches targeting the root causes of type 2 diabetes can lead to improved well-being. One patient shared, “I was depressed, no energy, and had insomnia… I have lost 55 lbs. My A1C started at 9.1 after 8 months it is now 5.7.” Another noted, “I feel so much better… I lost a lot of weight, have more energy and feel great. I am not depressed anymore and I don’t need my meds anymore!” These heartfelt testimonials underscore the transformative power of lifestyle changes and personalized care.
Moreover, specialists in blood sugar management emphasize that lifestyle changes are essential for effectively managing both type 1 & 2 diabetes. These adjustments not only enhance quality of life but also reduce reliance on traditional medical treatments. Dr. Jason Shumard advocates for this comprehensive viewpoint, highlighting the importance of individualized support and education in achieving lasting health improvements. Furthermore, the development of intermittently scanned CGM (isCGM) offers a more affordable option for glucose monitoring, further expanding treatment choices for individuals facing blood sugar management challenges.
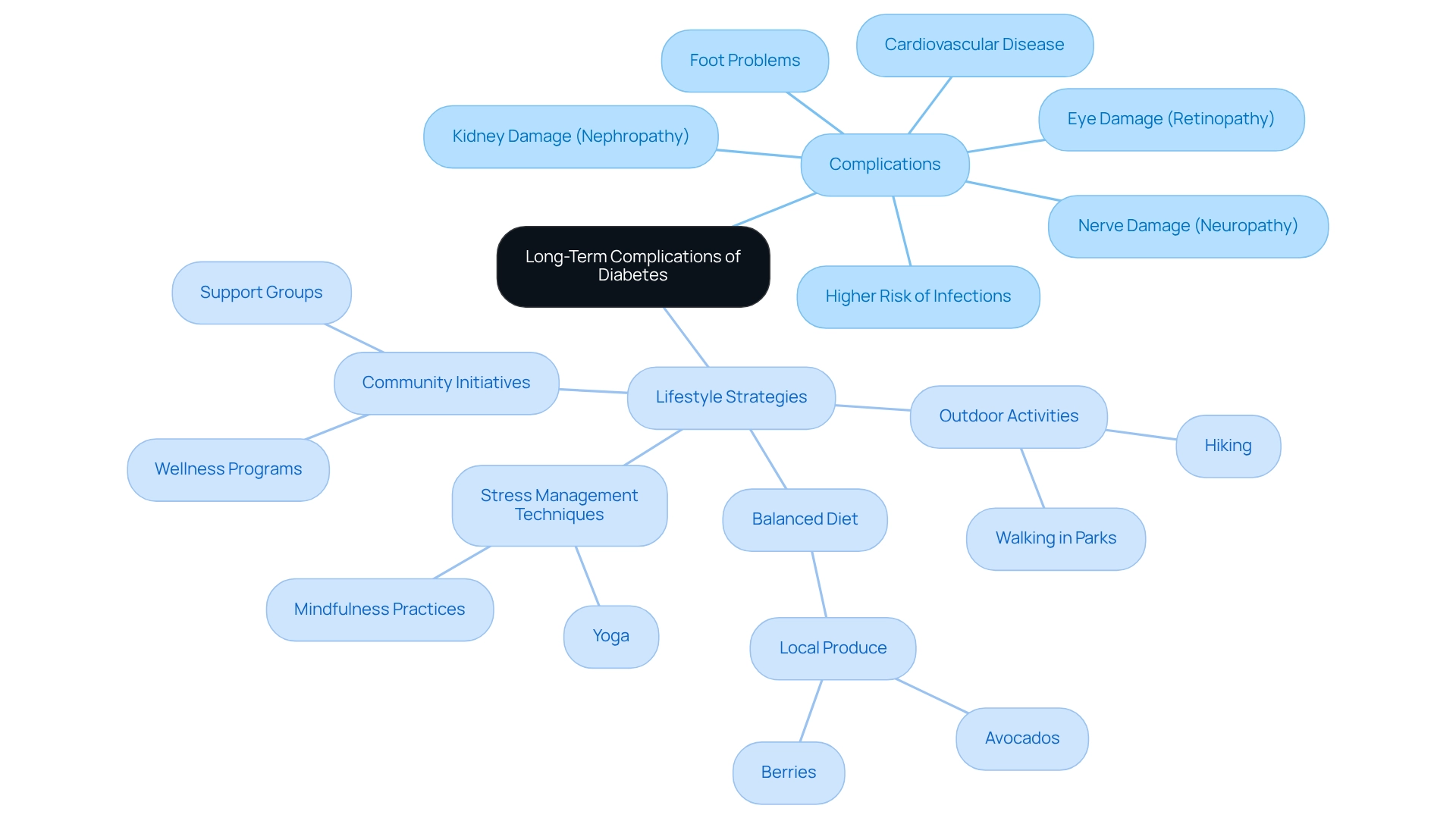
Long-Term Complications: Risks Associated with Type 1 and Type 2 Diabetes
It’s important to recognize that both type 1 & 2 diabetes can lead to serious long-term complications if not managed effectively. These complications may include cardiovascular disease, nerve damage (neuropathy), kidney damage (nephropathy), eye damage (retinopathy), and foot problems. Individuals with diabetes often face a higher risk of infections and slower healing. However, many patients find that adopting a holistic lifestyle approach can significantly reduce these risks.
