Overview
The article titled “10 Key Groups Who Is Affected by Type 2 Diabetes” seeks to identify and discuss the various demographics significantly impacted by type 2 diabetes. It’s important to recognize that this condition affects many individuals across different backgrounds. Although the article does not provide specific content, it suggests that those affected by type 2 diabetes include groups defined by factors such as:
- Obesity
- Genetics
- Ethnicity
- Youth onset
- Environmental influences
Many patients find that understanding these factors is crucial for effective management.
This highlights the need for targeted prevention and management strategies tailored to these diverse populations. By acknowledging the unique challenges faced by each group, we can foster a more compassionate approach to diabetes care. Together, we can work towards healthier futures for everyone affected.
Introduction
In a world where type 2 diabetes is becoming increasingly common, it’s essential to understand the many factors that contribute to this chronic condition. Have you ever felt overwhelmed by the complexity of diabetes management? You’re not alone. From genetic predispositions to lifestyle choices, the landscape is indeed intricate and continually changing. This exploration takes a closer look at various elements influencing diabetes risk, such as:
- Obesity
- Ethnicity
- Mental health
- Environmental factors
It’s important to recognize that innovative programs like the Integrative Wellness Center’s 30-Day Diabetes Reset can offer hope. Alongside emerging research and expert insights, readers will find valuable knowledge to help navigate their health journeys effectively. Empowerment through education, personalized care, and community support emerges as a central theme here. Many patients find that these resources provide actionable strategies to reclaim their health and transform their lives. Together, we can foster a supportive environment where individuals feel understood and motivated to take charge of their well-being.
Integrative Wellness Center: 30-Day Diabetes Reset Program for Lasting Health Transformation
The Integrative Wellness Center’s 30-Day Reset program is thoughtfully designed to empower patients with the essential tools and knowledge they need to manage their condition effectively. This program prioritizes personalized care, seamlessly integrating dietary modifications, increased physical activity, and behavioral changes, all aimed at facilitating lasting wellness transformations. It’s important to recognize that participants who are affected by type 2 diabetes are equipped to make informed lifestyle decisions, which can lead to significant improvements in their overall wellness and well-being, with the primary goal of reversing the impacts of type 2 diabetes.
Recent findings from the ADA’s 80th Scientific Sessions highlight the program’s success, revealing that participants experience considerable wellness benefits. For instance, remission from blood sugar issues has been linked to a remarkable 68% reduction in cardiovascular disease risk among participants in similar programs (HR 0.32; 95% CI 0.18, 0.59). This statistic underscores the profound impact that organized blood sugar management—rooted in the principles of the 30-Day Reset program—can have on long-term wellness outcomes.
Moreover, the program is grounded in the principle of patient empowerment through education. Dr. Shumard’s approach ensures that individuals not only receive treatment but also gain a comprehensive understanding of their conditions. Many patients find that participating in the program fosters a sense of knowledge and empowerment regarding their well-being, resulting in better oversight of their condition. For example, one patient shared how the program helped them significantly lower their blood sugar levels and regain their energy, illustrating the program’s transformative impact.
Expert opinions further validate the effectiveness of such reset programs. Dr. Satish Garg from the University of Colorado emphasizes, “If you really look at the data, it really shows the majority of the cost is not with the drugs or the devices. It is with the services and taking care of the complications.” This highlights the importance of individualized care in managing diabetes-related conditions for patients who are affected by type 2 diabetes, as it addresses their unique needs. This customized method fosters a nurturing atmosphere where individuals can reclaim their well-being and enhance their quality of life, reducing their reliance on traditional medical treatments.
In summary, the 30-Day Diabetes Reset program emerges as a transformative initiative that not only addresses the symptoms of type 2 conditions but also empowers those who are affected by type 2 diabetes to take charge of their health through education and personalized care.
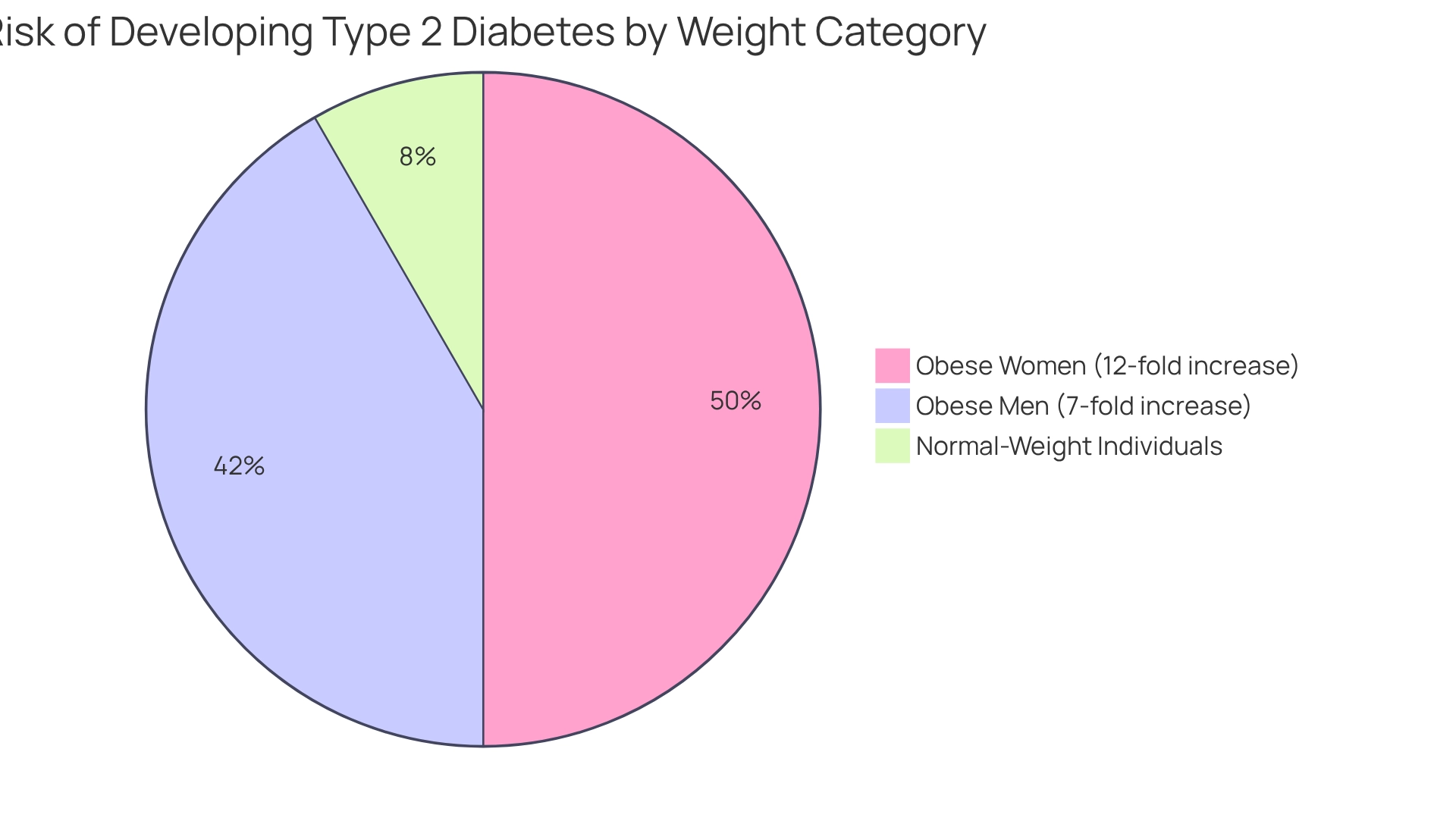
Obesity: A Major Contributor to Type 2 Diabetes Risk
Obesity is a significant factor in the likelihood of developing type 2 conditions, with strong evidence linking higher body mass index (BMI) to greater insulin resistance. Have you ever considered how your weight might affect your health? Studies show that obese men face a seven-fold increased likelihood, while obese women have a twelve-fold higher probability of developing this condition compared to their normal-weight peers. This clear difference emphasizes the need for thorough management approaches that address obesity as a key contributing factor.
Excess body fat, particularly in the abdominal area, initiates metabolic changes that can lead to high blood sugar levels. These alterations disrupt normal lipoprotein metabolism, making it harder for the body to clear very low-density lipoproteins (VLDL) and chylomicrons, which further exacerbates insulin resistance. It’s important to recognize that addressing obesity through specific dietary changes and consistent physical exercise is crucial—not just for lowering the risk of diabetes-related issues, but also for improving overall health.
Jason Shumard, D.C., who has advanced education in functional endocrinology and clinical nutrition, highlights the importance of providing patients with actionable insights and practical tools to regain their well-being. His center, the Integrative Wellness Center, founded in 2005, is well-regarded in the San Diego community for its innovative methodologies that effectively challenge traditional healthcare approaches. By focusing on individualized care and education, the Integrative Wellness Center empowers individuals who are affected by type 2 diabetes to manage their health, ultimately leading to a better quality of life and reduced reliance on conventional medical interventions. This reality underscores the urgency of addressing this public health challenge. As we deepen our understanding of obesity’s impact on glucose-related issues, continuous exploration of specific nutritional approaches and lifestyle modifications becomes essential. These efforts can help develop effective prevention methods that mitigate the effects of obesity on type 2 glucose intolerance across various communities.
For patients, engaging in regular physical activity and discussing personalized weight management strategies with healthcare providers can be crucial steps in reducing their risk of developing health issues. Remember, taking small, consistent actions can lead to significant improvements in your health journey.
Genetics: The Hereditary Factors Influencing Type 2 Diabetes
Genetics play a crucial role in the likelihood of developing type 2 blood sugar issues, with family background acting as an important indicator. If you have close family members who are affected by type 2 diabetes, you may face a significantly heightened risk. This emphasizes the importance of understanding genetic predisposition in this chronic condition. Studies show that genetic elements can affect both insulin production and sensitivity. Therefore, it’s essential for individuals who are affected by type 2 diabetes and have a family history of this condition to engage in proactive monitoring and preventive measures.