Engaging in regular outdoor exercise, such as hiking or walking in local parks, can be a wonderful way to enhance insulin sensitivity and help control blood sugar levels. Imagine the joy of enjoying nature while taking care of your health! A balanced diet rich in local produce, like avocados and berries, promotes overall well-being and assists in blood sugar regulation.
Moreover, participating in community wellness initiatives can offer vital assistance and resources tailored for managing blood sugar conditions. Have you considered joining a local group? Stress management techniques, such as yoga and mindfulness practices, can further contribute to better health outcomes. Consistent observation and control of blood sugar levels, along with these lifestyle strategies, are crucial to minimizing the risk of complications related to type 1 & 2 diabetes.
Key Tips for a Healthier Lifestyle:
- Engage in regular outdoor activities.
- Incorporate a balanced diet with local produce.
- Join community wellness initiatives for support.
- Practice stress management techniques like yoga.
Remember, every small step you take can lead to significant improvements in your health and well-being.
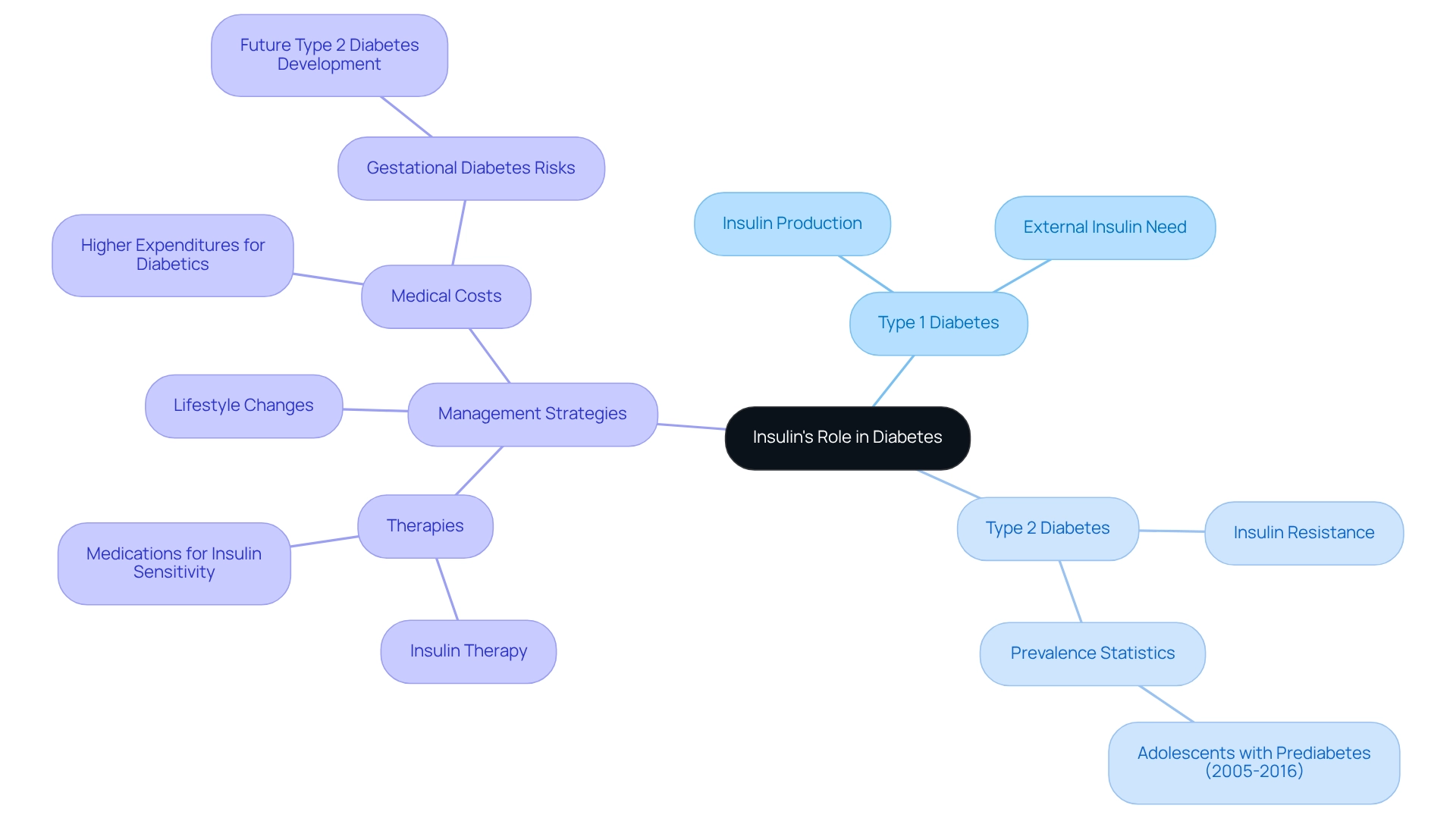
Insulin’s Role: How It Functions in Type 1 and Type 2 Diabetes
Insulin is a crucial hormone produced by the pancreas, playing a vital role in facilitating the absorption of glucose from the bloodstream into cells for energy. For those living with insulin-dependent conditions, the pancreas generates minimal to no insulin, making external insulin delivery essential for managing blood sugar levels. Conversely, individuals with type 1 & 2 diabetes may produce