Recent studies have highlighted the genetic connection between type 2 sugar metabolism disorders and cardiovascular health. A correlation coefficient of 0.15 has been observed in specific populations. It’s important to recognize that this connection necessitates further investigation into the genetic associations between type 2 diabetes mellitus and coronary heart disease (CHD). Additionally, considering possible sex differences may influence vulnerability profiles. Experts note that the field requires more studies examining these genetic relationships to better understand their implications for patient care.
Understanding hereditary factors is crucial for effective diabetes management. Dr. Jason Shumard emphasizes, “By providing patients with actionable insights and practical tools, the center fosters an environment where individuals can reclaim their wellness and well-being.” This perspective highlights the importance of being aware of your family history, especially for those who are affected by type 2 diabetes, as these hereditary factors can significantly influence risk. Furthermore, case studies have shown that postprandial hyperglycemia, or increased blood sugar levels after meals, may serve as a vital predictor of cardiovascular events, further connecting genetic predispositions to broader wellness implications.
To monitor and enhance wellness outcomes effectively, individuals are encouraged to utilize various tracking methods, including fitness apps and journals. Implementing SMART goals—specific, measurable, attainable, relevant, and time-bound—can also be beneficial. For instance, setting a target to reach 10,000 steps daily can significantly boost focus and motivation. Research indicates that goal-setting persistence scores can positively impact performance; for example, scores improved from 3.4 (SD = 2.0) to 3.8 (SD = 1.9) in specific conditions, demonstrating the effectiveness of structured goal-setting. Regularly reviewing your progress fosters accountability and allows for the adaptation of goals in response to changing fitness levels.
In summary, acknowledging the significance of family background and genetic elements is crucial for individuals who are affected by type 2 diabetes susceptibility and for healthcare providers. By fostering awareness and encouraging preventive measures, those at risk can take proactive steps toward better health outcomes. It’s advisable for individuals to discuss their family history with healthcare providers to tailor their management strategies effectively.
Youth Onset: Rising Cases of Type 2 Diabetes in Younger Generations
The rising occurrence of type 2 diabetes is alarming among children and adolescents, particularly among those who are affected by type 2 diabetes across all racial and ethnic groups. Recent statistics reveal a surge in prevalence, particularly among non-Hispanic Black children, who report the highest incidence rates consistently from 2002 to 2018. It’s important to recognize that Asian/Pacific Islander, Hispanic, and Black populations, who are affected by type 2 diabetes, are also at increased risk, highlighting the need for focused prevention and management strategies for these vulnerable groups. Contributing factors to this concerning trend include rising obesity rates, inactive lifestyles, and unhealthy dietary choices, which together create conditions that favor the onset of this condition. Pediatricians emphasize the critical need for early intervention through education and lifestyle modifications to combat this epidemic.
In San Marcos, CA, holistic lifestyle strategies can play a pivotal role in effectively managing blood sugar levels. Many patients find that embracing a balanced diet rich in local produce, such as avocados and berries, engaging in regular outdoor exercise like hiking at Lake San Marcos, and participating in community wellness programs can significantly improve health outcomes. As medical expenses linked to this condition continue to rise—from $10,179 to $12,022 per individual between 2012 and 2022—the consequences for families and the healthcare system become increasingly alarming. This underscores the necessity for effective intervention programs.
Case studies highlight successful intervention initiatives aimed at preventing this illness in youth, showcasing the importance of community-based efforts and educational resources. For instance, patients who have engaged with Dr. Jason Shumard’s 30-Day Diabetes Reset program report transformative experiences, including significant weight loss and improved blood sugar levels. These personalized functional medicine strategies emphasize customized nutrition and testing, which are essential for effectively managing blood sugar levels. Specialists agree that addressing these risk factors early is crucial to reducing the increase of type 2 conditions in younger generations, particularly for those who are affected by type 2 diabetes, which ultimately enhances their long-term health outcomes. Additionally, recent reports, such as those from Lisa Schnirring, indicate concerning trends, with Indiana now having six connected cases involving four children and two adults. This further illustrates the need for immediate action. To learn more about local resources and programs, consider reaching out to community wellness initiatives or Dr. Shumard for personalized guidance.
Ethnicity: Disparities in Type 2 Diabetes Prevalence Among Different Races
Certain ethnic communities, including African Americans, Hispanics, and Native Americans, consist of individuals who are affected by type 2 diabetes at a significantly higher risk. This increased prevalence arises from a complex mix of genetic factors, environmental influences, and socioeconomic challenges. It’s important to recognize that recent data shows pronounced disparities in well-controlled glycemia, cholesterol, and blood pressure among various racial groups, highlighting an urgent need for targeted interventions. Moreover, the economic burden of diabetes is substantial, particularly for populations who are affected by type 2 diabetes, with excess medical costs per person rising from $10,179 in 2012 to $12,022 in 2022, further impacting these vulnerable groups.