insulin, but their bodies often struggle to use it efficiently due to insulin resistance. This resistance is particularly concerning, as recent data indicates that around 18% of adolescents aged 12 to 18 experienced prediabetes between 2005 and 2016, highlighting the growing prevalence of insulin resistance among younger populations.
Understanding insulin’s role in managing blood sugar conditions is more important than ever. Research shows that the average medical costs for individuals diagnosed with diabetes are 2.6 times higher than for those without the condition, underscoring the financial burden associated with poor glycemic control. Additionally, gestational glucose intolerance affects 2% to 10% of pregnancies in the U.S., posing risks for both mothers and infants. Alarmingly, about 50% of women who experience this condition go on to develop type 1 & 2 diabetes later in life, emphasizing the need for effective monitoring and management of blood sugar levels during pregnancy.
At Integrative Wellness Center, Dr. Jason Shumard emphasizes that functional medicine provides safe, effective, and lasting solutions to chronic health issues, including type 1 & 2 diabetes. It’s essential for everyone with this condition to maintain balanced blood sugar levels. While insulin therapy remains a cornerstone of treatment for insulin-dependent conditions, managing non-insulin-dependent diabetes often involves lifestyle changes and medications aimed at improving insulin sensitivity. By understanding the unique roles of insulin in type 1 & 2 diabetes, patients can better appreciate the importance of adhering to their treatment plans and making informed lifestyle choices to enhance their overall health.