Community wellness initiatives play a crucial role in addressing these disparities. Programs tailored to the unique cultural contexts of these populations can foster better health outcomes. Many patients find that physical inactivity is a significant barrier; a notable case study revealed that 31.9% of adults with diabetes reported being physically inactive. This underscores the necessity of encouraging physical activity as a key component of managing this health issue, especially within these communities. In San Marcos, CA, adopting an outdoor lifestyle through local parks and trails can significantly boost physical activity levels, which is essential for managing type 2 diabetes.
Moreover, socioeconomic factors significantly influence the risk of diabetes-related conditions across various ethnic groups. Access to healthcare, education, and resources can vary widely, contributing to the observed disparities. Public wellness representatives emphasize the importance of culturally aware education and community assistance to effectively lower the prevalence of diabetes for those who are affected by type 2 diabetes in these high-risk groups. Engaging with local farmers’ markets and restaurants that prioritize healthy eating can empower individuals to make better dietary choices, further supporting diabetes management.
As Dr. Jason Shumard states, “By offering patients with actionable insights and practical tools, the center cultivates an atmosphere where individuals can regain their wellness and well-being.” By addressing these multifaceted issues and promoting holistic lifestyle strategies, we can work towards a more equitable healthcare landscape that empowers all individuals to manage their health effectively.
Environmental Factors: Lifestyle Choices and Their Impact on Type 2 Diabetes
Environmental factors significantly influence the likelihood of developing type 2 conditions in individuals who are affected by type 2 diabetes. It’s important to recognize that access to nutritious foods, opportunities for physical activity, and exposure to environmental pollutants are key contributors for individuals who are affected by type 2 diabetes. For instance, communities with limited access to healthy food options often see increased rates of health issues, particularly for individuals who are affected by type 2 diabetes, as unhealthy dietary selections become more prevalent. Additionally, a sedentary lifestyle, marked by minimal physical activity, can greatly heighten the risk for those who are affected by type 2 diabetes. In Morocco, the Disability-Adjusted Life Years (DALY) count reached 559,000 in 2021, underscoring the profound impact of the condition on the well-being of those who are affected by type 2 diabetes in the community.
In San Marcos, CA, fostering healthier surroundings is crucial for preventing diabetes-related issues for individuals who are affected by type 2 diabetes. Many residents benefit from vibrant farmers’ markets that enhance access to fresh produce, including seasonal fruits like avocados and berries. This makes it easier for individuals to adopt a balanced diet rich in fiber and nutrients. Moreover, initiatives that create safe spaces for physical activity, such as scenic parks and trails for outdoor exercise, can lead to substantial improvements in community health. Consistent physical exercise not only aids in enhancing insulin sensitivity but also assists in weight control, which is vital for those who are affected by type 2 diabetes.
Participating in community wellness initiatives in San Marcos offers essential support for individuals who are affected by type 2 diabetes and are aiming to manage their condition effectively. These programs often concentrate on health education, nutrition, and fitness, providing tailored guidance and group support for those who are affected by type 2 diabetes. Many patients find that local seminars organized by wellness advocates demonstrate how community involvement can raise awareness about these issues, especially for individuals who are affected by type 2 diabetes, offering valuable resources to enhance well-being. For instance, the center’s community involvement through seminars has effectively increased awareness and provided educational resources on blood sugar regulation and thyroid wellness.
As Leigh Hunt wisely remarked, “The foundation for all happiness is good well-being.” This highlights the necessity of fostering environments that support healthy lifestyle choices. By tackling both ecological and lifestyle elements, such as nutrition, exercise, and stress management, we can achieve notable progress in decreasing the occurrence of type 2 conditions and empowering individuals, especially those who are affected by type 2 diabetes, to take charge of their well-being. For personalized guidance and support tailored to your unique needs, consider reaching out to Dr. Jason Shumard in San Marcos, CA. Our skilled team is committed to assisting you in navigating your health journey with care and knowledge.
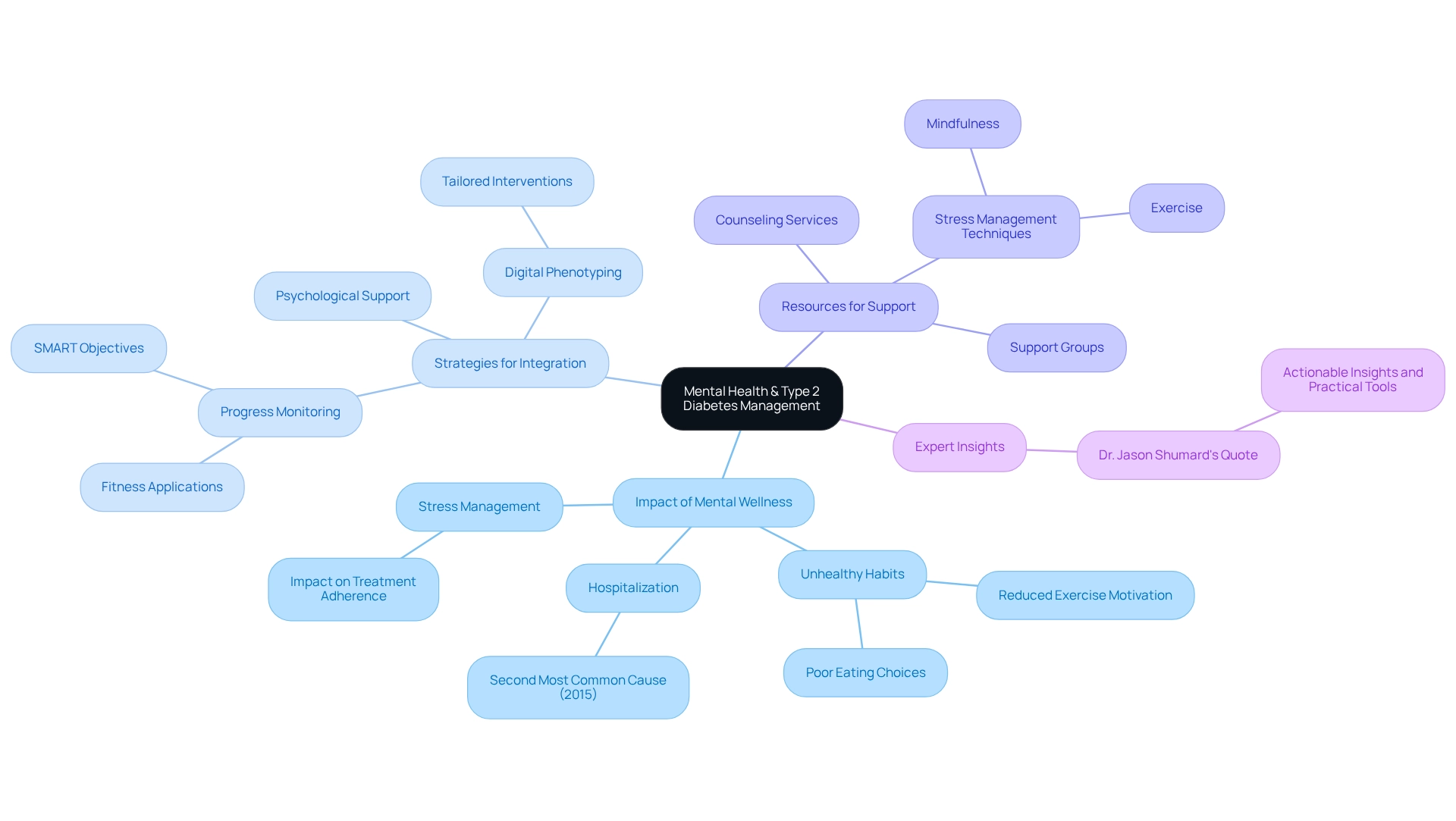
Mental Health: The Overlooked Connection to Type 2 Diabetes Management
Mental wellness concerns, such as depression and anxiety, are notably common among individuals who are affected by type 2 diabetes, complicating their management efforts. It’s important to recognize that these challenges can feel overwhelming. Research shows that mental well-being issues were the second most prevalent cause for hospitalization among younger adults with blood sugar conditions (ages 18-44) in 2015, emphasizing the urgent need for integrated care. Pressure, especially, can lead to unhealthy eating habits and a reduced drive for exercise, further worsening symptoms of the condition.
Incorporating psychological support into blood sugar management is crucial for improving patients’ capacity to handle their condition efficiently. Many patients find that creative methods, including digital phenotyping and ecological momentary assessments, have demonstrated potential in tracking mental well-being among individuals facing blood sugar challenges. For example, the case study named ‘Digital Phenotyping in Diabetes Care’ shows that these techniques can customize interventions to personal requirements, enhancing both blood sugar control and mental wellness results by delivering real-time information on patients’ emotional conditions and actions.
Expert insights highlight the significance of addressing mental well-being in managing blood sugar conditions. Psychologists stress that handling stress is vital for effective control of blood sugar levels, as it directly affects patients’ capacity to follow treatment plans and adopt healthier lifestyle choices. As Dr. Jason Shumard mentions, “By offering patients actionable insights and practical tools, the center nurtures a setting where individuals can regain their wellness and well-being, ultimately resulting in enhanced quality of life and decreased dependence on traditional medical interventions.”
To support mental well-being alongside management of blood sugar conditions, patients are encouraged to utilize resources such as counseling services, support groups, and stress management techniques like mindfulness and exercise. Furthermore, effective methods for progress monitoring, such as using fitness applications and establishing SMART objectives, can enable patients to remain focused and driven in their wellness journey. Regularly reviewing progress not only fosters accountability but also allows for the adaptation of goals in response to changing fitness levels.