If you’re interested in learning more about how Dr. Shumard can support you in managing your condition, please contact the Integrative Wellness Center or sign up for our upcoming events.
Lifestyle Factors: Managing Type 2 Diabetes Through Diet and Exercise
Successfully handling condition 2 can feel overwhelming, but it’s important to recognize that significant lifestyle changes, especially in nutrition and physical activity, can lead to positive outcomes. A balanced diet rich in whole foods, fiber, and healthy fats is crucial for regulating blood sugar levels. Many patients find that focusing on specific dietary strategies can make a real difference, particularly when considering how education and urban living conditions influence health. Regular physical activity, including aerobic exercises and strength training, is equally vital. It not only enhances insulin sensitivity but also supports achieving a healthy weight. Recent insights suggest that incorporating physical activity into daily routines can greatly improve insulin sensitivity, making it a fundamental aspect of managing diabetes-related conditions.
Establishing achievable objectives and gradually integrating these lifestyle adjustments can promote lasting improvements in well-being. Real-life stories show that individuals who embrace these practices often experience significant enhancements in their overall health. Moreover, the latest dietary guidelines emphasize the importance of nutritional education and the availability of healthy foods. These elements are essential in reducing wellness disparities associated with type 1 & 2 diabetes. By empowering patients with actionable insights and practical tools, we can help them reclaim their health and improve their quality of life, ultimately reducing reliance on conventional medical interventions.