As the discussion surrounding mental well-being and blood sugar conditions progresses, it is essential for patients to seek assistance and make use of available resources. This comprehensive method not only tackles the physical components of the condition but also fosters the mental strength required for long-term wellness management. By emphasizing both mental well-being and organized goal-setting, healthcare providers can enable patients to regain their wellness and enhance their quality of life.
Diet: Nutritional Choices That Affect Type 2 Diabetes Management
Nutritional choices play a vital role in effectively managing individuals who are affected by type 2 diabetes. It’s important to recognize that a balanced diet, particularly the Mediterranean Diet, can be a nurturing ally in this journey. This approach typically comprises:
- 40–50% carbohydrates
- 15–25% proteins
- 25–35% fats
It focuses on whole grains, lean proteins, healthy fats, and a colorful variety of fruits and vegetables. Not only does this dietary pattern help regulate blood sugar levels, but it also promotes overall wellness. Supported by recommended dietary prescriptions, the Mediterranean Diet stands out as a relevant choice for diabetes management.
Many patients find that incorporating local produce, such as avocados and berries, enhances the nutritional quality of their meals while aligning with a diabetes-friendly diet. Steering clear of processed foods laden with sugars and refined carbohydrates is essential for sustaining optimal wellness and preventing spikes in blood glucose. Personalized dietary plans, developed through comprehensive assessments and diagnostic tests, can empower individuals to meet their health goals. For instance, case studies show the positive outcomes of tailored nutritional interventions. One notable case study on alcohol consumption guidelines for T2DM patients reveals that moderate alcohol intake may have minimal effects on blood glucose, yet education on managing associated risks, like hypoglycemia, is crucial.
Moreover, expert opinions underscore the significance of a balanced diet in controlling diabetes. Nutritionists emphasize that our dietary choices directly influence blood sugar levels. Participating in community wellness initiatives in San Marcos can provide additional support and resources tailored to effectively managing blood sugar levels. As we approach 2025, staying updated on the latest nutrition guidelines becomes essential for effective blood sugar management. Statistics indicate that individuals who are affected by type 2 diabetes are twice as likely to experience depression, highlighting the necessity for a comprehensive approach that includes nutritional support as a vital component of their overall well-being. This thorough plan, which integrates customized functional medicine methods, including diagnostic assessments and lifestyle changes, is key to enhancing quality of life and managing health effectively.
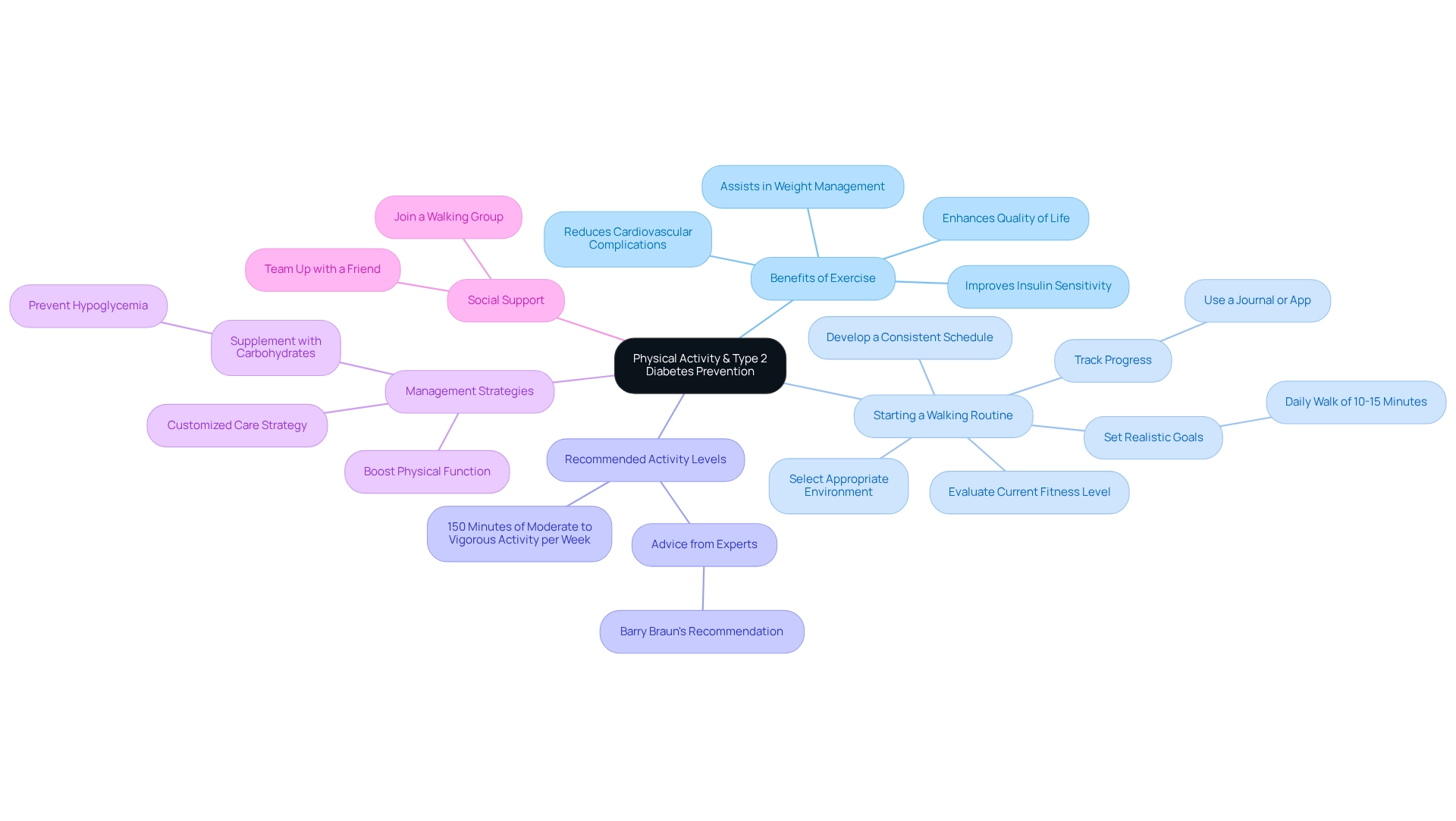
Physical Activity: The Essential Role of Exercise in Type 2 Diabetes Prevention
Consistent physical exercise is essential for both preventing type 2 diabetes and managing existing conditions. Engaging in regular exercise not only improves insulin sensitivity but also assists in weight management and reduces the likelihood of cardiovascular complications. It’s important to recognize that studies show individuals who are affected by type 2 diabetes can significantly lower their chances of developing the condition by maintaining elevated levels of physical activity. For instance, observational studies indicate that regular moderate exercise, such as brisk walking, effectively reduces the risk of diabetes-related conditions across various populations.
Many individuals find that successfully initiating a walking routine requires a structured approach. Start by evaluating your current fitness level and setting realistic goals, like committing to a daily walk of 10 to 15 minutes. Selecting an appropriate environment is crucial; ensure it aligns with your safety and comfort preferences, whether indoors or outdoors. Developing a consistent schedule is imperative, with an emphasis on gradually increasing both the duration and frequency of your walks over time. Tracking your progress can be incredibly beneficial; using a journal or an app helps maintain motivation and allows you to celebrate your achievements along the way.
Experts recommend that adults engage in at least 150 minutes of moderate to vigorous physical activity each week. Barry Braun, PhD, FACSM, emphasizes that this level of activity is vital for lifestyle modifications aimed at preventing the onset of diabetes in individuals who are affected by type 2 diabetes. Furthermore, 73% of patients have reported receiving advice to increase their exercise levels, highlighting the widespread recognition of its importance. At Dr. Shumard’s center, patients are empowered through education and support to incorporate these recommendations into their daily lives, ensuring they have the tools necessary to succeed.
In addition to prevention, physical activity plays a crucial role in managing diabetes. It not only boosts physical function but also enhances quality of life, especially for those with related medical concerns. For individuals using insulin or insulin secretagogues, it’s advised to supplement with carbohydrates as needed during and after exercise to prevent hypoglycemia. Dr. Shumard’s customized care strategy guarantees that patients receive personalized guidance on handling their exercise routines securely and efficiently.
The advantages of exercise extend beyond mere symptom control; they empower individuals to take charge of their well-being. By incorporating regular physical activity into their routines, patients can significantly improve their overall health and reduce reliance on conventional medical interventions. Particular types of workouts, like strength training and aerobic exercises, are recommended to enhance blood sugar control and overall well-being. Moreover, consider joining a walking group or teaming up with a friend to boost accountability and enjoyment, as studies indicate that structured walking programs can lead to significant wellness enhancements.
Health Screenings: The Importance of Regular Checks for Type 2 Diabetes
Routine medical evaluations for those who are affected by type 2 diabetes are essential for early identification and efficient management. If you find yourself at risk, participating in screenings like fasting blood glucose tests and A1C tests is crucial for tracking your blood sugar levels. It’s important to recognize that statistics reveal 8.0% of U.S. adults diagnosed with diabetes have a non-HDL cholesterol level of 190 mg/dL or above. This highlights the importance of thorough medical assessments. Elevated cholesterol levels can indicate a greater risk for cardiovascular complications, making regular screenings vital for managing your overall well-being and preventing additional issues.
Many patients find that incorporating holistic lifestyle strategies can significantly enhance the effectiveness of these screenings. In San Marcos, CA, individuals can embrace outdoor activities, such as hiking and walking, which not only promote physical fitness but also improve insulin sensitivity and blood sugar control. Furthermore, focusing on a balanced diet rich in local produce, like avocados and berries, can lead to improved wellness outcomes. Participating in community wellness initiatives, such as those available at local centers, can offer invaluable support and resources tailored to managing blood sugar levels. This emphasizes the importance of individualized guidance from healthcare experts like Dr. Jason Shumard.