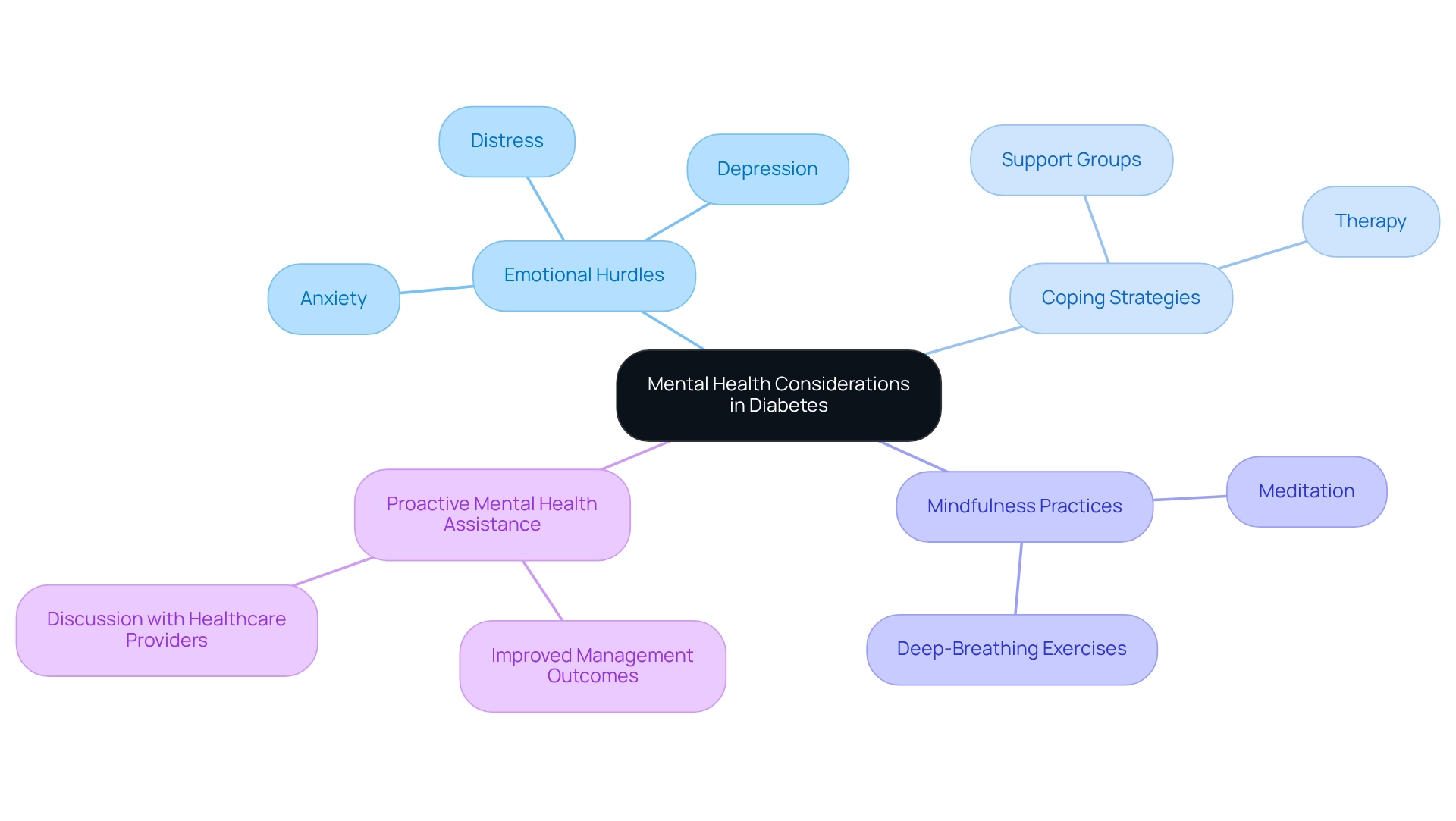
Mental Health Considerations: Coping with Type 1 and Type 2 Diabetes
Coping with this condition often brings emotional hurdles, such as anxiety, depression, and distress related to the illness, impacting nearly 30% of those affected. It’s important to recognize that these feelings can be overwhelming, and acknowledging them is crucial for effective management. Many patients find that participating in support groups fosters a sense of community and shared experience, while therapy or counseling offers personalized coping strategies tailored to their unique needs.
Mindfulness practices and stress-reduction techniques, such as meditation and deep-breathing exercises, can significantly enhance emotional well-being. Have you ever tried these techniques? They can be a gentle way to nurture your mental health. Moreover, research suggests that people who proactively pursue mental health assistance report improved management outcomes for their condition. This emphasizes the significance of tackling mental health alongside physical health.
By promoting a nurturing atmosphere and making use of accessible resources, individuals can manage their health journey with enhanced resilience and a better quality of life. Remember, you are not alone in this journey, and there are supportive paths available to help you thrive.
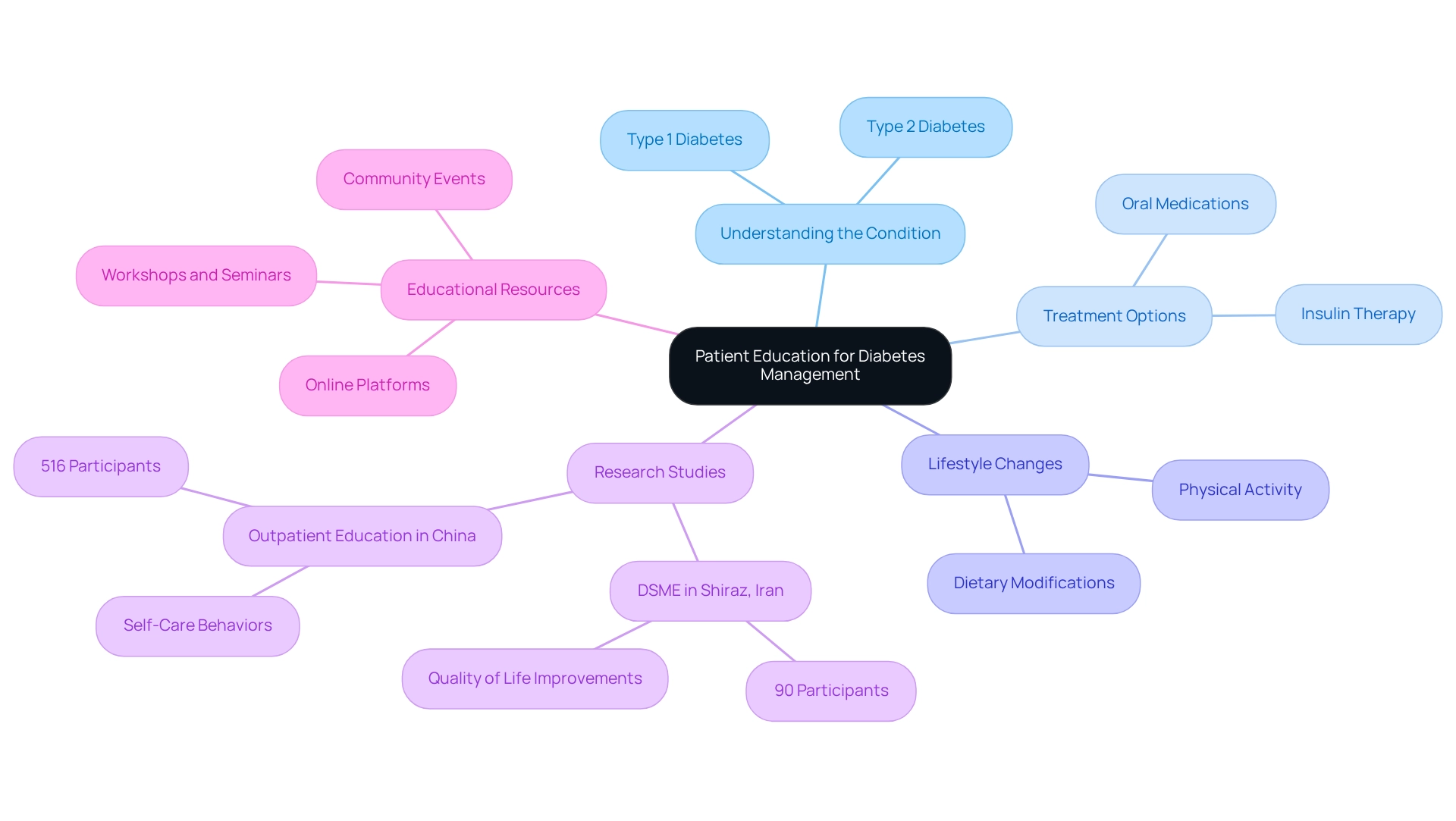
Patient Education: Empowering Individuals to Manage Type 1 and Type 2 Diabetes
Empowering patients through education is essential for effective management of type 1 & 2 diabetes. Understanding your condition, treatment options, and the significance of lifestyle changes enables you to take charge of your health, particularly in relation to type 1 & 2 diabetes. Research shows that self-management education for blood sugar control significantly enhances the quality of life for those with type 1 & 2 diabetes.
For instance, a study involving 90 elderly females with type 1 & 2 diabetes in Shiraz, Iran, demonstrated notable improvements in well-being following these educational interventions. Many patients find that a randomized controlled trial in China, involving 516 participants, validated the positive effects of outpatient education on self-care behaviors and glycemic control for type 1 & 2 diabetes.
Workshops, seminars, and educational resources play a crucial role in improving understanding and promoting proactive management of type 1 & 2 diabetes. Health education programs have shown the ability to cultivate a supportive community, allowing individuals to exchange experiences and strategies. This cooperative atmosphere not only enhances confidence but also underscores the importance of ongoing education in effectively managing your condition.
Present trends in health education highlight the availability of varied resources, such as online platforms and community events, which cater to different learning preferences.
By offering access to these educational materials, you are more prepared to manage your condition. The influence of education on management is significant, as demonstrated by testimonials from participants who express feeling empowered and more in command of their well-being. Ultimately, a well-informed patient is a more effective manager of their condition, leading to improved health outcomes and a reduced reliance on conventional medical interventions.
To learn more about how you can manage your condition and explore personalized care options, call Integrative Wellness Center at 858-564-7081 today for a FREE consultation.