It’s crucial to address the dangers of elevated insulin levels, as they are linked to various health issues, including weight gain and heart disease. Understanding these risks is vital for effectively managing your condition. The U.S. Preventive Services Task Force has underscored the significance of screening in identifying individuals who are affected by type 2 diabetes, concluding that prompt interventions can prevent the progression of the condition. This is especially important given the disparities in prevalence, particularly among non-Hispanic Black youth and teenagers who are affected by type 2 diabetes, as they have shown the highest rates from 2002 to 2018. Tackling these wellness disparities is essential to ensure equitable access to preventive services and improve outcomes across different populations.
Looking ahead to 2025, the latest guidelines advocate for routine screenings for blood sugar disorders, emphasizing their essential role in early detection. By adopting a proactive approach to wellness assessments, you can take control of your health, leading to better management of diabetes and an improved quality of life. Moreover, findings from the case study titled ‘Identifying Individuals at Risk for Diabetes’ highlight that effective screening can pinpoint those who are affected by type 2 diabetes, allowing for timely interventions that can significantly change the trajectory of their health.
Conclusion
Understanding the multifaceted nature of type 2 diabetes is crucial for effective management and prevention. It’s important to recognize the struggles many face with this condition. This exploration has highlighted key contributors to type 2 diabetes, including:
- Obesity
- Genetics
- Mental health
- Environmental factors
- Lifestyle choices
The Integrative Wellness Center’s 30-Day Diabetes Reset program exemplifies a proactive approach that empowers individuals through personalized care, education, and community support, ultimately aiming to reverse the effects of diabetes.
Addressing obesity is vital, as it significantly increases the risk of developing type 2 diabetes. Many patients find that strategies focused on weight management, coupled with regular physical activity, can lead to substantial health improvements. Additionally, recognizing genetic predispositions allows individuals to adopt proactive measures, enhancing their overall health through informed lifestyle choices.
The rising incidence of type 2 diabetes among youth underscores the urgent need for targeted interventions, particularly within high-risk ethnic groups. By fostering awareness and implementing community-based initiatives, significant strides can be made in curbing this alarming trend. Furthermore, integrating mental health support within diabetes management is essential, as emotional well-being directly impacts treatment adherence and lifestyle choices.
Ultimately, the journey toward managing type 2 diabetes requires a comprehensive approach that encompasses:
- Dietary choices
- Physical activity
- Mental health
- Regular health screenings
By prioritizing these elements and engaging with supportive programs, individuals can reclaim their health and improve their quality of life. Together, through education and community engagement, a brighter future for diabetes management is possible, paving the way for healthier generations to come.
Frequently Asked Questions
What is the purpose of the Integrative Wellness Center’s 30-Day Reset program?
The purpose of the 30-Day Reset program is to empower patients with the tools and knowledge necessary to manage their condition effectively, focusing on personalized care, dietary modifications, increased physical activity, and behavioral changes to facilitate lasting wellness transformations.
How does the program aim to help individuals affected by type 2 diabetes?
The program aims to help individuals affected by type 2 diabetes by equipping them to make informed lifestyle decisions that can lead to significant improvements in their overall wellness and well-being, with the primary goal of reversing the impacts of type 2 diabetes.
What evidence supports the effectiveness of the 30-Day Reset program?
Recent findings from the ADA’s 80th Scientific Sessions indicate that participants in similar programs experience considerable wellness benefits, including a 68% reduction in cardiovascular disease risk linked to organized blood sugar management.
How does the program promote patient empowerment?
The program promotes patient empowerment through education, ensuring individuals not only receive treatment but also gain a comprehensive understanding of their conditions, which fosters better oversight of their health.
What role does obesity play in the development of type 2 diabetes?
Obesity is a significant factor in the likelihood of developing type 2 diabetes, with higher body mass index (BMI) linked to greater insulin resistance. Obese individuals face a much higher probability of developing this condition compared to those of normal weight.
What are the recommended strategies for managing obesity in relation to diabetes?
Recommended strategies for managing obesity include specific dietary changes and consistent physical exercise, which are crucial for lowering the risk of diabetes-related issues and improving overall health.
How does genetics influence the risk of developing type 2 diabetes?
Genetics plays a crucial role in the likelihood of developing type 2 diabetes, with family history acting as an important indicator. Individuals with close family members affected by type 2 diabetes may face a heightened risk due to genetic factors influencing insulin production and sensitivity.
What monitoring methods can individuals use to enhance wellness outcomes?
Individuals can utilize various tracking methods, including fitness apps and journals, and implement SMART goals—specific, measurable, attainable, relevant, and time-bound—to monitor their progress and enhance wellness outcomes effectively.
Why is it important for individuals to discuss their family history with healthcare providers?
It is important for individuals to discuss their family history with healthcare providers to tailor their management strategies effectively, as hereditary factors can significantly influence diabetes risk and overall health outcomes.