Summary of Key Differences: Type 1 vs. Type 2 Diabetes
It’s important to recognize that type 1 & 2 diabetes comes in different forms, each with its own challenges. Form 1 is an autoimmune disorder that necessitates lifelong insulin treatment. In contrast, form 2 is often linked to lifestyle choices and can frequently be managed through dietary adjustments and exercise alone. Many patients find that understanding these differences helps them feel more empowered in their health journey.
Typically, form 1 develops during childhood or adolescence, while form 2 is more common in adults. However, we are seeing an increase in its occurrence among younger individuals. Recent statistics reveal that non-Hispanic Black children experience the highest rates of the second variation of this condition. This highlights the urgent need for focused prevention initiatives to support these communities, as understanding these distinctions is crucial for implementing effective management and treatment strategies tailored to type 1 & 2 diabetes. By acknowledging the struggles patients face and providing supportive guidance, we can foster a nurturing environment for those navigating their diabetes journey. Remember, you are not alone, and there are resources available to help you thrive.
Conclusion
Recognizing the differences between Type 1 and Type 2 diabetes is essential for effective management and prevention. Many patients find that understanding these distinctions can alleviate some of their concerns. Type 1 diabetes, an autoimmune disorder, requires lifelong insulin therapy, while Type 2 diabetes is often influenced by lifestyle choices and can frequently be managed through diet and exercise alone.
The Integrative Wellness Center’s 30-Day Diabetes Reset Program exemplifies a holistic approach to diabetes care. This program empowers individuals to regain control of their health through education, lifestyle modifications, and community support. By focusing on whole foods, regular physical activity, and behavioral coaching, participants can stabilize their blood sugar levels and enhance their overall well-being.
It’s important to recognize that understanding the underlying mechanisms, symptoms, and treatment differences equips individuals to navigate their diabetes journey more confidently. Engaging in support systems, prioritizing mental health, and embracing patient education are vital components that contribute to improved health outcomes. Ultimately, the journey to managing diabetes is not just about treatment; it is about reclaiming one’s well-being through informed choices and supportive community resources.
Taking the first step towards a healthier future is crucial. With the right tools and guidance, lasting health transformation is within reach. Remember, you are not alone on this journey; support is available, and positive change is possible.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at the Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a compassionate approach designed to help individuals manage type 1 and type 2 diabetes through nutritional education, physical activity, and behavioral coaching. It aims to empower participants to rejuvenate their metabolic well-being and stabilize blood sugar levels.
Who leads the 30-Day Diabetes Reset Program?
The program is led by Dr. Jason Shumard, who has nearly two decades of experience in helping patients recover from type 1 and type 2 diabetes.
What are the benefits of participating in the 30-Day Diabetes Reset Program?
Participants often experience improved blood sugar stabilization, renewed energy, and access to ongoing support through seminars and educational resources, fostering a community environment for health transformation.
What are the main differences between type 1 and type 2 diabetes?
Type 1 diabetes is an autoimmune disorder that typically appears in childhood or adolescence, characterized by the destruction of insulin-producing beta cells in the pancreas. Type 2 diabetes involves insulin resistance, often linked to lifestyle factors such as obesity and poor dietary choices.
What symptoms should individuals look out for regarding type 1 and type 2 diabetes?
Common symptoms include increased thirst, frequent urination, extreme hunger, fatigue, and blurred vision. Type 1 symptoms can develop quickly, while type 2 symptoms often appear gradually, highlighting the need for regular screening.
How can individuals manage their diabetes more effectively?
Effective management includes recognizing symptoms, implementing tracking methods like fitness apps, setting SMART goals, and engaging in regular outdoor activities, which can improve insulin sensitivity and overall well-being.
Why is it important to understand the causes of type 1 and type 2 diabetes?
Understanding the distinct causes and traits of each type is crucial for developing tailored management approaches, which can significantly enhance the support provided to patients in managing their conditions effectively.
What lifestyle strategies can help manage diabetes?
Embracing a balanced diet rich in whole foods, engaging in regular physical activity, staying hydrated, and managing stress through practices like yoga or meditation can all contribute to better blood sugar regulation and overall health.